Abstract
The world is facing a global crisis and health emergency of COVID-19. Understanding of COVID-19 pathophysiology in ayurvedic host centric framework is prerequisite for apt use of Ayurveda. This paper reviews COVID-19 pathophysiology, clinical presentations and prognosis in ayurvedic perspective. Concept of exogenous pathogenic diseases can be traced in fever, microbes, toxins, epidemics and seasonal regimens chapters of Ayurveda. Such exogenous diseases later manifest multi-system presentation according to involvement of different ‘Dosha’ and derangement of ‘Agni’. The pathology of COVID-19 is primarily that of Sannipata Jwara (fever) with involvement of respiratory system. Secondary manifestations include coagulopathies, cardiovascular, neural, and renal complications. Gastrointestinal system is closely associated with respiratory mechanism in ayurvedic pathophysiological conceptualization of Srotas. Abnormal immune responses in COVID-19 are result of abnormalities of Tridosha, Rakta (blood) and Ojus (Vital nectar). The initial phase is Vata-Kapha dominant whereas later stage of aggravated immune response is Vata-Pitta dominant. Alveolar damage, coagulopathies indicate Rakta dhatu vitiation. With this integrative understanding of COVID-19, we propose novel strategies for therapeutics and prophylaxis. Measures for ‘Conservation of Agni-bala’, ‘Attainment of Rakta- Pitta-Prana homeostasis and ‘Protection of Tri-Marma i.e. vital organs’ can be important Host based strategies for reduction in the mortality in COVID-19 and for better clinical outcomes. This host centric approach can make paradigm shift in management of this epidemic.
Keywords: Complimentary medicine, Physiopathology, Ayurveda, SARS COV-2, Host centric, Prophylaxis
1. Introduction
The world is facing a never like pandemic of COVID-19 with its implications at economical, psychological and more levels in society. Pragmatic strategies are being proposed for possible role of Ayurveda in management of COVID-19 [1]. Scientists are proposing need of ‘Systems approach’ as it can provide more comprehensive structure to manage disease as well as epidemic components, as society is itself a complex adaptive system [2]. Potential of Ayurvedic immunomodulators (Rasayana) medicines and need of host centric approaches are proposed by the time [3,4]. The need for ‘host centric approach’ gets underlined amidst recurrence (of infection and disease) in cured patients of COVID-19 [5].
Understanding COVID-19 Pathophysiology is basic prerequisite for deciding Ayurveda preventive and curative strategies. One cannot appropriately bridge Ayurveda with evidence based medicine without understanding epistemology of Ayurveda [6]. Ayurveda deals at more comprehensive levels of abstraction like Dosha and Dhatu (tissues). Thus an appropriate translation of COVID-19 in Ayurvedic anatomical and pathophysiological terminology is needed. This article reviews COVID-19 pathology and its Ayurvedic perspective and discuss host centric approach of Ayurveda for COVID-19.
2. Infectious diseases in Ayurveda
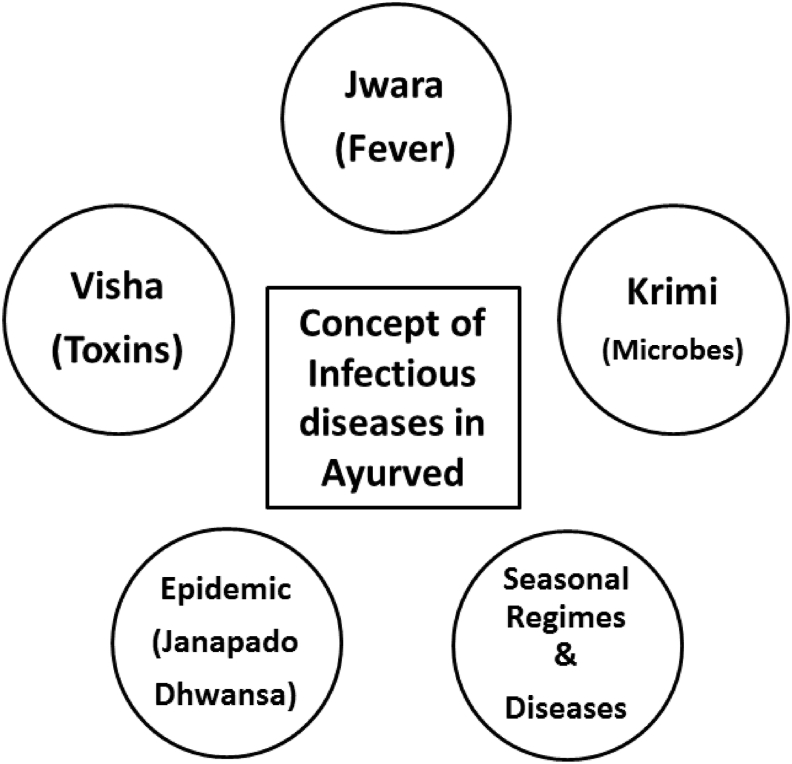
The concept of pathogenic agents and infectious disease was not unknown to Ayurveda. Fundamentally Ayurveda classifies diseases as Nija (from Intrinsic Causes), Agantuja (Extrinsic causes) and Manasa (Psychosomatic). Aupsargika (Infectious) and Sankramak (Contagious) are mentioned by Sushruta (7th century BC). The concept of infectious diseases is explained under five chapters Jwara, Krimi, Visha, Janapadodhwamsa and Ritucharya (Seasonal regimes). Jwara (Hyperthermia) is cardinal symptom in many of infectious diseases. Krimi is all encompassing term used for parasites, worms and microbes. Arundatta the commentator of Ashtang Hridaya clarifies that pathogen of the blood is totally invisible to the human eye, their existence can be inferred [7].
Janapadodhwamsa is the concept of epidemics in Ayurveda. Ritucharya is the season specific regimes where prophylaxis and management of seasonal flu can be seen. Autumn and spring fevers are associated with Pitta and Kapha dominance [8]. Role of seasonal changes in environment, particularly temperature and humidity are proven to be associated with modifications in host intrinsic, innate, and adaptive immune responses to viral infections in the respiratory tract [9] (Fig. 1).
Fig. 1.
Concept of Infectious diseases in Ayurveda
‘Dosha’ and ‘Agni’ are the pivotal concepts as imbalance or balance of Dosha and Agni are synonymous with state of disease or being healthy. Even in exogenous diseases, there is the role of Dosha and Agni in disease manifestation and prognosis. Dosha, Dhatu, Mala, Srotas, Agni and Manas (mind) is the framework in which any disease is needed to be interpreted. Concept of diagnosis in Ayurveda is less about naming diseases but understanding the underlying in-equilibrium. Charaka says that innumerable diseases can origin from same vitiated Dosha according to variations in aetiology and involved body tissues [8]. With these insights COVID-19 is reviewed here.
3. Understanding COVID-19 disease & Ayurveda
3.1. The virus and Ayurveda
Coronaviruses is a genus in the Coronaviridae family (order Nidovirales) of pleomorphic and enveloped viruses. Three human coronaviruses HCoV-OC43, HCoV-229 E and SARS CoV-1 were acknowledged as pathogenic agents for upper respiratory tract infections [10].
Although not mentioned as virus but microbes and pathogenic agents are described in Ayurveda as reviewed earlier. The initial stage of COVID-19 is exogenous (Agantu) disease which later converts into systemic (Nija) disease [11]. Abhishangaja Jwara is the term for those caused by the contact of the poisonous air or toxic plants or other such toxins [11]. However this Abhishangaja Jwara later complicates with involvement of multiple tissues and organs.
3.2. The epidemics/contagious complement and ayurveda
According to few reports SARS-CoV-2 can be detected in the air, three hours after aerosolisation. WHO has issued guidelines for contact and droplet precautions for healthcare workers working for suspected COVID-19 patients, also USA-CDC has recommended airborne precautions [12].
Janapadodhwamsa is the Ayurvedic term for epidemics. Janapada refers to particular geographic consideration. Interestingly there is mention of an epidemic fever with respiratory system presentation (fever, cough, breathing difficulty, rhinorrhoea, headache and even anosmia) caused by entry of pathogenic agent through the nasal passages. This clinical presentation by Sushruta is amazingly analogous to epidemics like SARS, MERS, Swine Flu and even COVID-19 [13]. Contagious diseases and means of contagion as physical contact, inhalation, eating together, sleeping, sitting together and sharing used linens and garlands are well discussed by Sushruta.
3.3. Stage wise disease progression, immune response, lung events and ayurveda
There are four stages of Disease progression viz Asymptomatic Stage, Stages with upper and Lower Respiratory tract involvements and last Stage of ARDS/MODS. The disease progression and stagewise Immune Responses are summarised in Table 1.
Table 1.
COVID-19 Disease Progression: Pathophysiology and Immune Response.
| Disease progression | Local pathophysiology | Stage wise immune response |
|---|---|---|
| Stage 1 Asymptomatic stage | Entry of virus in nasal passage Epithelial cells (particularly Ciliated cells) get affected [14]. ACE2 is important receptor along with TMPRSS2 [15,16]. Although less viral load, individuals are infectious. | Mild Innate immune response. Th1 response by host is crucial to decide fate of infection. |
| Stage 2 Upper Respiratory Tract involvement | Sputum swab exhibit SARS CoV-2 In few Cough, sore throat starts here. In most cases progression ends here. | Strong Innate immune response. Increased plasma IP-10,MIG, IL- 8 and MCP levels during the first week are considered independent predictor of outcome & with adverse outcome. (intensive care unit admission or death) [17,18] |
| Stage 3 Lower Respiratory Tract involvement | Virus starts affecting alveoli. It affects type II pneumocytes (responsible for production of surfactant and are precursor for type I pneumocytes) than type I pneumocytes (responsible for gaseous exchange). Type II pneumocytes undergo apoptosis and die due to viral particles [19]. | Aggravated immune response: Cytokine storm: lower lymphocyte counts and higher plasma concentrations of a number of inflammatory cytokines such as IL- 6 and tumor necrosis factor (TNF) [20]. |
| DAD: Diffuse alveolar lung damage: This is most commonly seen histopathologic feature [21]. Histologically: Injury to the alveolar epithelial cells, Hyaline membrane formation, Hyperplasia of type II pneumocytes, Consolidation by fibroblastic proliferation with extracellular matrix and fibrin forming clusters [22]. | Crucial role of T cells: Another study reported that CD4+ T cells, CD8+ T cells, and natural killer cells were reduced in severely ill patients compared with those with mild disease symptoms. Moreover, a substantial reduction of CD4+ T cell and CD8+ T cell counts in the peripheral blood was also observed in a patient who died [23]. | |
| Alveolar macrophages affected: Alveolar macrophages expressing ACE2 are again target cells for SARS-CoV-2 infection. | ||
| Alveolar condensation, Ground glass infiltrations, Hypoxia | ||
| Stage 4 ARDS, MODS | Acute Respiratory Distress SyndromePulmonary thrombosis HLH-like (haemophagocytic lymphohistiocytosis) cytokine storm with characteristics of HLH, including hypercytokinemia, unremitting fever, cytopenias, hyperferritinemia, and multi- organ damage, are commonly seen in seriously ill patients with COVID-19 [20]. | Raised Serum Ferritin (doubling in24 h) and raised IL-6, LDH, D- dimer, C-reactive Protein (CRP) levels mark severe condition. |
Events in Lung and Ayurveda Perspectives (Table 2).
Table 2.
Lung Events and Ayurveda. Importantly COVID-19 lung pathology is more restrictive than obstructive as it is more an alveolar diseases than airway disease, the basic lung pathology classification. Pathological events in lungs and Ayurveda Perspectives are summarized in this table
| Lung pathology | Ayurveda pathophysiological interpretations |
|---|---|
| Diffuse Alveolar Lung Damage: Type II pneumocytes hyperplasia Diffuse alveolar damage with presence of multinucleated pneumocytes. Fibro-granulation tissue proliferation in small airways and airspaces (organizing pneumonia-like lesions) in subpleural locations in some patients [23]. Some studies report along with classical DAD, there are evidences of: Capillary injury Mural and luminal fibrin deposition Infusion of the inter-alveolar septa by Neutrophils/macrophages. | Embryologically lungs are made of bubbling in Rakta (blood) Dhatu. The airsacs represent bubbles, whereas the alveolar composite structure is made from Rakta. COVID-19 is Alveolar disease and thus ‘Rakta Dhatu’ remains pivotal in pathology. Type II pneumocytes which serve as precursor for Type I pneumocytes and those produce surfactants get affected. This Regenerative ability of cells/tissue is attributed to Rasa & Shukra Dhatu the first and last tissue in hierarchy of body tissues. Ayurvedic Rasayana & Vajikarana medicines have regenerative efficacies. |
| Hyaline membrane formation: A membrane composed of proteins and dead cells lines the alveoli, making gas exchange difficult or impossible, Alveolar condensation | The word exudate is derived from latin “exsudare”, literally meaning ‘to sweat out’. Exudative inflammation is like Vishyandana,Ayurvedic term indicating phenomenon of liquefaction. This further result in alveolar condensation. The hyaline membrane formation and obstruction is nothing but Avarodha (Obstruction) by Kapha in turn leading to further vitiation of Vata. |
| Only Kapha is not necessarily responsible for obstructive phenomena. Even Vata subtypes may obstruct each other. COVID-19 symptoms like anosmia, ageusia and impaired Bala (immunity) are seen as symptoms of ‘Prana Avruta Vyana’ [24]. ‘Prana Avruta Vyana’ is condition when Prana Vata (Vata subtype responsible for pulmonary and nervous and cognitive functions) obstructs Vyana Vata (Vata subtype for cardio-pulmonary pumping and Bala i.e. strength and immunity) | |
| Interstitial widening and patches of Lung fibrosis | This can be Upadrava (complication) or Udarka (residual effect) Khara Paka i.e. abnormal metabolism leads to hardening of tissues/fibrotic changes. It will be interesting to see if these post COVID-19 fibrotic changes are therapeutically reversible or not. They can be called as upadrava (Complications) or Udarka (residual effect of the disease that is not relieved by the specific treatment) of COVID-19 |
3.4. Symptomatology, cytokine storm and Ayurveda
Symptoms include aches and pains, sore throat, diarrhea, conjunctivitis, headache, loss of taste or smell. A rash on skin and discoloration of fingers or toes are less common symptoms. Serious symptoms include difficulty breathing or shortness of breath, chest pain or pressure, loss of speech or movement. Nasopharyngeal swab Polymerase chain reaction analysis confirms the disease.
3.4.1. Respiratory symptoms in Sannipata Jwara
Abhishangaja Jwara, Bhootopasangaja Jwara is Vishama Jwara according to Vagbhata. Sannipatika is a disease variant with vitiation of all three Dosha in pathogenesis. Agantuja varieties of any diseases can complicate into Sannipatika state with severe prognosis. The viral or bacterial fevers, along with malignancy, auto immune diseases, etc. are needed to be considered as Sannipatika state. In COVID-19 Primary manifestations are seen at Pranavaha Srotas as virus enters through nasal passage (Table 3).
Table 3.
Respiratory symptoms in Sannipata Jwara.
| Symptoms | Variant of Sannipata Jwara | Classic |
|---|---|---|
| Pratishyay (Rhinorrhoea) | Diminished Kapha, moderate Pitta & increased Vata Sannipata | Charaka Samhita |
| Kasa (Cough) | Increased Kapha –diminished Vata and Pitta Sannipatika, Increased Vata and Kapha & diminished Pitta Sannipata Diminished Kapha, moderate Pitta & increased Vata Sannipata | Charaka Samhita |
| Shwasa (Dyspnea) | Diminished Kapha, moderate Pitta & increased Vata Sannipata | Charaka Samhita |
| Vata Kapha dominant Sannipata | BhavaPrakasha | |
| Pleural pain | Diminished Kapha, moderate Pitta & increased Vata Sannipata | Charaka Samhita |
| Vata Kapha dominant Sannipata | BhavaPrakasha |
Respiratory symptoms are seen in different types of Sannipata jwara.
The most mimicking ‘Kanthkubja Sannipata’ symptoms include throat pain, dyspnoea, tastelessness, delirium, Malaise, dehydration, head ache, shaking [25]. Out of the 29 Lakshanas of SarvaDoshaSannipata, 25 Lakshanas are found in the COVID-19 infection [26].
To summarize, the early presentation of COVID-19 is ‘Kapha Vata’ dominant whereas late phase of complications is ‘Vata Pitta’ dominant. The later phase of secondary infections, sepsis & multi organ failure is indicative of involvement of ‘Marma-Asthi-Sandhi Roga Marga’ (disease pathway).
Abhishangaja Jwara, Bhootopasangaja Jwara is Vishama Jwara according to Vagbhata, Sannipatika is a disease variant with vitiation of all three Dosha in pathogenesis [27]. Agantuja varieties of any diseases can complicate into Sannipatika state with severe prognosis. The viral or bacterial fevers, along with malignancy, auto immune diseases, etc. are needed to be considered as Sannipatika state [28]. Primary manifestations are seen at Pranavaha Srotas as virus enters through nasal passage.
3.4.2. Understanding Cytokine storm in Ayurveda Perspectives
Cytokine storm is overreaction of immune system exhibiting numerous cytokines and resulting in inflammation/necrosis of internal organs, and organ failure. It can be tempting for Ayurveda authors to compare cytokine storm with aggravated Vata, aggravated Agni, Dhatu paka (Body tissue disintegration as result of aggravated Agni), Shotha (Inflammation) or diseases like Jwara and Visarpa where the involvement of body tissues can become fatal very rapidly. There cannot be one single comparable phenomenon in Ayurved for cytokine storm. The ‘effect’ of cytokine storm is seen on vital organs, quoted as Marma in Ayurveda. Heart, brain and kidney are three important Marmas i.e. vital organs which are accounted into Madhyama Rogamarga (middle pathway for manifestation of disease), amongst three Roga marga (three broad based groups of disease pathways).
In Ayurvedic epistemology vyavayee guna (the important attribute of Visha) makes pathogenesis rapid. Gara Visha is the relevant Ayurveda concept of toxins where Gara literally means the one digluted. Ashtang Sangraha has mentioned that Gara Visha (A group of poisons where one can find ‘Combination of parts of the body and excreta of different animals enlisted) can be fast acting. Thus Visha is an important consideration as there is speedy and lethal pathogenesis that affects vital organs. The speediness is important virtue of pathogenesis in COVID-19.
3.5. Complications & multi-organ involvement in COVID-19 and Ayurveda
ACE2 receptors are there in many tissues and thus COVID-19 presents as Multi-systemic disease [29].
3.5.1. Gastrointestinal complications
Abundant amount of ACE2 is present in the small intestine and colon, which can be the probable reasoning for gastrointestinal symptoms like diarrhea, nausea, vomiting, and abdominal discomfort or pain. Mild to moderate liver injury (elevated aminotransferases, hypoproteinemia, and prothrombin time prolongation) has been reported. Analysts have suggested that abdominal pain can be used as a clinical predictor of more severe disease and be involved in future risk stratification algorithms [30].
3.5.2. Neural complications
Agitation, confusion, diffuse corticospinal tract signs with enhanced tendon reflexes, ankle clonus, bilateral extensor plantar reflexes, disorientation, and poorly organized movements in response to command, were reported during and or at the time of discharge [31].
3.5.3. Cardiac complications
After respiratory system, the second most affected body system known by COVID-19 is the cardiovascular system [32]. Patients with cardiovascular risk factors are at increased risk to develop severe complications. Some cardiovascular diseases associated with COVID-19 include myocarditis, heart failure, cardiac arrhythmias, and acute coronary syndrome as direct consequences of systemic inflammation [33].
3.5.4. Vascular complications
Reports about association of coagulopathies with poor prognosis and probable role of anti-coagulants like low molecular heparin are published [34]. Elevated D-dimer and FDP (Fibrin Degradation products) are common in deaths with COVID-19. Poor prognosis is also associated with disseminated intravascular coagulopathy (DIC) [35].
In Ayurveda terminology coagulopathies are ‘Kapha dominant Raktapitta’. Charaka has mentioned Raktapitta as complication of Jwara. Raktapitta represents a group of pathologies including coagulopathies, vascular complications etc.
3.5.5. Renal complications
The ACE2, is abundant in renal tubular epithelial cells. This can be linkage for some associations between COVID-19 and acute kidney injury (AKI), proteinuria, microhematuria and raised serum creatinine. Acute kidney injury is more common among patients with more severe disease, and is considered a negative prognostic factor with respect to survival [36]. Perhaps a maladaptive systemic inflammatory immune response, cytokine storm may contribute to hypoperfusion and thus result in injury to the renal tubules. Systemic hypoxia, abnormal coagulation are causes and diffuse proximal tubule injury with frank necrosis was evident. There were prominent erythrocyte aggregates obstructing the lumen of capillaries without platelet or fibrinoid material [37].
3.5.6. Sepsis/MODS (Multi Organ Dysfunction Syndrome)
Critically ill COVID-19 patients are reported to develop typical clinical manifestations of shock, with severe metabolic acidosis, indicating possible microcirculation dysfunction and impaired liver and kidney functions [38]. Sepsis in COVID-19 cases have wide range of signs and symptoms of multi-organ involvement, including respiratory manifestations, hypoxemia, renal impairment with reduced urine output, tachycardia, altered mental status, and functional alterations of organs expressed as laboratory data of hyperbilirubinemia, acidosis, high lactate, coagulopathy, and thrombocytopenia [39].
Ayurveda scholars have mentioned similitudes between Sama Sannipatika Jwara with ‘sepsis/septic shock/systemic inflammatory response syndrome (SIRS)/multiple organ dysfunction syndrome (MODS)/septic encephalopathy/delirium’ [40].
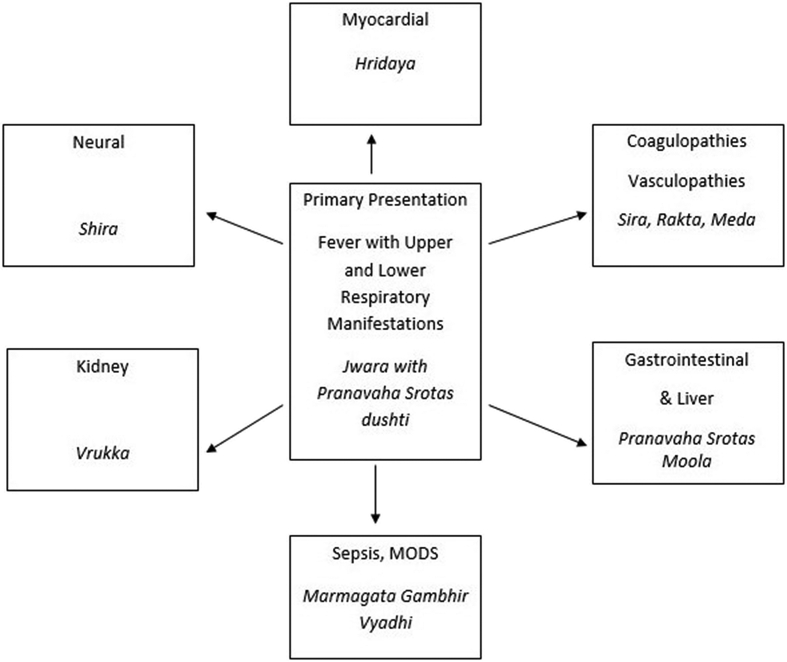
Cardiac, Renal and Neural presentations indicate involvement of Tri Marma (three most vital organs). Hepatic derangements and coagulopathies underline vitiation of Rakta. Involvement of all three Roga marga (Ayurveda diseases pathways) is seen (Fig. 2).
Fig. 2.
Primary and secondary manifestations of COVID-19 in Ayurveda perspective.
4. COVID-19 in Ayurvedic model of Hetu (Etiology)- Linga (Symptomatology) - Samprapti (Pathogenesis)
4.1. Etiology factor (Hetu) and probability of disease progression
The COVID-19 pathogen is Agantuj (exogenous) 80% patients of COVID-19 remain asymptomatic. Contact with viral material can be considered as Pradhanik Hetu (etiological factor weak enough to cause disease at its own). SARS CoV-2 can be better interpreted as Vyanjaka Hetu (etiological factor acting at time of genesis of disease), whereas Utpadak Hetu are etiological factors are mainly diet and lifestyle leading to accumulation of Dosha. In Ayurvedic conceptualization accumulated Dosha makes the body susceptible to disease. Even in an exogenous disease, there is involvement of Dosha and the role of Agni in prognosis of disease. As COVID-19 prognosis is associated with comorbidities, this concept of Utpadaka Hetu becomes important. Original retrospective studies of non survivors or critically ill cases of COVID-19 can contribute as evidence for these life style factors as Utpadaka Hetu for bad prognosis of COVID-19.
4.2. Linga
The symptoms of COVID resemble with sannipatika jwara as reviewed earlier. COVID-19 symptoms are summarized here in Table 4.
Table 4.
Analysis of Symptoms in Ayurvedic terminology.
| Common symptoms | |||
| Ayurvedic name | Dosha status | Srotas | |
| Fever | Jwara | Pitta dominant Tridosha | |
| Dry cough |
Vata dominant Kasa |
Viloma Vata | Pranavaha Srotas |
| Tiredness | Related with Jwara | Vata dominant | Rasavaha Srotas |
| Less common symptoms | |||
| Aches/Pains | Angamarda | Vata dominant | |
| Sore throat | Galadhwnasa | Kapha, (and Rakta vitiation) | Pranavaha Srotas |
| Rhinorrhea | Pratishyay | Vata, Kapha | Pranavaha Srotas |
| Conjunctivitis | Netrabhishyanda | Kapha dominant triDosha | Majja vaha Srotas |
| Headache | Shirashoola | Kapha dominant (and Rakta vitiation) | Raktavaha Srotas |
| Diarrhoea | Atisara | Vata dominant Tridosha | Purishavaha Srotas |
| Loss of taste | Aroochi | Kapha, Pitta, Vata | Annavaha Srotas |
| Loss of smell | Anosmia | Vata | Pranavaha Srotas |
| Discoloration of fingers | Araktatata, Karshnya | Pitta (and Rakta vitiation) | Raktavaha Srotas |
| Serious symptoms | |||
| Difficulty breathing or shortness of breath | Shwasa | Vata- Kapha and Pitta as Shwasa is originated from Amashaya | Pranavaha Srotas, Marma |
| Chest pain or pressure | Ura Shoola | Vata dominant | Pranavaha Srotas, Marma |
| Loss of speech or movement | Vakgraha, Vatavyadhi | Vata dominant | Marma involvement |
Thus there are variety of symptoms showing involvement of Pranavaha, Rasavaha, Raktavaha and Majjavaha Srotas and Marma involvement. Symptoms are from Jwara, Shwasa, Pratishyay, Vatavyadhi, HrudRoga, TriMarma chapters again implying COVID-19 as multi-systemic disease.
4.3. Samprapti
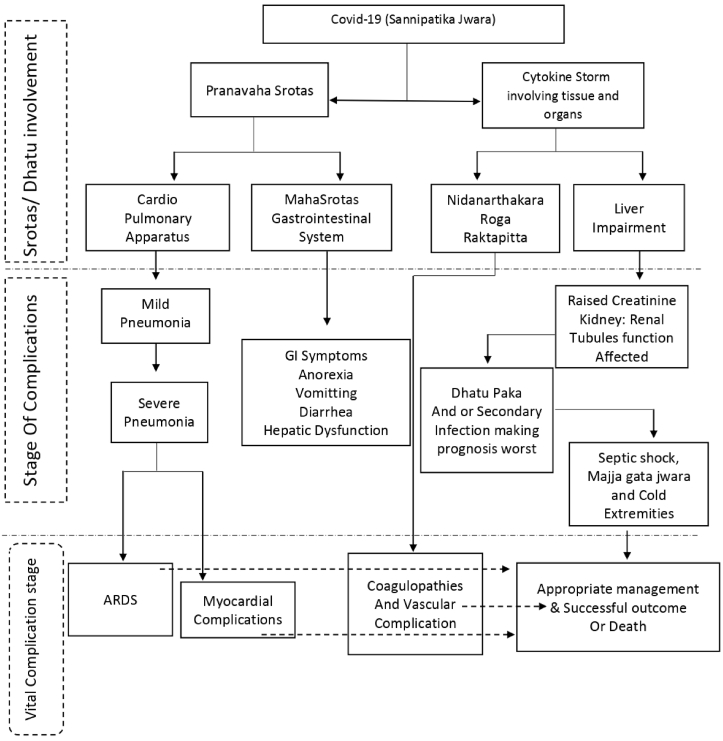
Initial pathogenesis is of Agantu (exogenous) Jwara and thus exhibit symptoms of Rasavaha Srotas i.e. tastelessness, headache, nausea, bodyache. This is followed by symptoms of Pranavaha and Raktavaha Srotas. Udana Dushti is evident as there is extreme loss of Bala i.e. deterioration of immune response, speech related symptoms in few. Raktavaha Srotodusthti is also evident from coagulopathies and extremity discolorations. Fatal complications are possible because ‘Prana’ (vitality or oxygen in this context) follows ‘Rakta’ (blood). In Ayurveda embryological view point Fuffusa (lungs) are made up of Rakta only. In context with respiratory mechanism Ayurveda considers the cardiopulmonary unit as a whole without differentiating heart and lungs. Mahasrotas (gastrointestinal tract) is also associated with Pranavaha Srotas as moolasthana. The pathogenesis later involves heart and kidney which are considered as third ‘Roga marga’ (disease pathway). In Ayurveda, hematuria is seen as associated symptom under Kasa Roga (Many Bronchial conditions) indicating involvement of urinary system as complication of respiratory pathologies. Pathogenesis worsens and complicates in ARDS (if there is kha-vaigunya i.e. susceptibility in lungs), or involves Heart or Kidney (according to kha-vaigunya). Interestingly Hiccup, dyspnea, cough and complications in vital organs are symptoms when fever pathogenesis invades Majja Dhatu according to Charaka and Sushruta [8,41]. Thus the later stage of COVID-19 with aggravated immune response indicates invasion of fever in Dhatu hierarchy (Fig. 3).
Fig. 3.
Stage wise disease progression in Covid-19 integrated approach.
5. Ayurvedic host centric approach in COVID-19 and remarks
The ‘Germ theory’ received more importance and was followed by development of Medical Microbiology and anti-microbial medicines in last century. With these advances infectious diseases were treated far well. So far as Host-Germ approach is concerned ‘virulence factor theory’ was later followed by concept of ‘Damage response framework’. DRF is an approach for incorporation of range of host responses to microbes with a parabolic curve in which host damage is plotted as a function of the host response. Importantly neither host nor microbial properties, are adequate to predict the outcome of host–microbe interaction because this outcome exhibits emergent properties [42].
In ayurvedic epistemology, microbe is viewed as nimitta karana (instrumental cause), contact of microbe with receptors as asamavayee karana (non-intimate cause) and host internal milieu as samavayee karana (intimate cause). As reviewed earlier the dynamic status of Dosha, Dhatu, mala and Agni the physiological elements of internal milieu are important in fate of exogenous and pathogenic diseases like COVID-19. The disease presentation is a dynamic phenomenon. Bala (body strength), Agni (digestive power) and Pradnya (mental ability) are as markers for prognosis, and Charaka has recommended continuous assessment of these three [43]. Thus it is host internal milieu in totality that is important for the immune response and prognosis.
Bala is often considered as body strength but is inclusive of various activities such as immunomodulator, bulk promoting, nutritional etc. [44] Pathophysiology and Immune responses in COVID-19 are important to be discussed in Ayurveda perspectives. Immunity is popularly imitated as ‘Vyadhikshmatwa’ in Ayurveda which is an incomplete translation. Prana/vitality is an important consideration. Rakta (Blood), Shukra (Reproductive tissues and Reproductive hormones) and Ojus (Quintessence of the seven body tissues) are the body tissues responsible for immune functions and appropriate immune responses. In fact it is not only immunity but a holistic network of Bala, Agni, Dosha, DhatuBala, Vaya and many more factors that decide the immune responses and fate of disease progression.
Pathophysiology of COVID-19 is primarily that of Respiratory system. Gastrointestinal, cardiac, renal, neural and coagulative complications follow. Pranavaha Srotas (Cardiopulmonary apparatus), MahaSrotas (Gastrointestinal tract) with Agni and Raktavaha Srotas (Blood and liver) are vitiated. Earlier presentation of COVID-19 is Vata-Kapha dominant whereas later stage of cytokine storm is Vata-Pitta dominant. Rakta (Blood) is most important Dhatu because lung alveolar tissues are made from Rakta only, coagulopathies are related with Rakta and immune responses too are also associated with Rakta Dhatu. COVID- 19 affects Pneumocytes type II which are precursor for Type I pneumocytes. Thus reproductive/tissue repairing mechanism of body is another important factor. This reproductive ability is associated with Shukra Dhatu. Ojus is next important body tissue as vital organs are affected in COVID-19. Thus Prana- Rakta- Shukra-Ojus is the pathophysiological quadrant in Ayurvedic perspective of COVID-19.
This proposed integrative understanding of Pathophysiology and holistic quadrant of Prana-Rakta-Shukra-Ojus can give novel leads for Preventive and Therapeutic approaches for COVID-19. Here we propose Novel approaches (Preventive and Therapeutic) based on this integrative understanding. They are summarized in Table 5.
Table 5.
Contemporary and Novel approaches (Preventive and Therapeutic) based on. Ayurvedic Pathophysiology of COVID-19.
| Pathogen centric approaches | Host centric approaches | Rationale |
|---|---|---|
| Contemporary approaches | ||
| Hygiene, Sanitization, Physical Distancing and other measures to avoid possibility of infection. | 7–8 H of sleep. Vitamin C, D3 and other supplements. Yoga and Respiratory Exercises. Interventions of Pulmonary Function improving agents | Evidences of immunomodulatory mechanisms of exercise, micronutrients and sleep |
|
Ayurveda Immunomodulator Herbs for minimizing virus replication and to arrest Cytokine syndrome. |
Evidences of Ayurveda immunomodulatory herbs/formulations mechanisms in biomedical terminology |
|
| Proposed Novel Approaches based on Host centric Approach and Ayurveda Pathophysiology of COVID-19 | ||
| Nasya, Gandusha can be local measures for care of pathogen entry points. | Conservation of Agni-Bala & maintenance of Agni (Digestive and metabolic equilibrium). | As MahaSrotas is associated with Pranavaha Srotas as moolasthana |
| Attainment of ‘Rakta–Pitta-Prana’ homeostasis with specific dietary, lifestyle modifications and therapeutic interventions. | According to Ayurveda Physiology Prana (not mere oxygen but vitality) follows Rakta and both are interdependent [8]. The Inflammatory Responses, Sepsis as well as Coagulopathy are result of Rakta and Pitta vitiation |
|
| Protection of Marma (Vital organs, the dedicated sites of Prana) with specific dietary, lifestyle modifications and interventions ‘Prana Kamiya Rasayana’ (Rasayana medicines particularly for vitals). Basti (Medicated enema) and Other relevant measures for protection of Heart, Brain and kidney from relevant chapters like Visha Chikitsa [8]. | Cytokine storm results in Inflammation and even necrotic changes in vital organs [45]. Basti is recommended as best measure for protection of vital organs [8]. |
|
| Ayurveda Immunomodulator Herbs for arresting viral load in different organs. This can be decided (from variety of Rasayana Herbs having efficacy on different systems and Organs) on basis of involvement of Organs and Tissues in the patient. | ||
Last few decades there is a good amount of research on virus–host interactions, particularly with approach of systems biology. Virus-host systems biology can make predictions on host responses and dynamic interactions between viruses and hosts by computational modelling. It is interesting to note that modelling are expected to be done at different levels of abstraction like genes, proteins, cells, and organisms [46]. Ayurvedic foundational framework of ‘Dosha-Dhatu-Mala-Agni-Srotas’ can serve as a model for these proposed studies. Ayurvedic foundational concepts have great potential and hence such studies can indeed make paradigm shift. Conservation of Agni-Bala and homeostasis of Prana-Rakta-Shukra-Ojus quadrant can be best host centric approach to improve clinical outcomes in COVID-19.
Source(s) of funding
None.
Conflicts of interest
None.
Acknowledgement
Authors are thankful to Dr Supriya Bhalerao & Prof Asmita Wele for inputs on scientific writing.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Rastogi S., Pandey D.N., Singh R.H. COVID-19 pandemic: a pragmatic plan for ayurveda intervention. J Ayurveda Integr Med. 2020 doi: 10.1016/j.jaim.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luke D.A., Stamatakis K.A. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Publ Health. 2012;33:357–376. doi: 10.1146/annurev-publhealth-031210-101222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhushan Patwardhan, Preeti Chavan-Gautam, Manish Gautam, girish Tillu, Chopra Arvind, Sunil Gairola, et al. Ayurveda rasayana in prophylaxis of Covid 19. Curr Sci. 2020;118:1158–1160. [Google Scholar]
- 4.Tillu G., Chaturvedi S., Chopra A., Patwardhan B. Public health approach of ayurveda and Yoga for COVID-19 prophylaxis. J Altern Compl Med. 2020;26:360–364. doi: 10.1089/acm.2020.0129. [DOI] [PubMed] [Google Scholar]
- 5.Gousseff M., Penot P., Gallay L., et al. Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound? J Infect. 2020;81(5):816–846. doi: 10.1016/j.jinf.2020.06.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patwardhan B. Bridging Ayurveda with evidence-based scientific approaches in medicine. EPMA J. 2014;5:19. doi: 10.1186/1878-5085-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ram Manohar P. Accounts of pathogenic organisms in the early texts of ayurveda. Indian J Hist Sci. 2012;47:545–559. [Google Scholar]
- 8.Jadhavji T., editor. Charaka Samhita by Agnivesha. 1st ed. Chaukhambha Orientalia; Varanasi: 2007. [Google Scholar]
- 9.Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol. 2020;7 doi: 10.1146/annurev-virology-012420-022445. annurev-virology. [DOI] [PubMed] [Google Scholar]
- 10.Garbino J., Crespo S., Aubert J.-D., Rochat T., Ninet B., Deffernez C., et al. A prospective hospital-based study of the clinical Impact of non–severe acute respiratory syndrome (Non-SARS)–Related human coronavirus infection. Clin Infect Dis. 2006;43:1009–1015. doi: 10.1086/507898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trikamji J., editor. 1 st. Choukhamba Surbharati Prakashan; Varanasi: 2007. (Charaka Samhita of Agnivesa). [Google Scholar]
- 12.Bahl P., Doolan C., de Silva C., Chughtai A.A., Bourouiba L., MacIntyre C.R. Airborne or droplet precautions for health Workers treating coronavirus disease 2019? J Infect Dis. 2020 doi: 10.1093/infdis/jiaa189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.P R. No Title https://www.amrita.edu/news/amrita-ayurveda-research-director-writes-epidemics-ayurveda n.d.
- 14.Sims A.C., Baric R.S., Yount B., Burkett S.E., Collins P.L., Pickles R.J. Severe acute respiratory syndrome coronavirus infection of human ciliated airway Epithelia: role of ciliated cells in viral Spread in the conducting airways of the lungs. J Virol. 2005;79:15511–15524. doi: 10.1128/JVI.79.24.15511-15524.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verdecchia P., Cavallini C., Spanevello A., Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur J Intern Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iwata-Yoshikawa N., Okamura T., Shimizu Y., Hasegawa H., Takeda M., Nagata N. TMPRSS2 contributes to virus Spread and Immunopathology in the airways of murine models after coronavirus infection. J Virol. 2019;93 doi: 10.1128/JVI.01815-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong C.K., Lam C.W.K., Wu A.K.L., Ip W.K., Lee N.L.S., Chan I.H.S., et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Y., Shen C., Li J., Yuan J., Wei J., Huang F., et al. Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19. J Allergy Clin Immunol. 2020;146:119–127. doi: 10.1016/j.jaci.2020.04.027. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qian Z., Travanty E.A., Oko L., Edeen K., Berglund A., Wang J., et al. Innate immune response of human alveolar type II cells infected with severe acute respiratory syndrome–coronavirus. Am J Respir Cell Mol Biol. 2013;48:742–748. doi: 10.1165/rcmb.2012-0339OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tian S., Xiong Y., Liu H., Niu L., Guo J., Liao M., et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tse G.M.-K. Pulmonary pathological features in coronavirus associated severe acute respiratory syndrome (SARS) J Clin Pathol. 2004;57:260–265. doi: 10.1136/jcp.2003.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trikamji J., editor. Charaka Samhita of Agnivesa. 1 st. Chaukhmba Surbharati Prakashana; Varanasi: 2014. [Google Scholar]
- 25.Misra B.S., editor. 5th ed. Vol. 2. Chowkhambha Sanskrit series; Banaras: 2001. (Bhavpraksh of Bhavmisra). [Google Scholar]
- 26.Trikamji J., editor. Charaka Samhita. 1st ed. Chaukhambha Orientalia; Varanasi: 2007. [Google Scholar]
- 27.Hari P., editor. AshtangaHridaya (with the commentaries “SarvangaSundara” of Arunadatta and “ayurveda rasayana” of Hemadri) 1st ed. ChaukhmbaSurbharatiPrakashana; Varanasi: 2002. [Google Scholar]
- 28.Panja A., Chaudhuri S., Chattopadhyaya A. A comprehensive outlook of Sannipata. AYU (An Int Q J Res Ayurveda) 2011;32:154. doi: 10.4103/0974-8520.92541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Temgoua M.N., Endomba F.T., Nkeck J.R., Kenfack G.U., Tochie J.N., Essouma M. Coronavirus disease 2019 (COVID-19) as a multi-systemic disease and its Impact in low- and middle-income Countries (LMICs) SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00417-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henry B.M., de Oliveira M.H.S., Benoit J., Lippi G. Gastrointestinal symptoms associated with severity of coronavirus disease 2019 (COVID-19): a pooled analysis. Intern Emerg Med. 2020 doi: 10.1007/s11739-020-02329-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu P.P., Blet A., Smyth D., Li H. The science underlying COVID-19. Circulation. 2020;142:68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 34.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L., et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Su H., Yang M., Wan C., Yi L.-X., Tang F., Zhu H.-Y., et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98:219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang C., Shi L., Wang F.-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seymour C.W., Kennedy J.N., Wang S., Chang C.-C.H., Elliott C.F., Xu Z., et al. Derivation, validation, and potential treatment implications of novel clinical Phenotypes for sepsis. J Am Med Assoc. 2019;321:2003. doi: 10.1001/jama.2019.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mamidi P. Sama Sannipata jwara- sepsis, SIRS, MODS, septic shock and delirium. Int J Complement Altern Med. 2017;8 doi: 10.15406/ijcam.2017.08.00257. [DOI] [Google Scholar]
- 41.Trikamji J., “kavyatirtha” N ram A., editors. Sushruta Samhita. 4th ed. Chaukhambha Orientalia; Varanasi: 1980. [Google Scholar]
- 42.Casadevall A., Pirofski L. What is a host? Incorporating the Microbiota into the damage-response framework: table 1. Infect Immun. 2015;83:2–7. doi: 10.1128/IAI.02627-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jadhavji T., editor. Charaka Samhita. 1st ed. Chaukhambha Orientalia; Varanasi: 2007. [Google Scholar]
- 44.Mahesh T.S., Shreevidya M. A review on balya action mentioned in Ayurveda. J Ayurveda Integr Med. 2014;5:80. doi: 10.4103/0975-9476.133796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maisch B. SARS-CoV-2 as potential cause of cardiac inflammation and heart failure. Is it the virus, hyperinflammation, or MODS? Herz. 2020;45:321–322. doi: 10.1007/s00059-020-04925-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peng X., Chan E.Y., Li Y., Diamond D.L., Korth M.J., Katze M.G. Virus–host interactions: from systems biology to translational research. Curr Opin Microbiol. 2009;12:432–438. doi: 10.1016/j.mib.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]