Abstract
The relentless spread of coronavirus disease 2019 (COVID-19) and its penetration into the least developed, fragile, and conflict-affected countries (LDFCAC) is a certainty. Expansion of the pandemic will be expedited by factors such as an abundance of at-risk populations, inadequate COVID-19 mitigation efforts, sheer inability to comply with community mitigation strategies, and constrained national preparedness. This situation will reduce the benefits achieved through decades of disease control and health promotion measures, and the economic progress made during periods of global development. Without interventions, and as soon as international travel and trade resume, reservoirs of COVID-19 and other vaccine-preventable diseases in LDFCAC will continue ‘feeding’ developed countries with repeated infection seeds. Assuring LDFCAC equity in access to medical countermeasures, funds to mitigate the pandemic, and a paradigm change in the global development agenda, similar to the post-World War II Marshall Plan for Europe, are urgently needed. We argue for a paradigm change in strategy, including a new global pandemic financing mechanism for COVID-19 and other future pandemics. This approach should assist LDFCAC in gaining access to and membership of a global interdisciplinary pandemic taskforce to enable in-country plans to train, leverage, and maintain essential functioning and also to utilize and enhance surveillance and early detection capabilities. Such a task force will be able to build on and expand research into the management of pandemics, protect vulnerable populations through international laws/treaties, and reinforce and align the development agenda to prevent and mitigate future pandemics. Lifting LDFCAC from COVID-related failure will offer the global community the best economic dividends of the century.
Keywords: COVID-19, Conflict-countries
Introduction
The extension of the declaration of coronavirus disease 2019 (COVID-19) as a Public Health Emergency of International Concern by the World Health Organization (WHO) on April 30, 2020, underscores its continued pandemic spread beyond the initial epicenters. The transmission dynamics of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, including the high transmission rate (an estimated R0 of between 2 and 3.5), large numbers of asymptomatic transmitters, and uncertainty about post-infection immunity, mean that the battle against COVID-19 will not be won until every country in the world can mitigate and ultimately control it (Inglesby, 2020, Kirkcaldy et al., 2020, Miller et al., 2020, Salje et al., 2020, Editorial, 2020). Other recent diseases of global concern (for example, Ebola) evolved and remained largely contained in a few developing countries. This provided the opportunity for developed countries to shield themselves and support proactive action in the source countries. COVID-19 took a different path, beginning and spreading mostly in developed economies. Multiple factors including powerful governments, resilient and technologically sophisticated economies, well-established institutions, robust public health and health care systems, social security infrastructure, low household occupancy, and public solidarity all helped these early hotspots to embark on mitigation efforts. Now, COVID-19 has spread to most of the countries grouped as ‘least developed, fragile, or conflict-affected countries’ (LDFCAC), where SARS-CoV-2 could establish a strong footing.
The challenges: immunity confounders, at-risk populations, and limits of preparedness
There is insufficient evidence to support the assumption that some factors in LDFCAC might offer protection from SARS-CoV-2 transmission, including ambient hot temperature, humidity, and open-air ventilation typical for developing country dwellings (Miller et al., 2020). The reasons for a disproportionate COVID-19 burden in countries with comparable climates, socio-demographics, and timing of seeding or mitigation efforts are not fully understood. Comparison of the extensive spread in India, Iran, Brazil, Ecuador, Peru, and Singapore, with the limited spread in countries such as Iraq, Cambodia, Laos, and Myanmar offer no uniform discernable trends.
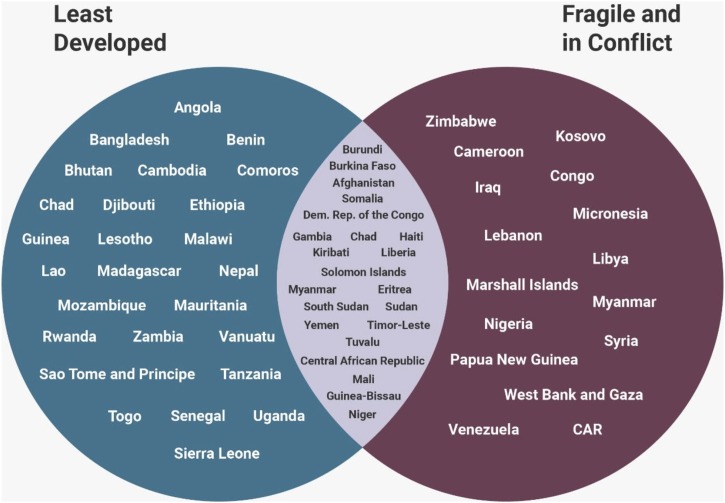
Many factors prevalent in LDFCAC limit the population’s ability to comply with pandemic mitigation measures that are feasible in developed countries (Ebrahim et al., 2020). These include frequent handwashing with clean water, physical distancing, and feeding families during prolonged periods of unemployment. Such measures cannot be enforced in LDFCAC. The World Bank classifies 47 countries and territories as ‘least developed’, of which 22 are considered fragile and conflict-affected (Figure 1). An additional 12 countries (not listed as least developed) are conflict-affected.
Figure 1.
Countries designated as least developed and/or fragile and in conflict.
Source:https://data.worldbank.org/region/fragile-and-conflict-affected-situations https://unctad.org/en/Pages/ALDC/Least%20Developed%20Countries/UN-list-of-Least-Developed-Countries.aspx.
Of the total 68.5 million forcefully displaced people globally, 40 million are internally displaced and 25 million are refugees. People in refugee camps face a heightened risk of COVID-19 due to more densely populated conditions than even the Diamond Princess (24 persons/1000 m2); for example Moria Camp, Greece (204/1000 m2) and Cox’s Bazar, Bangladesh (40/1000 m2) (McLauglin, 2020). Given the disruption to health systems during conflicts, surveillance systems may be non-existent in conflict-affected countries (McLauglin, 2020, Editorial, 2017). When most refugee-host governments themselves are facing economic challenges and are unable to achieve adequate support even for their own citizens, refugees are unlikely to be a priority in host government budgets for current or future pandemic countermeasures. The sizes of other ill-defined types of population movements and groupings, documented by the United Nations High Commissioner for Refugees as ‘situations’, are difficult to quantify (Box 1). Some displaced persons are stateless, a mix of economic migrants and undocumented refugees, and transient, and are not likely to be confined to a geographic location, adding to the challenge of interventions.
Box 1. Select population displacement situationsa.
Asylum and migration in West and Central Africa
A mix of refugees alongside people fleeing financial hardship. West and Central Africa is a place of complex mixed movements inside the region or from the region to other parts of the world, such as Europe, through the Central Mediterranean route.
Stateless in the Great Lakes region
Highlighting statelessness in the 12 Member States.
Stateless in West and Central Africa
At least 700 000 stateless people are in West and Central Africa.
Mediterranean situation
Persecution, conflict, and poverty forced over 1 million people to flee to Europe in 2015. Many came seeking safety for themselves and their families, risking their lives and facing a treacherous journey.
Western Balkans
Following the de facto closure of the so-called Western Balkans route in March 2016, strict border policies led to the fragmentation of the mixed flows of migrants and refugees through Southeast Europe, opening new smuggling pathways in parts of the Western Balkans that had not been affected so far. In addition to the shift in movement patterns, the intensity of migration has also increased substantially throughout the region. Still, most new arrivals view Southeast Europe as a transit region for their journey to final destinations in Northern and Western Europe.
ahttps://data2.unhcr.org/en/situations.
Alt-text: Box 1
Conflict and/or poor development in LDFCAC have led to large populations of impoverished people living in crowded megacity slums (>50% of the urban population in 51 LDFCAC), with limited or no access to clean water (>50% of the population in 38 countries) and with a significant proportion of the population already facing a food crisis (in 2019, 135 million people across LDFCAC; >10% of the population in 24 countries) (Table 1). Open defecation is highly prevalent in LDFCAC (2017: range 6–75%), raising concerns of fecal–oral transmission and challenges for surveillance innovations, such as sewage sampling to assess population burden (World Health Organization, 2020a). The average household occupancy is nearly double in LDFCAC (>5 persons per household) compared to developed country COVID-19 hotspots (<3 persons per household) (UN, 2017). How can social distancing be done in such crowded circumstances? Who can practice hand hygiene where there is no water? Furthermore, the perception of the impact of COVID-19 in LDFCAC populations is likely to be dwarfed by their experience with other existential threats, such as the daily need to find food for their families, violence, or even death from conflicts (as in Afghanistan recently) or diseases with a higher fatality (such as Ebola in the Democratic Republic of the Congo (DRC)).
Table 1.
COVID-19: select predisposing factors and mitigation challenges in the least developed, fragile, and conflict-affected countries and territories.
| Predisposing factors |
Preexisting diseases |
Mitigation challenges |
|||||
|---|---|---|---|---|---|---|---|
| Country/territory statusa, b( Conflict, development, fragile) |
Slum residents as % of urban populationb | Diabetes burden, age 20–79 yearsc (%) | Tuberculosis burdend (average number) | People living with HIVe (number) | Population without water on living premisesf (%) | Population facing food crisisg, % (number in millions) | Global Health Security Indexh |
| Conflicted-affected, fragile, and least developed | |||||||
| Afghanistan | 63 | 9.2 | 70 000 | 7200 | 60 | 37 (11.3) | 21.0 |
| Burkina Faso | 66 | 7.3 | 9500 | 96 000 | 85 | 6 (1.2) | 30.1 |
| Burundi | 58 | 5.1 | 12 000 | 82 000 | 93 | 2 (0.2) | 22.8 |
| Central African Republic | 93 | 6.0 | 25 000 | 110 000 | 92 | 41 (1.8)i | 27.3 |
| Chad | 88 | 6.0 | 21 000 | 120 000 | 90 | 4 (0.6) | 28.8 |
| Congo, DR | 75 | 6.0 | 270 000 | 450 000 | 91 | 26 (15.6) | 26.5 |
| Eritrea | 70 | 5.1 | 3100 | 18 000 | 81 | -- | 22.4 |
| Gambia | 35 | 1.9 | 4000 | 26 000 | 55 | 10 (0.2) | 34.2 |
| Guinea-Bissau | 82 | 2.4 | 6800 | 44 000 | 68 | 10 (0.1) | 20.0 |
| Haiti | 74 | 6.7 | 20 000 | 160 000 | 93 | 35 (3.7) | 31.5 |
| Kiribati | -- | 22.5 | 400 | -- | 44 | -- | 19.2 |
| Liberia | 66 | 2.4 | 15 000 | 39 000 | 97 | 1 (0.4) | 35.1 |
| Mali | 56 | 2.4 | 10 000 | 150 000 | 68 | 3 (0.6) | 29.0 |
| Myanmar | 41 | 3.9 | 181 000 | 240 000 | 47 | 1 (0.7) | 43.4 |
| Niger | 70 | 2.4 | 19 000 | 36 000 | 87 | 7 (1.4) | 32.2 |
| Solomon Islands | -- | 19.0 | 480 | -- | 49 | -- | 20.7 |
| Somalia | 74 | 5.1 | 39 000 | 11 000 | 81 | 17 (2.1) | 16.6 |
| South Sudan | 96 | 10.2 | 16 000 | 190 000 | 98 | 61 (7.0) | 21.7 |
| Sudan | 92 | 22.1 | 30 000 | 59 000 | 62 | 14 (5.9)i | 26.2 |
| Timor-Leste | -- | 6.7 | 6300 | -- | 50 | -- | 26.0 |
| Tuvalu | -- | 22.1 | 31 | -- | 3 | -- | 21.6 |
| Yemen | 61 | 5.4 | 14 000 | 11 000 | 51 | 53 (15.9) | 18.5 |
| Fragile and conflicted-affected | |||||||
| Cameroon | 38 | 6.0 | 47 000 | 540 000 | 71 | 8 (1.4)i | 34.4 |
| Congo, Republic of | 47 | 6 | 20 000 | 89 000 | 63 | -- | 23.6 |
| Iraq | 47 | 8.8 | 16 000 | -- | 29 | 18 (1.8) | 25.8 |
| Kosovo | -- | -- | -- | -- | -- | -- | -- |
| Lebanon | 53 | 11.2 | 750 | 2500 | 19 | 30 (0.4)i | 43.1 |
| Marshall Islands | -- | 30.5 | 250 | -- | 26 | -- | 18.2 |
| Micronesia | -- | 11.9 | -- | -- | 37 | -- | 32.8 |
| Nigeria | 50 | 3.1 | 429 000 | 1 900 000 | 80 | 5 (5.0)i | 37.8 |
| Papua New Guinea | -- | 17.9 | 37 000 | 46 000 | 81 | -- | 27.8 |
| Syria | 19 | 13.5 | 3300 | <1000 | 29 | 36 (6.6) | 19.9 |
| Venezuela | 32 | 7.0 | 13 000 | -- | 21 | 32 (9.3) | 23.0 |
| West Bank, Gaza | -- | 9.5 | 38 | -- | 20 | -- | -- |
| Zimbabwe | 25 | 1.8 | 30 000 | 1 300 000 | 78 | 38 (3.6) | 38.2 |
| Least developed | |||||||
| Angola | 56 | 9.0 | 109 000 | 330 000 | 77 | 62 (0.6)i | 25.2 |
| Bangladesh | 55 | 9.2 | 357 000 | 14 000 | 23 | 37 (1.3)i | 35.0 |
| Benin | 62 | 1.0 | 6500 | 73 000 | 73 | -- | 28.8 |
| Bhutan | 70 | 10.3 | 1100 | 1300 | 13 | -- | 40.3 |
| Cambodia | 55 | 6.4 | 49 000 | 73 000 | 42 | -- | 39.2 |
| Comoros | 70 | 12.3 | 290 | <200 | 35 | -- | 27.2 |
| Djibouti | 66 | 5.1 | 2500 | 8800 | 54 | -- | 23.2 |
| Ethiopia | 74 | 4.3 | 165 000 | 690 000 | 84 | 27 (8.0)i | 40.6 |
| Guinea | 43 | 2.4 | 22 000 | 120 000 | 65 | 3 (0.3) | 32.7 |
| Lao | 31 | 6.4 | 11 000 | 12 000 | 32 | -- | 43.1 |
| Lesotho | 51 | 4.5 | 13 000 | 340 000 | 75 | 30 (0.4)i | 30.2 |
| Madagascar | 77 | 4.5 | 61 000 | 39 000 | 76 | 28 (1.3)i | 40.1 |
| Malawi | 67 | 4.5 | 33 000 | 1 000 000 | 84 | 22 (3.3) | 28.0 |
| Mauritania | 80 | 7.1 | 4100 | 5600 | 37 | 50 (0.6) | 27.5 |
| Mozambique | 80 | 3.3 | 162 000 | 2 200 000 | 87 | 34 (1.7)i | 28.1 |
| Nepal | 54 | 7.2 | 42 000 | 30 000 | 39 | -- | 35.1 |
| Rwanda | 53 | 5.1 | 7300 | 220 000 | 87 | 1 (0.1) | 34.2 |
| Sao Tome | 87 | 2.1 | 260 | -- | 64 | -- | 17.7 |
| Senegal | 39 | 2.4 | 19 000 | 42 000 | 40 | 3 (0.4) | 37.9 |
| Sierra Leone | 76 | 2.4 | 23 000 | 70 000 | 89 | 4 (0.3) | 38.2 |
| Togo | 51 | 2.4 | 2800 | 110 000 | 85 | -- | 32.5 |
| Uganda | 54 | 2.5 | 86 000 | 1 4 00 000 | 94 | 4 (0.5) | 44.3 |
| Tanzania | 51 | 5.7 | 142 000 | 1 600 000 | 81 | -- | 36.4 |
| Vanuatu | -- | 11.9 | 130 | -- | 50 | -- | 26.1 |
| Zambia | 54 | 4.5 | 60 000 | 1 200 000 | 77 | 24 (2.3)i | 28.7 |
--, data unavailable. https://data.worldbank.org/region/fragile-and-conflict-affected-situations.
https://data.worldbank.org/indicator/en.pop.slum.ur.zs, since 2014.
https://www.who.int/tb/country/data/download/en/“TB_burden_countries_2020-04-20”, 2018 data.
https://www.wfp.org/publications/2020-global-report-food-crises 2018–2019 data, Criteria for food crisis estimation: households either have food consumption gaps that are reflected by high or above usual acute malnutrition, or are marginally able to meet minimum food needs but only by depleting essential livelihood assets or through crisis-coping strategies.
https://www.ghsindex.org/ Global Health Security Index. The perfect score is 100.
Based on select populations or regions of the country or refugee populations.
Regarding COVID-19 severity and mortality patterns in LDFCAC, it remains unclear whether innate immunity achieved through exposure to other vaccines (such as BCG and polio) may be beneficial in overriding the role of comorbidities prevalent in LDFCAC in the spread of COVID-19 in these areas (Hamiel et al., 2020). The comorbidity burden is high in LDFCAC: 13 countries have a diabetes prevalence >10% among persons aged 20–79 years, 35 countries have >10 000 tuberculosis patients, and 40 countries have >10 000 persons living with HIV/AIDS (Table 1). While the information on the effects of SARS-CoV-2 in children is still emerging, the finding that SARS-CoV-2 successfully infects human gut enterocytes is of concern, because of the high burden of intestinal polyparasitism in all LDFCAC, which poses a serious threat to millions of children and women of reproductive age (Viner and Whittaker, 2020, Bradbury et al., 2020). Hookworm infections exacerbate anemia, which further increases maternal mortality from peripartum blood loss. Each country faces unique challenges from being overburdened with one or more of the existing preventable or treatable infections, such as measles, tuberculosis, polio, cholera, yellow fever, malaria, meningitis, and HIV/AIDS. It is unknown whether the high prevalence of the aforementioned infections and other potential confounders, including genetic mutations (glucose-6-phosphate dehydrogenase (G6PD) deficiency, sickle cell trait) and the prevalence of herpes simplex virus type 2 (HSV-2) (women, 44%; men 25%, in select LDFCAC (James et al., 2020)), may directly or inversely impact COVID-19 progression or severity.
What we do know is that two critical factors that underscore the exponential spread of COVID-19 – density and/or movement of the population – are highly relevant to LDFCAC. The low airline volume and frequency of flights in these countries may have helped to slow down the initial spread of COVID-19 in LDFCAC. However, once community seeding and spread begin, the informal rural–urban transportation modes prevalent in LDFCAC, along with migration, porous borders, and displacement of people, will be sufficient to sustain continued community transmission. Even if the predominantly younger age population in LDFCAC can be a protective factor in reducing COVID-19 mortality, the concentration of people living with HIV/AIDS (about two-thirds of the global total, or 25 million), mostly in the 15–49 years age groups, may negate such protection. Only about 50% of the people living with HIV/AIDS in LDFCAC benefit from adequate treatment, as reflected by their HIV viral load suppression rates (Marsh et al., 2019). The destruction of road and transport networks in conflict-affected countries (for example, in DRC only 5% of 58 000 km of roads are usable) may help to impede COVID-19 expansion deeper to rural areas. However, the reach of COVID-19 to Amazon Indian tribes suggests that minimal population contact is sufficient for the seeding of the highly contagious SARS-CoV-2.
Health systems in LDFCAC are chronically underfunded and are often sustained largely by international development assistance (World Health Organization, 2020b). Together with low domestic spending on health (average in 2016, US$23) and suboptimal infrastructure and economic development, the majority of LDFCAC score the lowest in pandemic preparedness: 40 countries score below 33 out of 100 (the top score) in the Global Health Security Index (Table 1). Hospitals in Afghanistan and other conflict-affected countries are still treating war casualties, along with COVID-19 cases, and access to personal protective equipment is limited. In 2016, in Afghanistan, international financing contributed to 50% of the US$57 per-capita spending on health (compared to US$5180 in high-income countries), and the government contribution remained at 5% (World Health Organization, 2020b). Survival crisis mitigation efforts in some countries are likely to facilitate community transmission of COVID-19. For example, in Afghanistan, physical distancing and face-covering were uncommon among crowds at the free bread distribution centers.
Consequences of the expansion of COVID-19 in LDFCAC
The impact of mitigation in LDFCAC on general health care delivery, the redirection of health care resources for the COVID-19 response, and task-shifting will undoubtedly impede ongoing public health efforts and reverse gains in health indices made in recent decades (Roberton et al., 2020). The COVID-19 response has already absorbed response capacities for other diseases, such as for the Ebola response in the DRC. Testing and treatment of HIV/AIDS and tuberculosis have been interrupted in many high HIV/AIDS and tuberculosis burden countries. An estimated 117 million children in 37 countries may miss out on receiving the measles vaccine as a result of delays in campaign implementation. During the 2014–2015 Ebola outbreak, deaths caused by measles, malaria, HIV/AIDS, and tuberculosis attributable to health system failures exceeded deaths from Ebola. The WHO issued revised operational guidelines in April 2020 that halted all mass drug administrations for deworming that benefited close to 600 million in 2017.
While developed countries can boost their economies through intra- and post-pandemic economic stimulus packages, already indebted LDFCAC have no such economic leverage. Stalling existing or continued multi- and bilateral development assistance due to the inward focus of the usual donor countries or investments in COVID-19 research, will exacerbate the financial shock that is likely to linger in COVID-19-affected LDFCAC. The compounded impact will further stress the already dysfunctional health systems due to reduced allocations to health and social services with the shrunken gross domestic product (GDP). Lockdowns without adequate online options and unemployment could further deteriorate the food crisis, encourage economic migration, and thereby reverse previous socio-economic improvements, including in education and gender equity. Population displacements may propagate other prevalent or reemerging vaccine-preventable diseases globally.
Even when a vaccine is developed, vaccine-induced immunity against SARS-CoV-2 is not a given, as the benefits could be partial, population-dependent, or transient (Editorial, 2020). The finding that 95% of the population in France and Spain remain susceptible to the virus does not offer much hope for relying on herd immunity (Kirkcaldy et al., 2020, Salje et al., 2020, Editorial, 2020). As long as human mobility cannot be adequately curtailed, circulating SARS-CoV-2 in LDFCAC will become a permanent threat, and further outbreaks will be inevitable in all countries.
Is there a way forward?
A successful medical countermeasure for COVID-19 will be in limited supply, and assuring equitable access and distribution to LDFCAC is important (Bollyky et al., 2020, Ledford, 2020). Experience from the dissemination of interventions such as those for tuberculosis, polio, and HIV/AIDS underscores the inverse equity hypothesis that public health interventions usually benefit the well-resourced earlier than the resource-poor, even during pandemics (Victora et al., 2018, Wade, 2020). Treatment options have helped developed countries to transform HIV/AIDS into a controlled and manageable disease, whereas LDFCAC are still struggling to achieve similar outcomes despite unprecedented funding. The ongoing European Commission-backed Access to COVID-19 Tools (ACT) Accelerator vaccine initiative is commendable and could be usefully informed by equity considerations outlined in the Pandemic Influenza Preparedness Framework (WHO, 2020, Polansky et al., 2016). However, for full exploitation of the benefits of the ACT initiative, a framework and funding for complementary economic and social redevelopment to avert the unintended consequences of COVID-19 is crucial (UN, 2020, Marmot, 2005).
There is an urgent need in LDFCAC for funds to expand testing and contact-tracing, and when feasible, for the use of proximity-tracing technology and apps that allow people to self-report symptoms and confirmed infections. This is the only pathway to ascertain the burden and address the many unanswered questions on the natural history of SARS-CoV-2. It is critical to determine whether the many immunological or disease situations prevalent in LDFCAC have a role in COVID-19 progression, so that the country-specific response can be moderated accordingly.
Although the immediate focus of donor nations has been a national pandemic response, this is a moment for ethical reckoning and calls for new resolve (Kavanagh et al., 2020, UN, 2020, Thorp, 2020). A different type of pandemic mitigation battle plan is required in LDFCAC. Given the health, economic, and development impact of COVID-19, similar to post-World War II events, a globally agreed and funded framework, platform, and mechanisms are required to avert the disproportional impact of COVID-19 on LDFCAC. We propose the following seven-point framework for action (this is detailed in Appendix 1).
-
1
A new global pandemic financing mechanism for COVID-19 and beyond needs to be established. Similar to the Marshall Plan of 1948, aimed at postwar Europe, economic assistance must be made available to restore the economic infrastructure, public health systems, and social development required to enable LDFCAC to overcome the COVID-19 impact. The Marshall Plan (officially the European Recovery Program, ERP) was an American initiative passed in 1948 for foreign aid to Western Europe. The United States transferred over $12 billion (equivalent to $130 billion in 2019) in economic recovery programs to Western European economies after the end of World War II. Such a structure should also include funding for preparedness for future pandemics. The emergence of Ebola and monkeypox virus reminds us that climate change, conflicts, and development will continue to increase human proximity to vectors of unknown viruses. Economic recovery and human development is beyond the scope of the WHO.
-
2
A global all-hands pandemic taskforce. Preparedness and the deliverables for a pandemic response are beyond the remit of public health systems alone or the WHO and must be interdisciplinary, crosscutting, and include all elements of governance and social systems at a global level. An entity that can provide broader guidelines to all countries and specific technical assistance to countries in greater need could help unify the response.
-
3
A forward-looking country plans to train, leverage, and maintain essential capabilities. Plans, procedures, and cataloged inventory are required to fully repurpose existing capacities (disease control programs, public–private partnerships, religious institutions) and infrastructure (buildings, supply chains, and defense personnel) to respond to COVID-19 and future pandemics. LDFCAC must have access to tests, treatments, and vaccines as they become available in developed countries.
-
4
Utilize, enhance, and institutionalize surveillance and early detection capabilities. The 11 core prevention, detection, and response capacities developed by the Global Health Security Initiative, complemented by other disease-specific programs, including the influenza sentinel surveillance systems (Polansky et al., 2016), could be enhanced to usefully supplement COVID-19 basic surveillance and monitoring needs. They should be integral to the country’s plan for a pandemic response.
-
5
Establish, expand, and sustain research and development readiness. Country-level epidemiology and statistical capacity are required to analyze and model trends from local tests and contact-tracing data and conduct environmental and sero-epidemiological studies. Bio-repositories and advanced computational capacities can be shared by a regional group of countries.
-
6
Inclusion of pandemics in international humanitarian law. The Geneva Conventions (The International Committee of the Red Cross, 2020) should be amended to allow for truces during pandemics so that the pandemic response can be extended to conflict-affected areas and populations (Editorial, 2017).
-
7
A renewed development agenda for LDFCAC. A revival of the WHO Alma-Ata Declaration of 1978 calling for a comprehensive development plan addressing socio-economic issues.
Existing organizations may be insufficient
Smart management principles would advocate for inclusion. As such, there are significant roles that all existing organizations could play. However, none of these organizations were created to respond to a crisis such as that posed by COVID-19. Overreliance on the WHO may not help. The WHO is grossly underfunded to achieve even its fundamental mandate, which is to improve health and prevent disease (The economist, 2020). Adding economic recovery to its mandate would not be welcome at this time. Flagship public initiatives, for example the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFTAM), Gavi, the Vaccine Alliance (GAVI), and the President’s Emergency Plan For AIDS Relief (PEPFAR), have collaborated well with the WHO and are complementary entities. Similarly, the United Nations (UN) created a peace and security mandate to “save succeeding generations from the scourge of war”. The UN General Assembly’s increasing involvement in AIDS and other diseases is paying dividends and this role should be continued. The task ahead of us may require renewed organizational dynamics to save us from the scourge of a pandemic; however a prototype for this does not currently exist.
Conclusions
The collective stewardship of global leaders, the UN, G7, G20, and the Davos platforms have helped garner momentum for major global health and development initiatives. The United States Pandemic Influenza Initiative, steered by President George W. Bush in 2005, helped formulate the non-pharmaceutical pandemic interventions that we are using in the COVID-19 response today (Charatan, 2005). In 2001, the late Kofi Annan, the Secretary-General of the UN at that time, donated his Philadelphia Liberty Award of US$100 000 to seed the Global Fund, the largest financing mechanism ever for health (UN News, 2020). COVID-19 presents another opportunity to reaffirm such solidarity. True success in overcoming the global COVID-19 pandemic will only be achieved by developing global stewardship and mechanisms to mount an effective response in LDFCAC. COVID-19 has massively disrupted lives; there have been close to 40 million cases of disease and one million deaths, and an economic fallout due to poor planning and a haphazard global response. We must protect and support LFDCAC. COVID-19 anywhere is COVID-19 everywhere.
Data sharing statement
Except for the Appendix, there are no additional data to share.
Funding
None.
Patient and public involvement
None.
Patient consent for participation
None.
Conflict of interest
None.
Author contributions
All authors contributed equally to drafting, reviewing, and finalizing the manuscript.
Appendix.
COVID-19 in fragile and least developed countries—time for a paradigm change in global health
Seven proposed interventions to empower LDFCAC to avert a COVID-19-related massive reversal of the health and development trajectory:
1. New global pandemic financing mechanism for COVID-19 and beyond. COVID-19 will not be the last pandemic, and our experience of this disease should be used as a prelude to developing future resilience. Our global community is significantly more inter-dependent now than after World War II in 1945, when the UN and the international financing institutions were created. The progression of COVID-19 across geographical regions has been temporally and geographically staggered, allowing us to use lessons learned. A consolidated pandemic funding mechanism for health, social, and economic development that empowers countries through local expertise, government stewardship, and international technical assistance in an inter-dependent partnership, would ensure the maximum benefits. Paradigm changes in development stewardship could help minimize the skepticism towards development assistance. Despite DRC’s reputation for failure, the government, with international assistance, led a successful national response to its tenth Ebola outbreak. That country’s recent anti-corruption drives are making progress. A combination of mechanisms used by the GFTAM and PEPFAR could serve as models for managing a new global fund for pandemics. Concerted stewardship by the G7, G20, and public–private meeting platforms such as the Davos Summit could help. Such a funding mechanism could be informed by existing technical and policy leadership from development and health stakeholders, including the UN and the international financial intuitions. A global all-hands pandemic taskforce could advise the governance of such a fund.
2. A global all-hands pandemic taskforce. Pandemic mitigation through non-pharmaceutical interventions is less about public health and more about public policy. It covers resilience in essential service delivery, economic stability, food security, education sector, religious services, and population behavior beyond the purview of global health experts. Therefore, a global pandemic response requires a balanced representation of all relevant entities that collectively contribute to the functioning of society. Global public health entities, including the WHO, can and should continue to play a critical role in analyzing and synthesizing biomedical epidemiological and public health developments. The support the WHO is providing through the COVID-19 Solidarity Fund is commendable, yet such funds do not address the survival needs of the people. Informed by public health entities, an all-hands taskforce, with sufficient representation of all sectors, would be uniquely positioned to propose and monitor a coordinated and balanced global pandemic response in member countries that would not only facilitate mitigation measures, but also measures to avert the adverse effects of mitigation.
3. A forward-looking country’s plans to train, leverage, and maintain essential capabilities. Along with sufficient funding from the global COVID-19 Solidarity Fund described above, the global all-hands pandemic task force could help countries to achieve essential capabilities. Irrespective of their development status, all countries have capacities that can be leveraged, repurposed, or reallocated, including university students, military infrastructure, religious and community organizations, and large venues such as schools and university buildings. LDFCAC are not new to infectious disease threats. They have varying levels of surveillance, laboratory, and field epidemiology capacities that share useful features for a pandemic response. What many LDFCAC lack is a national framework for the rapid leveraging of existing resources. For example, countries with experience of HIV/AIDS, tuberculosis, and Ebola have developed expertise in contact-tracing, laboratory testing, and national surveys and could rapidly train respective teams for COVID-19 deployment. Polio-affected countries have environmental (sewage) sampling experience. Door-to-door vaccination assessment and promotion are used in many vaccination programs and these could easily be deployed to conduct screening and testing. All countries have universities where volunteers can be recruited and buildings that can be designated as ad-hoc treatment or isolation facilities. Religious and philanthropic entities could complement food and essential commodity distribution if the military can provide logistics and peacekeeping. Students at medical, pharmacy, nursing, and laboratory schools could help triage patients or provide supervised treatment.
4. Utilize and enhance surveillance and early detection capabilities. The Global Health Security Initiative has developed 11 country-based competencies for outbreak prevention, detection, and response that could complement the International Health Regulations (IHR). The IHR were used to develop the Joint External Evaluation (JEE) tool that together with the National Action Plan for Health Security (NAPHS), both developed by the WHO, is sufficiently broad and flexible to accommodate variations including COVID-19. There is an urgent need to achieve and maintain these competencies and this will require external funding. Regionalization of some competencies, such as laboratories and training infrastructure, could help minimize costs.
5. Establish, expand, and sustain research and development readiness. It is neither cost-effective nor sustainable for each country to establish biomedical research and development (R&D) infrastructure, particularly those with small populations. However, a set of R&D institutions (e.g., biobanks and specimen banks, advanced laboratories, advanced mathematical and statistical centers for competence) that serve multiple countries could be strategically located in different countries in regional collaboration. Basic epidemiology and statistical expertise need to be maintained in all countries to support epidemiological and clinical research. They could help analyze and interpret contact-tracing and testing data, develop warning systems using environmental samples, and conduct sero-epidemiology studies to fully resolve population susceptibility profiles for SARS-CoV-2 infection, as well as refine age- and comorbidity-specific estimates of susceptibility to infection and infectiousness and severity among symptomatic persons.
6. Inclusion of pandemics in international humanitarian law. Given the role of conflicts in pandemics, the first and fourth Geneva Conventions (the rules of war, or international humanitarian law) should be updated to mandate a ceasefire during pandemic periods to enable mitigation efforts both for armed persons and conflict-affected civilians. The rules of war are a set of international rules that set out what can and cannot be done during an armed conflict and have been ratified by all 196 states.
7. A renewed development agenda for LDFCAC. Access to health care during COVID-19 has renewed the debate on the principles underlying the 1978 WHO Alma-Ata Declaration that was later paraphrased in the 1990s as the social determinants of health. It has become clear that health improvement with foundational socio-economic development is required to reap the full and sustainable benefits of modern health interventions. The gains from a patchwork of sporadic disease-specific initiatives may not supersede the sequelae of a new threat such as COVID-19. The economic prosperity brought about by education, freedom, and equity will equip countries to withstand such renewed shocks. COVID-19 requires the global community to redefine its commitment to achieving equilibrium in health across all countries.
References
- Bollyky T.J., Gostin L.O., Hamburg M.A. The equitable distribution of COVID-19 therapeutics and vaccines. JAMA. 2020;323(24):2462–2463. doi: 10.1001/jama.2020.6641. Published online May 07, 2020. [DOI] [PubMed] [Google Scholar]
- Bradbury R.S., Piedrafita D., Greenhill A., Mahanty S. Will helminth co-infection modulate COVID-19 severity in endemic regions? Nat Rev Immunol. 2020;20(June):342. doi: 10.1038/s41577-020-0330-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charatan F. Bush announces US plan for flu pandemic. BMJ: Br Med J. 2005;331(November 7525):1103. doi: 10.1136/bmj.331.7525.1103-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim S.H., Ahmed Q.A., Gozzer E., Schlagenhauf P., Memish Z.A. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020;368:m1066. doi: 10.1136/bmj.m1066. [DOI] [PubMed] [Google Scholar]
- Editorial Health care in conflict: war still has rules. Lancet. 2017;390:2516–2566. [Google Scholar]
- Editorial Sustained suppression. Nat Biomed Eng. 2020 doi: 10.1038/s41551-020-0567-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamiel U., Kozer E., Youngster I. SARS-CoV-2 rates in BCG-vaccinated and unvaccinated young adults. JAMA. 2020;323(22):2340–2341. doi: 10.1001/jama.2020.8189. Published online May 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglesby T.V. Public health measures and the reproduction number of SARS-CoV-2. JAMA. 2020;323(21):2186–2187. doi: 10.1001/jama.2020.7878. Published online May 01. [DOI] [PubMed] [Google Scholar]
- James C., Harfouche M., Welton N.J., Turner K.M., Abu-Raddad L.J., Gottlieb S.L. Herpes simplex virus: global infection prevalence and incidence estimates, 2016. Bull World Health Organ. 2020;98(May):315–329. doi: 10.2471/BLT.19.237149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh M.M., Erondu N.A., Tomori O., Dzau V.J., Okiro E.A., Maleche A. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. The Lancet. 2020;(May (10238)):1735–1738. doi: 10.1016/S0140-6736(20)31093-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkcaldy R.D., King B.A., Brooks J.T. COVID-19 and postinfection immunity: limited evidence, many remaining questions. JAMA. 2020;323(22):2245–2246. doi: 10.1001/jama.2020.7869. Published online May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford H. Dozens of coronavirus drugs are in development — what happens next? Nature. 2020;581(May):247–248. doi: 10.1038/d41586-020-01367-9. [DOI] [PubMed] [Google Scholar]
- Marmot M. Social determinants of health inequalities. The Lancet. 2005;365(March 9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- Marsh K., Eaton J., Mahy M., Sabin K., Autenrieth C., Wanyeki I. Global, regional and country-level 90–90–90 estimates for 2018. AIDS. 2019;33(December):S213–S226. doi: 10.1097/QAD.0000000000002355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLauglin The Unseen Pandemic. Refugee camps such as those in Bangladesh are a tinderbox for the spread of the coronavirus. The Atlantic. 2020 April 2 https://www.theatlantic.com/international/archive/2020/04/refugees-coronavirus-covid19-bangladesh/609259/. [Accessed 2 April 2020] [Google Scholar]
- Miller M.J., Loaiza J.R., Takyar A., Gilman R.H. COVID-19 in Latin America: Novel transmission dynamics for a global pandemic? PLoS Negl Trop Dis. 2020;14(5):e0008265. doi: 10.1371/journal.pntd.0008265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polansky L.S., Outin-Blenman S., Moen A.C. Improved global capacity for influenza surveillance. Emerging Infect Dis. 2016;22(June 6):993. doi: 10.3201/eid2206.151521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberton T., Carter E.D., Chou V.B., Stegmuller A., Jackson B.D., Tam Y. Early estimates of the indirect effects of the coronavirus pandemic on maternal and child mortality in Low-and Middle-Income countries. Lancet Global Health. 2020 doi: 10.1016/S2214-109X(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salje H., Kiem C.T., Lefrancq N., Courtejoie N., Bosetti P., Paireau J. Estimating the burden of SARS-CoV-2 in France. Science. 2020;369:208–211. doi: 10.1126/science.abc3517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The economist . 2020. COVID -19 and beyond. The world needs a better World Health Organization. September 12th. Geenva. https://www.economist.com/international/2020/09/12/the-world-needs-a-better-world-health-organisation. [Accessed 10 October 2020] [Google Scholar]
- The International Committee of the Red Cross . 2020. The Geneva Conventions of 1949 and their Additional Protocols.https://www.icrc.org/en/document/geneva-conventions-1949-additional-protocols [Google Scholar]
- Thorp H.H. Editorial. Time to pull together. Science. 2020;(March) doi: 10.1126/science.abb7518. [DOI] [PubMed] [Google Scholar]
- UN . 2017. Household Size and Composition Around the World.https://www.un.org/en/development/desa/population/publications/pdf/ageing/household_size_and_composition_around_the_world_2017_data_booklet.pdf [Google Scholar]
- UN . 2020. Shared responsibility, global solidarity: responding to socio-economic impacts of COVID-19.https://unsdg.un.org/sites/default/files/2020-03/SG-Report-Socio-Economic-Impact-of-Covid19.pdfDate [Google Scholar]
- UN News . 2020. Annan receives Philadelphia Liberty Medal, donates grant to AIDS fund.https://news.U.N.org/en/story/2001/07/3692-annan-receives-philadelphia-liberty-medal-donates-grant-aids-fund [Google Scholar]
- Victora C.G., Joseph G., Silva I.C.M., Maia F.S., Vaughan J.P., Barros F.C. The Inverse equity hypothesis: analyses of institutional deliveries in 286 national surveys. Am J Public Health. 2018;108(April 4):464–471. doi: 10.2105/AJPH.2017.304277. Epub 2018 Feb 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R.M., Whittaker E. Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet. 2020;395(10239):P1741–P1743. doi: 10.1016/S0140-6736(20)31129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade L. From Black Death to fatal flu, past pandemics show why people on the margins suffer most. Science. 2020 https://www.sciencemag.org/news/2020/05/black-death-fatal-flu-past-pandemics-show-why-people-margins-suffer-most May 14. [Google Scholar]
- WHO . 2020. Access to COVID-19 Tools (act) Accelerator.https://www.who.int/who-documents-detail/access-to-covid-19-tools-(act)-accelerator [Google Scholar]
- World Health Organization . 2020. Global health observatory data repository; Open defecation Data by country.https://apps.who.int/gho/data/node.main.WSHOPENDEFECATION [Google Scholar]
- World Health Organization . 2020. Global health expenditure database.https://apps.who.int/nha/database [Google Scholar]