Abstract
Objective
Hospital-acquired infections (HAIs) are frequent complications among acute patients hospitalized in neurological units, especially among those hospitalized for stroke. This study aimed to investigate if enhanced hygienic measures, including the systematic use of personal protective equipment (PPE), determined a decrease in HAI during the recent COVID-19 outbreak in “COVID-free” neurological units.
Methods
Patients hospitalized in neurology and stroke units of Policlinico Umberto I Hospital in Rome from March 8, 2020 and discharged prior to May 31, 2020 were included in the study and compared with patients hospitalized during the same period in 2019.
Results
A total of 319 patients were included in the study (n = 103 in 2020, n = 216 in 2019). Among patients hospitalized in 2019, the incidence of HAIs was 31.5% (95% confidence interval (CI): 0.25–0.38), compared with 23.3% (95% CI: 0.15–0.32) in 2020 (p = 0.12). Multivariable logistic regression showed that hospitalization during 2020 was independently associated with a lower risk of HAIs (odds ratio: 0.34, 95% CI:0.16–0.71, p = 0.004). Poisson regression models showed that hospitalization during 2020 was also independently associated with both a lower number of HAIs (relative risk [RR]: 0.56, 95% CI:0.38–0.81, p = 0.01) and a lower number of prescribed antibiotics per patient (RR: 0.66, 95% CI: 0.49–0.87, p = 0.02).
Conclusion
Our study design provides evidence regarding the impact of stricter hygienic measures, such as increased PPE use, on HAIs. Larger studies are needed to support the extension of preventive measures even after the COVID-19 outbreak in order to limit the occurrence of HAIs.
Keywords: COVID-19, Sars-CoV-2, Hospital infections, Stroke unit, Neurology unit
Highlights
-
•
During the COVID-19 outbreak, stricter hygienic measures were followed in hospitals.
-
•
Our study explores the impact of such measures on Hospital-Acquired Infections (HAI).
-
•
A reduced risk of HAI was observed in our units compared with the previous year.
-
•
A significant decrease in antibiotic prescription was also observed.
-
•
An extension of stricter hygienic measures beyond the pandemic could be beneficial.
1. Introduction
The first autochthonous severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection-associated syndrome (COVID-19) in Italy was diagnosed in the second half of February and the infection rapidly spread across the country during the subsequent weeks [1,2]. During this COVID-19 pandemic, an extraordinary increase in the use of personal protective equipment (PPE) was implemented for both healthcare workers and patients [3,4]. Moreover, greater attention was given to personal hygienic precautions, such as hand washing and medical equipment disinfection [5]. Both PPE and hand hygiene are considered powerful preventive measures against hospital-acquired infections (HAIs) [6,7]. HAIs represent a frequent and serious complication among hospitalized patients, which can result in increased morbidity and mortality rates and costs [8]. Despite some contrasting results, HAIs represent a particularly frequent complication among hospitalized neurological patients, especially among those suffering from stroke or other conditions burdened by disability and dysphagia [9]. Recent European reports have depicted a challenging situation in Italy in terms of HAI-related deaths and antimicrobial resistance [10,11].
With this background, we aimed to analyze the incidence of HAIs among patients hospitalized in neurological units during the COVID-19 outbreak in Italy as compared with the same period of the previous year.
2. Methods
The study was conducted according to STROBE guidelines as a retrospective case-control study and approved by the local Ethics committee. Data from patients hospitalized in the neurology and stroke units of Policlinico Umberto I Hospital in Rome from March 8, 2020 and discharged prior to May 31, 2020 were retrospectively reviewed (study group) and compared with hospitalized patients during the same period in 2019 (control group). The neurology and stroke divisions, which usually include a total of 42 beds, were considered “COVID-free” from the beginning of the pandemic and the number of beds was limited to 23. The following hygienic measures were adopted in our units during the COVID-19 outbreak: All patients wore a surgical mask during the hospital staying; healthcare workers systematically used protective face masks (FFP2 or surgical depending on whether the contact with patients was either direct or indirect), as well as disposable coats, gloves and safety goggles for eye protection; a distance of at least 1.5 m between hospital beds was also guaranteed. The study included patients who came to neurological units directly from the emergency room (ER). In order to ensure the homogeneity of the study setting and avoid possible confounding factors, patients transferred to our unit from wards other than the ER were excluded from the study. This study design gave us the opportunity to evaluate the impact of increased PPE use without the confounding effect of SARS-CoV-2 co-infection.
We collected demographic data, information on medical comorbidities, length and reason of hospitalization, number of invasive devices (urinary catheter, peripheral venous line, central venous line, nasogastric tubes, etc.), occurrence and number of HAIs, and the number of prescribed antibiotics. Antibiotic prophylaxis was never used in any patient during both years, and no antibiotic was prescribed before the occurrence of a HAI. HAIs were defined as infections occurring after at least 48 h of hospitalization [12]. We also included aspiration pneumonias occurring after this time point so as to encompass the whole spectrum of infections that may complicate neurological unit hospitalization.
The primary outcome of our study was to assess possible differences in HAIs and antibiotic prescriptions between study group patients hospitalized during the COVID-19 outbreak and control group patients hospitalized during the same period in 2019.
2.1. Statistical analysis
Descriptive statistic methods and data visualization were used to assess data distribution. Comparisons across means were performed with independent sample t-test in cases of normal distribution, whereas the Mann-Whitney U test was used in cases of non-normal distribution. Comparisons across proportions were performed with Fisher's exact test.
A multivariable logistic regression model (M0) was elaborated to evaluate the effect of hospitalization in 2020 on the presence of HAIs. The model was corrected for the number of invasive devices and medical comorbidities, age, sex, and diagnosis of ischemic/hemorrhagic stroke. The variable “number of comorbidities” was obtained by the sum of the medical comorbidities (i.e diabetes, arterial hypertension, history of previous cancer, obesity, history of previous stroke, chronic kidney failure, chronic obstructive pulmonary disease, peripheral arterial disease and neurodegenerative diseases) reported during patients' previous medical history. This choice allowed us to reduce the number of covariates included in the model and to obtain an event per variable (EPV) of 15.
Due to a Poisson distribution of the dependent variable, Poisson generalized linear models were elaborated to assess the effect of hospitalization in 2020 on the number of infections (M1) and antibiotics (M2) per patient. M1 and M2 were corrected for the same covariates as M0. Analyses were performed and figures generated using R 3.5.1 (R Project for Statistical Computing, Vienna, Austria).
3. Results
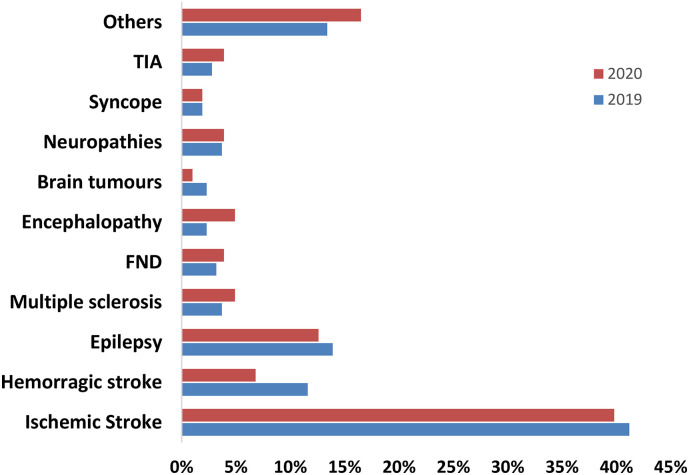
A total of 319 patients were included in the study according to study criteria. This figure included 216 control group patients hospitalized in 2019 and 103 study group patients hospitalized in 2020, representing a 52.3% decrease in the hospitalization rate in our units in 2020. Clinical and demographic data of the study and control groups are reported in Table 1 . Ischemic stroke was the most frequent cause of hospitalization, accounting for 89 patients in 2019 and 41 in 2020, whereas hemorrhagic stroke was diagnosed in 25 and 7 subjects in 2019 and 2020, respectively. The causes of hospitalization in study and control patients are detailed in Fig. 1 . Among patients with neurodegenerative diseases, the most frequent was Alzheimer's disease, observed in 9 subjects during 2019 and in 6 during 2020, followed by Parkinson's Disease, accounting for 8 and 3 patients in 2019 and 2020, respectively.
Table 1.
Demographic and clinical characteristics stratified by year of hospitalization.
| 2019 N = 216 pts. | 2020 N = 103 pts | p value | |
|---|---|---|---|
| Age, n, mean (SD) | 65.1 (18.8) | 65.4 (17.7) | 0.9 |
| Female sex, n, % | 110 (50.9) | 40 (38.8) | 0.04* |
| Arterial hypertension, n, % | 133 (61.6) | 62 (60.2) | 0.8 |
| Diabetes, n, % | 35 (16.3) | 24 (23.3) | 0.13 |
| Cardiopathy, n, % | 61 (28.2) | 32 (31.1) | 0.6 |
| COPD, n, % | 16 (7.4) | 8 (7.8) | 0.9 |
| History of cancer, n, % | 26 (12) | 15 (14.6) | 0.5 |
| Obesity, n, % | 7 (3.2) | 7 (6.8) | 0.1 |
| Neurodegenerative disease, n, % | 23 (10.6) | 16 (15.5) | 0.2 |
| Chronic kidney failure, n, % | 9 (4.2) | 6 (5.8) | 0.5 |
| Peripheral arterial disease, n, % | 12 (5.6) | 16 (15.5) | 0.003* |
| History of previous stroke, n, % | 22 (10.2) | 12 (11.9) | 0.6 |
| History of MS or autoimmune disease, n, % | 9 (4.2) | 6 (5.9) | 0.5 |
| Number of comorbidities, n, mean (SD) | 1.6 (1.3) | 1.9 (1.5) | 0.06 |
| Length of hospitalization, n (SD) | 14.2 (14.3) | 11.4 (8.4) | 0.2 |
| Number of invasive devices, n, mean (SD) | 1.5 (0.7) | 1.7 (0.6) | 0.002* |
| Central venous catheters, n, % | 20 (9.3) | 10 (9.7) | 0.9 |
| Number of antibiotics, n, mean (SD) | 0.75 (1.5) | 0.63 (1.3) | 0.039* |
| Subjects admitted for stroke, n, % | 114 (52.8) | 48 (46.6) | 0.3 |
Abbreviations: COPD = chronic obstructive pulmonary disease; MS = multiple sclerosis; SD = standard deviation. * p value less than 0.05.
Fig. 1.
Discharge diagnoses stratified by year of hospitalization.
Discharge diagnoses expressed as percentages. Patients hospitalized during 2019 are in blue while those hospitalized during 2020 are in red. Abbreviations: FND = functional neurological disorders; TIA = transient ischemic attack.
The overall number of HAIs considering both the years was 92 (28.8% of the patients). Among control patients, HAI incidence was 31.5% (95% confidence interval (CI): 0.25–0.38), as compared with 23.3% (95% CI: 0.15–0.32) in study patients (Fisher's exact test, p = 0.12). The number of HAIs per patient was 0,44 (95% CI: 0.34–0.55) among control patients, as compared with 0,26 (95% CI: 0.15–0.37) in study patients (p = 0.02).
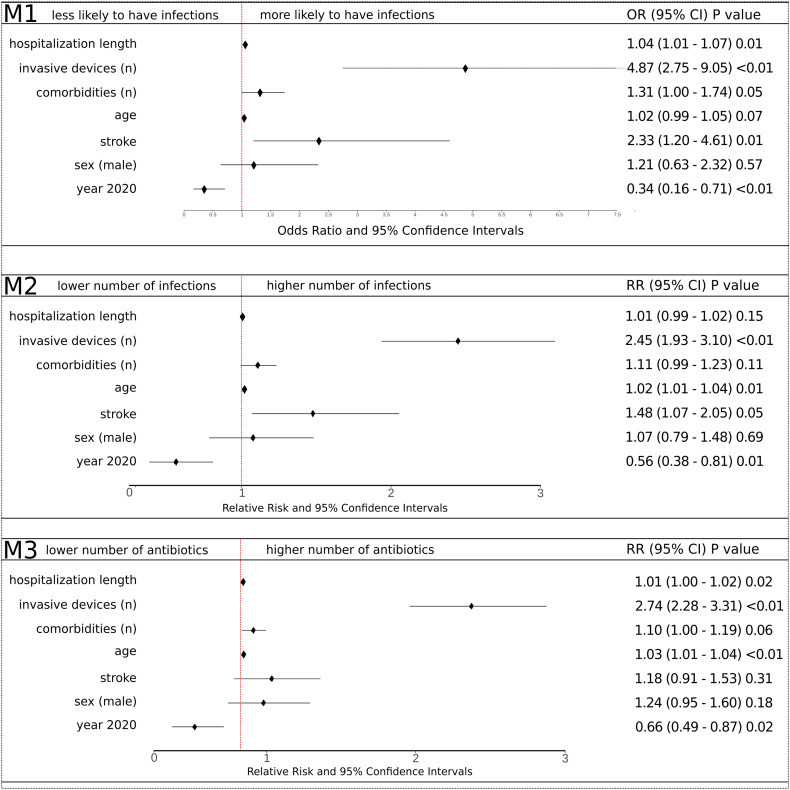
According to M0, hospitalization in 2020 was independently associated with a decreased incidence of HAIs (odds ratio: 0.34, 95% CI: 0.16–0.71, p = 0.004) (Fig. 2 ).
Fig. 2.
Forest plot of regression analyses.
Forest plot of multivariable regression analyses. All independent variables in the models are represented. The upper panel shows the multivariable logistic regression model (M0) and relative factors associated with the absence/presence of hospital-acquired infections (HAIs). The X-axis represents the relative odds ratio (OR) and 95% confidence interval (CI) of each covariate. P values are reported on the right. The middle panel shows the multivariable Poisson regression model with the number of infections per patient as the outcome (M1). For each variable, the relative risk (RR) and 95% CI are reported and P values are shown on the right. The lower panel shows the multivariable Poisson regression model with the number of antibiotics administered per patient as the outcome (M2). For each variable, the RR and 95% CI are reported and P values are shown on the right.
Hospitalization in 2020 was also associated with a significant reduction in the number of HAIs per patient (M1: relative risk (RR): 0.56, 95% CI: 0.38–0.81, p < 0.01) (Fig. 2) and a significant reduction in the number of antibiotics per patient (M2: RR: 0.66, 95% CI: 0.49–0.87, p = 0.02) (Fig. 2).
4. Discussion
In our single-center case-control study, we found that the patients hospitalized between March 8–May 31, 2020 had a reduced likelihood of HAIs as compared with patients hospitalized during the same period in 2019. We also found a reduced number of antibiotic prescriptions per patient during the COVID-19 outbreak as compared with the same period in 2019. The documented reduced HAI risk could be related to increased hygienic measures and widespread use of PPE due to the concurrent COVID-19 outbreak. Besides, the 1.5-m distance between hospital beds might have contributed as well. To the best of our knowledge, this is the first study reporting a possible association between reduced HAIs and stricter hygienic measures, including the use of PPE, among healthcare workers during the COVID-19 pandemic.
As regards the overall rate of HAIs in our cohort, we found a high incidence of infections as compared to literature [10]. This finding may be due to the high prevalence of stroke patients, who are known to be at high risk of HAIs [9,13], and to the frequent use of invasive devices (e.g. urinary and central catheters, nasogastric tubes, etc.) in these subjects, which is also associated with a higher HAI risk [11,14]. As expected, we also found that the use of invasive devices, a stroke diagnosis, and the length of hospitalization were significantly associated with an increased HAI risk, as previously reported by other authors [9,15].
In conclusion, our study found decreased HAI occurrence in patients hospitalized in our neurological unit during the COVID-19 outbreak with respect to the previous year, in spite of comparable clinical severity. Considering the possible association between reduced HAI risk and adherence to stricter hygienic measures, our data further highlights the great impact of precautionary measures, including the use of PPE, on hospitalized patients' care and management. These findings appear particularly relevant when considering the potential burden of HAIs on the Italian healthcare system in terms of both mortality and public spending.
5. Limitations
The main limitations of our study are the relatively small number of patients and the single-center retrospective design. Larger studies are needed to confirm our findings and to support the extension of preventive measures even after the SARS-CoV-2 outbreak in order to limit the occurrence of HAIs among hospitalized patients.
Funding/support
None.
Author contributions
Cerulli Irelli: Conceptualization, Data curation, Investigation, Formal analysis, Writing - original draft, review and editing. Orlando: Data curation, Methodology, Writing- review and editing. Cocchi: Conceptualization, Methodology, Software, Writing- review and editing. Morano: Data curation, Writing- review and editing. Fattapposta: Supervision, Writing- review and editing. Di Piero: Supervision, Writing-review and editing. Toni: Methodology, Supervision, Validation, Writing-review and editing. Ciardi: Validation, Writing-review and editing. Giallonardo: Data curation, Supervision, Writing- review and editing. Fabbrini: Methodology, Writing- review and editing. Berardelli: Methodology, Project administration, Supervision, Writing-review and editing. Di Bonaventura: Conceptualization, Data curation, Methodology, Supervision, Validation, Writing- original draft, review and editing.
Declaration of Competing Interest
None.
References
- 1.Gagliano A., Villani P.G., Co’ F.M. COVID-19 epidemic in the Middle Province of northern Italy: impact, logistics, and strategy in the first line hospital [published online ahead of print, 2020 mar 24] Disaster Med. Public Health Prep. 2020:1–5. doi: 10.1017/dmp.2020.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gatto M., Bertuzzo E., Mari L. Spread and dynamics of the COVID-19 epidemic in Italy: effects of emergency containment measures. Proc. Natl. Acad. Sci. U. S. A. 2020;117(19):10484–10491. doi: 10.1073/pnas.2004978117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html Available at.
- 4.World Health Organization Rational use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations During Severe Shortages: Interim Guidance. 2020. https://apps.who.int/iris/handle/10665/331695 Avalaible at.
- 5.Lotfinejad N., Peters A., Pittet D. Hand hygiene and the novel coronavirus pandemic: The role of healthcare workers [published online ahead of print, 2020 Mar 19] J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.03.017. S0195–6701(20)30116-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Guidelines on hand hygiene in health care First Global Patient Safety Challenge Clean Care Is Safer Care. 2020. https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1 Available at: [PubMed]
- 7.Allegranzi B., Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J. Hosp. Infect. 2009;73(4):305–315. doi: 10.1016/j.jhin.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 8.Haque M., Sartelli M., McKimm J., Abu Bakar M. Health care-associated infections - an overview. Infect. Drug Resist. 2018;11:2321–2333. doi: 10.2147/IDR.S177247. Published 2018 Nov 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emsley H.C., Hopkins S.J. Acute ischaemic stroke and infection: recent and emerging concepts. Lancet Neurol. 2008;7(4):341–353. doi: 10.1016/S1474-4422(08)70061-9. [DOI] [PubMed] [Google Scholar]
- 10.Suetens C., Latour K., Kärki T. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017 [published correction appears in Euro Surveill. 2018 Nov;23(47):] Euro Surveill. 2018;23(46) doi: 10.2807/1560-7917.ES.2018.23.46.1800516. 1800516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.European Centre for Disease Prevention and Control Surveillance of Antimicrobial Resistance in Europe. 2018. https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2018 Avalaible at.
- 12.Revelas A. Healthcare - associated infections: a public health problem. Niger Med. J. 2012;53(2):59–64. doi: 10.4103/0300-1652.103543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aslanyan S., Weir C.J., Diener H.C., Kaste M., Lees K.R. GAIN international steering committee and investigators. Pneumonia and urinary tract infection after acute ischaemic stroke: a tertiary analysis of the GAIN international trial. Eur. J. Neurol. 2004;11(1):49–53. doi: 10.1046/j.1468-1331.2003.00749.x. [DOI] [PubMed] [Google Scholar]
- 14.Nicolle L.E. Catheter associated urinary tract infections. Antimicrob Resist Infect Control. 2014;3:23. doi: 10.1186/2047-2994-3-23. Published 2014 Jul 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pellizzer G., Mantoan P., Timillero L. Prevalence and risk factors for nosocomial infections in hospitals of the Veneto region, North-Eastern Italy. Infection. 2008;36(2):112–119. doi: 10.1007/s15010-007-7092-x. [DOI] [PubMed] [Google Scholar]