Abstract
Background
Waiters working in different food and drinking establishments have a higher risk of contracting COVID-19 and transmitting the infection to others because they interact with many people. Most COVID-19 related studies in Ethiopia mainly focused on the general population, whereas, this study aimed to assess the knowledge of COVID-19 and preventive behaviors among waiters in Southwest Ethiopia.
Methods
A cross-sectional study was conducted from June 1 to June 15, 2020, among waiters working in food and drinking establishments found in Mizan-Aman, Jemu, and Masha towns in Southwest Ethiopia. A total of 422 waiters were selected using a simple random sampling technique, and the data were collected through face-to-face interviews using a structured questionnaire. The data were entered into Epi-data manager version 4.0.2 and analyzed using SPSS version 22. Multivariable binary logistic regression analysis was carried out to identify predictors of good preventive behaviors at a p-value of less than 0.05.
Results
Four hundred and sixteen respondents participated in this study, with a response rate of 98.6%. A significant proportion of participants know the cause, route of transmission, symptoms, and prevention methods of COVID-19 virus. However, very few (21.2%) had good preventive behaviors. The study showed that good preventive behavior was positively associated with female sex (AOR = 2.33, 95% CI: 1.38–3.94), higher schooling (AOR = 0.39, 95% CI: 0.17–0.88), high-risk perception (AOR = 2.26, 95% CI: 1.51–4.32), and high perceived self-efficacy (AOR = 1.1.75, 95% CI: 1.05–2.90).
Conclusions
A significant proportion of waiters know common symptoms of COVID 19, route of transmission, and its prevention methods. However, the preventive behavior was very low. Thus, all concerned bodies working on the prevention and control of COVID-19 should give attention to this population group to enhance compliance with recommended preventive behaviors.
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It was first discovered in the Hubei province of China in December 2019 [1] and on 11th March 2020, the World Health Organization (WHO) announced the outbreak of COVID-19 as a global pandemic due to the rapid increase in the number of cases outside China [2]. In Ethiopia, the first case of COVID-19 was reported on 13th March 2020 [3].
COVID-19 virus is transmitted from person-to-person through respiratory droplets, direct contact with an infected individual, or indirect contact with a surface or object that is contaminated with respiratory secretions [4]. Although not common, coronaviruses can also be transmitted from animals to humans [5]. During the early phase of the pandemic, the WHO suspected the zoonotic source of the virus and recommended precautionary measures to reduce the risk of transmission of emerging pathogens from animals to humans [6]. The disease is clinically presented with fever, cough, difficulty breathing, and other flu-like signs and symptoms including runny and stuffy nose, sneezing, and sore throat. While most people with COVID-19 develop only mild to moderate (81%) disease, approximately 15% develop severe disease that requires oxygen support, and 5% have critical disease with complications [7–9].
Currently, there is no effective treatment and vaccine for the virus. However, active case finding and isolation, quarantine, frequent handwashing with water and soap or alcohol-based sanitizers, social distancing, avoiding travel/travel restrictions, use of facemasks, and avoiding public gatherings are the measures of choice to prevent and mitigate the effect of the pandemic [10–14]. However, the effectiveness of such measures depends on public awareness and strict obedience to those recommendations.
Food and drinking establishments are potential hotspots for COVID-19 spread because many people share food, talk loudly, and drink alcohol in enclosed spaces [15]. The high interactions between guests and staff could lead to high transmission rates. Furthermore, the transmissibility of COVID-19 virus from asymptomatic patients could lead to a higher probability of work-related transmission as people with mild or no symptoms could continue to work or travel [16]. Thus, waiters working in different food and drinking establishments have a higher risk of contracting COVID-19 or easily spread the virus in the community.
Although waiters are at a higher risk of contracting and spreading the infection [16], information regarding their level of knowledge of COVID-19 and preventive behaviors is scarce. Most studies conducted so far have focused on the general public ignoring this vulnerable population group [17–19]. Therefore, the current study was intended to assess the knowledge of COVID-19 and preventive behaviors of waiters in Southwest Ethiopia.
Methods and materials
Ethical statements
Ethical approval was obtained from Mizan-Tepi University Institutional Review Board (IRB) before the commencement of the study. Written informed consent was obtained from all participants after explaining the study’s purpose, risks, and benefits. Moreover, participants were assured the participation is entirely voluntary and personal information is not disclosed to third parties.
Study design and area
A cross-sectional study was conducted among waiters working in hotels, restaurants, cafeterias, and bars found in Mizan-Aman, Jemu, and Masha towns in Southwest Ethiopia from June 1 to 15, 2020. Mizan-Aman, Jemu, and Masha are the administrative centers of Bench-Sheko, West-Omo, and Sheka zones, respectively. Mizan-Aman town is located 585 km from Addis Ababa, while Jemu and Masha are found at 625 km and 6132 km from Addis Ababa, respectively. The areas are commonly known by gold mining and cash crop production, such as coffee and different spices. As a result, there are high social mobilities in the areas that make a conducive environment for the spread of the COVID-19 virus.
Population
The source population was all waiters working in food and drinking establishments that were found in Mizan-Aman, Sheka, and Masha towns. Waiters on duties in the selected hotels, restaurants, cafeterias, and bars during the data collection period were randomly selected for interview.
Sample size and sampling procedure
The sample size was calculated using a formula for single population proportion by considering the following assumptions: 5% margin of error, 95%confidence level, and expected proportion of waiters with good preventive behavior to be 50%. A proportion of 50% was taken because there were no previous similar studies in Ethiopia. After adding a 10% contingency for non-response, the final sample size was determined to be 422.
A simple random sampling technique was used to select the study participants. First, lists of all food and drinking establishments found in the three towns were obtained from the respective town administration. Then, the sample size was proportionally allocated to each town depending on the total number of food and drinking establishments in each town. Finally, simple random sampling technique was use to select establishments from each town using computer generated random numbers. At establishment level, one waiter per establishment was selected for interviews. If more than one eligible individual presented in selected establishments, one person was randomly selected using the lottery method. All waiters in an establishment were listed on separate slips of paper of the same size and shape. Then, papers were folded carefully, and finally, a blindfold selection was made.
Measures
The data were collected through face-to-face interviews using a pretested structured questionnaire. The questionnaire was developed from related studies and guidelines [20–23]. The tool consisted of five parts: participants' characteristics (age, sex, marital status, religion, occupation, ethnicity, and the number of people living in the home), knowledge of COVID-19, perceived self-efficacy regarding prevention measures, COVID-19 preventive behaviors, and risk perception regarding COVID-19.
COVID-19 preventive behavior was measured using 10 items. Respondents were asked to rate how often they had been practicing the preventive measures recommended by the WHO during the pandemic on five-point scales: (1) never, (2) rarely, (3) sometimes, (4) frequently, and (5) always. During analysis, each item was recoded into “not practiced or inadequate practice” if subjects scored never, rarely, or sometimes and into “adequate practice” if scored frequently or always. Finally, respondents who scored adequate practice for at least 60% of the items were considered as having “good preventive behavior”; otherwise “poor preventive behavior”. A 60% cutoff point was achieved based on a study done in Iran [24].
Knowledge of COVID-19 (etiology, mode of transmission, symptoms, prevention methods, and treatment or vaccine) was measured using 15 items that were answered on" yes”, “no” or “I don’t know” responses. The correct answers were coded with 1 and the incorrect answers were coded with 0. Finally, participants who scored ≤ 59% were categorized as having “poor knowledge”, 60%-79% as “moderate knowledge”, and ≥80% as “good knowledge” of COVID-19 based on Bloom’s cut-off point [25].
Self-efficacy to practice commonly recommended COVID-19 prevention methods was measured using 4 items that were responded on a five-point scale: (1) certainly not, (2) probably not, (3) perhaps not to perhaps yes, (4) probably yes, and (5) most certainly. The respondents were asked if they were able to carry out the recommended measures. A mean score was computed and a score at mean or less indicates low self-efficacy, while a score above the mean indicates high self-efficacy.
Risk perception regarding COVID-19 was measured using 12 items of five Likert scale: (1) strongly disagree, (2) disagree, (3) neutral, (4) agree, and (5) strongly agree. The items were stated in a way that a higher value indicates higher risk perception. The cumulative risk perception score (range 12–60) was computed [22]. Based on the mean score, risk perception was categorized as high if scored above the mean score and low if scored at the mean or less.
The reliability (internal consistency) of the questionnaire was checked based on the results of the pretest. The Cronbach's alpha was 0.703 for practice, 0.682 for knowledge, 0.679 for risk perception, and 0.764 for self-efficacy items.
Data were collected by health care professionals who had a bachelor's degree qualification, and prior data collection experiences. The data collectors and supervisors were trained on the data collection tool, the objective of the study, how to ensure confidentiality of information, and how to prevent transmission of COVID-19 during the interview. To reduce the risk of COVID-19 transmission during data collection, the data collectors used necessary personal protective equipment (PPE).
Data processing and analysis
The collected data were manually checked for completeness, entered into Epi data manager version 4.0.2 and exported to SPSS version 22 for analysis. Descriptive statistics were done for different variables and bivariate binary logistic regression analysis was done to select candidate variables for multivariable binary logistic regression analysis at p value < 0.25 [26]. Finally, multivariable logistic regression analysis was done to control for the effect of possible confounders, and variables with p value < 0.05 were taken as statistically significant determinants of COVID-19 preventive behavior. Model fitness was evaluated using the Hosmer-Lemeshow goodness of fit test, and multicollinearity was checked using variance inflation factor (VIF).
Results
Socio-demographic characteristics
From the 422 total sample size, 416 participated in the study, resulting in a 98.6% response rate. The mean age of respondents was 27.26 (SD = ±8.35) years and more than half were aged 18–25 years. More than half (54.1%) of the study participants were female. The majority (84.1%) of the participants were single, and 44% of the participants had attended primary school. Three hundred thirty (79.3%) study participants were living with one or more persons (Table 1).
Table 1. Socio-demographic characteristics of waiters working in food and drinking establishments, Southwest Ethiopia, 2020.
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Age group | 18–25 | 218 | 52.4 |
| 26–35 | 142 | 34.1 | |
| >35 | 56 | 13.5 | |
| Sex | Male | 191 | 45.9 |
| Female | 225 | 54.1 | |
| Marital status | Single | 350 | 84.1 |
| Married | 24 | 5.8 | |
| Divorced/ Widowed | 42 | 10.1 | |
| Religion | Orthodox | 283 | 68.0 |
| Muslim | 61 | 14.7 | |
| Protestant | 72 | 17.3 | |
| Educational status | No education | 79 | 19.0 |
| Primary | 183 | 44.0 | |
| Secondary/ Above | 154 | 37.0 | |
| Ethnicity | Kafa | 165 | 39.7 |
| Amhara | 110 | 26.4 | |
| Gurage | 36 | 8.7 | |
| Bench | 34 | 8.2 | |
| Tigre | 18 | 4.3 | |
| Oromo | 18 | 4.3 | |
| Sheka | 10 | 2.4 | |
| Meinit | 9 | 2.2 | |
| Others* | 9 | 2.2 | |
| How many people live in your house? | Live alone | 86 | 20.7 |
| Live with one or more persons | 330 | 79.3 |
Others*: Silte, Sheko and Dawuro.
Knowledge of COVID-19
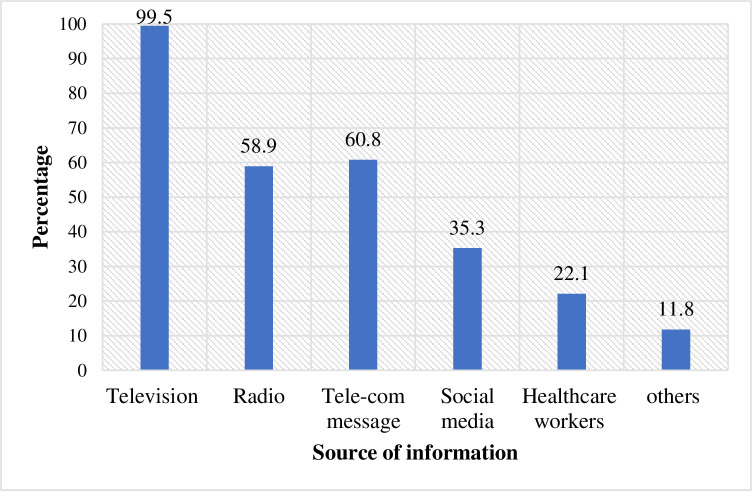
All study participants heard about the COVID-19 pandemic. The main sources of information were television (99.5%), followed by short messages from telecommunication (60.8%) and radio (58.9%) (Fig 1). The majority (84.4%) of the respondents know the cause of the new coronavirus disease. Three hundred twenty-eight (78.8%) study participants mentioned direct contact with infected people as a mode of transmission for the virus. Nearly three-fourths (72.8%) thought that contact with contaminated animals and 60.6% thought that touching contaminated objects/surfaces represent modes of spread for COVID-19. Furthermore, cough (86.6%), fever (83.2%), and shortness of breath (48.1%) were the commonly known symptoms of COVID 19. Regarding preventive methods, about 82.7% know frequent handwashing with soap and water or using alcohol-based sanitizer helps prevent COVID-19. Also, 75.5% of the respondents know that keeping social distance prevents COVID-19 (Table 2).
Fig 1. Source of information about COVID-19 among waiters working in food and drinking establishments in Southwest Ethiopia, 2020 (n = 416).
Table 2. Knowledge of COVID-19 among waiters working in food and drinking establishments, Southwest Ethiopia, 2020.
| Variables (n = 416) | Correct | Incorrect |
|---|---|---|
| N- (%) | N- (%) | |
| What causes a new coronavirus disease? | 351(84.4) | 65(15.6) |
| Can COVID-19 virus transmit through the following routes/modes? | ||
| Droplets from infected people | 250(60.1) | 166(39.9) |
| airborne | 206 (49.5) | 210(50.5) |
| Direct contact with an infected person | 328 (78.8) | 88 (21.2) |
| Touching of contaminated objects/surfaces | 252 (60.6) | 164 (39.4) |
| Contact with contaminated animals | 303 (72.8) | 113(17.2) |
| Mosquito bites | 395(95.0) | 21(5.0) |
| Can COVID-19 infected patients present with the following symptoms? | ||
| Fever | 346 (83.2) | 70 (16.8) |
| Cough | 361(86.8) | 55 (13.2) |
| Shortness of breath | 200(48.1) | 216 (51.9) |
| Can COVID-19 virus be prevented by the following methods? | ||
| Frequent hand washing using soap and water or alcohol-based sanitizer | 344 (82.7) | 72 (17.3) |
| Avoid close contact with anyone who has a fever and cough | 314 (75.5) | 102 (24.5) |
| Avoid unprotected direct contact with live animals and surfaces | 156(62.5) | 260 (37.5) |
| Sleeping under the mosquito net | 397 (95.4) | 19 (4.6) |
| Is there effective treatment or vaccine for the COVID-19 currently? | 312 (75.0) | 104(25.0) |
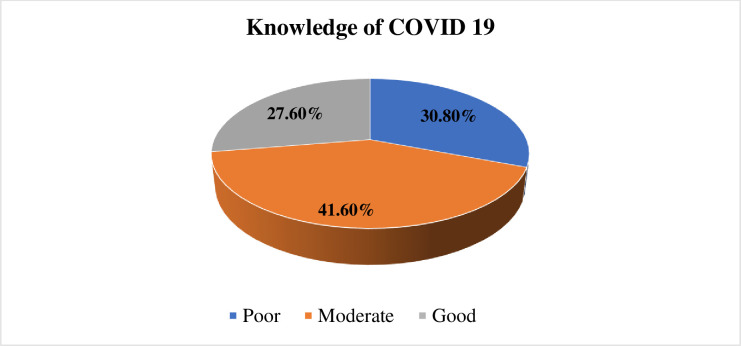
The mean cumulative score of knowledge was 10.32 (SD = 2.37), and the minimum and maximum scores were 3 and 15 respectively. Regarding compressive knowledge of COVID, 30.8% of the respondents had poor knowledge and 27.6% had good knowledge (Fig 2).
Fig 2. Comprehensive knowledge about COVID 19 among waiters working in food and drinking establishments in Southwest Ethiopia, 2020 (n = 416).
Preventive behavior of COVID 19
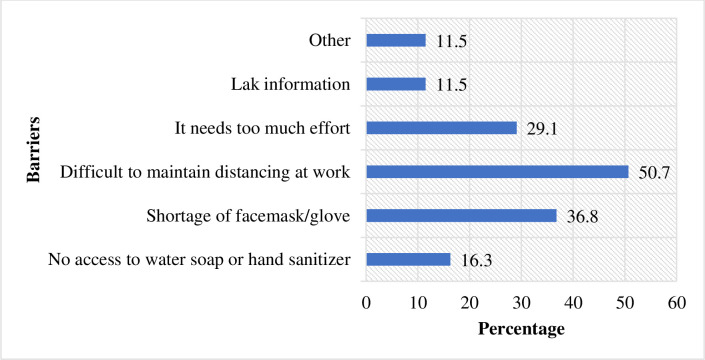
About 27% of the respondents never keep physical distance, while only 5% keep physical distance always. About 18.8% and 19.2% of the respondents wash their hands with water and soap or with sanitizer frequently and always, respectively. Only 6% of the respondents using facemasks at work or outside their home always, and about 6.7% and 4% were using gloves frequently and always, respectively (Table 3). The overall proportion of study participants with good COVID-19 preventive behavior were only 21.2%. The common barriers reported were the difficulty of maintaining social distance at work due to the nature of their work, shortage of facemasks and gloves, and high efforts needed to implement prevention measures (Fig 3).
Table 3. Preventive behavior of COVID-19 virus among waiters working in food and drinking establishments, Southwest Ethiopia, 2020.
| Questions | Never | Rarely | Sometimes | Frequently | Always |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| How often are you maintaining physical distance? | 22(5.3) | 39(9.4) | 112(26.9) | 151(36.3) | 92(22.1) |
| How often are you avoiding larger gatherings? | 57(13.7) | 58(13.9) | 94(22.6) | 110(26.4) | 97(23.3) |
| How often are you avoiding touching your face, eyes, mouth, and nose? | 73(17.5) | 78(18.8) | 122(29.3) | 68(16.3) | 75(18) |
| How often are you washing your hands with water and soap or sanitizers? | 111(26.7) | 45(10.8) | 78(18.8) | 102(24.5) | 80(19.2) |
| How often are you avoiding contact with people who had fever and cough? | 110(26.4) | 38(9.1) | 60(14.4) | 110(26.4) | 98(23.6) |
| How often are you wearing a facemask when you are at work or outside the home | 161(38.7) | 74(17.8) | 108(26.0) | 48(11.5) | 25(6.0) |
| How often do you use public transportation during the months of the pandemic? | 118(28.4) | 67(16.1) | 124(29.8) | 46(11.1) | 61(14.7) |
| How often you avoid unprotected contacting (touching) of frequently contacted surfaces | 68(16.3) | 65(15.6) | 126(30.3) | 99(23.8) | 58(13.9) |
| Did you avoid unnecessary travel during the months of the pandemic? | 178(42.8) | 57(13.7) | 74(17.8) | 42(10.1) | 65(15.6) |
| How often are you wearing a glove at work? | 189(45.4) | 72(17.3) | 110(26.4) | 28(6.7) | 17(4.1) |
Fig 3. Barriers or hindering factors to implement COVID-19 prevention measures among waiters working in food and drinking establishments in Southwest Ethiopia, 2020 (n = 416).
Risk perception and self-efficacy to practice preventive measures
Two hundred twenty-two (53.4%) of the participants had a high-risk perception towards COVID-19, while the remaining 46.6% had a low-risk perception. Besides, 53.1% of study participants had high self-efficacy to practice COVID-19 preventive methods.
Factors associated with COVID-19 preventive behavior
In simple binary logistic regression analysis, sex, marital status, educational status, number of people living in the house, risk perception, and perceived self-efficacy had a p value ≤ 0.25; hence, they were candidates for the multivariable binary logistic model. However, age and knowledge about COVID-19 were excluded from the multivariable model because their p-values were greater than 0.25 in the bivariate binary logistic regression analysis. The number of people living in the home was excluded from the model because the model best fit when this variable removed from the model. In the final multivariable binary logistic regression model, sex, educational status, risk perception, and perceived self-efficacy were significantly associated with COVID-19 preventive behavior (p <0.05) (Table 4).
Table 4. Factors associated with COVID 19 preventive behavior among waiters working in food and drinking establishments, Southwest Ethiopia, 2020.
| Variables | Preventive behavior | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Good (%) | Poor (%) | ||||
| Age group | |||||
| 18–25 | 48(21.1) | 180(78.9) | 1 | 1 | |
| 26–35 | 26(19.0) | 111(81.0) | 0.88(0.52–1.50) | 0.81(0.45,1.43) | 0.462 |
| >35 | 14(27.5) | 37(72.5) | 1.42(0.71–2.84) | 1.49(0.72,3.07) | 0.284 |
| Sex | |||||
| Male | 27(14.1) | 164(85.9) | 1 | 1 | |
| Female | 61(27.1) | 167(72.9) | 2.26(1.37–3.73) | 2.33(1.38–3.94) | 0.002 |
| Marital status | |||||
| Single | 74(21.1) | 276(78.9) | 1 | 1 | |
| Married | 8(33.3) | 16(66.7) | 1.86(0.76–4.53) | 2.26(0.89,5.73) | 0.087 |
| Divorced/ Widowed | 6(14.3) | 36(85.7) | 0.62(0.25–1.53) | 0.69(0.27,1.77) | 0.444 |
| Educational status | |||||
| No education | 9(11.4) | 70(88.6) | 0.48(0.17–0.83) | 0.39(0.17–0.88) | 0.023 |
| Primary | 40(21.9) | 143(78.1) | 0.82(0.49–1.37) | 0.99(0.58–1.69) | 0.978 |
| Secondary/ Above | 39(25.3) | 115(74.7) | 1 | 1 | |
| Knowledge of COVID 19 | |||||
| Poor | 25(19.5) | 103(80.5) | 1 | 1 | |
| Fair | 36(20.8) | 137(79.2) | 0.79(0.42–1.46) | 0.96(0.49,1.89) | 0.911 |
| Good | 27(23.5) | 88(76.5) | 0.86(0.48–1.51) | 0.98(0.53,1.82) | 0.949 |
| Risk perception | |||||
| Low | 27(13.9) | 167(86.1) | 1 | 1 | |
| High | 61(27.5) | 161(72.5) | 2.34(1.42–3.87) | 2.56(1.51–4.32) | <0.001 |
| Self-efficacy | |||||
| Low | 38(17.2) | 183(82.8) | 1 | 1 | |
| High | 50(25.6) | 145(74.4) | 1.66(1.03–2.67) | 1.75(1.05–2.90) | 0.030 |
Hosmer and Lemeshow test; X2 = 9.36; df = 8; p = 0.313.
The odds of good COVID-19 preventive behavior among females was 2.33 times higher than their counterparts (AOR = 2.33, 95% CI: 1.38–3.94). The odds of good COVID-19 preventive behavior among waiters who had no formal education was about 0.39 times lower compared to those who attended at least secondary education (AOR = 0.39, 95% CI: 0.17–0.88). The odds of good COVID-19 preventive behavior among waiters who had high-risk perception toward COVID-19 was 2.56 times higher compared to those who had low-risk perception toward COVID-19 (AOR = 2.26, 95% CI: 1.51–4.32). The odds of good COVID-19 preventive behavior among waiters who had high perceived self-efficacy was almost twice as high as those who had low self-efficacy to practice COVID-19 prevention methods (AOR = 1.1.75, 95% CI: 1.05–2.90).
Discussion
After the first case of COVID-19 was detected in Ethiopia on March 13th, 2020 [3], the government started responding to the pandemic aggressively. A state of emergency was declared to counter and control the spread of COVID-19 and mitigate its impact. During the periods of the state of emergency: land borders were closed, schools and universities remained shut, all gathering of more than four persons were forbidden unless specially permitted, all vehicles (public and private) and railway, and light railway allowed to operate only at 50% and 25% of passenger capacity, respectively. Moreover, hotels, restaurants, and cafeterias didn't allow service to more than three patrons at a single table and should ensure that tables that are being used by patrons simultaneously are at least two adult strides apart [27]. However, still date a full lockdown has not been declared in Ethiopia. Hotels, bars, restaurants, and cafeterias are not completely closed during the pandemic in Ethiopia; hence, the risk of the spread of the virus is high because they are visited by many people who interact among themselves and with employees. Therefore, every staff must strictly follow the basic protective measures.
This study aimed to assess knowledge of COVID-19 and the practice of preventive behaviors among waiters in southwest Ethiopia. The finding of this study showed that the majority of the respondents knew the cause of COVID-19. It was revealed that a significant proportion of participants know the mode of spread of the virus (inhalation of droplets from infected people, direct contact with infected people, contaminated animals, and contaminated objects/surfaces). A few participants thought that COVID-19 can be transmitted by mosquito bites. A study conducted in Nigeria also reported a similar misconception [28]. Furthermore, the majority of the respondents know common symptoms of COVID-19 disease and its prevention methods. The main source of information for study participants was from television.
It was also identified that only 21.2% of the study participants had good COVID-19 preventive behavior. This finding is almost similar to a study conducted in Myanmar [29]. However, this finding is lower than a study conducted in Northwest Ethiopia, and Pakistan [30–32]. This variation could be due to the differences in socio-economic characteristics of study participants or it might be due to disparity in access to media. The current study was conducted in remote areas of the country where access to the internet and electronic media is relatively low. Also, it might be due to barriers related to the nature of the work, shortage of facemasks and gloves during early phase of the outbreak. The low COVID-19 preventive behavior among waiters has a great public health implication; if waiters are infected with COVID-19, there will be a high risk of spreading the disease to the community because they frequently come in contact with many people due to the nature of their work.
The odds of good practice of COVID-19 prevention methods among females was higher compared to males. Most of the time females are more careful of themselves and others around them. Other studies also indicated that males are less likely to practice COVID-19 prevention methods compared to females [33, 34]. Thus, behavioral intervention programs had better consider women as change agents in adopting a particular preventive behavior in the family and the community as well.
This study identified that a higher score of COVID-19 preventive behavior is associated with higher risk perception. This finding is consistent with findings from other studies [4, 14]. This could be due to individuals who perceive they are at high risk might engage in preventive behaviors. This may imply it could be possible to enhance the desired behavior by proper risk communication about the disease.
The educational status of participants was also associated with COVID-19 preventive behavior. The odds of good COVID-19 preventive behavior among study participants who had no formal education was lower compared to those who attended at least secondary education. Similarly, a study conducted among visitors in Jimma University Medical Center in Ethiopia showed that proper handwashing with soap and water or sanitizer was negatively associated with lower educational status [35]. This could be because educated people are in a better position to have access to COVID-19 related information. Moreover, they could easily comprehend instruction/recommendations made by health personnel, media, and other relevant bodies.
The odds of good COVID-19 preventive behavior among subjects who had high perceived self-efficacy was higher when compared to those with low self-efficacy to practice COVID-19 prevention methods. A similar claim was forwarded by a previous study conducted elsewhere [33]. This is substantiated by the theory of self-efficacy which states that self-efficacy influences every human endeavor; by determining the belief a person holds regarding his or her ability to perform a particular action [36]. Thus, enabling people to enhance their self-efficacy through various individualized approach could bring the desired behavioral changes.
Limitation of the study
Due to the cross-sectional nature of this study, it is difficult to establish cause-effect relationships. Also, since data were collected through self-reports, there might be a risk of desirability bias. Furthermore, due to the fact that the study design is purely quantitative, we cannot explain the reasons for the observed effect and their meanings in that particular context.
Conclusion
A significant proportion of waiters knew common symptoms of COVID 19, route of transmission, and its prevention methods. However, good COVID-19 preventive behavior was very low. It was recognized that being a female, higher schooling, having a high-risk perception, and having a high perceived self-efficacy were positively associated with good COVID-19 preventive behavior. Thus, all concerned bodies working on the prevention and control of COVID-19 should give attention to this population to enhance compliance with recommended preventive behaviors through addressing these significant predictors. Since widespread infection among waiters with COVID-19 has an important public health implication, law enforcement bodies shall employ a compulsory mechanism to monitor the implementation of all recommendations.
Supporting information
(SAV)
(DOCX)
Acknowledgments
We would like to express our heartfelt gratitude to Mizan-Tepi University for providing us an ethical clearance to undertake this research project. Also, we thanks the study participants and data collectors for their valuable contributions.
List of abbreviation
- AOR
Adjusted Odd Ratio
- CI
Confidence Intervals
- SPSS
Statistical Package for Social Scientists
- WHO
World Health Organization
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Vandeweerd V, Vliet D Van Der. COVID-19 Overview of information available to support the development of medical countermeasures and interventions against COVID-19. 2020;1–120. [Google Scholar]
- 2.Hauck Grace, Gelles Karl, Bravo Veronica and MT. Coronavirus updates_ How COVID-19 unfolded in the US. 2020. [Google Scholar]
- 3.World Health Organization. First Case of COVID-19 confirmed in Ethiopia-WHO Regional Office for Africa [Internet]. 2020. Available from: https://www.afro.who.int/news/first-case-covid-19-confirmed-ethiopia
- 4.World Health Organization. COVID-19 management in hotels and other entities of the accommodation sector: interim guidance, 25 August 2020 [Internet]. 2020. Available from: https://apps.who.int/iris/handle/10665/333992
- 5.Singla R, Mishra A, Joshi R, Jha S, Sharma AR, Upadhyay S, et al. Human animal interface of SARS-CoV-2 (COVID-19) transmission: a critical appraisal of scientific evidence. Vet Res Commun. 2020;44(3–4):119–30. 10.1007/s11259-020-09781-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. WHO recommendations to reduce risk of transmission of emerging pathogens from animals to humans in live animal markets or animal product markets, 26 March 2020 [Internet]. 2020. Available from: https://apps.who.int/iris/handle/10665/332217 [Google Scholar]
- 7.Zhonghua Liu Xing Bing Xue Za Zhi. Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. 2020;41(2):145–151. [Google Scholar]
- 8.CDC. Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) [Internet]. 2020 [cited 2020 Dec 24]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
- 9.World Health Organization. Clinical management of COVID-19: interim guidance, 27 May 2020 [Internet]. 2020. Available from: https://apps.who.int/iris/handle/10665/332196
- 10.Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, et al. : The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. The Lancet Psychiatry 2018, 5(3):237–286. 10.1016/S2215-0366(17)30513-8 [DOI] [PubMed] [Google Scholar]
- 11.Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJ, Goodwin RD, Kubzansky L, et al. : Anxiety disorders and comorbid medical illness. General hospital psychiatry 2008, 30(3):208–225. 10.1016/j.genhosppsych.2007.12.006 [DOI] [PubMed] [Google Scholar]
- 12.Burke RM: Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020. MMWR Morbidity and mortality weekly report 2020, 69 10.15585/mmwr.mm6909e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zettler I, Schild C, Lilleholt L, Böhm R: Individual differences in accepting personal restrictions to fight the COVID-19 pandemic: Results from a Danish adult sample. 2020. [Google Scholar]
- 14.World Health Organization. Q&A on coronaviruses (COVID-19) [Internet]. 2020. Available from: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
- 15.What Makes Bars and Restaurants Potential Covid-19 Hot Spots—WSJ [Internet]. [cited 2020 Aug 13]. Available from: https://www.wsj.com/articles/what-makes-bars-and-restaurants-potential-covid-19-hot-spots-11593768600
- 16.Lan FY, Wei CF, Hsu YT, Christiani DC, Kales SN. Work-related COVID-19 transmission in six Asian countries/areas: A follow-up study. PLoS One [Internet]. 2020;15(5):1–11. Available from: 10.1371/journal.pone.0233588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jemal B, Ferede ZA, Mola S, Hailu S, Abiy S, Wolde GD, et al. : Knowledge, attitude and practice of healthcare workers towards COVID-19 and its prevention in Ethiopia: a multicenter study. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FMOH: COVID 19 Handbook for health professionals Federal Minstry of Health, Ethiopia, Availabile: https://www.moh.gov.et/ accesed on May 12, 2020.
- 19.FMOH: Infection Prevention and Control Interim Protocol for COVID-19 In Health Care Settings in Ethiopia. April, 2020. Availabile: https://www.moh.gov.et, accesed on May 12, 2020.
- 20.Municipal Public Health Service Rotterdam-Rijnmond, National Institute for Public Health and the Environment. Standard questionnaire on risk perception of an infectious disease outbreak. 2015.
- 21.World Health Organization. Survey Tool and Guidance: Rapid, simple, flexible behavioural insights on COVID-19 Monitoring. 2020.
- 22.Wol K, Larsen S, Øgaard T. How to define and measure risk perceptions. Ann Tour Resaerch. 2019;79:102759. [Google Scholar]
- 23.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Heal Psychol [Internet]. 2007. March [cited 2020 Apr 26];26(2):136–45. Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/0278-6133.26.2.136 [DOI] [PubMed] [Google Scholar]
- 24.Honarvar B, Lankarani KB, Kharmandar A, Shaygani F. Knowledge, attitudes, risk perceptions, and practices of adults toward COVID-19: a population and field-based study from Iran. Int J Public Health [Internet]. 2020; Available from: 10.1007/s00038-020-01406-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmed N, Taneepanichskul S. Knowledge, attitude and practices of dengue fever prevention among people in Males’, Maldives. J Heal Res. 22:33–7. [Google Scholar]
- 26.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:1–8. 10.1186/1751-0473-3-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Federal Negarit Gazette of the Federal Democratic Republic of Ethiopia. State of Emergency Proclamation No. 3/2020 Implementation Regulation No.466/2020 [Internet]. 2020 [cited 2020 Nov 9]. Available from: http://www.moh.gov.et/ejcc/sites/default/files/2020-04/negarit.pdf
- 28.Christopher R, Margaret R, Dauda MAD, Saleh A, Ene P. Knowledge, Attitudes and Practices Towards COVID ‑ 19: An Epidemiological Survey in North ‑ Central Nigeria. J Community Health [Internet]. 2020;(0123456789). Available from: 10.1007/s10900-020-00881-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christopher R, Margaret R, Dauda MAD, Saleh A, Ene P. Knowledge, Attitudes and Practices Towards COVID ‑ 19: An Epidemiological Survey in North ‑ Central Nigeria. J Community Health [Internet]. 2020;(0123456789). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hospital AZ. Knowledge, Attitude and Practice Towards COVID-19 Among Chronic Disease Patients at. 2020;1949–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tadesse AW, Melese N, Eshetie S, Chanie M, Ali A. Knowledge, Attitude, and Practice and Associated Factors towards COVID-19 among College Students in Amhara Region, Ethiopia; A Cross-Sectional Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saqlain M, Munir MM, Rehman SU, Gulzar A, Naz S, Ahmed Z, et al. Knowledge, attitude, practice and perceived barriers among healthcare workers regarding COVID-19: a cross- sectional survey from Pakistan. J Hosp Infect [Internet]. 2020;105(3):419–23. Av. 10.1016/j.jhin.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ibuka Y, Chapman GB, Meyers LA, Li M, Galvani AP. The dynamics of risk perceptions and precautionary behavior in response to 2009 (H1N1) pandemic influenza. BMC Infect Dis. 2010;10(296). 10.1186/1471-2334-10-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brug J, Aro AR, Richardus JH. Risk Perceptions and Behaviour: Towards Pandemic Control of Emerging Infectious Diseases. Int J Behav Med. 2009;16:3–6. 10.1007/s12529-008-9000-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. 2020;77:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luszczynska A., & Schwarzer R. (2005). Social cognitive theory In Conner M. & Norman P. (Eds.), Predicting health behaviour (2nd ed rev., pp. 127–169). Buckingham, England: Open University Press. [Google Scholar]