Abstract
A compelling body of evidence points to pulmonary thrombosis and thromboembolism as a key feature of COVID-19. As the pandemic spread across the globe over the past few months, a timely call to arms was issued by a team of clinicians to consider the prospect of long-lasting pulmonary fibrotic damage and plan for structured follow-up. However, the component of post-thrombotic sequelae has been less widely considered. Although the long-term outcomes of COVID-19 are not known, should pulmonary vascular sequelae prove to be clinically significant, these have the potential to become a public health problem. In this Personal View, we propose a proactive follow-up strategy to evaluate residual clot burden, small vessel injury, and potential haemodynamic sequelae. A nuanced and physiological approach to follow-up imaging that looks beyond the clot, at the state of perfusion of lung tissue, is proposed as a key triage tool, with the potential to inform therapeutic strategies.
Introduction
As the initial wave of the COVID-19 pandemic has receded, a spectrum of lung parenchymal and pulmonary vascular pathology related to acute illness has emerged. The combination of viral pneumonia and acute respiratory distress syndrome that characterises the severe manifestations of acute COVID-19 illness is considered to be a possible precursor to pulmonary fibrosis.1, 2, 3
Another major potential pulmonary morbidity is the propensity for thromboembolic phenomena, in both systemic and pulmonary circulations.4, 5, 6, 7 Apart from the generic risks for venous thromboembolism in acutely ill hospitalised patients, evidence is emerging for a more specific, angiocentric signature of COVID-19, related to an in-situ thrombotic microangiopathy and a complex immune inflammatory cascade, especially in the pulmonary vascular bed.4, 8, 9, 10, 11, 12, 13, 14, 15 Many patients with proven thromboembolism in COVID-19 have been from intensive care series, but thromboembolism is now being reported in less critically ill patients in hospital and ambulatory settings.16, 17, 18
Whether such a pulmonary vascular insult is transient and self-correcting, or has the potential to lead to sequelae, will only become apparent with longer-term follow-up. In this Personal View, we turn our attention to the post-COVID recovery cohort of patients, specifically with respect to the follow-up of pulmonary vascular sequelae. Within the constraints of an insufficient knowledge base on COVID-19 recovery, we propose an algorithm for follow-up that integrates testing and triage for a combination of potential pulmonary vascular and pulmonary fibrotic sequelae. Within this pathway, we propose using perfusion (rather than angiographic) imaging as a first-line imaging tool for triage to exclude or evaluate residual clot burden and small vessel injury. The reasons why perfusion imaging might be particularly useful for COVID-19 follow-up and the range of such perfusion imaging tools at our disposal are reviewed. Also addressed are the challenges posed by the pandemic to the practice of ventilation perfusion (VQ) single-photon emission computed tomography (SPECT) scintigraphy, the gold-standard perfusion imaging tool in the evaluation of chronic pulmonary thromboembolism.
Pulmonary sequelae after COVID-19
There is insufficient understanding of the recovery phase of COVID-19, but increasing recognition that patients need a multifaceted approach to the evaluation of residual symptoms and dysfunction.2, 19, 20, 21, 22, 23 Clinicians are commonly faced with patients who present with unexplained persistent chest pain, breathlessness, exercise limitation, and fatigue, weeks after hospitalisation or the onset of symptoms.22, 23 The causes of such symptoms are not fully understood, but various factors might be involved, such as restricted lung function, impairment in gas exchange, cardiac dysfunction, and partially resolved thrombus with flow limitation. Equally, not all breathlessness or functional limitation will be attributable to haemodynamic derangements; muscle deconditioning, dysfunctional breathing patterns, and psychosocial factors might contribute substantially to these symptoms.
Current recommendations from international societies and opinion leaders are variable and continue to evolve.20, 21, 24, 25 Local pathways differ between countries and institutions, as does the panel of tests used. For instance, the Zhejiang University School of Medicine in Hangzhou, China,26 advises outpatient visits at 1, 2, and 4 weeks after discharge, with blood tests, lung function tests, and CT scans done at the discretion of the clinical team. Current British Thoracic Society guidelines20 recommend a follow-up clinic evaluation at 12 weeks for patients with COVID-19 and a diagnosis of venous thromboembolism or a clinicoradiological diagnosis of COVID-19 pneumonia who do not require admission to the intensive care unit or a high-dependency unit. The guidelines advise further imaging with high-resolution CT and CT pulmonary angiogram (CTPA), as needed, based on an initial follow-up chest radiograph and functional assessment.
Key messages.
-
•
Venous thromboembolism and in-situ small vessel pulmonary thromboses are both implicated in COVID-19; these pulmonary vascular manifestations are a potential precursor to chronic thromboembolic disease and pulmonary hypertension
-
•
Small vessel thrombosis can be underestimated on conventional CT pulmonary angiogram (CTPA); perfusion imaging looks beyond the clot and assesses residual blood flow limitation
-
•
Ventilation perfusion (VQ) planar scintigraphy and VQ single-photon emission computed tomography (SPECT) are gold-standard screening tests in the assessment of chronic thromboembolism
-
•
A normal VQ scan excludes the presence of a clinically significant perfusion deficit; if positive, the extent of deficit can be of prognostic value
-
•
Contrast dual-energy CT (DECT) is a surrogate perfusion technique with potential for detecting clot and perfusion in one sitting; DECT studies of chronic thromboembolic disease have shown promising results, with reasonable concordance with VQ imaging
-
•
Lung perfusion phenotypes in COVID-19 could include a mix of classical segmental and the more atypical distal small vessel-related deficits, which might be subtle and easily overlooked
-
•
Ventilation scintigraphy was discontinued in many nuclear medicine units at the start of the pandemic; international guidance on the aerosol-generating potential of radio-nebulisers varies and uncertainties remain, but risks can be safely managed in the post-COVID-19 cohort
-
•
Imaging departments and, specifically, nuclear medicine should be supported to adapt and manage risks to provide an appropriate service for COVID-19 survivors
Preliminary reports of the follow-up of patients after COVID-193, 27, 28 have been published. Mo and colleagues3 evaluated a cohort of discharged survivors (n=110) at 25–40 days after initial symptoms and found that impairment of diffusion capacity was the most common abnormality (in 51 [47·2%] of 110 cases) and was associated with initial clinical severity of disease. Frija-Masson and colleagues28 analysed 50 patients retrospectively and found an association between lung function at day 30 and initial CT severity and clinical grade of pneumonia. They found 27 (54%) of 50 patients to have a mix of restrictive and low diffusion patterns. Pertinently, they reported an isolated decreased diffusing capacity in 13 (26%) of 50 patients, raising the possibility that, in addition to alveolar cell damage-related potential for fibrosis, pulmonary vascular insult might also play a part.
Experience from severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) is also relevant, as both viral illnesses were associated with an inflammatory response and thrombotic complications.29, 30 Published follow-up series of patients with SARS31, 32, 33 have shown functional deficits with dominant residual impaired lung diffusing capacity in about 15–40% (and reduced total lung capacity in 5–10%) of patients at various timepoints between 6 months and 2 years. Isolated impairment of diffusing capacity of carbon monoxide has been reported in MERS survivors at 12 months.34 The scarce evidence thus far from the COVID-19 recovery cohort and the SARS and MERS follow-up cohorts reinforces the need to consider an optimal and efficient modality mix for the testing and triage of patients for a combination of potential residual thromboembolic disease and pulmonary fibrosis.
Follow-up algorithm for post-thrombotic sequelae
A follow-up algorithm for the investigation of patients after COVID-19 is proposed, with the aim of evaluating the twin potential for both lung fibrosis and thromboembolic pulmonary vascular sequelae (Figure 1, Figure 2 ). The algorithm is designed to be proactive in investigating pulmonary vascular sequelae, with perfusion imaging as a key tool in the triage tree. Within this framework, perfusion imaging is recommended if mandated by lung function, exercise physiology, or transthoracic echocardiography, even in the absence of proven thromboembolism during the acute illness. This approach is driven by our current insufficient understanding of post-COVID-19 sequelae. The group of patients who receive perfusion imaging in follow-up is expected to be drawn from both hospitalised patients with COVID-19 and an easily forgotten cohort of patients who recover from an acute illness in the community but present with breathlessness and exercise limitation afterwards. Although the cost–benefit considerations of this testing strategy might be skewed at first, we believe that systematic early follow-up experiences will be key to informing future practice. Indeed, we view this algorithm as a dynamic and responsive decision tree that we expect to adapt and change as experience and evidence evolves. The inclusion of perfusion imaging might prove to be prescient or wholly unnecessary.
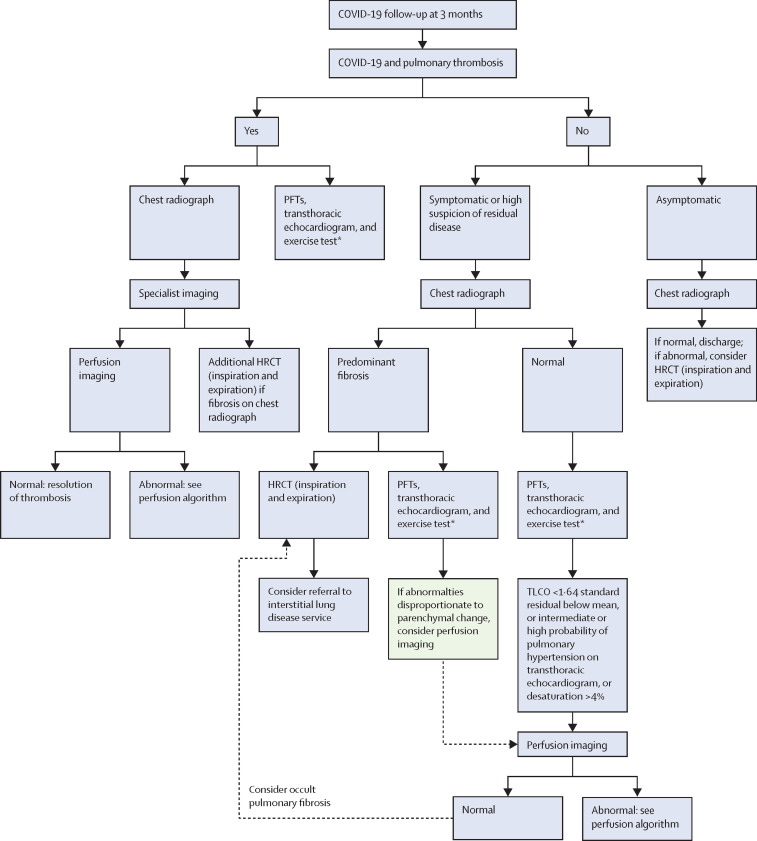
Figure 1.
Follow-up algorithm at approximately 3 months after COVID-19
HRCT=high-resolution CT. PFT=pulmonary function test. TLCO=transfer factor of the lung for carbon monoxide. *The exercise test is an incremental shuttle walk test, a 6-min walk test, or a sit-to-stand test (a cardiopulmonary exercise test might be available in some centres to evaluate breathlessness following COVID-19).
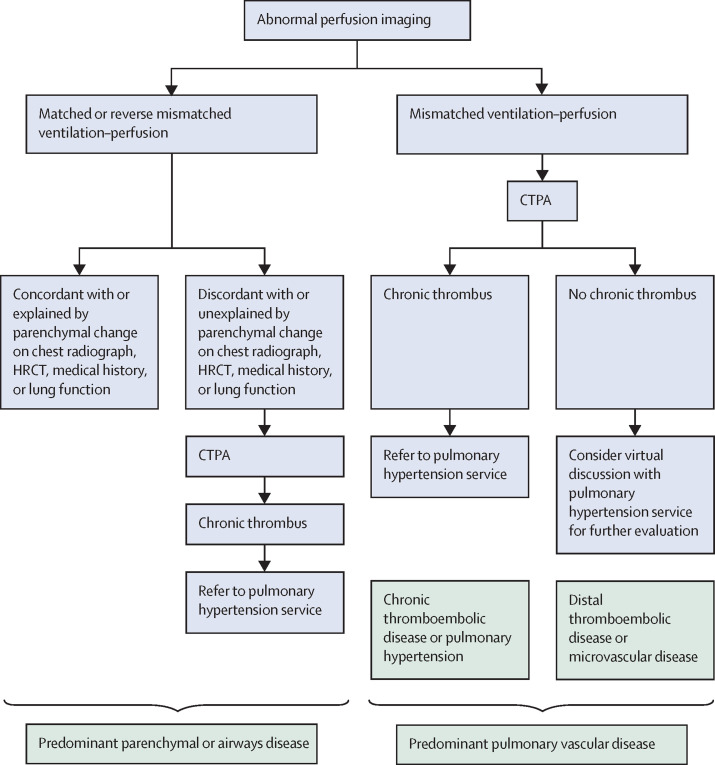
Figure 2.
Follow-up algorithm in the event of abnormal perfusion imaging
CTPA=CT pulmonary angiogram. HRCT=high-resolution CT.
As our practice is based in the UK, the basic tenets of the British Thoracic Society guidelines20 for post-COVID follow-up, notably an initial radiographic and clinical assessment at 3 months, are assimilated within this pathway with the proviso that an earlier assessment might be necessary if symptoms require it. The proposed follow-up evaluation of patients with a known diagnosis of thromboembolism during acute COVID-19 draws from the European Society of Cardiology 2019 venous thromboembolism guidelines35 and the views of opinion leaders,36, 37 albeit with blanket use of perfusion imaging alongside the standard functional triage tools of transthoracic echocardiography and exercise testing. Local or regional specialist interstitial lung disease and pulmonary hypertension services are integral to supporting such a pathway.
Rationale for perfusion imaging in follow-up
Our proposal of perfusion imaging as a triage tool in post-COVID-19 recovery is informed by two considerations. First, by pre-pandemic understanding of the prognostic value of perfusion scintigraphy in the evaluation of chronic thromboembolic disease and chronic thromboembolic pulmonary hypertension.35, 38, 39, 40 Second, by the potential of perfusion imaging to examine the in-situ thrombotic small vessel signature of COVID-19.6, 8, 9, 10, 11, 12, 13, 14, 15, 41 It is widely accepted that distal subsegmental small vessel thrombi can be underestimated on conventional CTPA, which is tailored to look at the clot within the lumen rather than at the tissue perfusion beyond. This limitation of CTPA was considered to be of little consequence to overall clinical outcomes in the pre-pandemic context of venous thromboembolism.42 However, in the context of the small vessel pattern of COVID-19, this limitation needs to be revisited. Among published series of CTPA in acutely ill patients with COVID-19, some investigators report a distinct preponderance of exclusively branch vessel or distal thrombi.14, 15, 43, 44 Indeed, van Dam and colleagues43 proposed a CTPA phenotype involving peripheral lung segments, concluding that a combination of thromboembolic disease and in-situ thrombosis is likely in COVID-19. Given that the extent of microvascular injury syndrome can be underestimated by CTPA, the question arises as to whether we are under-detecting the extent of vascular pathology in COVID-19. In this context, a more physiological approach to imaging that looks beyond the clot, directly at lung perfusion, could be of value as a triage tool, contribute to understanding of the natural history of vascular pathophysiology, and inform therapeutic strategies.
VQ SPECT scintigraphy in follow-up
The key lung perfusion imaging modalities to consider for post-COVID-19 follow-up are novel spectral CT perfusion techniques—notably, dual-energy CT (DECT)—and the time-honoured VQ scintigraphy. The VQ scan, previously notorious as an unclear, hot-spot imaging technique, has evolved into a modern three-dimensional (3D) single-photon emission computed tomography with CT fusion (SPECT-CT) avatar with added CT lung overlay and fusion, conferring greater diagnostic certainty (appendix p 2). We share VQ SPECT images in two patients from the post-COVID-19 recovery cohort who presented with persistent breathlessness 5–6 weeks after initial symptoms (Figure 3, Figure 4 ). Of note, these patients were not diagnosed or treated for thromboembolic disease during acute illness.
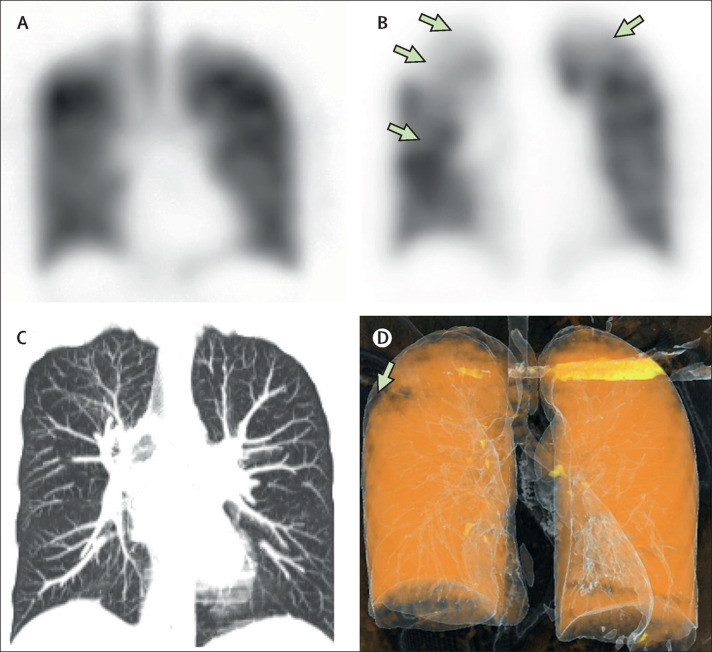
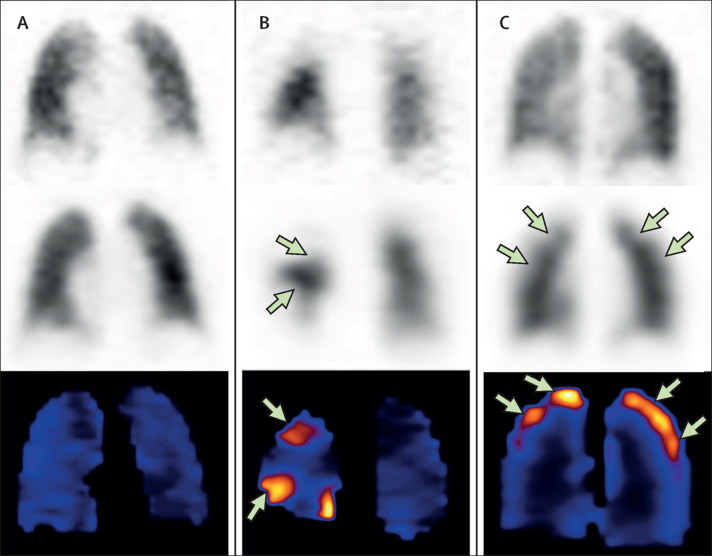
Figure 3.
Coronal VQ SPECT, lung CT, and DECT in patient X
Imaging in patient X, a 29-year-old woman, during the acute phase of COVID-19 and 6 weeks after the acute illness. (A, B) Coronal VQ SPECT 6 weeks after acute illness. (A) 81mKr ventilation coronal SPECT showing relatively preserved ventilation. (B) 99mTc MAA coronal perfusion SPECT showing subsegmental perfusion deficits (green arrows) in upper and middle lung zones. (C, D) Coronal lung CT and DECT lung perfusion 6 weeks earlier, during the acute phase of illness, showing no air-space changes in the lung. (D) Small perfusion defect on DECT lung perfusion (green arrow) identified retrospectively with the benefit of findings on the 6 week VQ SPECT scan. A CT pulmonary angiogram (not depicted) done in the acute phase of illness showed no macrothrombus. DECT=dual-energy CT. MAA=macroaggregated albumin. SPECT=single-photon emission computed tomography. VQ=ventilation perfusion.
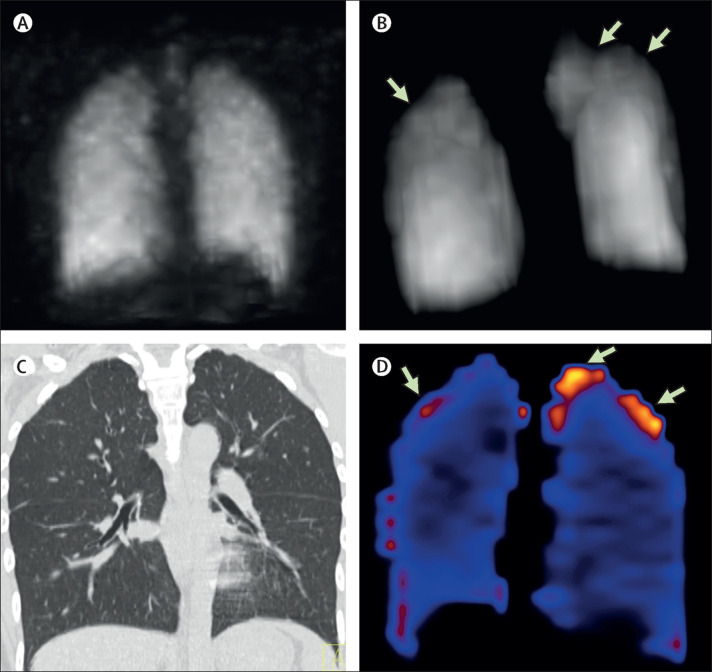
Figure 4.
VQ SPECT and coronal lung CT in patient Y
VQ SPECT-CT in a 22-year-old woman, 6 weeks after the acute COVID-19 illness. (A, B) 99mTc MAA perfusion coronal MIP (B), showing subtle, tiny peripheral subpleural perfusion deficits (green arrows) in the upper zones with relatively preserved 99mTc DTPA aerosol ventilation (A). (C) Coronal lung CT (from VQ SPECT-CT template) showing no abnormal lung morphology. (D) VQ parametric images showing VQ quotient abnormalities highlighted in pink-orange colour tones (green arrows) at sites of ventilation–perfusion discordance, representing ventilation–perfusion mismatch. This pattern of tiny subpleural upper zone ventilation–perfusion mismatches is atypical for classical pulmonary thromboembolism and taken in the COVID-19 context to represent residual small vessel insult. MAA=macroaggregated albumin. MIP=maximum intensity projection. DTPA=diethylenetriamine pentacetic acid. SPECT-CT=single-photon emission computed tomography with CT fusion. VQ=ventilation perfusion.
Given the in-situ thrombotic pathophysiology of COVID-19, we should also reconsider the patterns of perfusion deficits and ventilation–perfusion mismatches to expect in follow-up. In alignment with the aforementioned description of a distal vessel clot phenotype on CTPA,43 the perfusion pattern will depend on which segments of the vascular tree are affected. Proposed mismatch phenotypes on VQ SPECT are shown in figure 5 . A patchy, mottled peripheral pattern of perfusion mismatch (figure 5C) not conforming to typical segmental geometry might be the only marker of small vessel damage, similar to the pattern observed in patient Y (figure 4). Such atypical non-segmental mismatches are well described in pulmonary arterial hypertension-associated microangiopathy (figure 5C; eg, scleroderma, connective tissue disease, veno-occlusive disease, and sickle-cell disease).45, 46 As these perfusion defects are often subtle and diffuse, they can potentially be overlooked. In addition to this small vessel footprint, the component of large and medium vessel clot related to venous thromboembolism can result in a mixed phenotype of both mottled peripheral defects and classical segmental or subsegmental ventilation–perfusion mismatches (figure 5C), as also shown in patient X (figure 3). Perfusion defects described by Patel and colleagues14 on DECT perfusion imaging in acute severe COVID-19 pneumonia align with these phenotypes, capturing both venous thromboembolism and a small vessel angiopathy.
Figure 5.
Predicted COVID-19 VQ imaging phenotypes with normal, classical, and small vessel patterns
These images of classical vascular patterns are drawn from pre-COVID experience of VQ imaging. The proposed phenotypes are deduced from a combination of our CTPA and VQ experience in post-COVID-19 patients and the DECT COVID-19 literature. The top row shows 99mTc DTPA aerosol ventilation coronal SPECT slices, the middle row 99mTc MAA perfusion coronal SPECT slices, and the bottom row VQ quotient parametric images. (A) Uniform ventilation and perfusion pattern. (B) Classical segmental geometry of perfusion defects typical of venous thromboembolism, with corresponding ventilation–perfusion mismatch on VQ quotient images. (C) Non-geometric small, peripheral subpleural perfusion defects, with corresponding peripheral mismatch pattern of a small vessel angiopathy. CTPA=CT pulmonary angiogram. DECT=dual-energy CT. DTPA=diethylenetriamine pentacetic acid. MAA=macroaggregated albumin. SPECT=single-photon emission computed tomography. VQ=ventilation perfusion.
It is important to emphasise that ventilation–perfusion mismatches do not necessarily indicate an acute thromboembolic event. Reports of the natural history of reperfusion trajectories in the venous thromboembolism studies show that perfusion defects could persist in about 50% of patients, with resolution stabilising between 6 weeks to 6 months.47 However, when considered with symptoms and non-imaging investigations, this perfusion information can be used to trigger further anatomical imaging (figure 2). The extent of ventilation–perfusion mismatch can also be a useful index35, 38, 39, 40 when interpreted alongside functional indices of echocardiography and exercise physiology.35, 48 A normal VQ SPECT scan (figure 5A) essentially excludes clinically significant post-thromboembolic sequelae, with the caveat that it remains to be seen how VQ SPECT imaging responds to the more subtle footprints of COVID-19 small vessel disease.
It is worth being mindful, when using any perfusion technique, that classical segmental ventilation–perfusion mismatches (figure 5B) could occur with non-thrombotic conditions of the vascular tree, such as vasculitis and sarcoidosis.49 In the context of COVID-19 follow-up, some patterns of interstitial morphology, particularly those with large cystic air spaces, might show a relative ventilation–perfusion mismatch, with perfusion affected more than ventilation,50, 51 although this is easily resolved with modern SPECT-CT imaging with a CT template to corroborate lung morphology.
Novel CT lung perfusion techniques
Although VQ SPECT-CT scintigraphy is the accepted gold-standard screening tool for the evaluation of chronic thromboembolism,35 novel spectral CT perfusion techniques have been under investigation for several years, gaining more visibility in the COVID-19 context. Spectral or DECT perfusion relies on the way in which tissues of different densities handle different energy spectra. This enables contrast-enhanced iodine density maps of lung parenchyma to be computed that reflect regional blood flow. Such perfused blood volume (PBV) maps are surrogate markers of lung perfusion and add a physiological component to conventional CTPA (appendix p 3). Although not universally available, several centres with necessary CT hardware have been evaluating this technique in the context of COVID-19 acute illness.52, 53 Another modified CT method with the same goal is CT lung subtraction iodine mapping (CT-LSIM), which does not require special hardware; rather, it involves the subtraction of non-contrast CT from contrast-enhanced CTPA to produce surrogate parenchymal iodine maps.54, 55, 56
Both DECT and CT-LSIM hold exciting potential as a one-stop triad of perfusion mapping, imaging of luminal clot on CTPA, and visualisation of lung parenchymal changes (appendix p 3). However, the evaluation of these techniques, especially with regard to acute thromboembolic events, when air-space pathology might induce reflex changes in perfusion, is a work in progress to which the COVID-19 studies should contribute. Available evidence suggests that such perfusion information offers valuable physiological insights into acute COVID-19 pathophysiology,14, 52, 53, 57 and might have an important role in research, at least. Lang and colleagues52 reviewed a DECT series of 25 patients and concluded that COVID-19 pneumonia is associated with pulmonary vascular and perfusion derangements of uncertain mechanisms. Idilman and colleagues53 reported DECT perfusion defects in 8 of 31 patients with COVID-19 in lung zones unaffected by air-space changes, the majority (6 of 8) without CTPA evidence of macroscopic thromboembolism. Patel and colleagues14 analysed DECT imaging in 20 patients with severe COVID-19 pneumonia, alongside physiological and haematological parameters; they found extensive pulmonary perfusion and structural vascular abnormalities, and proposed that pulmonary angiopathy and thrombosis were major contributors to pulmonary pathophysiology. They observed enlarged segmental and subsegmental vessels in COVID-19 pneumonia, in keeping with several such previous reports.52, 58 The authors highlighted the so-called vascular tree-in-bud sign, hypothesising that this might be a marker of in-situ small vessel thrombosis and angiogenesis. This imaging-based thrombotic hypothesis,14 although unproven by histopathological evidence, points yet again to the small vessel target of disease.
In a preliminary post-COVID-19 follow-up cohort, Patelli and colleagues59 reported CTPA findings in five patients with persistent breathlessness. They supplemented a CTPA readout with a rudimentary computer-aided perfusion map of lung contrast distribution and reported perfusion abnormalities without any related structural lung abnormality in three such patients, speculating on the possibility of unresolved microvasculature damage.
A meta-analysis60 of pre-pandemic spectral DECT perfusion studies examined available evidence for DECT-CTPA with iodine PBV maps to establish whether it can reliably diagnose acute pulmonary embolism or chronic thromboembolic disease and obviate the need for additional VQ scans in patients already undergoing CTPA. The meta-analysis included four eligible studies with 206 examinations of spectral DECT-CTPA and PBV maps with one or the other form of VQ scintigraphy as reference standard. The authors concluded that data on spectral DECT-CTPA for pulmonary embolism remains promising, but only small studies with methodological issues are available. Similar to other investigators, they found that evidence was best for chronic pulmonary embolism and chronic thromboembolic pulmonary hypertension.46, 60, 61 The authors emphasised the need for large prospective studies with a robust composite reference standard, including modern CTPA and VQ scans with SPECT-CT and formalised follow-up in unselected patients with suspected acute and chronic pulmonary embolism.
The validation of CT-LSIM is also a work in progress; published studies on chronic thromboembolic disease are promising,54, 55 and the outcome of the UK INSPIRE trial, examining CT-LSIM in chronic pulmonary thromboembolic disease against VQ SPECT reference imaging,62 should provide further information on the usefulness of this technique.
Other investigators have looked at the potential of gadolinium-enhanced MRI pulmonary angiography and 3D lung perfusion (appendix p 3). The technique has shown comparable sensitivity to planar and SPECT perfusion scintigraphy for diagnosing chronic thromboembolic disease.63 The absence of ionising radiation is a singular advantage of MRI; however, expertise and often the availability of relevant resources are restricted to specialist centres.
VQ SPECT versus CT perfusion in the follow-up pathway
Perfusion scintigraphy relies on the capture of intravenously injected technetium99m-labelled macro-aggregated albumin particles on first pass at the pulmonary arteriolar level, directly mirroring regional lung perfusion, whereas CT perfusion iodine maps are surrogate markers of perfusion. Assumptions inherent in surrogate methods, both technique-related and physiological, could affect the resulting perfusion maps.60 The VQ scan is also subject to limitations, but the link between the imaging method and tissue perfusion is more direct and the technique is the reference standard in non-COVID-19 venous thromboembolism follow-up pathways.36, 37 Therefore, if availability and expertise allow, VQ SPECT-CT remains the more validated and mature modality to use in the follow-up of pulmonary vascular sequelae after COVID-19. From a research perspective, this presents an excellent opportunity to add to the compendium of experience in evaluating DECT and CT-LSIM perfusion in parallel with VQ SPECT-CT, particularly as perfusion deficits in small vessel disease could bring new imaging insights (panel ).
Panel. Research priorities for investigating pulmonary vascular disease and sequelae after COVID-19.
-
•
Evaluation of the prevalence and extent of perfusion abnormalities in survivors of COVID-19 across the spectrum of illness—from non-hospitalised patients to those in the intensive care unit—and their effect on functional capacity, physiology, and quality of life
-
•
Assessment of the effect of clinical trial interventions and hospital protocols (eg, anticoagulation strategies during and after admission) on residual perfusion abnormalities at follow-up
-
•
Evaluation of CT pulmonary angiogram (CTPA) phenotypes in the acute stage, with follow-up of residual perfusion deficit phenotypes at 3–6 months to assess the dominant residual site of COVID-19 vasculopathy
-
•
Evaluation of novel CT perfusion methods—dual-energy CT (DECT) and CT lung subtraction iodine mapping (CT-LSIM)—versus the reference standard methods of VQ single-photon emission computed tomography (SPECT) and CTPA in post-COVID-19 follow-up cohorts
Although most CT perfusion techniques available in clinical practice rely on a static lung CT ventilation surrogate, VQ SPECT-CT uses a dynamic physiological alveolar ventilation map with radio-labelled aerosols or gas to assess physiological ventilation–perfusion concordance or discordance. The benefit of this paired ventilation–perfusion rubric, alongside a structural lung CT template, is to improve interpretation by ascertaining ventilation–perfusion mismatch. VQ scan abnormalities of a mostly matched nature can occur with airway and primary parenchymal pathology, with the caveat of some exceptions in interstitial fibrosis.50, 51 However, in the absence of local VQ SPECT infrastructure, the choice of perfusion imaging technique is best dictated by local resources and expertise, given that some centres have a substantial body of experience in CT techniques. Importantly, the interpretative criteria of perfusion imaging in the COVID-19 context, whatever the technique, must go beyond the conventional classical segmental, subsegmental approach, in looking for subtle distal peripheral footprints, to capture residual small vessel insult.
Challenges of performing VQ SPECT in the COVID-19 era
Although a combined ventilation and perfusion procedure is desirable in the post-COVID-19 patient cohort, service delivery has not been consistent because ventilation scintigraphy was discontinued in many nuclear medicine centres at the start of the COVID-19 pandemic on the basis of concerns raised by many international professional nuclear medicine societies.64, 65, 66 The ventilation phase involves the inhalation of radio-labelled aerosols or gas to map regional alveolar ventilation. At the heart of these concerns is the risk and the perception of risk with respect to the aerosol-generating potential (AGP) of radio-nebulisers. In the UK, Public Health England67 proffers that nebulisation droplets are derived from the machine, not the patient, and do not therefore have virus-transmitting potential. WHO68 and the US Centers for Disease Control and Prevention69 conclude in their advisories that there is a possible risk, and the European Centre for Disease Prevention and Control revised their advisory in July, 2020,70 to conclude that the infectious risk of administration of nebulised treatment is unclear, there being no consensus on their classification as AGP. This subject is naturally very emotive, complicated by conflicting perceptions of AGP risks. A systematic review of the SARS studies71 acknowledged that substantial research gaps exist in the epidemiology of transmission risks during nebulisation. Our understanding of available guidance67 and the evidence base71, 72, 73, 74 is that the generation of radio-aerosols or radio-labelled gases is not of virus-carrying potential, given that it is conducted in a separate compartment and mitigated by a single-use patient administration set with unidirectional airflow. However, uncertainty remains as to whether exhaled aerosols, not mitigated by mouthpiece design and filters, might be a source of infection. Additionally, coughing—potentially provoked by tidal breathing efforts by mouth—constitutes a discrete mini-AGP event.
Importantly, as VQ SPECT is not being proposed for the acute COVID-19 illness, but for patients who are being followed up after COVID-19, the risks should be safely managed. Indeed, in our view, VQ imaging has no real practical place in the evaluation of acute pulmonary thromboembolism during the acute COVID-19 illness, for which CTPA and point-of-care tests such as leg compression ultrasound and echocardiography are central. In the post-COVID-19 cohort, it should be feasible to re-establish the service, coordinating with local infection control units with regard to cleaning regimens, air-exchange systems, and appropriate personal protective equipment. Additionally, COVID-19 PCR testing could be considered as an added layer of risk mitigation to ensure a low-risk environment.
Conclusion
Until 5–7 years ago, pulmonary thromboembolism was viewed as an acute illness with a low prevalence (<4%) of long-term sequelae of chronic thromboembolic pulmonary hypertension.75, 76 It is now well recognised that a post-pulmonary embolism clinical syndrome, resulting from a heterogeneous mix of factors, from deconditioning to haemodynamic derangements, occurs in almost 40–50% of patients with venous thromboembolism, affecting quality of life long after an acute thromboembolic event.75, 77, 78
Although the long-term outcomes in survivors of COVID-19 are unknown at present, should thrombotic sequelae prove to be clinically significant, these have the potential to become a public health problem. Lung perfusion imaging offers a simple triage tool, within the broader panel of investigations, to improve understanding of the natural history of thromboembolic phenomena in COVID-19 and contribute, alongside tests of exercise physiology and function, towards separating haemodynamic sequelae from deconditioning and dysfunctional breathing-related functional limitations. We believe that such imaging should be embedded in routine post-COVID-19 follow-up pathways. On the research front, should immunomodulatory or anti-complement treatments emerge that are targeted at reducing the inflammatory cascade in COVID-19, then follow-up with objective, robust reference tools will be desirable to monitor benefits in the long term, in both treated and untreated cohorts. We believe that imaging specialists should be involved early in the formulation of post-discharge pathways that are tailored to local expertise and resources. In this context, imaging departments and, specifically, nuclear medicine should be supported to adapt and manage risks to provide an appropriate service for COVID-19 survivors.
Search strategy and selection criteria
We searched PubMed for articles published in or translated into the English language between Jan 1, 2001, and Aug 10, 2020, using combinations of the terms “COVID-19”, “SARS”, “MERS”, “thromboembolism”, “PE”, “VTE”, “thrombosis”, “small vessel”, “microangiopathy, “CTED”, “CTPEH”, “post-PE syndrome”, “SSPE subsegmental pulmonary emboli”, “post-COVID follow up”, “post-COVID recovery”, “lung function”, “diffusing capacity”, “pulmonary”, “lung perfusion”, “perfusion defects”, “VQ”, “VQ SPECT”, “DECT perfusion”, “spectral CT”, “CTPA”, “MRI perfusion”, “aerosol”, “AGP”, “nebulizer”, and “nuclear medicine guidelines”. We determined relevance on the basis of content. We also found articles through the authors' personal files and from references cited in retrieved articles. We searched and summarised international guidelines—for instance, those issued by WHO, the US Centers for Disease Control and Prevention, the UK National Health Service and Public Health England, and the International Atomic Energy Agency. The final reference list was generated on the basis of relevance to this Personal View, with the aim of advancing approaches to follow-up of pulmonary vascular sequelae.
Acknowledgments
Acknowledgments
We thank Hermes Medical Solutions AB, Stockholm, Sweden for complimentary use of the ventilation perfusion (VQ) Quotient Lung Analysis software in analysing VQ single-photon emission computed tomography (SPECT) images included in this Personal View.
Contributors
RTD, OMK, and DG conceptualised the manuscript. RTD, OMK, and DG wrote the manuscript with contributions from LH. LH produced the algorithms with input from DG, OMK, and RTD. RTD, DG, OMK, LH, KM, MP, HB, GR, AV, and IW searched the clinical and imaging studies. AV, MP, KM, OMK, IW, PM, SD, ND, and RTD researched the ventilation perfusion and aerosol-generating potential studies and provided intellectual input on this subject matter. AV, RTD, DG, GR, and HB provided the images and cases. RTD, OMK, LH, AV, and DG did the manuscript revisions. All authors approved the revised manuscript.
Declaration of interests
RTD reports the use of ventilation perfusion (VQ) Quotient Lung Analysis software, provided by Hermes Medical Solutions, Sweden, on a no-fee gratis basis to analyse some of the VQ images displayed in this Personal View. DG reports speaking and consultancy fees from Bayer Pharmaceuticals, and speaking fees from Actelion, outside the submitted work. All other authors declare no competing interests.
Supplementary Material
References
- 1.Spagnolo P, Balestro E, Aliberti S. Pulmonary fibrosis secondary to COVID-19: a call to arms? Lancet Respir Med. 2020;8:750–752. doi: 10.1016/S2213-2600(20)30222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee L, Iyer S, Jose RJ, Manuel A. COVID-19 follow-up planning: what will we be missing? ERJ Open Res. 2020;6:00198–02020. doi: 10.1183/23120541.00198-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mo X, Jian W, Su Z. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020;55 doi: 10.1183/13993003.01217-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wichmann D, Sperhake J-P, Lütgehetmann M. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020;173:268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klok FA, Kruip MJHA, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helms J, Tacquard C, Severac F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oxley TJ, Mocco J, Majidi S. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ackermann M, Verleden SE, Kuehnel M. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teuwen L-A, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20:389–391. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGonagle D, O'Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020;2:e437–e445. doi: 10.1016/S2665-9913(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lax SF, Skok K, Zechner P. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. 2020;173:350–361. doi: 10.7326/M20-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lax SF, Skok K, Trauner M. Pulmonary arterial thrombosis as an important complication of COVID-19 pulmonary disease: letter to the editor. Virchows Arch. 2020;477:467–468. doi: 10.1007/s00428-020-02896-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merrill JT, Erkan D, Winakur J, James JA. Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat Rev Rheumatol. 2020;16:581–589. doi: 10.1038/s41584-020-0474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel BV, Arachchillage DJ, Ridge CA. Pulmonary angiopathy in severe COVID-19: physiologic, imaging and hematologic observations. Am J Respir Crit Care Med. 2020;202:690–699. doi: 10.1164/rccm.202004-1412OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucatelli P, Del Monte M, De Rubeis G. Did we turn a blind eye? The answer is simply there. Peripheral pulmonary vascular thrombosis in COVID-19 patients explains sudden worsening of clinical conditions. Imaging. 2020;12:4–7. [Google Scholar]
- 16.Overstad S, Tjonnfjord E, Garabet L. Venous thromboembolism and coronavirus disease 2019 in an ambulatory care setting—a report of 4 cases. Thromb Res. 2020;194:116–118. doi: 10.1016/j.thromres.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gervaise A, Bouzad C, Peroux E, Helissey C. Acute pulmonary embolism in non-hospitalized COVID-19 patients referred to CTPA by emergency department. Eur Radiol. 2020 doi: 10.1007/s00330-020-06977-5. published online June 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uppuluri EM, Shapiro NL. Development of pulmonary embolism in a nonhospitalized patient with COVID-19 who did not receive venous thromboembolism prophylaxis. Am J Health Syst Pharm. 2020 doi: 10.1093/ajhp/zxaa286. published online Aug 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klok FA, Boon GJAM, Barco S. The Post-COVID-19 Functional Status (PCFS) scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020;56 doi: 10.1183/13993003.01494-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.British Thoracic Society COVID-19: information for the respiratory community. July, 2020. https://www.brit-thoracic.org.uk/about-us/covid-19-information-for-the-respiratory-community/
- 21.Polastri M, Nava S, Clini E, Vitacca M, Gosselink R. COVID-19 and pulmonary rehabilitation: preparing for phase three. Eur Respir J. 2020;55 doi: 10.1183/13993003.01822-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halpin SJ, McIvor C, Whyatt G. Post-discharge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2020 doi: 10.1002/jmv.26368. published online July 30. [DOI] [PubMed] [Google Scholar]
- 23.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waldmann C, Meyer J, Slack A. FICM position statement and provisional guidance: recovery and rehabilitation for patients following the pandemic. May, 2020. https://www.ficm.ac.uk/sites/default/files/ficm_rehab_provisional_guidance.pdf
- 25.Barker-Davies RM, O'Sullivan O, Senaratne KPP. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54:949–959. doi: 10.1136/bjsports-2020-102596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liang T. Handbook of COVID-19 prevention and treatment compiled according to clinical experience. March 18, 2020. https://esge.org/documents/Handbook_of_COVID-19_Prevention_and_Treatment.pdf
- 27.Wang Y, Dong C, Hu Y. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020;296:E55–E64. doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frija-Masson J, Debray M-P, Gilbert M. Functional characteristics of patients with SARS-CoV-2 pneumonia at 30 days post infection. Eur Respir J. 2020;56 doi: 10.1183/13993003.01754-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiang-Hua Y, Le-Min W, Ai-Bin L. Severe acute respiratory syndrome and venous thromboembolism in multiple organs. Am J Respir Crit Care Med. 2010;182:436–437. doi: 10.1164/ajrccm.182.3.436. [DOI] [PubMed] [Google Scholar]
- 30.Ding Y, Wang H, Shen H. The clinical pathology of severe acute respiratory syndrome (SARS): a report from China. J Pathol. 2003;200:282–289. doi: 10.1002/path.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hui DS, Joynt GM, Wong KT. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60:401–409. doi: 10.1136/thx.2004.030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hui DS, Wong KT, Ko FW. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest. 2005;128:2247–2261. doi: 10.1378/chest.128.4.2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ngai JC, Ko FW, Ng SS, To KW, Tong M, Hui DS. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15:543–550. doi: 10.1111/j.1440-1843.2010.01720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park WB, Jun KI, Kim G. Correlation between pneumonia severity and pulmonary complications in Middle East respiratory syndrome. J Korean Med Sci. 2018;33:e169. doi: 10.3346/jkms.2018.33.e169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Konstantinides SV, Meyer G, Becattini C. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) Eur Respir J. 2019;54 doi: 10.1183/13993003.01647-2019. [DOI] [PubMed] [Google Scholar]
- 36.McCabe C, Dimopoulos K, Pitcher A. Chronic thromboembolic disease following pulmonary embolism: time for a fresh look at old clot. Eur Respir J. 2020;55 doi: 10.1183/13993003.01934-2019. [DOI] [PubMed] [Google Scholar]
- 37.Pugliese SC, Kawut SM. The post-pulmonary embolism syndrome: real or ruse? Ann Am Thorac Soc. 2019;16:811–814. doi: 10.1513/AnnalsATS.201901-061PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pesavento R, Filippi L, Palla A. Impact of residual pulmonary obstruction on the long-term outcome of patients with pulmonary embolism. Eur Respir J. 2017;49 doi: 10.1183/13993003.01980-2016. [DOI] [PubMed] [Google Scholar]
- 39.Marconi L, Palla A, Cestelli L. Should perfusion scintigraphy be performed to follow patients with acute pulmonary embolism? When? J Nucl Med. 2019;60:1134–1139. doi: 10.2967/jnumed.118.222737. [DOI] [PubMed] [Google Scholar]
- 40.Meneveau N, Ider O, Seronde M-F. Long-term prognostic value of residual pulmonary vascular obstruction at discharge in patients with intermediate to high-risk pulmonary embolism. Eur Heart J. 2013;34:693–701. doi: 10.1093/eurheartj/ehs365. [DOI] [PubMed] [Google Scholar]
- 41.Bösmüller H, Traxler S, Bitzer M. The evolution of pulmonary pathology in fatal COVID-19 disease: an autopsy study with clinical correlation. Virchows Arch. 2020;477:349–357. doi: 10.1007/s00428-020-02881-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carrier M, Righini M, Wells PS. Subsegmental pulmonary embolism diagnosed by computed tomography: incidence and clinical implications. A systematic review and meta-analysis of the management outcome studies. J Thromb Haemost. 2010;8:1716–1722. doi: 10.1111/j.1538-7836.2010.03938.x. [DOI] [PubMed] [Google Scholar]
- 43.van Dam LF, Kroft LJM, van der Wal LI. Clinical and computed tomography characteristics of COVID-19 associated acute pulmonary embolism: a different phenotype of thrombotic disease? Thromb Res. 2020;193:86–89. doi: 10.1016/j.thromres.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cavagna E, Muratore F, Ferrari F. Pulmonary thromboembolism in COVID-19: venous thromboembolism or arterial thrombosis? Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200289. published online July 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chan K, Ioannidis S, Coghlan JG, Hall M, Schreiber BE. Pulmonary arterial hypertension with abnormal V/Q single-photon emission computed tomography. JACC Cardiovasc Imaging. 2018;11:1487–1493. doi: 10.1016/j.jcmg.2017.07.026. [DOI] [PubMed] [Google Scholar]
- 46.Giordano J, Khung S, Duhamel A. Lung perfusion characteristics in pulmonary arterial hypertension (PAH) and peripheral forms of chronic thromboembolic pulmonary hypertension (pCTEPH): dual-energy CT experience in 31 patients. Eur Radiol. 2017;27:1631–1639. doi: 10.1007/s00330-016-4500-6. [DOI] [PubMed] [Google Scholar]
- 47.Nijkeuter M, Hovens MMC, Davidson BL, Huisman MV. Resolution of thromboemboli in patients with acute pulmonary embolism: a systematic review. Chest. 2006;129:192–197. doi: 10.1378/chest.129.1.192. [DOI] [PubMed] [Google Scholar]
- 48.Klok FA, Couturaud F, Delcroix M, Humbert M. Diagnosis of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Eur Respir J. 2020;55 doi: 10.1183/13993003.00189-2020. [DOI] [PubMed] [Google Scholar]
- 49.Narechania S, Renapurkar R, Heresi GA. Mimickers of chronic thromboembolic pulmonary hypertension on imaging tests: a review. Pulm Circ. 2020;10 doi: 10.1177/2045894019882620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Strickland NH, Hughes JM, Hart DA, Myers MJ, Lavender JP. Cause of regional ventilation-perfusion mismatching in patients with idiopathic pulmonary fibrosis: a combined CT and scintigraphic study. AJR Am J Roentgenol. 1993;161:719–725. doi: 10.2214/ajr.161.4.8372745. [DOI] [PubMed] [Google Scholar]
- 51.Suga K, Kawakami Y, Koike M, Iwanaga H, Matsunaga N. Characteristic crescentic subpleural lung zones with high ventilation (V)/perfusion (Q) ratios in interstitial pneumonia on V/Q quotient SPECT. Nucl Med Commun. 2009;30:881–889. doi: 10.1097/MNM.0b013e328330571d. [DOI] [PubMed] [Google Scholar]
- 52.Lang M, Som A, Carey D. Pulmonary vascular manifestations of COVID-19 pneumonia. Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Idilman I, Dizman GT, Duzgun SA. Lung and kidney perfusion deficits diagnosed by dual-energy computed tomography in patients with COVID-19-related systemic microangiopathy. Eur Radiol. 2020 doi: 10.1007/s00330-020-07155-3. published online Aug 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tamura M, Yamada Y, Kawakami T. Diagnostic accuracy of lung subtraction iodine mapping CT for the evaluation of pulmonary perfusion in patients with chronic thromboembolic pulmonary hypertension: correlation with perfusion SPECT/CT. Int J Cardiol. 2017;243:538–543. doi: 10.1016/j.ijcard.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 55.Grob D, Smit E, Prince J. Iodine maps from subtraction CT or dual-energy CT to detect pulmonary emboli with CT angiography: a multiple-observer study. Radiology. 2019;292:197–205. doi: 10.1148/radiol.2019182666. [DOI] [PubMed] [Google Scholar]
- 56.Dissaux B, Le Floch P-Y, Robin P. Pulmonary perfusion by iodine subtraction maps CT angiography in acute pulmonary embolism: comparison with pulmonary perfusion SPECT (PASEP trial) Eur Radiol. 2020;30:4857–4864. doi: 10.1007/s00330-020-06836-3. [DOI] [PubMed] [Google Scholar]
- 57.Santamarina MG, Boisier D, Contreras R, Baque M, Volpacchio M, Beddings I. COVID-19: a hypothesis regarding the ventilation-perfusion mismatch. Crit Care. 2020;24:395. doi: 10.1186/s13054-020-03125-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Parry AH, Wani AH, Yaseen M. Spectrum of chest computed tomographic (CT) findings in coronavirus disease-19 (COVID-19) patients in India. Eur J Radiol. 2020;129 doi: 10.1016/j.ejrad.2020.109147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Patelli G, Paganoni S, Besana F. Preliminary detection of lung hypoperfusion in discharged Covid-19 patients during recovery. Eur J Radiol. 2020;129 doi: 10.1016/j.ejrad.2020.109121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lysdahlgaard S, Hess S, Gerke O, Weber Kusk M. A systematic literature review and meta-analysis of spectral CT compared to scintigraphy in the diagnosis of acute and chronic pulmonary embolisms. Eur Radiol. 2020;30:3624–3633. doi: 10.1007/s00330-020-06735-7. [DOI] [PubMed] [Google Scholar]
- 61.Masy M, Giordano J, Petyt G. Dual-energy CT (DECT) lung perfusion in pulmonary hypertension: concordance rate with V/Q scintigraphy in diagnosing chronic thromboembolic pulmonary hypertension (CTEPH) Eur Radiol. 2018;28:5100–5110. doi: 10.1007/s00330-018-5467-2. [DOI] [PubMed] [Google Scholar]
- 62.Shahin Y, Johns C, Karunasaagarar K, Kiely DG, Swift AJ. IodiNe Subtraction mapping in the diagnosis of Pulmonary chronIc thRomboEmbolic disease (INSPIRE): rationale and methodology of a cross-sectional observational diagnostic study. Contemp Clin Trials Commun. 2019;15 doi: 10.1016/j.conctc.2019.100417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johns CS, Swift AJ, Rajaram S. Lung perfusion: MRI vs SPECT for screening in suspected chronic thromboembolic pulmonary hypertension. J Magn Reson Imaging. 2017;46:1693–1697. doi: 10.1002/jmri.25714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Society of Nuclear Medicine and Molecular Imaging COVID-19 and ventilation/perfusion (V/Q) lung studies. March 19, 2020. https://www.snmmi.org/NewsPublications/NewsDetail.aspx?ItemNumber=33543
- 65.International Atomic Energy Agency COVID-19 pandemic: technical guidance for nuclear medicine departments. July, 2020. https://www-pub.iaea.org/MTCD/Publications/PDF/COVID19_web.pdf
- 66.Buscombe JR, Notghi A, Croasdale J. COVID-19: guidance for infection prevention and control in nuclear medicine. Nucl Med Commun. 2020;41:499–504. doi: 10.1097/MNM.0000000000001206. [DOI] [PubMed] [Google Scholar]
- 67.Public Health England COVID-19: infection prevention and control guidance. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/893320/COVID-19_Infection_prevention_and_control_guidance_complete.pdf
- 68.WHO Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. March 27, 2020. https://apps.who.int/iris/bitstream/handle/10665/331601/WHO-2019-nCoV-Sci_Brief-Transmission_modes-2020.1-eng.pdf
- 69.Centers for Disease Conrol and Prevention Clinical questions about COVID-19: questions and answers. July, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html
- 70.European Centre for Disease Prevention and Control Infection prevention and control and preparedness for COVID-19 in healthcare settings—fifth update. Oct 6, 2020. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings
- 71.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Raboud J, Shigayeva A, McGeer A. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One. 2010;5 doi: 10.1371/journal.pone.0010717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Loeb M, McGeer A, Henry B. SARS among critical care nurses, Toronto. Emerg Infect Dis. 2004;10:251–255. doi: 10.3201/eid1002.030838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wong TW, Lee CK, Tam W. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerg Infect Dis. 2004;10:269–276. doi: 10.3201/eid1002.030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kahn SR, Hirsch AM, Akaberi A. Functional and exercise limitations after a first episode of pulmonary embolism. Chest. 2017;151:1058–1068. doi: 10.1016/j.chest.2016.11.030. [DOI] [PubMed] [Google Scholar]
- 76.Konstantinides SV. Chronic thromboembolic disease following pulmonary embolism: more work ahead. Eur Respir J. 2020;55 doi: 10.1183/13993003.00229-2020. [DOI] [PubMed] [Google Scholar]
- 77.Kahn SR, Houweling AH, Granton J, Rudski L, Dennie C, Hirsch A. Long-term outcomes after pulmonary embolism: current knowledge and future research. Blood Coagul Fibrinolysis. 2014;25:407–415. doi: 10.1097/MBC.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 78.Klok FA, van der Hulle T, den Exter PL, Lankeit M, Huisman MV, Konstantinides S. The post-PE syndrome: a new concept for chronic complications of pulmonary embolism. Blood Rev. 2014;28:221–226. doi: 10.1016/j.blre.2014.07.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.