Abstract
Objectives
The purpose of this study was to evaluate in-hospital outcomes among patients with a history of heart failure (HF) hospitalized with coronavirus disease-2019 (COVID-19).
Background
Cardiometabolic comorbidities are common in patients with severe COVID-19. Patients with HF may be particularly susceptible to COVID-19 complications.
Methods
The Premier Healthcare Database was used to identify patients with at least 1 HF hospitalization or 2 HF outpatient visits between January 1, 2019, and March 31, 2020, who were subsequently hospitalized between April and September 2020. Baseline characteristics, health care resource utilization, and mortality rates were compared between those hospitalized with COVID-19 and those hospitalized with other causes. Predictors of in-hospital mortality were identified in HF patients hospitalized with COVID-19 by using multivariate logistic regression.
Results
Among 1,212,153 patients with history of HF, 132,312 patients were hospitalized from April 1, 2020, to September 30, 2020. A total of 23,843 patients (18.0%) were hospitalized with acute HF, 8,383 patients (6.4%) were hospitalized with COVID-19, and 100,068 patients (75.6%) were hospitalized with alternative reasons. Hospitalization with COVID-19 was associated with greater odds of in-hospital mortality as compared with hospitalization with acute HF; 24.2% of patients hospitalized with COVID-19 died in-hospital compared to 2.6% of those hospitalized with acute HF. This association was strongest in April (adjusted odds ratio [OR]: 14.48; 95% confidence interval [CI]:12.25 to 17.12) than in subsequent months (adjusted OR: 10.11; 95% CI: 8.95 to 11.42; pinteraction <0.001). Among patients with HF hospitalized with COVID-19, male sex (adjusted OR: 1.26; 95% CI: 1.13 to 1.40) and morbid obesity (adjusted OR: 1.25; 95% CI: 1.07 to 1.46) were associated with greater odds of in-hospital mortality, along with age (adjusted OR: 1.35; 95% CI: 1.29 to 1.42 per 10 years) and admission earlier in the pandemic.
Conclusions
Patients with HF hospitalized with COVID-19 are at high risk for complications, with nearly 1 in 4 dying during hospitalization.
Key Words: coronavirus, COVID-19, heart failure
Abbreviations and acronyms: COVID-19, coronavirus disease-2019; HF, heart failure; ICD, International Classification of Diseases; OR, odds ratio; SARS-CoV2, severe acute respiratory syndrome-coronavirus-2
Central Illustration
The coronavirus disease-2019 (COVID-19) pandemic has led to devastating morbidity and mortality worldwide. Underlying comorbidities including diabetes, coronary artery disease, and hypertension are common in patients presenting with more severe forms of COVID-19 (1,2). There is growing evidence of cardiac injury, thrombosis, and ventricular dysfunction that may contribute to increased cardiovascular risk (3, 4, 5). It has been postulated that, because severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) enters cells through the angiotensin-converting enzyme-2 (ACE-2) receptor (6, 7, 8), dysregulations of the renin-angiotensin system may play a role in COVID-19 severity. Patients with underlying heart failure (HF), in whom maladaptive activation of the renin-angiotensin system is common, may be particularly susceptible to COVID-19 complications. Myocardial injury and worsening ventricular function associated with COVID-19 infection have also been reported (9,10). There are currently limited data examining clinical outcomes in patients with a history of HF hospitalized with COVID-19; therefore, we investigated clinical characteristics, resource use, and in-hospital outcomes in patients with HF hospitalized with COVID-19 in a large, administrative U.S. health care database.
Methods
Data sources
Patients with HF were identified in the Premier Healthcare Database (Premier, Inc., Charlotte, North Carolina). The Premier Healthcare Database is a large, multicenter, all-payer database which includes data from more than 1,041 health care entities and health systems in the United States, encompassing more than 8 million annual U.S. hospitalizations in addition to outpatient encounters (11). Data were collected and deidentified by Premier, Inc., and raw data were transferred to and analyzed at Brigham and Women’s Hospital. The Massachusetts General Brigham Institutional Review Board approved the study protocol.
Cohort identification
International Classification of Disease 10th revision (ICD-10) diagnostic codes were used to identify patients with a history of HF who were subsequently hospitalized during the pandemic period, defined as April 1, 2020, to September 30, 2020 (Supplemental Table 1). History of HF was defined based on the presence of either: 1) a qualifying hospitalization with HF from January 1, 2019 to March 31, 2020; or 2) 2 qualifying outpatient encounters with HF over the same time period, a claims-based approach associated with high specificity for HF (12). Hospitalizations during the pandemic period among patients identified as having a history of HF were categorized as being related to acute HF, COVID-19, or other reasons. Subsequent hospitalizations for acute HF were defined by a primary (first-coding position) discharge diagnosis for HF. Hospitalizations with COVID-19-infected patients during the same time frame were defined as those with a primary or secondary discharge diagnosis including the ICD-10 code U07.1 (COVID-19-virus identified), which was introduced by the Centers for Disease Control and Prevention on April 1, 2020 (Supplemental Figure 1). Patients with a primary discharge diagnosis of acute HF and a secondary diagnosis of COVID-19 were categorized as being hospitalized with COVID-19. Only a patient’s first hospitalization in this time period was considered.
Medical conditions were defined using ICD-10 codes reported during hospitalization (Supplemental Table 2). Outcomes during hospitalization were defined by ICD-10 procedure or billing codes (Supplemental Tables 3 and 4). Use of the intensive care unit (ICU) was defined by a billing code for ICU room or daily ventilator management. Discharge disposition and in-hospital mortality were available for all hospitalizations.
Statistical analysis
Baseline characteristics, comorbidities, and presenting characteristics were summarized by hospitalization category (acute HF, COVID-19, other). Use of ICU resources, mechanical ventilatory needs, renal replacement therapy requirements, invasive hemodynamic monitoring, and in-hospital mortality were compared between hospitalization categories by using Pearson’s chi-squared tests. Risk-adjusted odds of in-hospital mortality as well as of the composite of in-hospital mortality or mechanical ventilation in patients with HF hospitalized with COVID-19 were evaluated by multivariate logistic regression. Hospitalization with acute HF served as the reference group. Among patients with HF hospitalized for COVID-19, predictors of the outcomes of in-hospital mortality as well as of in-hospital mortality or mechanical ventilation were assessed using multivariate logistic regression modeling. Statistical analyses were conducted using STATA version 14.2 software (Stata Corp., College Station, Texas). A two-tailed p value < 0.05 was considered statistically significant.
Results
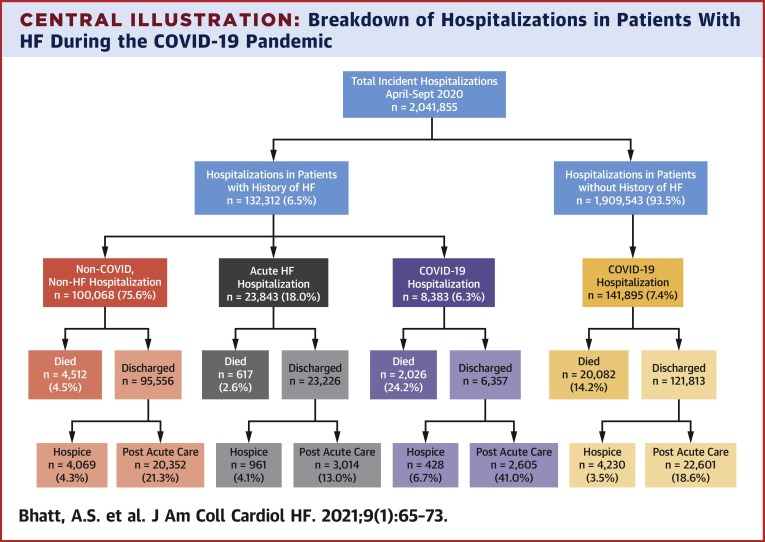
A total of 48,086,075 patient encounters were analyzed in the Premier Healthcare Database to identify 1,212,153 unique patients with a history of HF. From April 1, 2020, to September 30, 2020, there were 2,041,855 incident hospitalizations, of which 132,312 hospitalizations (6.5%) occurred in patients identified as having a history of HF. Among patients with a history of HF hospitalized during the pandemic, 23,843 patients (18.0%) were hospitalized with acute HF, 8,383 patients (6.4%) were hospitalized with COVID-19, and 100,068 patients (75.6%) were hospitalized with other reasons (Central Illustration ). A total of 178 patients (0.8%) had a primary discharge diagnosis of HF and a secondary diagnosis of COVID-19. Among patients hospitalized during the pandemic without a history of HF, 141,895 patients (7.4%) were hospitalized with COVID-19.
Central Illustration.
Breakdown of Hospitalizations in Patients With HF During the COVID-19 Pandemic
This figure shows hospitalizations among patients with HF during the pandemic in comparison to COVID-19 hospitalizations in patients without a history of HF. In-hospital mortality is described by hospitalization type. Among those who survived hospitalization, the proportion of patients requiring post-acute services, and those discharged with hospice services are also reported.
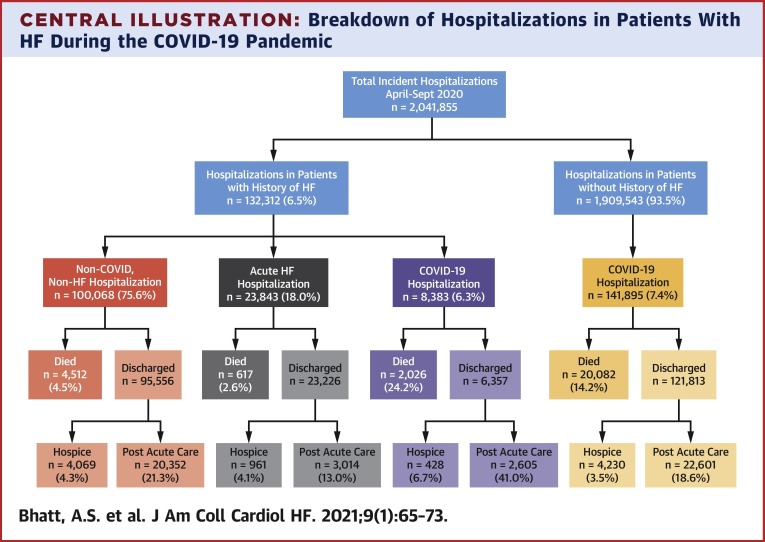
Patients with HF hospitalized with COVID-19 were older, more likely to identify as Black and/or Hispanic, and had higher rates of diabetes and kidney disease than those hospitalized with acute HF and other causes (p < 0.001 for all) (Table 1 ). Patients with HF hospitalized with COVID-19 had significantly greater in-hospital resource use as compared to those hospitalized with acute HF or other reasons. Resource utilization included multifold higher rates of ICU care (29% vs. 15%), mechanical ventilation (17% vs. 6%), and central venous catheter insertion (19% vs. 7%; p < 0.001 for all) (Figure 1 ). Among patients with HF hospitalized with COVID-19, extracorporeal membrane oxygenation (ECMO) was incorporated in the care of 3 patients (0.04%), whereas any form of temporary mechanical circulatory support, including ECMO, was used in 11 patients (0.13%). For reference, among patients without HF hospitalized with COVID-19, rates of ECMO and any temporary mechanical circulatory support use were 0.25% and 0.36%, respectively.
Table 1.
Baseline Characteristics in Patients With History of HF from April 1, 2020, to September 30, 2020
| Other Hospitalizations (n = 100,068) | Acute HF Hospitalizations (n = 23,843) | COVID-19 Hospitalizations (n = 8,383) | |
|---|---|---|---|
| Age, yrs | 70.3 ± 13.4 | 70.4 ± 13.6 | 71.7 ± 13.2 |
| Males | 50,592 (50.6) | 12,758 (53.5) | 4,178 (49.8) |
| Race/ethnicity | |||
| Black Hispanic | 256 (0.3) | 86 (0.4) | 34 (0.4) |
| Black non-Hispanic | 14,983 (15.0) | 4,807 (20.2) | 1,892 (22.6) |
| Other/unknown | 22,332 (22.3) | 5,389 (22.6) | 2,659 (31.7) |
| White Hispanic | 3,430 (3.4) | 904 (3.8) | 406 (4.8) |
| White non-Hispanic | 59,085 (59.0) | 12,657 (53.1) | 3,392 (40.5) |
| Black or Hispanic | 22,442 (22.4) | 6,939 (29.1) | 3,147 (37.5) |
| Discharge month | |||
| April | 26,471 (26.4) | 6,211 (26.0) | 2,781 (33.2) |
| May | 22,826 (22.8) | 5,903 (24.8) | 1,892 (22.6) |
| June | 20,317 (20.3) | 5,094 (21.4) | 1,044 (12.5) |
| July | 16,624 (16.6) | 3,711 (15.6) | 1,511 (18.0) |
| August | 10,463 (10.5) | 2,216 (9.3) | 900 (10.7) |
| September | 3,385 (3.4) | 708 (3.0) | 255 (3.0) |
| Region | |||
| Midwest | 28,589 (28.6) | 6,341 (26.6) | 1,843 (22.0) |
| Northeast | 17,000 (17.0) | 4,212 (17.7) | 2,852 (34.0) |
| South | 43,453 (43.4) | 10,605 (44.5) | 3,062 (36.5) |
| West | 11,044 (11.0) | 2,685 (11.3) | 626 (7.5) |
| Teaching hospital | 2,055 (61.9) | 2,074 (59.5) | 776 (49.1) |
| LVEF Category | |||
| HFrEF “systolic” | 40,500 (40.5) | 13,542 (56.8) | 3,318 (39.6) |
| HFpEF “diastolic” | 40,283 (40.2) | 8,263 (34.7) | 3,486 (41.6) |
| Unspecified | 19,303 (19.3) | 2,038 (8.5) | 1,579 (18.8) |
| Comorbidities | |||
| Obesity | 28,567 (28.5) | 8,478 (35.6) | 2,461 (29.4) |
| Morbid obesity | 16,558 (16.5) | 5,372 (22.5) | 1,425 (17.0) |
| Hypertension | 82,535 (82.5) | 22,819 (95.7) | 6,997 (83.5) |
| Diabetes | 53,785 (53.7) | 13,669 (57.3) | 5,107 (60.9) |
| History of arrhythmia | 54,374 (54.3) | 14,980 (62.8) | 4,548 (54.3) |
| Valvular disease | 20,622 (20.6) | 7,985 (33.5) | 1,417 (16.9) |
| Kidney disease | 52,247 (52.2) | 15,692 (65.8) | 5,020 (59.9) |
| ESKD | 13,609 (13.6) | 2,493 (10.5) | 1,689 (20.1) |
| Smoking | 53,103 (53.1) | 13,170 (55.2) | 3,665 (43.7) |
| Pulmonary disease | 44,353 (44.3) | 11,503 (48.2) | 3,539 (42.2) |
| Asthma | 6,419 (6.4) | 1,515 (6.4) | 628 (7.5) |
| Anemia | 8,500 (8.5) | 2,670 (11.2) | 628 (7.5) |
| Malignancy | 6,562 (6.6) | 708 (3.0) | 290 (3.5) |
Values are mean ± SD or n (%). p < 0.001 for all comparisons.
ESKD = end-stage kidney disease; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; LVEF = left ventricular ejection fraction.
Figure 1.
Resource Use in Patients With HF During the COVID-19 Pandemic
In-hospital resource use among patients with a history of HF discharged from April to September 2020. Resource uses are compared among HF patients hospitalized with COVID-19, acute HF, and other reasons. Hospitalization with COVID-19 among patients with a history of HF was associated with greater resource needs compared to hospitalizations with acute HF and other reasons. p < 0.001 for all comparisons among patients with history of HF. COVID-19 = coronavirus disease-2019; HF = heart failure; Pts = patients; ICU = intensive care unit.
Patients with HF hospitalized with COVID-19 had an in-hospital mortality rate of 24.2% (n = 2,026) compared with 2.6% (n = 617) in patients hospitalized with acute HF and 4.6% (n = 4,542) in patients hospitalized with other reasons during the same time frame. Among patients surviving hospitalization, use of skilled nursing or rehabilitative care was higher in patients hospitalized with COVID-19 (41.0%) compared to those hospitalized with acute HF (13.0%) and other reasons (21.3%) (Central Illustration). For reference, among 141,895 patients without a history of HF who were hospitalized with COVID-19 during the study period, the in-hospital mortality rate was 14.2% and the use of post-acute care services was 18.6% among survivors. After adjustment for demographic and clinical covariates, hospitalization with COVID-19 among patients with HF was strongly associated with greater odds of in-hospital mortality as compared with hospitalization for acute HF. There was heterogeneity in this association by time of hospitalization, with greater odds of in-hospital mortality in those patients discharged in April 2020 (adjusted odds ratio [OR]: 14.48; 95% confidence interval [CI]: 12.25 to 17.12) compared with in those discharged in subsequent months (adjusted OR: 10.11; 95% CI: 8.95 to 11.42; pinteraction <0.001). Hospitalization with COVID-19 also conferred significantly greater odds for the composite outcome of in-hospital mortality or mechanical ventilation as compared with hospitalization with acute HF (Table 2 ).
Table 2.
Univariate and Multivariate Associations of Hospitalization Type in Patients With HF Admitted During the COVID-19 Pandemic
| Hospitalization Type (Reference = HF Hospitalization) | In-Hospital Mortality |
Death or Mechanical Ventilation |
||
|---|---|---|---|---|
| Unadjusted OR | Adjusted OR∗ | Unadjusted OR | Adjusted OR∗ | |
| April 2020 | ||||
| Other hospitalization | 1.82 (1.57–2.11) | 1.91 (1.65–2.22) | 1.84(1.67–2.03) | 1.98 (1.79–2.18) |
| COVID-19 hospitalization | 15.87 (13.55–18.60) | 14.48 (12.25–17.12) | 7.70(6.84–8.66) | 8.04 (7.10–9.12) |
| May–September 2020 | ||||
| Other hospitalization | 1.76 (1.59–1.97) | 1.87 (1.68–2.08) | 1.52 (1.43–1.63) | 1.69 (1.58–1.80) |
| COVID-19 hospitalization | 9.58 (8.50–10.79) | 10.11 (8.95–11.42) | 4.76 (4.38–5.18) | 5.30 (4.86–5.77) |
COVID-19 = coronavirus disease-2019; HF = heart failure; OR = odds ratio.
Adjusted for age, sex, race, ethnicity, region, HF ejection fraction status, obesity status, diabetes mellitus, hypertension, kidney disease, advanced pulmonary disease, history of smoking, and history of malignancy. p < 0.001 for all.
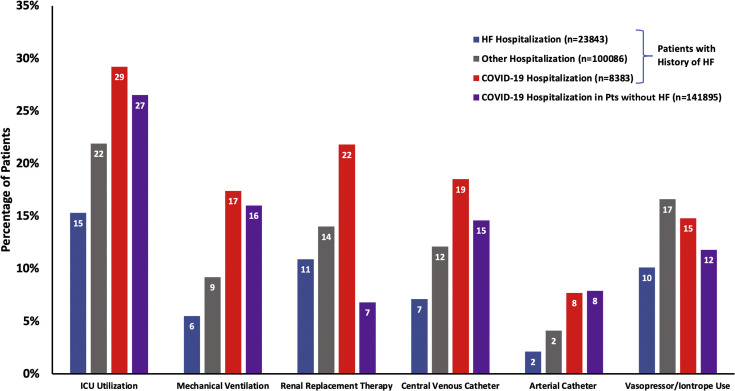
Among patients with HF hospitalized with COVID-19 (n = 8,383 patients), age and admission during earlier months of the pandemic were strongly predictive of adverse outcomes in multivariate analyses (Figures 2A and 2B ). Odds of in-hospital mortality increased with age (adjusted OR: 1.35; 95% CI: 1.29 to 1.42 per 10 years). Odds of in-hospital mortality were also greater in men (adjusted OR: 1.26; 95% CI: 1.13 to 1.40) and in those who were morbidly obese (adjusted OR: 1.25; 95% CI: 1.07 to 1.46), diabetic (adjusted OR: 1.13; 95% CI: 1.01 to 1.26), and had kidney disease (adjusted OR: 1.45; 95% CI: 1.30 to 1.62). Similarly, odds of in-hospital mortality or mechanical ventilation were greater in male patients (adjusted OR: 1.24; 95% CI: 1.12 to 1.37), in patients who were morbidly obese (adjusted OR: 1.52; 95% CI: 1.33 to 1.74), and in diabetic patients (adjusted OR: 1.13; 95% CI: 1.02 to 1.26). History of hypertension was not significantly associated with increased odds of in-hospital mortality alone or need for mechanical ventilation (adjusted OR: 1.04; 95% CI: 0.91 to 1.19) or in-hospital mortality (adjusted OR: 0.99; 95% CI: 0.86 to 1.14) among patients with HF hospitalized with COVID-19.
Figure 2.
Predictors of Adverse In-Hospital Outcomes Among HF Patients Hospitalized with COVID-19
(A) Predictors of in-hospital mortality or mechanical ventilatory need in HF patients hospitalized with COVID-19. This figure shows predictors of in-hospital mortality or mechanical ventilatory needs among patients with a history of HF hospitalized with COVID-19. Odds ratios are reported for clinical covariates of interest. Lowerandupper bounds correspond to 95% confidence intervals [CI]. (B) Predictors of in-hospital mortality in HF patients hospitalized with COVID-19. This figure describes predictors of in-hospital mortality among patients with a history of HF hospitalized with COVID-19. COVID-19 = coronavirus disease-2019; HFpEF = heart failure with preserved ejection fraction; OR = odds ratio.
Discussion
In this analysis of 132,312 patients with HF hospitalized during the COVID-19 pandemic, of whom 8,383 were hospitalized with COVID-19, nearly one in four patients hospitalized with COVID-19 died during hospitalization, corresponding to 14-fold greater odds of dying in April and 10-fold greater odds of dying in subsequent months compared with those hospitalized with acute HF during the same period. Hospitalization with COVID-19 was also associated with multifold increases in the use of resources, including ICU care, advanced hemodynamic monitoring, and renal replacement therapy. In patients surviving hospitalization with COVID-19, more than 40% required advanced supportive services in skilled nursing or rehabilitative care settings. Cardiometabolic risk factors including diabetes, morbid obesity, and kidney disease conferred greater risk of in-hospital mortality among HF patients hospitalized with COVID-19.
The relationship between underlying cardiovascular disease and infection with SARS-CoV-2 is poorly understood, although multiple reports have suggested a bidirectional influence between cardiovascular comorbidities and more severe presentations of COVID-19 (8,13). The prevalence of hypertension and diabetes, both of which are risk factors for adverse outcomes in HF (14,15), appear to be disproportionately high in patients presenting with severe forms of COVID-19 (1,2). This experience, to the best of the current authors’ knowledge, is the largest to date examining hospitalizations among HF patients during the COVID-19 pandemic. Mortality rates among patients with COVID-19 in this HF cohort were substantially higher than reported among broader cohorts, and comparable to rates observed in patients with COVID-19 and active malignancy on chemotherapy (16). Smaller evaluations of patients with heart failure in the United Kingdom (17) and in the United States (New York City) (18) have found comparable in-hospital mortality rates. In the present study, the risk of mortality in patients with HF hospitalized with COVID-19 later in the pandemic was attenuated, which might have been due to expanded testing capabilities, improved health system efficiencies in COVID-19 care, and use of disease-modifying therapy (19). Nevertheless, patients with HF hospitalized with COVID-19 remained at exceptionally high risk of in-hospital mortality, even in later stages of the pandemic, far greater than historical reports of HF patients hospitalized with other respiratory illnesses, including influenza (20).
Patients with HF hospitalized with COVID-19 were more likely to identify as Black and/or Hispanic and had high rates of diabetes and renal disease compared with patients with HF hospitalized with other reasons. These data are consistent with global reports, uncovering possible key health disparities and socioeconomic determinants of health (21). In patients with HF hospitalized with COVID-19, cardiometabolic comorbidities including obesity and diabetes were associated with increased risk of in-hospital mortality. These data are consistent with previous analyses of COVID-19 patient from in diverse cohorts, even among young adults hospitalized with COVID-19 (22, 23, 24). Congruent with other studies, male sex and advanced age were associated with higher risks of adverse in-hospital outcomes (25). Men with HF appeared to have higher circulating levels of ACE-2, the receptor facilitating SARS-CoV2 entry into host cells, and decreased immune response, both of which might have contributed to greater severity of COVID-19 illness (7,26). Acknowledging limitations in differentiating ejection fraction (EF)-based subgroups of HF in claims-based analyses, elevated risk of in-hospital death was consistent in patients with HF with reduced EF and HF with preserved EF. Further research, including from prospective registries such as the American Heart Association COVID-19 Cardiovascular Disease Registry may be helpful in providing additional information regarding prognostic factors among various subtypes of HF when patients are affected by COVID-19 infection.
Biological mechanisms underlying the relationship observed between COVID-19 hospitalization and outcomes in those with HF have not been fully established. Previous experiences with influenza illness have determined that rises in pro-inflammatory cytokines in the setting of acute viral infection contribute to accelerated atherogenesis and can depress myocardial contractility (27). In addition, variations in neurohormonal activity and ACE-2 levels may partially explain the susceptibility of patients with HF to more severe presentations with COVID-19 infection. Upregulation of the neurohormonal axis, including ACE-2 activity, are central components of HF (7,28). As SARS-CoV-2 uses the ACE-2 receptor for host cell entry, patients with HF may have increased susceptibility to more severe forms of viral infection. In addition, impaired innate immunity (29) and inherent endothelial dysfunction (28) may further render patients with HF more vulnerable to COVID-19 and its effects on the microvasculature (30, 31, 32).
Overall, the present data find an exceptionally high risk of poor outcomes in patients with HF hospitalized with COVID-19. Novel risk mitigation strategies may be needed to care for these high-risk patients, including expanded access to virtual care (33) and telemonitoring (34). Efforts to optimize HF status including medication optimization and annual influenza vaccination will be important priorities as the COVID-19 pandemic continues. Given the high rate of morbidity and mortality in patients with HF hospitalized for COVID-19, structured data collection to determine the prevalence of COVID-19 cases in ongoing research efforts will be critical for accurate endpoint ascertainment and regulatory trial data interpretation (35).
Study limitations
First, reliance on administrative coding may have led to misclassification of primary reasons for hospitalization. Previous analyses have shown variable identification of diagnoses for acute HF using administrative data, although coding specificity likely remains high (36). Formal diagnostic codes for COVID-19 were introduced on April 1, 2020; therefore hospitalized patients with COVID-19 earlier in the pandemic could not be captured in this experience. COVID-19 illness was defined by ICD-10 codes alone; documentation of a positive test was not required. Second, in the context of an observational study, unmeasured confounding may explain some of the elevated mortality risk of those hospitalized with COVID-19 and possible delays in coding and reporting in more recent months may introduce additional bias. Data for race, ethnicity, and laboratory markers were not available in all patients. Third, the effect of hospitalization with COVID-19 on other chronic diseases characterized by acute exacerbations is not well established, limiting the ability to compare these findings with other chronic disease states.
Conclusions
Among patients with chronic HF hospitalized with COVID-19, nearly 1 in 4 died in-hospital. Hospitalization with COVID-19 in patients with HF was associated with high use of in-hospital resources. Advanced age, morbid obesity, and diabetes were associated with worse in-hospital outcomes in patients with HF hospitalized with COVID-19. Dedicated and innovative efforts surrounding education and infection control are needed for this high-risk population as the pandemic continues to evolve.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: Hospitalization with COVID-19 in patients with heart failure is associated with particularly high healthcare resource utilization and in-hospital mortality. Predictors of death in patients with HF hospitalized with COVID-19 include advanced age, morbid obesity, and diabetes, among others. Targeted infection control measures and novel care pathways are needed to properly care for this high-risk group.
TRANSLATIONAL OUTLOOK: Patients with HF hospitalized with COVID-19 have high rates of in-hospital death, with nearly 1 in 4 dying in-hospital in the present study. These findings highlight the importance of structured data collection to determine COVID-19 prevalence across ongoing and planned randomized clinical trials in HF. The prevalence of COVID-19 in each individual trial may drastically influence interpretation of regulatory trial data.
Author Disclosures
Dr. Bhatt has received speaker fees from Sanofi Pasteur; and is supported by National Heart, Lung, and Blood Institute T32 post-doctoral training grant T32HL007604. Dr. Jering is supported by National Heart, Lung, and Blood Institute T32 post-doctoral training grant T32HL007604. Dr. Vaduganathan has received grants from Harvard Catalyst, grants and personal fees from Amgen, and personal fees from AstraZeneca, Baxter HealthCare, Bayer AG, Boehringer Ingelheim, Cytokinetics, and Relypsa outside the submitted work. Dr. Claggett has received personal fees from Amgen, Boehringer Ingelheim, Corvia, MyoKardia, and Novartis outside the submitted work. Dr. Cunningham is supported by National Heart, Lung, and Blood Institute T32 post-doctoral training grant T32HL007604. Dr. Rosenthal is an employee of Premier Inc., which curates the Premier Healthcare Database. Dr. Signorovitch is an employee of Analysis Group, Inc. Dr. Thune has received lecture fees from Bristol-Myers Squibb; and has received personal fees and travel support from Novartis. Dr. Vardeny has received research support from U.S. National Institutes of Health; and is a consultant for Sanofi-Pasteur. Dr. Solomon has received grants from Alnylam, Amgen, AstraZeneca, Bellerophon, Bayer, Bristol-Myers Squibb, Celladon, Cytokinetics, Eidos, Gilead, GlaxoSmithKline, Ionis, Lone Star Heart, Mesoblast, MyoKardia, Neurotronik, National Institutes of Health/National Heart, Lung, and Blood Institute, Novartis, Respicardia, Sanofi Pasteur, and Theracos; and has received personal fees from Akros, Alnylam, Amgen, Arena, AstraZeneca, Bayer, Bristol-Meyers Squibb, Cardior, Cardurion, Corvia, Cytokinetics, Daiichi-Sankyo, Gilead, GlaxoSmithKline, Ironwood, Merck, Myokardia, Novartis, Roche, Takeda, Theracos, Quantum Genetics, Cardurion, AoBiome, Janssen, Cardiac Dimensions, Sanofi-Pasteur, Tenaya, Dinaqor, Tremeau, CellProThera, and Moderna outside the submitted work.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables and figures, please see the online version of this paper.
Appendix
References
- 1.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi S., Qin M., Shen B., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oxley T.J., Mocco J., Majidi S., et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bilaloglu S., Aphinyanaphongs Y., Jones S., Iturrate E., Hochman J., Berger J.S. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382:1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sama I.E., Ravera A., Santema B.T., et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41:1810–1817. doi: 10.1093/eurheartj/ehaa373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishiga M., Wang D.W., Han Y., Lewis D.B., Wu J.C. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeFilippis E.M., Reza N., Donald E., Givertz M.M., Lindenfeld J., Jessup M. Considerations for heart failure care during the COVID-19 pandemic. J Am Coll Cardiol HF. 2020;8:681–691. doi: 10.1016/j.jchf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fried J.A., Ramasubbu K., Bhatt R., et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141:1930–1936. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Premier Applied Sciences Premier Healthcare Database: Data That Informs And Performs. https://learn.premierinc.com/white-papers/premier-health care-database-whitepaper Available at:
- 12.Rector T.S., Wickstrom S.L., Shah M., et al. Specificity and sensitivity of claims-based algorithms for identifying members of Medicare+Choice health plans that have chronic medical conditions. Health Serv Res. 2004;39:1839–1857. doi: 10.1111/j.1475-6773.2004.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo T., Fan Y., Chen M., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhatt A.S., Ambrosy A.P., Dunning A., et al. The burden of non-cardiac comorbidities and association with clinical outcomes in an acute heart failure trial---insights from ASCEND-HF. Eur J Heart Fail. 2020;22:1022–1031. doi: 10.1002/ejhf.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mentz R.J., Kelly J.P., von Lueder T.G., et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2014;64:2281–2293. doi: 10.1016/j.jacc.2014.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee L.Y., Cazier J.-B., Angelis V., et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395:1919–1926. doi: 10.1016/S0140-6736(20)31173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chatrath N., Kaza N., Pabari P.A., et al. ESC Heart Fail; 2020 Oct 11. The effect of concomitant COVID-19 infection on outcomes in patients hospitalized with heart failure. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alvarez-Garcia J., Lee S., Gupta A., et al. Prognostic impact of prior heart failure in patients hospitalized with COVID-19. J Am Coll Cardiol. 2020;76:2334–2348. doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horby P., Lim W.S., et al. The RECOVERY Collaborative Group Dexamethasone in hospitalized patients with Covid-19---preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Panhwar M.S., Kalra A., Gupta T., et al. Effect of influenza on outcomes in patients with heart failure. J Am Coll Cardiol HF. 2019;7:112–117. doi: 10.1016/j.jchf.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 22.Apicella M., Campopiano M.C., Mantuano M., Mazoni L., Coppelli A., Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8:782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson M.R., Geleris J., Anderson D.R., et al. Body mass index and risk for intubation or death in sars-cov-2 infection: a retrospective cohort study. Ann Intern Med. 2020;173:782–790. doi: 10.7326/M20-3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cunningham J.W., Vaduganathan M., Claggett B.L., et al. Effects of sacubitril/valsartan on N-terminal pro-B-type natriuretic peptide in heart failure with preserved ejection fraction. J Am Coll Cardiol HF. 2020;8:372–381. doi: 10.1016/j.jchf.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Bhopal S.S., Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. 2020;396:532–533. doi: 10.1016/S0140-6736(20)31748-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takahashi T., Ellingson M.K., Wong P., et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020 Oct 26 doi: 10.1038/s41586-020-2700-3. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vardeny O., Solomon S.D. Influenza vaccination: a one-shot deal to reduce cardiovascular events. Eur Heart J. 2017;38:334–337. doi: 10.1093/eurheartj/ehw560. [DOI] [PubMed] [Google Scholar]
- 28.Braunwald E. Heart failure. J Am Coll Cardiol HF. 2013;1:1–20. doi: 10.1016/j.jchf.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Mann D.L. Innate immunity and the failing heart: the cytokine hypothesis revisited. Circ Res. 2015;116:1254–1268. doi: 10.1161/CIRCRESAHA.116.302317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Libby P., Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41:3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varga Z., Flammer A.J., Steiger P., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lowenstein C.J., Solomon S.D. Severe COVID-19 is a microvascular disease. Circulation. 2020;142:1609–1611. doi: 10.1161/CIRCULATIONAHA.120.050354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wosik J., Fudim M., Cameron B., et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abraham W.T., Fiuzat M., Psotka M.A., O’Connor C.M. Heart failure collaboratory statement on remote monitoring and social distancing in the landscape of COVID-19. J Am Coll Cardiol HF. 2020;8:692–694. doi: 10.1016/j.jchf.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abraham W.T., Psotka M.A., Fiuzat M., et al. Standardized definitions for evaluation of heart failure therapies: scientific expert panel from the heart failure collaboratory and academic research consortium. J Am Coll Cardiol HF. 2020 Nov 10 doi: 10.1002/ejhf.2018. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 36.Cooper L.B., Psotka M.A., Sinha S., et al. Specificity of administrative coding for older adults with acute heart failure hospitalizations. Am Heart J. 2020;223:1–2. doi: 10.1016/j.ahj.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.