Abstract
Mortality from COVID-19 has obscured a subtler crisis – the swelling ranks of COVID-19 survivors. After critical illness, patients often suffer post-intensive care syndrome (PICS), which encompasses physical, cognitive, and/or mental health impairments that are often long-lasting barriers to resuming a meaningful life. Some deficits after COVID-19 critical illness will require otolaryngologic expertise for years after hospital discharge. There are roles for all subspecialties in preventing, diagnosing, or treating sequelae of COVID-19. Otolaryngologist leadership in multidisciplinary efforts ensures coordinated care. Timely tracheostomy, when indicated, may shorten the course of intensive care unit stay and thereby potentially reduce the impairments associated with PICS. Otolaryngologists can provide expertise in olfactory disorders; thrombotic sequelae of hearing loss and vertigo; and laryngotracheal injuries that impair speech, voice, swallowing, communication, and breathing. In the aftermath of severe COVID-19, otolaryngologists are poised to lead efforts in early identification and intervention for impairments affecting patients' quality of life.
Keywords: COVID-19; Intensive care unit; Ventilator; Tracheostomy; Tracheotomy; Pandemic; SARS-CoV-2, coronavirus; Quality of life; Laryngotracheal injury, Subglottic stenosis, Tracheal stenosis; Speech; Swallowing; Iatrogenic injury; Tracheocutaneous fistula; Patient safety and quality improvement; Critical care; Taste; Smell; Dizziness; Hearing loss; Olfactory; Gustatory; Head and neck cancer
1. Introduction
December 7, 1941, “A day that will live in infamy” marked the attack on Pearl Harbor – a day of massive, catastrophic loss of life. December 2020 witnessed similar loss of life with each day of the coronavirus disease-2019 (COVID-19) pandemic. This mortality represents the tip of the larger iceberg of COVID-19 survivorship. Even with the promise of widespread vaccination, the aftermath of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection can be crippling, particularly for those who have a severe course of illness requiring mechanical ventilation in an intensive care unit (ICU) [1]. Otolaryngologists play important roles in COVID-19 survivor care and have engaged with the pandemic response from investigating early symptoms of olfactory and gustatory loss to decisions around tracheostomy, airway interventions, and rehabilitation [2].
2. Post-intensive care syndrome (PICS)
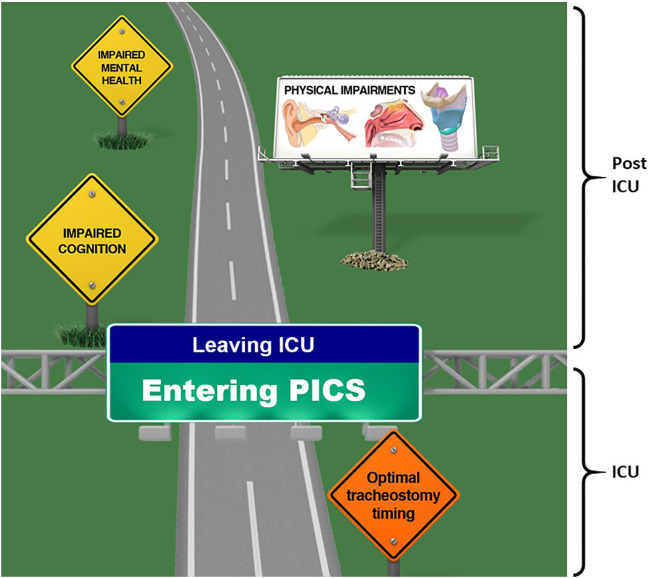
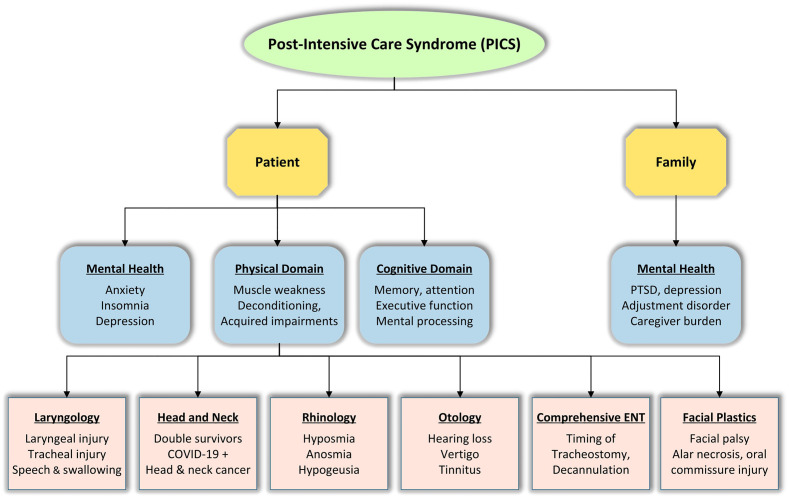
To provide optimal care for patients, Otolaryngologists need to understand COVID-19 survivorship after critical illness. PICS encompasses a spectrum of physical, cognitive, and/or mental health impairments experienced by patients after ICU stay that can be long-lasting barriers to resuming a meaningful life [3]. For some post-ICU impairments, a longer duration of critical illness is associated with greater impairment [4]. Timing of tracheostomy is therefore a key consideration [5]. Over 80% of patients requiring mechanical ventilation manifest residual impairments (Fig. 1 ), many directly relevant to otolaryngology and potentially lingering for years after hospital discharge (Fig. 2 ) [6].
Fig. 1.
Key reminders for Otolaryngologists-Head and Neck Surgeons along the road to intensive care recovery. Offering tracheostomy to avoid prolonged intubation may mitigate the severity of PICS. After intensive care unit stay, patients will often encounter complex cognitive, mental health, and physical impairments, many related to otolaryngology expertise.
Abbreviations: PICS, post-intensive care syndrome; ICU, intensive care unit.
Image credit: Larynx/trachea image. This work, “Anatomy of the Larynx,” is a derivative of “BodyParts3D by BodyParts3D, © The Database Center for Life Science used under CC Attribution-Share Alike 2.1 Japan. “Anatomy of the Larynx” is licensed under CC BY-SA 4.0.
Fig. 2.
Role of Otolaryngologist-Head and Neck Surgeons in COVID-19 survivorship.
Abbreviations: PTSD, post-traumatic stress disorder.
Patients who survive ICU stays often face profound debilitation–with muscle weakness, memory loss, anxiety, depression, and post-traumatic stress disorder (PTSD). Specifically, prolonged ventilation promotes patient frailty, which can require a very long period of rehabilitation. Laryngotracheal injury impairs voice, swallowing, and breathing. A year after ICU discharge, 34% of patients over age 50 have cognitive impairments similar to a moderate traumatic brain injury; a quarter demonstrate cognitive decline similar to mild Alzheimer's disease [7]. The joy that families experience when their loved ones survive is often replaced by grim realization that the road to recovery is long and arduous. Otolaryngologists are capable of providing timely diagnosis, education to patients and families, and specialized interventions (Table 1, Table 2 ).
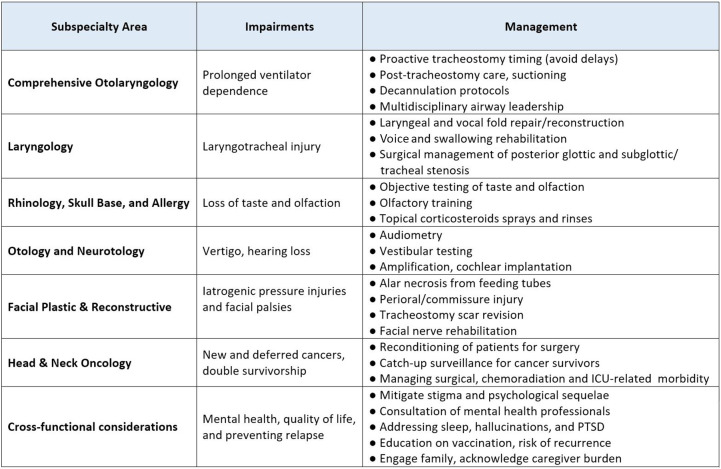
Table 1.
Delineation of otolaryngology domains related to COVID-19 survivorship.
Abbreviations: ICU, intensive care unit; PTSD, post-traumatic stress disorder.
Table 2.
Otolaryngology symptoms related to COVID-19.
| (Author, year) | Method | Sample Size | Tracheal injury | Pneumomediastinum | Laryngeal injury | Dysphonia | Dysphagia | SSNHL | Vertigo | Intralarbyrinthine hemorrhage | Tinnitus | Headache/ encephalopathy |
Gustatory disorder | Olfactory disorder | Psychosomatic |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Abou-Arab, 2020) [27] | CS | 2 | ++ | ++ | − | − | − | − | − | − | − | − | − | − | − |
| (Bassi, 2020) [28] | CS | 1 | + | + | − | − | − | − | − | − | − | − | − | − | − |
| (Bertone, 2020) [29] | CS | 1 | − | − | + | + | + | − | − | − | − | − | − | − | − |
| (Buselli, 2020) [30] | CS | 1 | − | − | − | + | − | − | − | − | − | − | − | − | + |
| (Chern, 2021) [14] | CS | 1 | − | − | − | − | − | + | + | + | − | − | − | − | − |
| (Chirakkal, 2020) [31] | CS | 1 | − | − | − | − | − | − | − | − | + | − | − | − | − |
| (Filatov, 2020) [32] | CS | 1 | − | − | − | − | − | − | − | − | − | + | − | − | − |
| (Koumpa, 2020) [33] | CS | 1 | − | − | − | − | − | + | − | − | + | − | − | − | − |
| (Lamounier, 2020) [34] | CS | 1 | − | − | − | − | − | + | − | − | + | − | − | − | − |
| (Lang, 2020) [35] | CS | 1 | − | − | − | − | − | + | − | − | + | − | − | − | − |
| (Wali, 2020) [36] | CX | 5 | 1 | 5 | − | − | − | − | − | − | − | − | − | − | − |
| (Brugliera., 2020) [37] | COH | 50 | − | − | − | − | 90% | − | − | − | − | − | − | − | − |
| (D'Ascanio, 2020) [15] | COH | 44 | − | − | − | − | − | − | − | − | − | 54% | 59% | − | − |
| (Fiacchini, 2020) [8] | COH | 30 | 33% | 33% | − | − | − | − | − | − | − | − | − | − | − |
| (Hajikhani, 2020) [38] | SR | 3739 | − | − | − | − | − | − | − | − | − | − | 49% | 61% | − |
| (Kaye, 2020) [39] | SY | 237 | − | − | − | − | − | − | − | − | − | − | − | 73% | − |
| (Lechien, 2020) [40] | EPI, MI | 702 | − | − | − | 27% | − | − | − | − | − | − | − | − | − |
| (Lechien, 2020) [41] | EPI, MI | 417 | − | − | − | − | − | − | − | − | − | − | 88% | 86% | − |
| (Ozcelik, 2020) [42] | OBS | 116 | − | − | − | − | 21% | 5% | 6% | − | 11% | − | 41% | 38% | − |
CS=case study, COH=cohort, SR = systematic review, SY=survey, EPI = epidemiologic, MI = multi-institutional, CX = case series, OBS=observational study, SSNHL = sudden sensorineural hearing loss. (Representative studies)
3. Airway injury
There is growing awareness of device-related pressure injuries and trauma that may arise in COVID-19 patients, resulting in lasting functional impairment. Laryngotracheal injuries include posterior glottic stenosis with resultant vocal cord immobility, vocal fold edema, or posterior glottic ulcerations. More distally, cuff injury may cause subglottic and/or tracheal stenosis. In one study of COVID-19 patients intubated more than 14 days, 14 of 30 (47%) patients had transmural tracheal erosion resulting in pneumomediastinum, pneumothorax, and tracheoesophageal fistulas [8]. Laryngeal injury is linked to duration of intubation [9], size of endotracheal tube, and difficulties with endotracheal tube insertion. Intubation can be more challenging due to reduced visualization or personal protective equipment that impedes communication. Otolaryngologist input into optimal tracheostomy timing and multidisciplinary care may decrease laryngeal injuries and expedite both early diagnosis and intervention [5].
4. Voice and swallowing
Dysphonia and dysphagia are common impairments associated with weakness and deconditioning of aerodigestive muscles; acute laryngotracheal insults might exacerbate such impairments [2]. Dysphagia is much more common than dysphonia in COVID-19 patients; it may be associated with otolaryngologic symptoms—dyspnea, ear pain, facial pain, throat pain, or nasal obstruction. Aspiration pneumonia, a complication of dysphagia, is among the main reasons for hospital readmissions and mortality post-ICU, highlighting the importance of laryngeal and dysphagia evaluation (e.g., using flexible endoscopic evaluation swallowing).
5. Hearing loss and vertigo
Neurologic involvement is common in COVID-19. Although literature is limited, neurotological manifestations including ataxia, dizziness, imbalance, tinnitus, and sensorineural hearing loss have been observed [[10], [11], [12], [13]]. Intralabyrinthine hemorrhage –similar to pulmonary and cerebral microhemorrhages attributed to COVID-19 associated coagulopathy– may be responsible for persistent hearing and balance disturbances [14]. Awareness of inner ear symptoms is paramount to prompt screening and timely management with oral and intratympanic steroids. Patients with persistent balance disturbances in addition to cognitive impairment are at significant risks for falls and might benefit from vestibular therapy.
6. Taste and smell
New-onset taste and smell disorders are well-recognized symptoms of COVID-19, affecting over 60% of patients [15,16]. SARS-CoV-2 entry is mediated via Angiotensin Coverting Enyzme 2 (ACE-2) and Transmembrane serine protease 2 (TMPRSS-2) receptors present throughout the olfactory cleft, with associated inflammatory disruption of the nervous system via nasal olfactory fibers [17]. Symptoms often persist for 4–6 weeks, affecting patients' overall quality of life [[18], [19], [20]]. While early studies demonstrate a high rate of spontaneous resolution, the residual 10% with persistent olfactory dysfunction underscore the tremendous need for improved treatment options [21]. Rhinology expertise in post-viral olfactory disorders is critical for the continued development of objective screening measures and treatments for these debilitating sequelae [22].
7. Multidisciplinary care
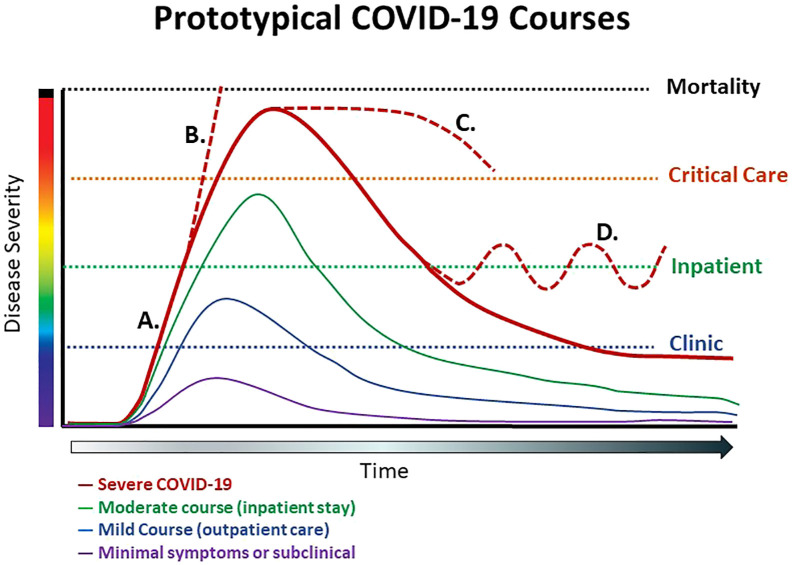
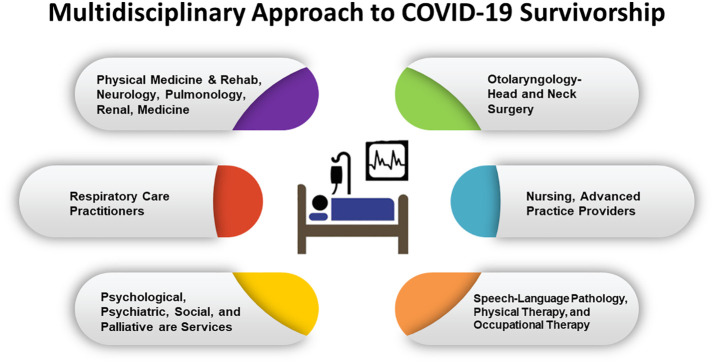
In the acute phase of illness, preventative measures to minimize risk of airway injuries, such as endotracheal tube cuff pressure monitoring, airway assessment, and proactive identification of underlying causes of dysphagia or dysphonia, may reduce long-term complications (Fig. 3 ) [23,24]. Otolaryngologists can partner with the multidisciplinary critical care team, including speech-language pathologists, nurses, respiratory therapists, and intensivists, to guide timely diagnosis and treatment of airway injuries (Fig. 4 ) [25].
Fig. 3.
Clinical courses of patients with COVID-19. A. Prototypical course of severe COVID-19, B. Progressive multiorgan failure, C. Protracted critical illness requiring extracorporeal membrane oxygenation (ECMO), D. Relapsing course requiring readmission. Other survivorship streams also depicted.
Fig. 4.
Multidisciplinary engagement in care of patients with COVID-19 during and after intensive care unit stay.
8. Implications for the future
Data science, machine learning, and biosensor technology will play increasingly prominent roles in patient care, ranging from early detection of physiological indicators of disease to timing for tracheostomy and other interventions to diagnosis and treatment of laryngotracheal injury or other manifestations of PICS. Prospective data registries, such as RegENT (www.entnet.org/content/reg-ent-1) and Global Tracheostomy Collaborative (www.globaltrach.org), provide platforms for data collection and analysis, risk adjustment, or future clinical prediction [1,26]. Otolaryngologists play a critical role in multidisciplinary efforts to facilitate high-quality recovery care and to improve COVID-19 patients' quality of life.
Funding support
Financial support for this review was provided by R01 DC018567 01 (Alexander T. Hillel) on the pathogenesis of laryngotracheal injury; R01 NIH 5-R017433 (Martin B Brodsky, Vinciya Pandian, and Dale M. Needham), on laryngeal injury post-extubation in intensive care unit settings; R01 DC14547 05 (Anil Lalwani), on intracochlear delivery of therapeutics across round window membrane; and K23 HL138206, (Ann Parker) a pilot feasibility randomized clinical trial to improve psychological and physical impairments in acute respiratory failure survivors.
Disclosures
Dr. Brodsky receives royalties from MedBridge, Inc.
Dr. Hillel is a consultant for Ambu and has a sponsored research agreement with Medtronic.
Dr. Rassekh was a collaborator for a Drexel University grant and patent pending for Biocontainment device (ABCD) which was assigned to University of Pennsylvania; Consultant/Speaker-Medtronic.
Dr. Needham is currently, or previously, a consultant to Haisco-USA Pharmaceuticals, Novartis Pharma (Switzerland), and GlaxoSmithKline (UK), and is a principal investigator on a NIH-funded, multi-centered randomized trial (R01HL132887) evaluating nutrition and exercise in acute respiratory failure, for which Baxter Healthcare Corporation has provided an unrestricted research grant and donated amino acid product, and Reck Medical Devices has provided an equipment loan to two study sites.
CRediT authorship contribution statement
| Author name | Contribution |
|---|---|
| Vinciya Pandian, PhD, MBA, MSN, ACNP-BC | Conceptualization; Data curation; Formal analysis; Methodology; Writing - original draft; review & editing. |
| Martin B. Brodsky, PhD, ScM, CCC-SLP | Conceptualization; Data curation; Writing - original draft, review & editing. |
| Emily P. Brigham, MD | Conceptualization; Data curation; Methodology; Writing - review & editing. |
| Ann M. Parker, MD, PhD | Conceptualization; Data curation; Writing - review & editing. |
| Alexander T. Hillel, MD | Data curation; Formal analysis; Methodology; Writing - original draft; review & editing. |
| Joshua M. Levy, MD, MPH | Data curation; Formal analysis; Methodology; Writing - original draft; review & editing. |
| Christopher H. Rassekh, MD, FACS | Conceptualization; Writing - original draft; review & editing. |
| Anil K. Lalwani, MD | Conceptualization; Writing - original draft; review & editing. |
| Dale M. Needham, MD, PhD, FCPA | Conceptualization; Data curation; Formal analysis; Methodology; Writing - review & editing. |
| Michael J. Brenner, MD, FACS | Conceptualization; Data curation; Formal analysis; Methodology; Writing – review & editing; supervision; review & editing. |
Declaration of competing interest
The authors discern no conflicts of interest; however to ensure to uncomprehensive disclosure, we list the relationships above.
References
- 1.McGrath B.A., Brenner M.J., Warrillow S.J., Pandian V., Arora A., Cameron T.S. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8(7):717–725. doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meister K.D., Pandian V., Hillel A.T., Walsh B.K., Brodsky M.B., Balakrishnan K. Multidisciplinary safety recommendations after tracheostomy during COVID-19 pandemic: state of the art review. Otolaryngol Head Neck Surg. 2020;194599820961990 doi: 10.1177/0194599820961990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hosey M.M., Needham D.M. Survivorship after COVID-19 ICU stay. Nat Rev Dis Primers. 2020;6(1):60. doi: 10.1038/s41572-020-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandharipande P.P., Girard T.D., Jackson J.C., Morandi A., Thompson J.L., Pun B.T. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bier-Laning C., Cramer J.D., Roy S., Palmieri P.A., Amin A., Anon J.M. Tracheostomy during the COVID-19 pandemic: comparison of international perioperative care protocols and practices in 26 countries. Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820961985. 194599820961985. [DOI] [PubMed] [Google Scholar]
- 6.Needham D.M., Davidson J., Cohen H., Hopkins R.O., Weinert C., Wunsch H. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–509. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 7.Pandharipande P.P., Girard T.D., Jackson J.C., Morandi A., Thompson J.L., Pun B.T. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fiacchini G., Trico D., Ribechini A., Forfori F., Brogi E., Lucchi M. Evaluation of the incidence and potential mechanisms of tracheal complications in patients with COVID-19. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.4148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brodsky M.B., Levy M.J., Jedlanek E., Pandian V., Blackford B., Price C. Laryngeal injury and upper airway symptoms after Oral endotracheal intubation with mechanical ventilation during critical care: a systematic review. Crit Care Med. 2018;46(12):2010–2017. doi: 10.1097/CCM.0000000000003368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mady O.M., El-Ozairy H.S., Wady E.M. Increased incidence of otitis externa in covid-19 patients. Am J Otolaryngol. 2020:102672. doi: 10.1016/j.amjoto.2020.102672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vijayasundaram S., Karthikeyan P., Mehta S.D. Proficiency of virtual follow-up amongst tinnitus patients who underwent intratympanic steroid therapy amidst COVID 19 pandemic. Am J Otolaryngol. 2020;41(6):102680. doi: 10.1016/j.amjoto.2020.102680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Satar B. Criteria for establishing an association between Covid-19 and hearing loss. Am J Otolaryngol. 2020;41(6):102658. doi: 10.1016/j.amjoto.2020.102658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sriwijitalai W., Wiwanitkit V. Hearing loss and COVID-19: a note. Am J Otolaryngol. 2020;41(3):102473. doi: 10.1016/j.amjoto.2020.102473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chern A., Famuyide A.O., Moonis G., Lalwani A.K. Bilateral sudden Sensorineural hearing loss and Intralabyrinthine hemorrhage in a patient with COVID-19. Otol Neurotol. 2021;42(1):e10–e14. doi: 10.1097/MAO.0000000000002860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D’Ascanio L., Pandolfini M., Cingolani C., Latini G., Gradoni P., Capalbo M. Olfactory dysfunction in COVID-19 patients: prevalence and prognosis for recovering sense of smell. Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820943530. 194599820943530. [DOI] [PubMed] [Google Scholar]
- 16.Amer M.A., Elsherif H.S., Abdel-Hamid A.S., Elzayat S. Early recovery patterns of olfactory disorders in COVID-19 patients; a clinical cohort study. Am J Otolaryngol. 2020;41(6):102725. doi: 10.1016/j.amjoto.2020.102725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meng X., Deng Y., Dai Z., Meng Z. COVID-19 and anosmia: a review based on up-to-date knowledge. Am J Otolaryngol. 2020;41(5):102581. doi: 10.1016/j.amjoto.2020.102581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reiter E.R., Coelho D.H., Kons Z.A., Costanzo R.M. Subjective smell and taste changes during the COVID-19 pandemic: short term recovery. Am J Otolaryngol. 2020;41(6):102639. doi: 10.1016/j.amjoto.2020.102639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakalli E., Temirbekov D., Bayri E., Alis E.E., Erdurak S.C., Bayraktaroglu M. Ear nose throat-related symptoms with a focus on loss of smell and/or taste in COVID-19 patients. Am J Otolaryngol. 2020;41(6):102622. doi: 10.1016/j.amjoto.2020.102622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lovato A., Galletti C., Galletti B., de Filippis C. Clinical characteristics associated with persistent olfactory and taste alterations in COVID-19: a preliminary report on 121 patients. Am J Otolaryngol. 2020;41(5):102548. doi: 10.1016/j.amjoto.2020.102548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fantozzi P.J., Pampena E., Di Vanna D., Pellegrino E., Corbi D., Mammucari S. Xerostomia, gustatory and olfactory dysfunctions in patients with COVID-19. Am J Otolaryngol. 2020;41(6):102721. doi: 10.1016/j.amjoto.2020.102721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levy J.M. Treatment recommendations for persistent smell and taste dysfunction following COVID-19-the coming deluge. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zaga C.J., Pandian V., Brodsky M.B., Wallace S., Cameron T.S., Chao C. Speech-language pathology guidance for tracheostomy during the COVID-19 pandemic: an international multidisciplinary perspective. Am J Speech Lang Pathol. 2020;29(3):1320–1334. doi: 10.1044/2020_AJSLP-20-00089. [DOI] [PubMed] [Google Scholar]
- 24.Pandian V., Morris L.L., Brodsky M.B., Lynch J., Walsh B., Rushton C. Critical care guidance for tracheostomy care during the COVID-19 pandemic: a global, multidisciplinary approach. Am J Crit Care. 2020:e1–e12. doi: 10.4037/ajcc2020561. [DOI] [PubMed] [Google Scholar]
- 25.Balakrishnan K., Schechtman S., Hogikyan N.D., Teoh A.Y.B., McGrath B., Brenner M.J. COVID-19 pandemic: what every otolaryngologist-head and neck surgeon needs to know for safe airway management. Otolaryngol Head Neck Surg. 2020;194599820919751 doi: 10.1177/0194599820919751. [DOI] [PubMed] [Google Scholar]
- 26.Brenner M.J., Pandian V., Milliren C.E., Graham D.A., Zaga C., Morris L.L. Global tracheostomy collaborative: data-driven improvements in patient safety through multidisciplinary teamwork, standardisation, education, and patient partnership. Br J Anaesth. 2020;125(1):e104–e118. doi: 10.1016/j.bja.2020.04.054. [DOI] [PubMed] [Google Scholar]
- 27.Abou-Arab O., Huette P., Berna P., Mahjoub Y. Tracheal trauma after difficult airway management in morbidly obese patients with COVID-19. Br J Anaesth. 2020;125(1):e168–e170. doi: 10.1016/j.bja.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bassi M., Anile M., Pecoraro Y., Ruberto F., Martelli S., Piazzolla M. Bedside Transcervical-Transtracheal Postintubation injury repair in a COVID-19 patient. Ann Thorac Surg. 2020;110(5):e417–e419. doi: 10.1016/j.athoracsur.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bertone F., Robiolio E., Gervasio C.F. Vocal cord ulcer following endotracheal intubation for mechanical ventilation in COVID-19 pneumonia: a case report from northern Italy. Am J Case Rep. 2020;21 doi: 10.12659/AJCR.928126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buselli R., Corsi M., Necciari G., Pistolesi P., Baldanzi S., Chiumiento M. Sudden and persistent dysphonia within the framework of COVID-19: the case report of a nurse. Brain Behav Immun Health. 2020;9:100160. doi: 10.1016/j.bbih.2020.100160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chirakkal P., Hail A.N.A., Zada N., Vijayakumar D.S. COVID-19 and tinnitus. Ear Nose Throat J. 2020;145561320974849 doi: 10.1177/0145561320974849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Filatov A., Sharma P., Hindi F., Espinosa P.S. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020;12(3) doi: 10.7759/cureus.7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koumpa F.S., Forde C.T., Manjaly J.G. Sudden irreversible hearing loss post COVID-19. BMJ Case Rep. 2020;13(11) doi: 10.1136/bcr-2020-238419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lamounier P., Franco Goncalves V., Ramos H.V.L., Gobbo D.A., Teixeira R.P., Dos Reis P.C. A 67-year-old woman with sudden hearing loss associated with SARS-CoV-2 infection. Am J Case Rep. 2020;21 doi: 10.12659/AJCR.927519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lang B., Hintze J., Conlon B. Coronavirus disease 2019 and sudden sensorineural hearing loss. J Laryngol Otol. 2020:1–3. doi: 10.1017/S0022215120002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wali A., Rizzo V., Bille A., Routledge T., Chambers A.J. Pneumomediastinum following intubation in COVID-19 patients: a case series. Anaesthesia. 2020;75(8):1076–1081. doi: 10.1111/anae.15113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brugliera L., Spina A., Castellazzi P., Cimino P., Arcuri P., Negro A. Nutritional management of COVID-19 patients in a rehabilitation unit. Eur J Clin Nutr. 2020;74(6):860–863. doi: 10.1038/s41430-020-0664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hajikhani B., Calcagno T., Nasiri M.J., Jamshidi P., Dadashi M., Goudarzi M. olfactory and gustatory dysfunction in covid-19 patients: a meta-analysis study. Physiol Rep. 2020;8(18) doi: 10.14814/phy2.14578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaye R., Chang C.W.D., Kazahaya K., Brereton J., Denneny J.C., 3rd. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg. 2020;163(1):132–134. doi: 10.1177/0194599820922992. [DOI] [PubMed] [Google Scholar]
- 40.Lechien J.R., Chiesa-Estomba C.M., De Siati D.R., Horoi M., Le Bon S.D., Rodriguez A. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. European Archives of Otorhinolaryngology. 2020 doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lechien J.R., Chiesa-Estomba C.M., Cabaraux P., Mat Q., Huet K., Harmegnies B. Features of mild-to-moderate COVID-19 patients with dysphonia. J Voice. 2020 doi: 10.1016/j.jvoice.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ozcelik Korkmaz M., Egilmez O.K., Ozcelik M.A., Guven M. Otolaryngological manifestations of hospitalised patients with confirmed COVID-19 infection. Eur Arch Otorhinolaryngol. 2020 doi: 10.1007/s00405-020-06396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]