Abstract
The coronavirus disease 2019 (COVID-19) pandemic created an extremely disruptive challenge for health care leaders that required a rapid, dynamic, and innovative response. The purpose of this manuscript is to share the leadership actions and decisions at Mayo Clinic in Florida during the first 6 months of the pandemic (February to July 2020). We note 4 strategies that contributed to an effective response: (1) leverage experience with disaster preparedness and mobilize regional and national networks; (2) use surge models to anticipate and to address supply chain issues as well as practical and financial effects of the pandemic; (3) adapt creatively to establish new safety and procedural protocols in various areas for various populations; and (4) communicate timely information effectively and be the common source of truth. Mayo Clinic in Florida was able to address the surges of patients with COVID-19, to provide ongoing tertiary care, and to restore function within the first 6 months with new, strengthened practices and protocols.
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019; HICS, Health Care Incident Command System; ICU, intensive care unit; IPAC, Infection Prevention and Control; MCF, Mayo Clinic in Florida; OR, operating room; PCR, polymerase chain reaction; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
When the first cases of coronavirus disease 2019 (COVID-19) were reported in the United States on January 20, 2020,1 hospitals around the country quickly began to assess their resources and to formulate steps they would take in the event of a surge of patients. Mayo Clinic began its preparations as an enterprise and at each of its 3 medical destination campuses: Rochester, Minnesota; Phoenix, Arizona; and Jacksonville, Florida.
The 34-year-old campus in Jacksonville, referred to as Mayo Clinic in Florida (MCF), has a 304-bed hospital and approximately 6500 employees, including 500 employed physicians and 130 researchers. The intensive care unit (ICU) has 54 beds with capacity to flex to 81 beds. Like all of Mayo Clinic, MCF holds as its guiding principle that “the needs of the patient come first.” It treats more than 100,000 patients annually, with the highest case mix index for patients insured through the Centers for Medicare & Medicaid Services in the state of Florida. MCF provides treatment in all specialties, with limited pediatrics, and is nationally ranked for its excellent outcomes and quality.2,3 The primary focus is on the treatment of patients with serious or complex diagnoses and on delivery of complex therapies, particularly in the fields of oncology, transplantation, and neurosciences.
Mayo Clinic worked across all 3 of its campuses to regulate supplies and personal protective equipment (PPE), to share best practices, and to provide support and communications with staff during the pandemic; however, leadership on each campus formulated the pandemic response relevant to the campus, region, and local population. The first case of COVID-19 in Florida was reported on March 1, 2020.4 The peak in our region was approximately 800 new confirmed cases per day in mid-July, and most hospitals were at their peak COVID-19 census in the last 2 weeks of July. At that time, our regional hospitals had, collectively, a daily census of more than 500 COVID-19–positive inpatients.
This manuscript provides an overall view of the pandemic response at MCF during the first 6 months of the COVID-19 outbreak in the United States from the perspective of its leadership team. Specifically, we describe 4 approaches that contributed to an effective response: (1) the leveraging of our well-established disaster preparedness and regional and national networking; (2) the proactive use of financial modeling and supply chain management; (3) the ability to continuously adapt creatively to establish new safety and procedural protocols in various areas of the hospital and for various populations as new information became available; and (4) the intentional effort to communicate the most up-to-date information quickly and to be a common source of truth. These strategies enabled MCF to weather the first months of the pandemic and to establish a new normal for future practice.
Strategy 1: Leverage Experience With Disaster Preparedness and Mobilize Regional and National Networks
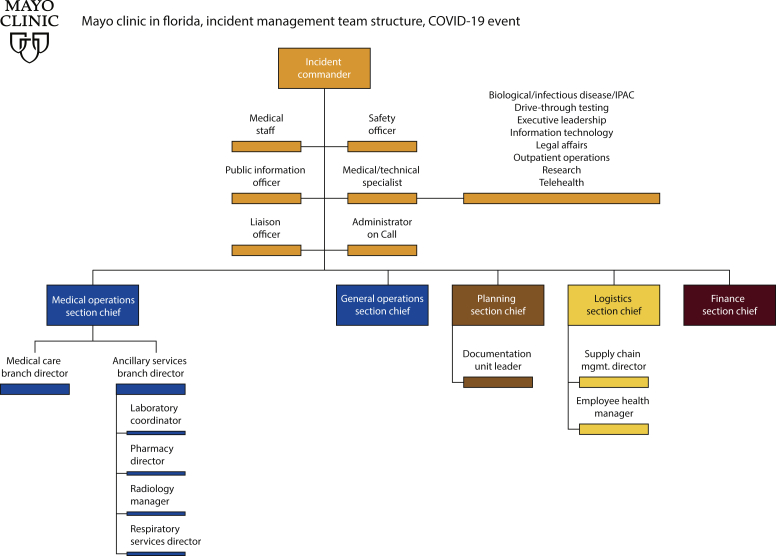
As we monitored the COVID-19 outbreak in China and as the first cases appeared in the United States in January, we began mobilizing our Health Care Incident Command System (HICS). As on Mayo Clinic’s other campuses, the Florida HICS team is a coordinated response team with a clear management hierarchy, engaging leaders from all areas to identify issues and to facilitate rapid changes. Because of the need for frequent hurricane response, the Florida HICS team has extensive disaster preparedness and management experience (Figure 1). By the time the first cases of COVID-19 were reported in Florida on March 1, 2020, HICS had a pandemic response in place and had engaged additional leaders from the departments of Infection Prevention and Control (IPAC) and Employee Health.
Figure 1.
Health Care Incident Command System (HICS). IPAC, Infection Prevention and Control; Mgmt, management.
Our HICS focus initially was on risk mitigation, identifying emerging needs, and planning changes to address safety issues. Members met 7 days a week, with rotation built in to avoid burnout. HICS leadership held daily meetings with practice and nursing leadership to exchange information and to coordinate efforts. As the scientific information and health guidelines changed daily, HICS had to make course corrections, implement changes, and promptly inform staff, ensuring an environment of physical and psychological safety for patients and employees.
However, it was also clear that no individual hospital would be able to face the pandemic on its own. As the scope and severity of the pandemic intensified, MCF benefited from staying connected to the other Mayo Clinic campuses and leadership and from leveraging its relationship with leaders of local hospitals not only to optimize Mayo Clinic’s internal efforts but also to use Mayo Clinic’s strengths to assist other facilities. The Hospital CEO Council, a group of 9 chief executive officers of local area hospitals and the commanding medical officer from the local Naval Hospital Jacksonville, increased the frequency of its monthly meetings and added a weekly call with the Jacksonville mayor to discuss the pandemic response and necessary public service announcements. The council engaged Florida’s Secretary of Health on multiple occasions to discuss the state-level pandemic response.
Despite being local market competitors, the area hospitals provided extensive mutually beneficial benchmarking and collaboration in best practices for patient and employee safety, COVID-19 testing protocols and access, supply chain management (particularly related to PPE), coordination of community surge planning, COVID-19 forecasting, visitor policies, and unified community education to inform local citizens of best practices to protect the community. This collaboration allowed the best possible response to the pandemic from all local health care institutions for the benefit of the community.
MCF sought to establish ongoing communication with city, state, and federal agencies. The chief executive officer at MCF served on the state of Florida COVID-19 Testing Task Force along with other local health care leaders. HICS members from the public affairs and government relations teams facilitated contacts as well as conversations with the nation’s vice president and an in-person visit with the Secretary of the US Department of Health & Human Services.5 These conversations enhanced MCF’s ability to have an impact on state and national responses to the pandemic and to disseminate information about clinical, research, and testing capabilities.
Strategy 2: Use Surge Models to Anticipate and to Address Supply Chain Issues as Well as Practical and Financial Effects of the Pandemic
At the onset of the pandemic, the HICS team established a predictive surge model in collaboration with Mayo Clinic practice and quality teams in Jacksonville and practice leadership. That model and subsequent iterations helped us plan proactive and flexible strategies to address the strains imposed by the pandemic, to restrict elective and nonelective surgical and other procedures, and eventually to restore the clinical practice.
One of the initial concerns for HICS was the availability of PPE and supplies critical for safe functioning of the hospital and outpatient clinics. By the time the first patient with suspected COVID-19 was admitted to Mayo Clinic Hospital in Jacksonville on March 13, HICS had predictive metrics of PPE stocks at MCF and on the other Mayo Clinic campuses. HICS members in supply chain collected data of available levels, daily consumption rate, and replenishment data of supplies. A centralized pipeline was established throughout Mayo Clinic’s campuses to distribute resources more efficiently.
The HICS team sought multiple sources of supplies and reviewed and secured various alternatives where risk of future shortage existed. For example, HICS worked with the HICS teams on the other Mayo Clinic campuses to procure reusable, laundered gowns when it looked like disposable gowns would be in short supply. As the demand for masks increased, the team worked to identify suitable substitute materials that could be used by non–patient-facing staff. Local Jacksonville companies shifted their production to manufacture thousands of cloth masks for MCF and other area hospitals. Because PPE and equipment were limited in March and April, contingency plans were developed. One such plan, devised by IPAC and HICS, was the implementation of a Mayo Clinic–adapted protocol to resterilize used N95 masks with ultraviolet light6,7 and vapor-phase hydrogen peroxide techniques.8,9 HICS also established plans for resterilized N95 respirators to be stored for future use in case of critical shortage. Throughout the pandemic, HICS continued to monitor data of local hospitalization rates, ICU bed availability, and COVID-19 patient census. Initially, daily models were used, which gradually changed to monthly forecasting models.
One critical, constantly changing strategy addressed diagnostic testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In early March, diagnostic testing was available only through the Florida Department of Health. At MCF, we implemented a 24/7 approval process, which required our clinicians to contact the IPAC infection preventionist on call, who would then consult with epidemiologists at the Florida Department of Health to determine whether each patient met criteria for testing at the state laboratory, and results would be returned within 3 to 5 days.
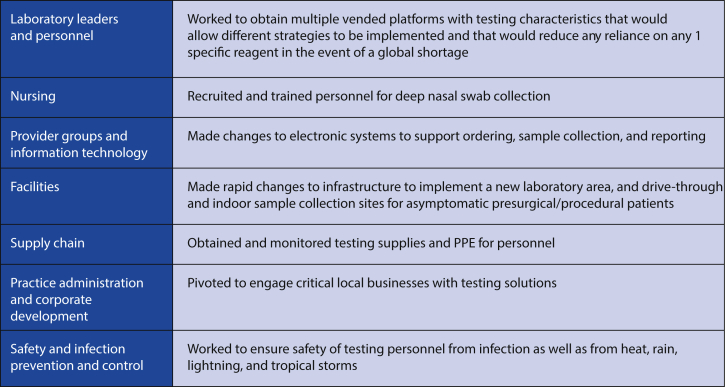
During a 10-day period in mid-March, the Department of Laboratory Medicine in conjunction with Mayo Clinic Laboratories expeditiously implemented deep nasal swab polymerase chain reaction (PCR) testing for SARS-CoV-2, which could be produced in high volume (up to 1100 tests per day) and provide results within 24 hours (Figure 2). As infection rates increased in the community and among asymptomatic patients, we designed and implemented a drive-through specimen collection unit, installed in a parking lot and staffed from 8 am to 2 pm, 7 days a week. As a safety measure, samples were transported to the laboratory by driverless autonomous vehicles provided in collaboration with the local transportation authority. Satisfaction ratings for the testing process from both patients and employees remained steadily high.
Figure 2.
Specialty teams that played a role in the implementation of high-volume testing. PPE, personal protective equipment.
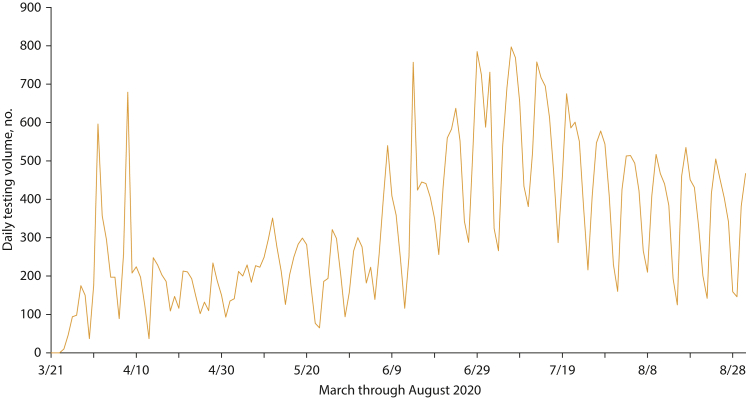
The need for daily tests grew rapidly (Figure 3). We implemented a universal SARS-CoV-2 testing strategy for all hospital admissions and for patients about to have surgical and other procedures, and we also provided testing for employee exposures. In addition, we established agreements to provide tests for Jacksonville’s first responders, local hospitals, businesses, and local naval base. The result was routine testing with a turnaround time of between 12 and 24 hours, same-day testing with a 4-hour turnaround for a select group of patients traveling from a distance for a procedure, and rapid testing with a 90-minute turnaround with prior authorization for urgent or emergent situations. As of April, MCF had provided more than 110,000 molecular PCR tests for our exposed or symptomatic patients; fire, rescue, and law enforcement personnel; local underserved communities; approximately 24 regional medical institutions (including the Naval Hospital Jacksonville); and more than 100 local businesses serving critical functions, including the Jacksonville Port Authority. In May, a storage area was repurposed to serve as an outpatient preprocedural testing area for asymptomatic patients to support the reopening of the surgical and procedural practices. Within a week, we were testing approximately1200 patients per week in this area.
Figure 3.
Daily testing volume by polymerase chain reaction for coronavirus disease 2019, March-August 2020.
The surge models also guided key workforce changes. In March, HICS established plans to mobilize 30 providers and allied health personnel from the outpatient practice to the hospital to staff new work areas including staff and patient screening areas, COVID-19 testing sites, and employee health telephone call lines. Outpatient appointments and elective procedures were rescheduled when providers determined a patient could safely and comfortably wait. More than 8700 appointments were rescheduled, and nearly 40,000 appointments were canceled during the week the initiative was activated. The capacity to provide care virtually with telephone and video visits was enhanced quickly and dramatically. MCF went from a prepandemic average of 50 video visits per week to more than 3000 per week at the height of the provision of virtual health services.
The models also prompted strategies to mitigate revenue losses, including institution-wide salary reductions and staff furloughs. Leaders across MCF were asked to scrutinize their expenses and to identify any opportunities to temporarily or permanently decrease them. On March 23, we halted elective surgical procedures to save bed space for COVID-19 patients and to preserve PPE in accordance with the directive from the Florida governor and guidance from organizations including the American College of Surgeons and the Centers for Medicare & Medicaid Services. The Florida directive considered elective surgical procedures to be procedures that could wait 3 to 6 months without significant harm coming to the patient. Frequent communications with our Legal Department and our MCF Surgical and Procedural Committee enabled us to scale back judiciously, and surgical calendars were monitored to ensure compliance with local and federal directives. With this measured response, we reduced our volume to 45% of our normal weekly surgical procedures until the prohibition on elective surgery was repealed in early May.
Updated models suggested the surge of COVID-19 cases would be delayed until the summer. The decision was made on May 4 to restore elective cases. We had robust safety protocols in place and a low hospital COVID-19 census and were able to plan the reactivation of our surgical practice as well as individual surgical services. Our strategy included the development of Saturday surgery protocols to allow services most affected by the restrictions to recover productivity. When a second wave of COVID-19 occurred in July, we were able to manage bed capacity by deferring surgical admissions to the weekend.
Strategy 3: Adapt Creatively to Establish New Safety and Procedural Protocols in Various Areas for Various Populations
As new information became available about the virus and health recommendations, it was essential to think flexibly and creatively to establish new safety and procedural protocols. Data from Wuhan, China, suggested that nearly 40% of infections were occurring within hospitals. Once high-volume testing became available, we made a rapid decision to test all inpatients, patients newly admitted to the hospital, and patients before surgical procedures. Testing enabled us to co-locate all positive cases, to isolate them from our patients receiving tertiary care, and to eliminate the need to move them from ICU to non-ICU care. Facilities operations oversaw the conversion of 2 hospital units to negative pressurization for care of patients with COVID-19. According to published recommendations, the rooms had recycled air filtered before recirculation with 6 air changes per hour.10,11 Our team was prepared to convert 2 other units to negative pressure, if needed. If those areas became full, our plan was to shift general nonimmunocompromised patients to our hospital-licensed space not typically used as overnight-stay patient care rooms (such as the outpatient surgery center).
The COVID-19 pandemic created challenges for treating MCF’s patients with complex conditions. Our population includes a high volume of patients who are immunocompromised, have received a solid organ transplant, or are undergoing chemotherapy. To maintain the safety of our non–COVID-19 patients, the allied health staff on the COVID-19 units did not care for patients on other units. Plans were made to cross-train health care practitioners if needed during COVID-19 surges. Nurses from the operating rooms (ORs) and clinics were assigned to inpatient training. Certified registered nurse anesthetists were cross-trained as ICU providers, as were our anesthesiologists. Internal medicine physicians were reappropriated from the outpatient clinic to the hospital to care for non-ICU patients with COVID-19.
We developed new protocols to provide surgery safely for patients with COVID-19. Those requiring emergency surgery were intubated in a negative pressure room and then transported intubated to the OR. Traffic in and out of the OR was minimized. Personnel in the OR wore appropriate PPE, including N95 respirators. Surgical leadership was in constant communication with ICU leadership to ensure that the surgical practice would not usurp ventilator capacity for COVID-19 patients.
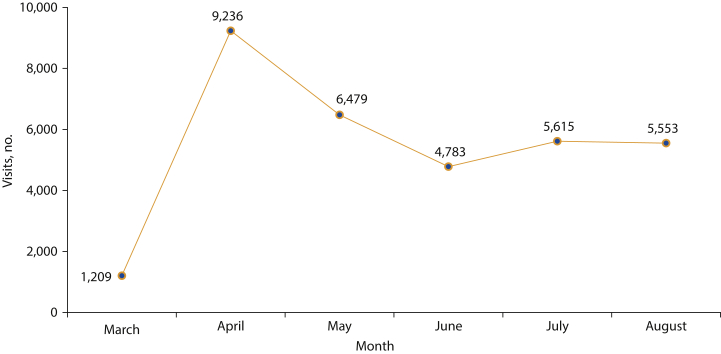
We established an entirely new service line for patients with COVID-19 who did not require hospitalization (Figure 4). The COVID-19 virtual clinic opened on the same day as our drive-through testing center with a full team of practitioners, including physicians, advanced practice providers, nurses, secretaries, and schedulers, and remains in effect. A patient who tests positive for COVID-19 is contacted through a patient portal and receives instructions about self-isolation and self-care. Our providers call patients and offer them enrollment in the COVID-19 virtual clinic, where their care can be managed through video visits and remote monitoring, including for temperature, oxygenation status, and vital signs. To date, 39 providers, 4 nurses, 2 secretaries, 2 schedulers, and an administrator have provided virtual care for approximately1800 patients.
Figure 4.
Virtual outpatient visits.
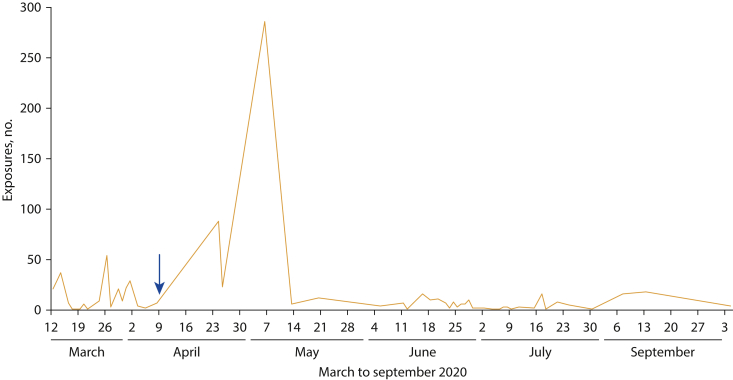
We responded quickly when several staff were exposed to COVID-19 by patients who had been infected in the community and who did not initially test positive on admission but developed symptoms during their hospitalization. On April 9, IPAC advocated implementing mandatory universal masking and eye protection for all patient-facing staff and using PPE conservation methods. After this important intervention, occupational patient-to-employee exposures were significantly reduced (Figure 5). Because of this speedy decision-making, MCF became an early adopter of universal mask use for employees and patients and eye protection for patient-facing employees.
Figure 5.
Reduction in staff exposure to coronavirus disease 2019 with the introduction of mandatory universal mask use.
Screening protocols were proactively and aggressively implemented. We consolidated available passage to our buildings to select entryways and established COVID-19 symptom screening and temperature checks on arrival for all ambulatory and hospital patients and for staff. Before our first case of COVID-19, we partnered with Environmental Health and Occupational Safety to create COVID-19 patient flow protocols and performed drills in the event of a COVID-19 patient encounter in ambulatory areas, the emergency department, the ICU, operating/procedure rooms, the radiology department, and laboratories.
For non–COVID-19 patients in the hospital, HICS made the difficult decision to restrict visitors. Exceptions were clearly defined and listed: end-of-life cases, minors, patients with special needs (dementia, mental illness), transplant patients (when family had to be trained for home care), and before discharge for patients requiring postsurgical instruction. Special requests beyond the list were reviewed on a case-by-case basis by top hospital leadership; visitation was for 1 person during the patient’s hospitalization. A plan was established to relax this policy when the regional PCR-positive rate remained below 5% and the COVID-19 patient daily census in the hospital remained below 15 cases.
On April 7, plans began to reopen the outpatient practice for face-to-face visits and outpatient care because of patient need and organizational viability. IPAC defined PPE and cleaning/disinfection protocols to be implemented in clinical areas. IPAC conducted site visits at all ambulatory practices that perform high-risk, aerosol-generating procedures to ensure optimal air exchanges in procedure rooms. In addition, general workflow and scheduling guidance was provided to include appropriate signage and social-distancing measures.
Strategy 4: Communicate Timely Information Effectively and Be the Common Source of Truth
As COVID-19 introduced an environment of sustained uncertainty and changing protocols, we determined that forthright and clear communication with all stakeholders was of paramount importance. Decisions by HICS about situational changes, including the inpatient census of COVID-19–positive patients, were communicated daily to all MCF employees. HICS leadership also held daily meetings with practice and nursing leadership to exchange information and to coordinate efforts.
Our goal was to establish the common source of truth for rapid understanding of the issues, answering common questions, and addressing issues and fears facing our staff. Numerous communication methods were used, with an emphasis on providing staff with information, education, and emotional support. Resources targeted different learning styles (eg, written communications, videos, infographics, flyers, in-person huddles). A website was initiated to provide immediate guidance about safety practices for COVID-19. The website contained answers to frequently asked questions and resources to help staff care for patients, themselves, their families, and each other and was continually updated as COVID-19 health and medical recommendations evolved. For the first 2 months of the pandemic, we also sent a daily COVID-19 staff update by email; by June, “The Florida Report” was decreased to 3 emails weekly containing current COVID-19 case volumes, appointment and visit data, and any urgent or semiurgent content relevant to staff. We also held interactive town hall meetings (available live and remotely) to answer questions about policy changes and Mayo Clinic’s response. To bolster the sense of community for our staff, we created a private Facebook group in mid-March, which was unmonitored by staff and grew to more than 1300 members.
Initially, anxiety among staff led to excessive use of N95 respirators and an accelerated consumption rate. In conjunction with IPAC and HICS, clear guidelines on which type of PPE to wear under specific situations were developed and implemented. We created videos12 for safe donning and doffing and for how to properly use N95 respirators. Guidelines for extended use of respirators were defined and disseminated, reducing usage rate without any negative effects. Responding to practice concerns and providing consistent directions helped reassure staff that appropriate measures were in place to keep them safe while preserving resources. In late June, as Jacksonville reopened, positive COVID-19 test results increased among employees and in the community. On June 26, MCF launched a “Lead by Example” campaign along with other Mayo Clinic campuses to encourage staff to promote safe practices, such as wearing masks at work and in the community.
Our communication strategies also reached beyond the hospital. Once we were able to offer testing, our infectious disease and IPAC teams reached out to local businesses to help mitigate the risk of outbreaks. We helped businesses determine appropriate masking or social-distancing requirements and testing strategies for their needs. We also provided advice about cleaning agents and mechanical filtration devices. Our consulting services were available to local universities and schools. Such comprehensive solutions have helped businesses avoid potentially catastrophic disruptions to their operations and have benefited the greater Jacksonville community.
Conclusion
The COVID-19 pandemic presented MCF with a crisis that initially destabilized normal practice. With our disaster preparedness and a strategic approach, we were able to respond nimbly, addressing the major life-threatening health concerns both for patients with COVID-19 and for our patients receiving tertiary care. We intentionally sought to learn from the experience and not simply to return to pre–COVID-19 operating models. Some of the changes we implemented aligned with our interests and with long-term enterprise-wide plans at Mayo Clinic, such as the expansion of virtual care. Other changes, such as streamlining staff, enabled us to question certain roles or expenses and to explore potentially better operational models. Our response positioned us to address the next stages of the COVID-19 outbreak as well as future pandemics.
Acknowledgments
The authors would like to thank Andrea L. Kane and Kate K. Ledger for editorial assistance. The authors would also like to extend gratitude to the employees of Mayo Clinic in Florida for their dedication and fortitude in serving patients during the COVID-19 pandemic.
Footnotes
Potential Competing Interests: The authors report no competing interests.
References
- 1.Holshue M.L., DeBolt C., Lindquist S., et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Business Wire Inc Vizient presents Clinical Performance Awards at the 2019 Connections Education Summit. September 20, 2019. https://www.businesswire.com/news/home/20190920005040/en/Vizient-Presents-Clinical-Performance-Awards-at-the-2019-Connections-Education-Summit
- 3.US News & World Report Best hospitals in Florida. https://health.usnews.com/best-hospitals/area/fl
- 4.Florida Department of Health Department of Health announces two presumptive positive COVID-19 cases in Florida. March 1, 2020. http://www.floridahealth.gov/newsroom/2020/03/030120-two-presumptive-positive-covid19-cases.pr.html
- 5.First Coast News They're doing everything right': US health secretary visits TIAA Bank's COVID-19 testing site. May 22, 2020. https://www.firstcoastnews.com/article/news/health/coronavirus/hhs-secretary-alex-azar-visits-tiaa-banks-covid-19-testing-site/77-2c2285c0-a98b-4666-a3bf-a07f8522be33 Accessed September 17, 2020.
- 6.Xenex Disinfection Services New testing confirms Xenex LightStrike pulsed Xenon UV robots do not damage N95 respirators. April 16, 2020. https://www.xenex.com/resources/news/new-testing-confirms-xenex-lightstrike-pulsed-xenon-uv-robots-do-not-damage-n95-respirators/ Accessed September 17, 2020.
- 7.Xenex Disinfection Services LightStrike pulsed Xenon UV: disinfection of N95 respirators: draft Xenex practice bulletin. https://www.hawaiihealthpartners.org/media/2437/xenex-using-uv-to-disinfect-n-95-respirators.pdf
- 8.Battell Memorial Institute Personal protective equipment (PPE) decontamination for reuse: delivering critical equipment to hospital systems. https://www.battelle.org/inb/battelle-critical-care-decontamination-system-for-covid19?gclid=EAIaIQobChMImcHssIDn6wIVg4bACh1qGwu0EAAYASAAEgI_HvD_BwE
- 9.US Food & Drug Administration Investigating decontamination and reuse of respirators in public health emergencies. May 13, 2020. https://www.fda.gov/emergency-preparedness-and-response/mcm-regulatory-science/investigating-decontamination-and-reuse-respirators-public-health-emergencies
- 10.National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. July 15, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
- 11.Goh K.J., Wong J., Tien J.C., et al. Preparing your intensive care unit for the COVID-19 pandemic: practical considerations and strategies. Crit Care. 2020;24(1):215. doi: 10.1186/s13054-020-02916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mayo Clinic for Medical Education and Research Donning and doffing a mask with intent to reuse. June 18, 2020. https://mssvideoupload.mayo.edu/media/Donning+and+Doffing+a+Mask+with+Intent+to+Reuse/0_ab9j45sq