Abstract
COVID-19 associated coagulopathy and mortality related to thrombotic complications have been suggested as biological mediators in racial disparities related to COVID-19. We studied the adjusted prevalence of acute ischemic stroke, pulmonary embolism, myocardial infarction, and deep venous thrombosis stratified by race in hospitalized patients in one New York City borough during the local COVID-19 surge. The multi-racial cohort included 4299 patients hospitalized with COVID-19, 9% of whom were white, 40% black, 41% Hispanic and 10% Asian or other. We found a 6.1% prevalence of composite thrombotic events. There were no significant race-specific differences in thrombotic events when adjusting for basic demographics, socioeconomic factors, medical comorbidities or biomarkers using a stepwise regression model. We therefore found no evidence that the racial disparities related to COVID-19, and specifically thrombotic complications, are caused by biological differences in race.
Abbreviations: COVID-19, coronavirus disease 2019; NYC, New York City; AIS, acute ischemic stroke; PE, pulmonary embolism; MI, myocardial infarction; DVT, deep vein thrombosis; AA, African American; NHW, non-Hispanic white; SES, socioeconomic status
Keywords: COVID-19, Racial disparities, Thrombosis, Stroke
1. Introduction
Explosive community spread and a disparate effect on the most vulnerable members of society by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has exposed long-standing racial/ethnic health inequities in the United States [1]. African Americans (AA) and Hispanics have been disproportionately affected by the virus, with higher rates of infection, hospitalization and death [2,3]. COVID-19 associated coagulopathy and mortality related to thrombotic complications have been suggested as plausible biological mediators in racial disparities related to COVID-19 [[4], [5], [6]]. Better understanding of the social versus biological mediators of race/ethnic disparities in COVID-19 can help guide future prevention and treatment strategies. We report the adjusted incidence of acute ischemic stroke (AIS), pulmonary embolism (PE), myocardial infarction (MI), and deep vein thrombosis (DVT) stratified by race in hospitalized patients in one New York City (NYC) borough during the local COVID-19 surge.
2. Methods
2.1. Study population and clinical features
We performed a retrospective analysis of patients admitted to three Montefiore Health System hospitals in the Bronx, New York, between March 1, 2020 and May 7th, 2020 with COVID-19. Emergency room visits not requiring admission were excluded. Baseline characteristics, medical comorbidities, medications and interventions, final disposition, and laboratory markers including SARS-CoV-2 real-time reverse transcriptase–polymerase chain reaction (RT-PCR) results (nasopharyngeal swab using FDA-approved assays), were systematically extracted from the electronic medical record using automated data extraction tools [7]. Median income and population density (population divided by land mass) were obtained by zip code using publicly available US Census Bureau data for years 2014–2018 and 2010 respectively (census.gov). We created concentrated poverty index (population density divided by mean income) to assess the unique interplay between housing density and poverty, a measure thought to be related to viral spread. Socioeconomic status (SES) was defined using a composite of median income, wealth (rental income and housing value), and education (percent graduated high school, percent with college education, percent in professional occupation), assessed by address and measured as a deviation from the population in New York State, based on census block [7].
Thrombotic events including AIS, MI (type 1 or 2), PE, and DVT were screened using the International Classification of Diseases, Tenth Revision codes at any location and confirmed by manual chart review. All cases of AIS, PE and DVT required clinical suspicion and confirmatory imaging to be included. Cases without confirmatory imaging were excluded. For quality assurance, we performed a separate detailed review of a subsample of 10 cases of DVT and PE each, and found 8 proximal and 2 distal cases of DVT; and anatomical heterogeneity in PE with 2 saddle, 6 segmental and 2 subsegmental. All cases of AIS were adjudicated by a vascular neurologist. Anticoagulants included heparin drip, enoxaparin at therapeutic doses, and direct oral anticoagulants at any dose. This included apixaban 2.5 mg and 5 mg twice daily, which were recommended in our hospital system starting at the height of the local pandemic as thromboprophylaxis in patients with a d-dimer of ≤3 μg/ml or >3 μg/ml respectively. COVID-19 medications include azithromycin and hydroxychloroquine. Race/ethnicity was self-reported and defined as non-Hispanic white (NHW), African American (AA), Hispanic, Asian or other. Those with missing race/ethnicity were excluded.
2.2. Statistics
The primary outcomes were AIS, PE, DVT and MI. Continuous values were represented using mean ± standard deviation (SD), or median and interquartile range (IQR). Categorical variables were described using frequencies and proportions. Comparisons were performed using Student's t-test, the nonparametric Mann–Whitney test or χ2 tests as appropriate. No imputation was made for missing data. Candidate predictors with P < 0.05 in the univariate analysis were included in the stepwise multiple regression model as follows: Model 1 (unadjusted), Model 2 (adjusted for age and sex), Model 3 (adjusted for Model 2 + socio-economic status (SES)), Model 4 (adjusted for Model 3 + comorbidities), Model 5 (adjusted for Model 4 + biomarkers) and Model 6 (adjusted for Model 5 + medications/treatments). P-value < 0.05 was considered statistically significant for all analyses. Data were analyzed using IBM SPSS version 24. This study was approved by the Albert Einstein College of Medicine/Montefiore Medical Center Institutional Review Board.
3. Results
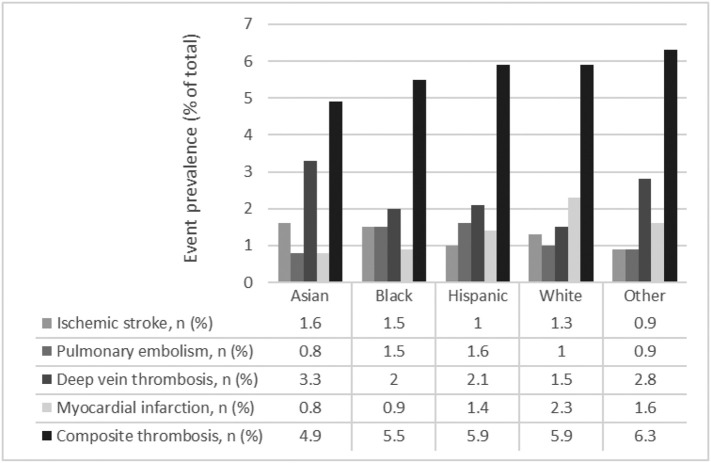
A total of 4299 patients, 391 NHW (9%), 1716 AA (40%), 1752 Hispanic (41%), 123 Asian (3%) and 317 other (7%), were hospitalized during the study period. Notably NHW patients were significantly older, had higher median income and SES, and were significantly more likely to live in communities with lower popoulation density compared to all other racial groups. There were no major differences in treatment with steroids and anticoagulants. There were significant differences in treatment with azithromycin and/or hydroxychloroquine, mechanical ventilation and a number of comorbidities and clinical variables (Table 1). There were 262 (6.1%, 95% CI 5.4–6.8%) total cases of thrombotic events, including 53 AIS (20%), 62 PE (24%), 91 DVT (35%) and 56 cases of MI (21%). There were no significant differences in composite thrombotic events by race in univariate or multivariate analysis (Model 3: demographics and SES; Model 5: adds comorbidities, biomarkers; Model 6: adds medications; see Fig. 1). In the fully adjusted model, composite thrombotic events were associated with diabetes (OR 2.25 [1.2–4.21], P = 0.011) and a D-dimer level >3 μg/ml (OR 3.09 [1.76–5.4] P < 0.001) (Supplemental material).
Table 1.
General characteristics.
| Variables | Asian (n = 123) |
Black (n = 1716) |
Hispanic (n = 1752) |
White (n = 391) |
Other (n = 317) |
P value |
|---|---|---|---|---|---|---|
| Age-years | ||||||
| <55 | 38 (30.9) | 453 (26.4) | 573 (32.7) | 58 (14.8) | 89 (28.1) | <0.001 |
| 55–65 | 38 (30.9) | 415 (24.2) | 378 (21.6) | 64 (16.4) | 89 (28.1) | |
| 65–75 | 21 (17.1) | 402 (23.4) | 364 (20.8) | 126 (32.2) | 76 (24) | |
| >75 | 26 (21.1) | 446 (26) | 437 (24.9) | 143 (36.6) | 63 (19.9) | |
| Female sex, n (%) | 49 (39.8) | 881 (51.3) | 790 (45.1) | 161 (41.2) | 125 (39.4) | <0.001 |
| Household income, k-US median (IQR) | 28.3 (21.7–29.3) | 26.8 (21.7–29.3) | 21.7 (17.9–28.3) | 29.3 (24.4–31.6) | 28.3 (21.7–31.1) | <0.001 |
| SES quartiles, n (%) | ||||||
| Quartile 1 | 12 (13) | 284(19.3) | 457 (33.2) | 39 (11.9) | 41 (16.9) | <0.001 |
| Quartile 2 | 33 (35.9) | 315 (21.4) | 483 (35.1) | 44 (13.4) | 56 (23) | |
| Quartile 3 | 29 (31.5) | 486 (32.9) | 239 (17.4) | 92 (28) | 67 (27.6) | |
| Quartile 4 | 18 (19.6) | 390 (26.4) | 198 (14.4) | 154 (46.8) | 79 (32.5) | |
| Population density-k, median (IQR) | 44.4 (29.9–52.1) | 35.9 (27.9–46.4) | 44.4 (29.9–65.3) | 29.9 (13–44.4) | 36.5 (25.1–52) | <0.001 |
| Poverty index, median (IQR) | 1 (0.57–1.01) | 0.63 (0.45–1.01) | 0.98 (0.57–1.75) | 0.45 (0.36–0.98) | 0.98 (0.45–1.01) | <0.001 |
| BMI, kg/m2, n (%) | ||||||
| 18–24.9 | 36 (35.3) | 416 (26.3) | 426 (26.8) | 122 (34.1) | 85 (29.5) | <0.001 |
| 25–29.9 | 42 (41.2) | 475 (30) | 529 (33.2) | 110 (30.7) | 106 (36.8) | |
| >30 | 24 (23.5) | 693 (43.8) | 636 (40) | 126 (35.2) | 106 (36.8) | |
| Smoking status, n (%) | ||||||
| Current | 4 (6.1) | 85 (7.9) | 70 (7) | 22 (9.2) | 3 (1.9) | 0.001 |
| Former | 10 (15.2) | 335 (31.1) | 321 (32.1) | 93 (38.8) | 47 (29) | |
| Never | 52 (78.8) | 658 (61) | 610 (60.9) | 125 (52.1) | 112 (69.1) | |
| Diabetes, n (%) | 25 (20.3) | 442 (25.8) | 340 (19.4) | 61 (15.6) | 61 (19.2) | <0.001 |
| Myocardial Infarction, n (%) | 8 (6.5) | 106 (6.2) | 141 (8) | 42 (10.7) | 15 (4.7) | 0.052 |
| Congestive heart failure, n (%) | 15 (12.2) | 338 (19.7) | 292 (16.7) | 76 (19.4) | 34 (10.7) | 0.004 |
| Cerebrovascular disease, n (%) | 23 (18.7) | 268 (15.6) | 214 (12.2) | 53 (13.6) | 37 (11.7) | 0.002 |
| Dementia, n (%) | 8 (6.5) | 219 (12.8) | 195 (11.1) | 62 (15.9) | 25 (7.9) | 0.002 |
| Chronic pulmonary disease, n (%) | 4 (3.3) | 26 (1.5) | 32 (1.8) | 4 (1) | 7 (2.2) | 0.569 |
| Renal disease, n (%) | 25 (20.3) | 519 (30.2) | 415 (23.7) | 80 (20.5) | 69 (21.8) | <0.001 |
| Hypertension, n (%) | 48 (39) | 638 (37.2) | 628 (35.8) | 168 (43) | 127 (40.1) | 0.010 |
| Oxygen saturation <94%, n (%) | 58 (47.9) | 566 (34.3) | 683 (40.4) | 156 (42.3) | 126 (40.5) | <0.001 |
| Temperature >38 °C, n (%) | 30 (24.8) | 325 (19.7) | 328 (19.5) | 62 (16.8) | 58 (18.6) | 0.404 |
| Troponin >0.1 ng/ml, n (%) | 9 (8.9) | 196 (12.9) | 152 (9.9) | 40 (11.4) | 31 (11.1) | 0.111 |
| Erythrocyte sedimentation rate (ESR) >60 mm/h, n (%) | 33 (71.7) | 265 (69.7) | 285 (67.2) | 50 (55.6) | 41 (59.4) | 0.065 |
| C-reactive protein >10 mg/l, n (%) | 63 (58.9) | 687 (48.2) | 766 (51.4) | 148 (46.4) | 118 (44) | 0.024 |
| D-dimer >3 μg/ml, n (%) | 25 (25) | 487 (36.6) | 414 (29.4) | 113 (36.5) | 70 (28.2) | <0.001 |
| Interleukin-6 >150 pg/ml, n (%) | 10 (18.2) | 89 (12.2) | 93 (11.3) | 24 (14) | 14 (9.7) | 0.442 |
| Hemoglobin <12 g/dl, n (%) | 44 (37.3) | 680 (40.6) | 546 (32) | 123 (32.3) | 109 (35.2) | <0.001 |
| Platelets-k per mm3 <100 k, n (%) | 4 (3.4) | 77 (4.6) | 75 (4.4) | 17 (4.5) | 11 (3.5) | 0.913 |
| White blood cells-k per mm3 >10,800, n (%) | 44 (37.3) | 675 (40.3) | 661 (38.8) | 156 (40.9) | 115 (37.1) | 0.710 |
| Fibrinogen >500 mg/dl, n (%) | 60 (75.9) | 726 (75) | 797 (77.5) | 138 (63) | 140 (76.5) | <0.001 |
| Ferritin >300 μg/l, n (%) | 79 (84.9) | 1002 (83.5) | 1018 (78.2) | 217 (78.9) | 192 (83.5) | 0.008 |
| Aspartate aminotransferase >40 U/l, n (%) | 64 (55.2) | 783 (48.1) | 809 (48.8) | 158 (42.8) | 157 (52) | 0.076 |
| Alanine aminotransferase >40 U/l, n (%) | 36 (31) | 443 (26.9) | 539 (32.3) | 88 (23.5) | 94 (30.8) | 0.001 |
| International normalized ratio (INR) >1.2, n (%) | 16 (14.2) | 300 (19.2) | 320 (20.1) | 96 (26.9) | 50 (17.1) | 0.004 |
| Partial thromboplastin time (PTT) >35 s, n (%) | 57 (53.8) | 490 (33.7) | 554 (38.1) | 118 (35.9) | 98 (36) | <0.001 |
| Creatinine >1.5 μmol/l, n (%) | 27 (22.9) | 710 (42.5) | 453 (26.6) | 106 (27.8) | 90 (28.9) | <0.001 |
| Procalcitonin >0.1 ng/ml, n (%) | 57 (65.5) | 681 (64.4) | 714 (59.5) | 138 (49.6) | 115 (58.7) | <0.001 |
| Sodium >145 mmol/l, n (%) | 9 (7.6) | 207 (12.4) | 129 (7.6) | 42 (11) | 23 (7.4) | <0.001 |
| LDH >280 U/l, n (%) | 84 (79.2) | 1191 (79.2) | 1151 (74.1) | 230 (69.1) | 219 (77.4) | <0.001 |
| Treatment & medication | ||||||
| Intubation, n (%) | 32 (26) | 260 (15.2) | 263 (15) | 53 (13.6) | 58 (18.3) | 0.008 |
| Anticoagulant, n (%) | 62 (50.4) | 830 (48.4) | 864 (49.3) | 184 (47.1) | 149 (47) | 0.870 |
| COVID-19 medication, n (%) | 90 (73.2) | 1423 (82.9) | 1425 (81.3) | 324 (82.9) | 249 (78.5) | 0.018 |
| Steroids, n (%) | 30 (24.4) | 293 (17.1) | 327 (18.7) | 67 (17.1) | 68 (21.5) | 0.116 |
Missing data: Median household income (n = 4), poverty index (n = 250), socio-economic status quartile (n = 821), BMI (n = 770), smoking status (n = 1886), oxygen saturation (n = 182), temperature (n = 160), troponin (n = 866), ESR (n = 3707), C-reactive protein (n = 1253), d-dimer (n = 1419), interleukin-6 (n = 2864), hemoglobin (n = 370), platelets (n = 370), white-blood cell count (n = 370), fibrinogen (n = 2351), ferritin (n = 1737), AST (n = 555), ALT (n = 493), INR (n = 761), PTT (n = 1136), creatinine (n = 378), procalcitonin (n = 2025), sodium (n = 386) and LDH (n = 1032).
Fig. 1.
Thrombotic event prevalence stratified by race.
P values: ischemic stroke 0.792, pulmonary embolism 0.784, deep vein thrombosis 0.724, myocardial infarction 0.264, composite events 0.967.
4. Discussion
Race/ethnic minorities have been hospitalized and are dying from COVID-19 at higher rates compared to NHWs, highlighting long standing health inequities rooted in structural racism and oppression of AA, Native American and Latinx populations on the local and national level [2,8,9]. To better understand possible mediators of the disparate effect of COVID-19-related mortality on race/ethnic minorities, we studied the prevalence of thrombotic events in patients treated in the Bronx, NY – a highly diverse borough with the highest incidence of COVID-19 in NYC [3]. While AAs and Hispanics were younger, more likely to be in the lowest quartile of SES and generally healthier, there were no differences in unadjusted rates of arterial and venous thrombosis. Adjusting for basic demographics, SES, comorbidities and clinical markers of disease severity did not yield any differences in composite thrombotic events when stratifying by race. Contrary to reports suggesting race-based biological differences in COVID-19 associated coagulopathy, we found no evidence of increased risk of arterial or venous thromboses in this large multi-racial cohort. Instead, we found significant differences in baseline demographic and socioeconomic characteristics between races, suggesting that community level factors drive differences in previously reported COVID-19-related racial disparities [10]. While only representative of local factors, these findings can inform future prevention and treatment strategies. This is one of the largest studies reporting specific outcomes related to race/ethnic and Covid-19 and is further strengthened by the large proportion of race/ethnic minorities, but was conducted solely in NYC, limiting generalizability. There are other important limitations having to do with the race/ethnic subgroups. While we did not see significant differences between race/ethnic subgroups, our cohort included only a small proportion of Asian patients making our findings related to this group limited and in need of further study. Another limitation is the likely undercount of thrombotic events in critically ill patients, given the limited ability to perform confirmatory studies. There is no reason to believe that this would lead to a differential misclassification. While prevalence of thrombotic events has varied across studies, we only included confirmed cases of AIS, PE, and DVT, likely yielding a conservative estimate.
In conclusion, we found no race-specific differences between the AA, Native American and Latinx populations on thrombotic complications in patients hospitalized with COVID-19. It is therefore unlikely that local racial disparities in COVID-19 are related to biological differences in thrombotic risk. Rather, more studies should focus on the effects of community-level healthcare inequities on race-specific outcomes in COVID-19.
The following is the supplementary data related to this article.
Stepwise regression model for composite thrombotic events.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank the entire Neurological Complications of COVID-19 research group for their invaluable involvement. We dedicate this work to the memory of the Montefiore associates who have lost their lives to COVID-19.
References
- 1.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price-Haywood E.G., et al. Hospitalization and mortality among black patients and white patients with Covid-19. N. Engl. J. Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wadhera R.K., Wadhera P., Gaba P., et al. Variation in COVID-19 hospitalizations and deaths across New York City Boroughs. JAMA. 2020;323(21):2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fogarty H., et al. COVID19 coagulopathy in Caucasian patients. Br. J. Haematol. 2020;189(6):1044–1049. doi: 10.1111/bjh.16749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramasamy R., et al. Molecular mechanisms for thrombosis risk in Black people: a role in excess mortality from COVID-19. Br. J. Haematol. 2020;190(2):e78–e80. doi: 10.1111/bjh.16869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellin E., et al. Democratizing information creation from health care data for quality improvement, research, and education-the Montefiore Medical Center Experience. Acad. Med. 2010;85(8):1362–1368. doi: 10.1097/ACM.0b013e3181df0f3b. [DOI] [PubMed] [Google Scholar]
- 8.Berkowitz S.A., Cené C.W., Chatterjee A. Covid-19 and health equity — time to think big. N. Engl. J. Med. 2020;383(12):e76. doi: 10.1056/NEJMp2021209. [DOI] [PubMed] [Google Scholar]
- 9.Evans M.K. Covid’s color line - infectious disease, inequity, and racial justice. N. Engl. J. Med. 2020;383(5):408–410. doi: 10.1056/NEJMp2019445. [DOI] [PubMed] [Google Scholar]
- 10.Boulware L.E. Race disparities in the COVID-19 pandemic-solutions lie in policy, not biology. JAMA Netw. Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.18696. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Stepwise regression model for composite thrombotic events.