Abstract
Background
Coronavirus Disease 2019 (COVID-19) is a disease that presents with acute respiratory symptoms that are well documented and sequelae that are yet to be fully understood.
Case Report
We present the case of a 51-year old woman, recently diagnosed with COVID-19, who presented with symptoms including chest pain, palpitations, difficulty swallowing, and anterior neck discomfort. We ultimately diagnosed her with COVID-19-induced thyroiditis and discharged her on propranolol and nonsteroidal anti-inflammatory medication.
Why Should an Emergency Physician Be Aware of This?
Thyroiditis can present with symptoms similar to other etiologies like pulmonary embolism. We discuss the process of evaluating and treating thyroiditis. We further discuss the risk of administering iodinated contrast media that could further exacerbate thyroid dysfunction.
Keywords: SARS-CoV-2, viral thyroiditis, COVID-19, coronavirus disease 2019
Introduction
Coronavirus Disease 2019 (COVID-19) is a respiratory disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first identified in Wuhan, China in late 2019 (1). It can present with mild symptoms like fever, cough, loss of taste and smell, or more severe symptoms including dyspnea and acute respiratory distress syndrome. Although presenting symptoms are well documented, clinicians continue to uncover sequelae. In addition to respiratory disease, some complications include hypercoagulability with venous thromboembolism, neurologic disease including stroke, and liver disease, which can include hepatic failure, cirrhosis, and encephalopathy (2, 3, 4).
Thyroiditis is an inflammatory condition leading to hyperthyroidism, with acute inflammation of the gland, causing neck pain, tremors, palpitations, dyspnea, insomnia, and anxiety. Unfortunately, these symptoms have a wide differential diagnosis among emergency department (ED) patients, which includes pulmonary embolism, dysrhythmia, myocardial ischemia, electrolyte derangements, and acute infection. Known causes of thyroiditis include autoimmune dysfunction, medications such as amiodarone or lithium, and viral infection. As cases of SARS-CoV-2 continue to rise, recognizing COVID-19 as a cause of thyroiditis can help guide ED work-up and management of these patients.
Case Report
The patient was a 51-year old woman with a past medical history of type 2 diabetes, hypertension, and hyperlipidemia who had been diagnosed with COVID-19 23 days prior. She presented to our ED reporting palpitations, chest pain, and worsening shortness of breath for 3 days. The progressing shortness of breath concerned her the most, and she had never made a full recovery from her COVID-19 diagnosis. Eight days after her COVID-19 diagnosis, she had begun having some additional symptoms. She reported having intermittent chills, occasional tremor, and intermittent fevers. Additionally, she endorsed difficulty performing simple tasks at home such as chopping vegetables for approximately 5 min prior to having to sit down for approximately 20 min to catch her breath. She continued to have a cough with some productive sputum. She further reported difficulty swallowing, stating that she felt something was twisted around at the back of her throat and in her neck, particularly at the left anterior aspect.
Her initial vital signs revealed an afebrile temperature of 36.8°C; a tachycardic heart rate of 117 beats/min; mild tachypnea, with a respiratory rate of 20 breaths/min, a slightly elevated blood pressure of 149/84 mm Hg, and a normal oxygen saturation of 97%. Physical examination revealed a distressed and ill woman appearing her stated age. She appeared mildly dehydrated, with dry mucous membranes and mild posterior pharyngeal erythema. Her cardiac examination revealed tachycardia but was otherwise normal. Her respiratory examination revealed tachypnea, mild respiratory distress, and mild increased work of breathing, with otherwise normal breath sounds. Her abdominal examination was normal, as were her skin, neurological, and psychiatric examinations. Her anterior neck was severely tender to palpation, worst on the left anterior aspect, with no thyroid enlargement noted. No skin changes overlay the anterior neck.
Given the continued and, in fact, worsening symptoms after her recent COVID-19 diagnosis, our concerns for worsening COVID-19 pneumonia, thyroiditis, and pulmonary embolism (PE), a known complication of COVID-19, were significant and shaped the initial work-up. A cardiac etiology such as viral myocarditis and acute coronary syndrome were also included in our differential diagnosis. Given our high suspicion for PE, we ordered a computed tomography (CT) angiogram of the chest as well as screening laboratory tests, including a comprehensive metabolic panel, complete blood count, venous blood gas with lactate, and troponin. An electrocardiogram had already been obtained in the triage area and showed sinus tachycardia at a rate of 106 beats/min without signs of ischemia. Because she would be going to the CT scanner and receiving a contrast study already, we reasoned that obtaining a CT of the soft tissue of the neck with contrast would be a good test to evaluate her neck pain and dysphagia, which was concerning for thyroiditis or a deeper space infection such as a retropharyngeal abscess or lymphadenitis, although neither was, to our knowledge, a condition associated with COVID-19.
The initial laboratory results were remarkable for a minimal leukocytosis of 10.95 k/uL (5–10 k/uL) with a normal differential, and a new, mild anemia with a hemoglobin of 9.9 g/dL (12–15.5 g/dL), which was down from 12.3 g/dL 2.5 months prior. She denied any hematemesis, hematochezia, melena, or heavy menstrual periods. Her CT angiogram of the chest was negative for PE and otherwise normal. There were none of the typical COVID-19 findings.
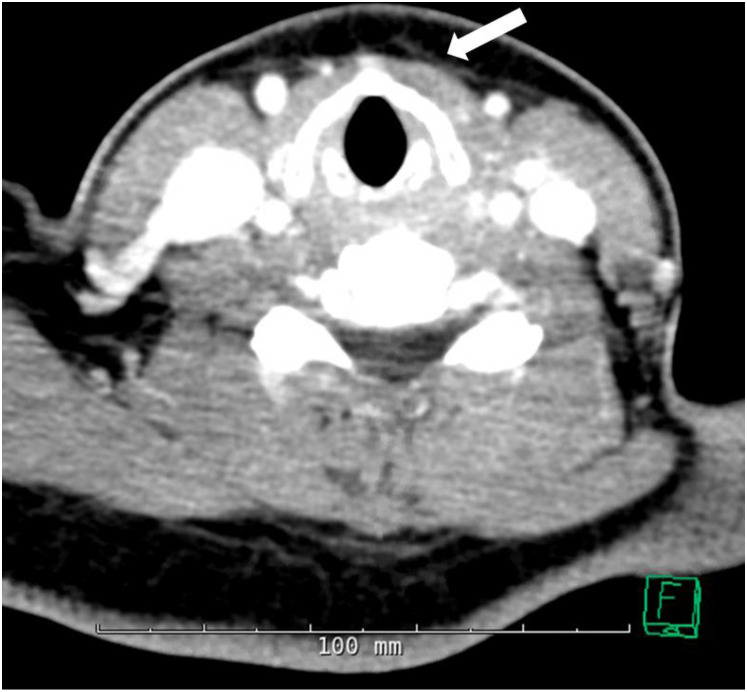
Her CT of the soft tissue of the neck, however, was revealing and concerning for thyroiditis (Figure 1 ). The radiologist report found “slightly heterogeneous attenuation/enhancement of the thyroid gland with mild perithyroidal edema.” In addition, there were a “few mildly enlarged right supraclavicular lymph nodes, [the] largest measuring about 1.5 × 2 cm.” These enlarged lymph nodes, however, were on the contralateral side of the neck from where the patient reported pain, implying that the etiology of her pain was not due to lymphadenitis. Given the lack of other etiology, we felt that her left-sided throat pain was likely secondary to thyroiditis. Given the CT finding, we ordered a thyroid-stimulating hormone (TSH) level, which resulted low at 0.00004 mU/mL (0.4–4.0 mU/mL), and a free thyroxine level, which resulted high at 1.90 ng/dL (0.8–1.8 ng/dL), although not as high as we expected given her clinical picture. However, in conjunction with the low TSH, this prompted a consultation with our endocrinologist on call who recommended propranolol and a nonsteroidal anti-inflammatory drug (NSAID) such as ibuprofen for her pain and for the anti-inflammatory benefit. They did not recommend any corticosteroid treatment. They additionally requested a thyroid-stimulating immunoglobulin to evaluate for Graves disease and none was detected. Additionally, the endocrinologist on call recommended close return precautions given that she had received an iodinated contrast bolus for her CT scans. We prescribed propranolol 20 mg twice daily for 2 weeks and recommended close outpatient follow-up with an endocrinologist.
Figure 1.
Computed tomography of the soft tissue of the neck, with arrow depicting mild perithyroidal edema.
Subsequent to her ED visit, she had no worsening of her symptoms. Seventeen days after her ED visit, repeat laboratory testing showed immeasurably low TSH, a normal free thyroxine (T4) level of 1.50 ng/dL, and an elevated total triiodothyronine (T3) level of 203 ng/dL (75–195 ng/dL). Her endocrinologist planned to repeat thyroid function testing but did not prescribe any further propranolol or other medication.
Discussion
As COVID-19 continues to spread, emergency physicians should consider viral thyroiditis in the differential diagnosis of patients presenting to the ED with palpitations or shortness of breath with recent COVID-19 infections. Viral infections, in addition to multiple other etiologies, are a known cause of thyroiditis and thyrotoxicosis. Subacute thyroiditis can occur either during an active viral infection or during a postviral inflammatory process, 2–8 weeks after an infection. Many viruses have been associated with thyroiditis, including coxsackievirus, mumps, measles, rubella, adenovirus, influenza, and parvovirus B19 (5). Case reports describing thyroiditis after COVID-19 infection are just now emerging. There is evidence that COVID-19 infection can alter the thyroid-pituitary axis, resulting in subacute thyroiditis in critically ill patients in the intensive care unit (6). Meanwhile, Brancatella et al. (7) described four women in Italy that developed subacute thyroiditis after COVID-19 infection. All four women were asymptomatic after 6 weeks, with two women having hypothyroidism, whereas the other two were euthymic. Similarly, Mattar et al. describe the case of a 34-year-old man who they diagnosed with COVID-19 thyroiditis and who made a full recovery after a course of corticosteroids (8). The growing number of case reports seems to demonstrate that the SARS-CoV-2 virus acts similarly to other viruses causing thyroiditis.
Diagnosing thyroiditis is particularly challenging in the ED, as it presents with vague symptoms such as low-grade fever, palpitations, fatigue, myalgias, pharyngitis, and may also include a swollen and painful neck, with up to 50% of patients presenting with thyrotoxicosis (9). Similarly, COVID-19 often presents with fever, fatigue, and myalgias in addition to respiratory symptoms, with sequelae that may include myocardial inflammation, ventricular abnormalities, stroke, pulmonary embolism, acute kidney injury, sleep irregularities, changes in mood, depression, and anxiety (10). Due to the similar overlapping symptom presentation of both COVID-19 and thyroiditis, clinicians should consider both when evaluating symptomatic patients.
In an ED setting, thyrotoxicosis, the clinical syndrome secondary to increased thyroid hormones regardless of etiology, is diagnosed using the patient's clinical presentation as well as a low TSH level. Therefore, if the emergency physician suspects thyrotoxicosis, the initial workup should include basic laboratory testing as well as serum TSH levels with subsequent free T4 if the TSH level is abnormal. Laboratory values guide management (Table 1 ) (11). Typically, thyrotoxicosis requires additional outpatient workup once the patient is stable for discharge and is started on symptomatic treatment. Further outpatient testing incorporates a combination of serum testing for TSH and T3/T4 levels, thyroid antibodies, thyroid duplex ultrasound studies, and a radioactive iodine uptake scan to help delineate the underlying cause of the thyrotoxicosis.
Table 1.
Thyroid Function Test Interpretation (11).
| TSH | Free T4 | Free T3 | Condition |
|---|---|---|---|
| Normal | Normal | Normal | Normal |
| Low | High | High | Primary hyperthyroidism |
| Low | Normal | Normal | Subclinical hyperthyroidism |
| Low | Normal | High | T3 toxicosis |
| Low | High | Normal | Thyroiditis |
| Low | Low | Low | Euthyroid or central hypothyroidism |
| High | Normal | Normal | Subclinical hypothyroidism |
| High | Low | Low | Primary hypothyroidism |
| High | High | High | TSH-producing pituitary adenoma |
TSH = thyroid-stimulating hormone.
Furthermore, emergency physicians should note the risk of further exacerbating the thyrotoxicosis by using iodinated contrast as part of the imaging modality of choice. The normal acute response to excess iodine by the thyroid gland, known as the Wolff-Chaikov effect, was first described in 1948 when rats exposed to high iodine levels transiently decreased thyroid hormone synthesis (12). If this effect is impaired, iodine-induced hyperthyroidism, known as the Jöd-Basedow phenomenon, can result (13). A single dose of iodinated contrast has been shown to increase the risk of hyperthyroidism by about 2–2.5 times in a nested case-controlled study over 20 years at two tertiary care facilities (14,15).
Treatment for thyroiditis focuses on symptom control. After ensuring the patient is hemodynamically stable and clinically not in thyroid storm, the ED treatment for thyroiditis is twofold: reduction of pain and inflammation, and, if present, thyrotoxicosis symptom relief. Emergency physicians can treat pain and inflammation with an NSAID such as naproxen 500 mg, or a corticosteroid such as prednisone 40 mg (16). For symptoms of hyperthyroidism, beta-blockers, especially propranolol 0.5–1 mg i.v. or 40–80 mg by mouth every 6 h, are the first choice to inhibit the adrenergic effects of excessive thyroid hormones. To inhibit further thyroid hormone production, thionamides like methimazole 20 mg by mouth every 6 h or propylthiouracil 500–1000 mg by mouth as a loading dose followed by 250 mg every 4 h can be used, although the former is contraindicated in pregnancy due to its teratogenic effects.
The prognosis of isolated subacute thyroiditis is generally very good. Most patients with classic painful subacute thyroiditis can expect a complete resolution of pain within 1–3 months, with 95% experiencing recovery of normal thyroid function within 12–18 months (17). If the SARS-CoV-2 virus behaves similarly to other known viruses causing thyroiditis, then we expect COVID-19-induced thyroiditis to have a similar prognosis. Time will allow clinicians to better describe other sequelae from COVID-19-induced thyroiditis, but the treatment for thyrotoxicosis in the ED setting should not change. Emergency physicians can discharge patients whose thyroiditis symptoms improve with treatment with strict return precautions to follow up with their primary care physician or endocrinologist for repeat thyroid function testing.
Why Should an Emergency Physician Be Aware of This?
Emergency physicians should be aware of COVID-19-induced thyroiditis to expand their differential diagnosis beyond the well-recognized sequelae of COVID-19 to expeditiously diagnose COVID-19 thyroiditis and initiate treatment. In evaluating COVID-19 patients with hyperthyroidism symptoms, emergency physicians may order a CT scan with iodinated contrast to evaluate for pulmonary embolism, a known sequela of COVID-19. However, emergency physicians should be aware that the iodinated contrast could exacerbate the thyrotoxicosis further. Having a high suspicion of COVID-19-induced thyroiditis could change the emergency physician's process of evaluating the patient. Case reports, including our own, indicate that emergency physicians can manage COVID-19-induced thyroiditis similarly to other forms of thyroiditis.
References
- 1.Guan W.J., Ni Z., Hu Y., et al. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Long B., Brady W.J., Koyfman A., Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38:1504–1507. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poyiadji N., Shahin G., Noujaim D., et al. COVID-19–associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020;296:E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu L., Liu J., Lu M., et al. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020;40:998–1004. doi: 10.1111/liv.14435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desailloud R., Hober D. Viruses and thyroiditis: an update. Virol J. 2009;6:5. doi: 10.1186/1743-422X-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muller I., Cannavaro D., Dazzi D., et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020;8:739–741. doi: 10.1016/S2213-8587(20)30266-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brancatella A., Ricci D., Cappellani D., et al. Is subacute thyroiditis an underestimated manifestation of SARS-CoV-2 infection? Insights from a case series. J Clin Endocrinol Metab. 2020;105:dgaa537. doi: 10.1210/clinem/dgaa537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattar S.A.M., Koh S.J.Q., Chandran S.R., et al. Subacute thyroiditis associated with COVID-19. BMJ Case Rep. 2020;13:237336. doi: 10.1136/bcr-2020-237336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pearce E.N., Farwell A.P., Braverman L.E. Thyroiditis. N Engl J Med. 2003;348:2646–2655. doi: 10.1056/NEJMra021194. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Late sequelae of COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/late-sequelae.html Available at:
- 11.Koulouri O., Gurnell M. How to interpret thyroid function tests. Clin Med. 2013;13:282–286. doi: 10.7861/clinmedicine.13-3-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolff J., Chaikoff I.L. Plasma inorganic iodide, a chemical regulator of normal thyroid function. Endocrinology. 1948;42:468–471. doi: 10.1210/endo-42-6-468. [DOI] [PubMed] [Google Scholar]
- 13.Coindet J. Nouvelles recherches sur les effets de l'iode, et sur les precautions a suivre dans le traitement de goitre par le nouveau remede. Bibl Univ Sci Belle-Lettres Arts. 1821;16:140. [in French] [Google Scholar]
- 14.Rhee C.M. Association between iodinated contrast media exposure and incident hyperthyroidism and hypothyroidism. Arch Intern Med. 2012;172:153. doi: 10.1001/archinternmed.2011.677. [DOI] [PubMed] [Google Scholar]
- 15.Lee S.Y., Rhee C.M., Leung A.M., et al. A review: radiographic iodinated contrast media-induced thyroid dysfunction. J Clin Endocrinol Metab. 2015;100:376–383. doi: 10.1210/jc.2014-3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto M., Saito S., Sakurada T., et al. Effect of prednisolone and salicylate on serum thyroglobulin level in patients with subacute thyroiditis. Clin Endocrinol. 1987;27:339–344. doi: 10.1111/j.1365-2265.1987.tb01160.x. [DOI] [PubMed] [Google Scholar]
- 17.American Thyroid Association Thyroiditis. https://www.thyroid.org/thyroiditis/ Available at: