Abstract
Background
In a short time, the COVID-19 pandemic turned into a global emergency. The fear of becoming infected and the lockdown measures have drastically changed people's daily routine. The aim of this study is to establish the psychological impact that the COVID-19 pandemic is entailing, particularly with regards to levels of stress, anxiety and depression, and to the risks of developing Post-Traumatic Stress Disorder (PTSD).
Methods
The study, carried out with a sample of 1612 subjects distributed in seven countries (Australia, China, Ecuador, Iran, Italy, Norway and the United States), allowed us to collect information about the psychological impact of COVID-19.
Results
The findings of this study show that the levels of stress, depression and anxiety, as well as the risks of PTSD, are higher than average in over half of the considered sample. The severity of these disorders significantly depends on gender, type of outdoor activities, characteristics of their homes, eventual presence of infected acquaintances, time dedicated to looking for related information (in the news and social networks), type of source information and, in part, to the level of education and income.
Conclusions
We conclude that COVID-19 has a very strong psychological impact on the global population. This appears to be linked to the coping strategies adopted, level of mindful awareness, socio-demographic variables, people's habits and the way individuals use means of communication and information.
Keywords: COVID-19, Depression, Stress, Anxiety, Psychological Impact, PTSD, Clinical psychology, Mental health
1. Introduction
The first cases of the Coronavirus Disease 2019 (COVID-19) were reported in December 2019 in China, and by January 2020 a novel coronavirus (SARS-CoV2) was clearly identified, as indicated in Huang et al. (2020) and in Acter et al. (2020). Coronaviruses originate from intestinal and respiratory infections and until now two other major coronavirus outbreaks have occurred, the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) in 2003 and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in 2012 (Ahmed et al., 2020; Bonilla-Aldana et al., 2020; Wang et al., 2020b).
As described by the European centre for Disease Prevention, 2020 and Control and by Sohrabi et al. (2020), typical signs and symptoms of COVID-19 patients include fever, dry cough, tachypnea, shortness of breath, asthenia, headache, rhinorrhea, gustatory dysfunction and sore throat. Moreover, although some patients are asymptomatic, some may show a clinical worsening leading to fatality (Lotfi et al., 2020; Tabata et al., 2020).
After initially spreading in China, the pandemic quickly had stark repercussions in Asia, Europe and then the rest of the world (Ahmed et al., 2020). On 30 January 2020 The World Health Organization (WHO) officially declared COVID-19 as a Public Health Emergency of International Concern (Sohrabi et al., 2020). Progressively, the pandemic has entailed a tremendous amount of reported cases and deaths, namely approximately 21 million infected people and 755,000 deaths reported across 188 countries up till 15 August 2020. By 30 April 2020, at the end of the online survey administered in this research, there were over 3.1 million confirmed cases and almost 250,000 deaths (WHO, 2020a, 2020b, 2020c).
The coronavirus outbreak spread quickly across the world due to the large amount of international travels and relative ease of transmission (Ahmed et al., 2020; Shuja et al., 2020). In particular, major ways of infection can occur by direct contact with an infected person and droplets or by indirect contact with infected surfaces in the environment (Lotfi et al., 2020; Ningthoujam, 2020).
National lockdowns have been the solution adopted by many countries to slow down the pandemic due to the current absence of vaccine and medical interventions. Furthermore, the economic consequences were added to the existing health and social crisis (Bonaccorsi et al., 2020; Brooks et al., 2020; Singh et al., 2020); in that sense some authors have even compared this financial crisis to the Great Depression of 1929 (Baker et al., 2020).
The intensive efforts to keep up social distancing have invariably been accompanied by social isolation (Banerjee and Rai, 2020); in addition, negative perceptions and fears associated with disease have increased several mental health disorders (Shuja et al., 2020). In fact, various studies point out a strong correlation between natural disasters and epidemics and mental illnesses like depression, anxiety, post-traumatic stress disorder (Brooks et al., 2020; Kar and Bastia, 2006; Liu et al., 2012; Mak et al., 2009; Sim and Chua, 2004; Sprang and Silman, 2013; Wu et al., 2005).
It is to stress that patients with a previous disorder, for example anxiety, may worsen their symptoms (Bystritsky et al., 2020). Moreover, it is known that psychological factors and personal beliefs are related with public health action to curtail the transmission (Leung et al., 2003); low social and mental support and a high perception of risk appear to be associated with psychological symptoms (Wu et al., 2005).
Together, these findings seem to be confirmed by recent research regarding social and psychological impact of SARS-Cov-2 infection in specific countries (Liu et al., 2020; Mazza et al., 2020; Serafini et al., 2020; Tabata et al., 2020; Wang et al., 2020d), but most of these explorations have been conducted on doctors and healthcare workers (for example, Tan et al., 2020).
According to the scientific literature, it is also known that the psychological symptoms might be related with different factors, like temperament and attachment style (Moccia et al., 2020), social support (Cao et al., 2020), inadequate information (Brooks et al., 2020; Serafini et al., 2020), coping strategies (Ho et al., 2020), rumors in social media (Roy et al., 2020) and precautionary measures such as face mask use (Wang et al., 2020c) and social distance.
Mental health interventions, like Cognitive Behavioral Therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR), are precious at an early stage because the lack of a psychological support seems to be an important risk factor (Kar e Bastia, 2006; Morganstein and Ursano, 2020), especially considering that an intermediate range of traumatic experience seems to predict a subsequent growth (Butler et al., 2005).
In addition to the stark consequences related to human health and individual well-being, the COVID-19 pandemic has also entailed several major effects encompassing society and environment, i.e. causing deep modifications related to individual mobility (Barbieri et al., 2020a; De Vos J., 2020; Wells et al., 2020) and environmental pollution (Barbieri et al., 2020b; Le Quéré et al., 2020; Shakil et al., 2020).
For these reasons, this research aims to investigate the psychological impact of the current COVID-19 pandemic in reference to several sociodemographic and personality factors in seven countries on five continents: Australia, China, Ecuador, Iran, Italy, Norway and the United States. This is important to better characterize this historical moment according to a global framework as well as understanding which factors most affect people's quality of life.
2. Methods
2.1. Setting, participants and procedure
This study adopted a cross-sectional survey designed to analyze the psychological impact of COVID-19 restrictive measures in the above-mentioned countries.
The anonymous online survey was administered using Google Forms and WenJuanXing platforms and distributed among adult students and workers between 17-04–2020 and 30–04–2020. The personal data collected were processed anonymously and aggregated for the analysis performed in this study. The research was conducted in compliance with the ethical principles of the Helsinki Declaration for human subjects research. The study, consisting of a series of queries related to individuals during the pandemic emergency, was considered "at minimum risk" for the participants, who were free to refuse participation or abandon the survey at any time.
2.2. Variables and measures
The online survey has been administered in seven countries and different aspects have been investigated, the questionnaire was subdivided into three major parts accordingly: (1) socio-demographic information, (2) use of free time, (3) use of information media and technologies. Overall, the survey focused particularly on awareness, coping strategies, and psychological impact of COVID-19.
The socio-demographic part gathered information about the gender, nationality, age, education, type of dwelling, knowledge of other infected people. The use of free time included some questions like: “Do you do some outdoor activities such as sport or walks?”, “Do you go out to do some non-essential activities?”, “How often do you look for information about the contagion?”. The use of information media and communication presented some questions like: “What is your main source of communication?” or “How long do you use social media?”.
Psychodiagnostics self-administered tests were employed to measure awareness, coping strategies and psychological impact of COVID-19, as already performed in literature (Moccia et al., 2020; Wang et al., 2020e) and clinical practice to evaluate personal characteristics and presence of psychopathology.
The Mindfulness Awareness Attention Scale (MAAS) is a 15-item scale designed to assess individual differences of attention and awareness. Higher scores correspond to higher levels of dispositional mindfulness awareness. Subject answer using a 6-point Likert scale ranging from 1 to 6 (Brown and Ryan, 2003).
The Event Scale-Revised (IES-R) is a self-report questionnaire that is used to define Post-Traumatic Stress Disorders (PTSD). The IES-R is composed of 22 items on 5-point Likert scale ranging from 0 to 4 which constitute three subscales: intrusion, hyperarousal and avoidance. A total score of 33 is evaluated as the best cut-off associated to a probable diagnosis of PTSD.
Moreover, IES-R rating scores can be divided into normal scores (0–23), mild psychological impact (24–32), moderate psychological impact (33–36) and severe psychological impact with scores of 37 or above (Creamer et al., 2003; Kawamura et al., 2001; Wang et al., 2020d; Weiss and Marmar, 1996).
The Depression, Anxiety and Stress Scale (DASS-21) is deemed to provide information about all these three psychological constructs. It is a 21-item self-report scale on 4-point Likert from 0 to 3. It is not a categorical measure of clinical diagnoses but is based along a continuum of severity. The scoring provides the multiplication of the scores by 2. The total depression subscale determined scores within the normal range (0–9), mild depression (10–12), moderate depression (13–20), severe depression (21–27), and extremely severe depression (28–42). The seven questions about the anxiety subscale identify scores within the normal range (0–6), mild anxiety (7–9), moderate anxiety (10–14), severe anxiety (15–19), and extremely severe anxiety (20–42). The seven questions about stress subscale define scores within the normal range (0–10), mild stress (11–18), moderate stress (19–26), severe stress (27–34), and extremely severe stress with 35 or above (Henry and Crawford, 2005).
The Patient Health Questionnaire (PHQ-9) is a short scale on 4-point Likert (0–3) and it is used for depression screening and diagnosis. It is composed of 9 items with the addition of another question about the functional impairment in the activities of daily life. Only the first 9 items contribute to the final score in a range of 0 to 27 (Kroenke et al., 2001; Spitzer et al., 1999). The scores determine ranges for absence of depression (0–4), mild depression (5–9), moderate (10–14), moderately severe (15–19), severe depression (20 or above).
The PSS10 is one of the most used psychological tests to measure perceived stress and it is based on 5-point Likert scale (0–4). A scoring ranging from 0 to 13 can be considered low stress. A range between 14 and 26 can indicate moderate stress. Total score of 27 or above represents a high perceived stress (Cohen et al., 1983; Cohen and Williamson, 1988).
The Brief-COPE is a short version of the COPE (Coping Orientation to Problems Experienced) inventory, this is a self-report questionnaire that identifies typical coping strategies when facing difficult situations. Two subscale possibilities have been identified: a subscale measuring avoidance strategies and another subscale assessing approach strategies (Carver, 1997; Eisenberg et al., 2012; Meyer, 2001).
Validated versions of the tests in the various languages spoken in the seven countries were employed. Moreover, considering previous researches performed on a one-country level, IES-R and DASS-21 were used during COVID-19 research in China (Hao et al., 2020), India (Chew et al., 2020), Vietnam (Le et al., 2020), Singapore (Tan et al., 2020), and Philippines (Tee et al., 2020); MASS was adopted in Italy (Conversano et al., 2020; Baiano et al., 2020) and Brazil (Kozasa et al., 2020); PSS10 was used in Brazil (Kozasa et al., 2020), China (Duan et al., 2020; Yan et al., 2020) and Colombia (Pedrozo-Pupo et al., 2020); PHQ9 was employed in Greece (Skapinakis et al., 2020), Italy (Rapisarda et al., 2020), Spain (Garre-Olmo et al., 2021) and China (Yao, 2020); Brief-COPE was used in Australia (Gurvich et al., 2020), Greece (Skapinakis et al., 2020), United Kingdom (Dawson and Golijani-Moghaddam, 2020) and USA (Umucu and Lee, 2020).
2.3. Statistical analysis
Data were analyzed using SPSS Version 25 and 26 (SPSS IBM, Armonk, NY, USA).
The method used in the study was the analysis of the covariance (ANCOVA), that combines the analysis of the variance (ANOVA) and the linear regression on the covariates.
Since the normality assumptions necessary to perform the analysis of the covariance (ANCOVA) were not respected, the techniques of bootstrap with the accidental simulation of Mersenne Twister were also considered (Delucchi and Bostrom, 2004; Hosseini et al., 2017; Wehrens et al., 2000; Wright et al., 2011); literature indicates that a number of 500 bootstrap extractions are sufficient for correctness of the resample (Deng et al., 2013).
Adopting the resample bootstrap, t-tests with the correction of Bonferroni for multiple comparisons were also requested, thus identifying the differences in groups means (MD) with a conservative approach.
The statistical analysis was conducted on a sample of 1612 subjects distributed in seven countries. Firstly, the descriptive statistics related to the main socio-demographic variables were calculated. The possibility to estimate the models on two levels was hypothesized, considering the sample like a hierarchical structure with countries as clusters. With the application of a mixed model with random intercept and random effects of the coefficient's explicative variables, the non-significance of the random components between the countries was characterized. Therefore, the applied ANCOVA model was used to estimate the regressors fixed effects of the explanatory variables including the fixed effects of the country. The model included the study of the different areas presented in subSection 2.2 dealing with the psychological consequences on stress, depression, anxiety and PTSD. The same analysis was performed six times to predict the means of the dependent variables linked to the psychopathological symptoms. In each model, the variables related to coping strategies (Brief-COPE) and mindful awareness (MAAS) were identified as covariates.
3. Results
3.1. Descriptive statistics
3.1.1. Sociodemographic characteristics
The survey participants were distributed on the seven countries with these percentage frequencies: Italy (26.1%), United States (9.8%), Ecuador (9.2%), Norway (6.6%), Iran (13.4%), Australia (8.1%) and China (26.8%). Globally the sample was composed by 644 males (40%) and 968 females (60%) with an average age of 28 (SD = 9.36). The age is not considered a determining factor of stress, depression, anxiety and post-traumatic stress disorder (PTSD), given the uniformity of the sample. Among the interviewees, 1351 (83.8%) have no children, while 261 (16.2%) have a child or more.
Among the cultural and economic factors, the survey collected information regarding the perceived family income, the employment (study, job or none), and the education. In the interviewed sample, 11.8% of the respondents considered themselves in the low-income group, 22.2% in the medium-low, 50.1% in medium, 14.1% in medium-high, and only 1.7% in the high one. The unemployed interviewees were 117 (7.3%) and students and workers were 1450 (90%), 44 respondents (2.7%) did not declare their job status. The education of the interviewees largely spanned from High school to Master degree (80.9%), 1.3% had education below Middle school, 14.8% declared a Ph.D. or to be attending Post graduated school, 48 interviewees did not answer.
3.1.2. Psychological impact
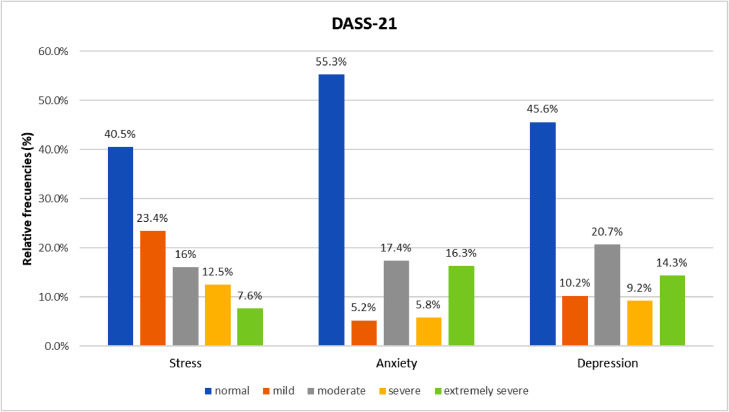
As displayed in Fig. 1 related to the DASS 21 stress subscale, 653 subjects (40.5%) obtain scores within the normal range, 377 (23.4%) seem to report mild stress, 258 (16%) suffer from moderate stress, 201 (12.5%) severe stress, 123 (7.6%) extremely severe stress.
Fig. 1.
Relative frequencies of DASS-21 scales in the sample.
Considering the DASS 21 anxiety subscale (Fig. 1), 892 subjects (55,3%) obtain scores within the normal range, 84 (5,2%) seem to report mild anxiety, 280 (17,4%) suffer from moderate anxiety, 94 (5,8%) severe anxiety, 262 (16,3%) extremely severe anxiety.
Taking into consideration the DASS 21 depression subscale (Fig. 1), 735 subjects (45,6%) obtain scores within the normal range, 165 (10,2%) seem to report mild depression, 333 (20,7%) suffer from moderate depression, 148 (9,2%) severe depression, 231 (14,3%) extremely severe depression.
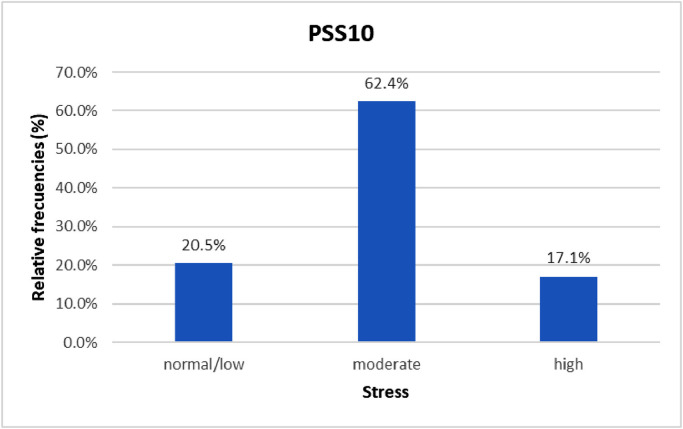
As illustrated in Fig. 2 related to the PSS10, stress levels are mild or absent in 331 subjects (20,5%), moderate in 1005 subjects (62,4%) and high in 276 subjects (17,1%).
Fig. 2.
Relative frequencies of PSS10 scale in the sample.
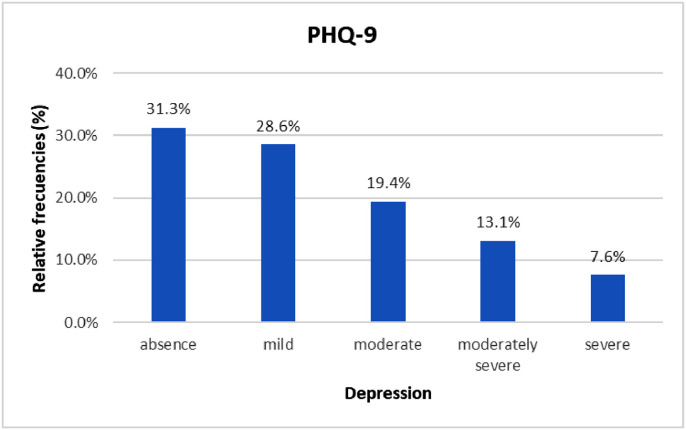
The PHQ-9 scores (Fig. 3 ) show 504 subjects (31.3%) with absence of depression, 462 (28.6%) with mild depression, 312 (19.4%) with moderate depression, 212 (13.1%) with moderately severe depression, 122 (7.6%) with severe depression.
Fig. 3.
Relative frequencies of PHQ-9 scale in the sample.
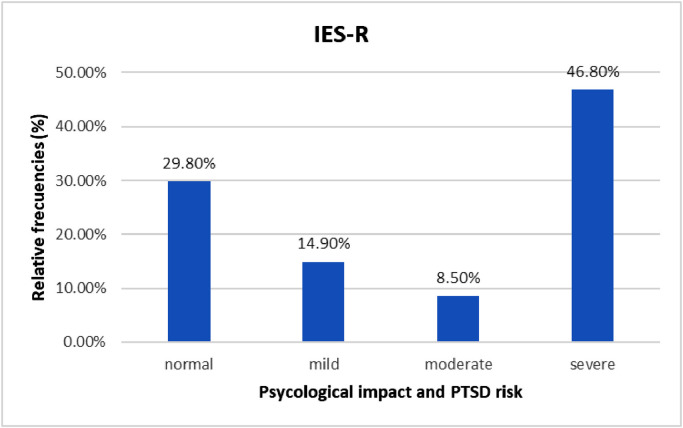
In the IES-R scale (Fig. 4 ), 481 subjects (29,8%) receive scores that can be considered as being in the norm, 250 (14,3%) are characterized by a mild psychological impact and borderline scores indicating the possibility of a partial PTSD or some of the symptoms, 136 (8,5%) receive scores indicating moderate psychological impact and probable diagnosis of PTSD and 745 (46,8%) are related to scores showing severe psychological impact and PTSD diagnosis.
Fig. 4.
Relative frequencies of IES-R scale in the sample.
In the MAAS scale, the sample of subjects received an average score of 61,16 (SD = 13.28) in levels of attention and awareness. In the URCS scale, the average sample score of 5,62 (SD = 1.24) indicates a high level of relationship closeness with family members.
The scores related to the Brief-COPE queries dealing with coping strategies, on the other hand, show a greater use of approach strategies (M = 35.40, SD = 6.23) compared to avoidance strategies (M = 26.15, SD = 5.91).
3.2. Model results
3.2.1. Sociodemographic characteristics and psychological impact
The DASS-21, IES-R, PSS10 and PHQ-9 variables are significantly linked to the particular countries (Table 1 , Table 3). The levels of post-traumatic symptoms in the IES-R Scale are significantly higher in Iran (M = 41.75, SE = 2.24) than in other countries, with the exception of Ecuador. Ecuador (M = 39.82, SE = 2.50) has trauma scores in the IES-R scale considerably higher than those of Norway (MD = 10.01, p = .002, 95% CI: 5.40 to 14.17), Australia (MD = 5.10, p = .032, 95% CI: 0.58 to 10.15) and China (MD = 5.70, p = .014, 95% CI: 1.17 to 9.65). On the other hand, subjects that were interviewed in Norway (M = 29.81, SE = 2.16) have scores that are significantly lower than in any other country. The Italian participants in this study showed PSS10 stress levels substantially higher (M = 21.14, SE = 0.76) than anywhere else, except for Australia (M = 19.65, SE = 0.84). On the other hand, China has evaluated PSS10 levels significantly inferior (M = 15.98, SE = 0.74) to those of any other country while Iran has levels lower than those of Italy (MD = −3.76, p = .002, 95% CI: −4.89 to −2.64), Ecuador (MD = −1.88, p = .006, 95% CI: −3.13 to −0.58) and Australia (MD = −2.28, p = .01, 95% CI: −3.86 to −0.90). The results are confirmed by the DASS-21 Stress Subscale in which the Italian subjects have an average score that is considerably higher (M = 20.60, SE = 1.32) than that of all other countries. On the contrary, China is the country where those who answered the questionnaire obtained considerably lower scores (M = 9.45, SE = 1.30). In the DASS-21 Anxiety Subscale, however, Ecuador has scores that are significantly higher (M = 13.39, SE = 1.36) than in any other country. Participants in China, however, showed substantially lower (M = 7.77, SE = 1.23) levels of anxiety than any other country. No significant variations were detected between all other countries in the DASS-21 Anxiety Subscale.
Table 1.
association between sociodemographic characteristics and the psychological impact of the 2019 coronavirus disease (COVID-19) in the DASS-21 subscales.
| Variables | n (%) | DASS Stress | DASS Depression | DASS Anxiety | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bootstrap | Bootstrap | Bootstrap | ||||||||||||||||||
| Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | |||||||||
| Country | ||||||||||||||||||||
| Italy | 420 (26.1) | 20.60 | 1.32 | 11.16** | 9.59 | to | 12.86 | 18.49 | 1.23 | 8.87** | 7.14 | to | 10.59 | 10.08 | 1.20 | 2.36** | 0.83 | to | 3.75 | |
| United States | 158 (9.8) | 14.99 | 1.39 | 5.54** | 3.71 | to | 7.64 | 14.26 | 1.29 | 4.65** | 2.75 | to | 6.78 | 10.72 | 1.26 | 2.95** | 1.31 | to | 4.78 | |
| Ecuador | 149 (9.2) | 16.3 | 1.48 | 6.85** | 4.43 | to | 9.34 | 13.73 | 1.41 | 4.11** | 1.80 | to | 6.28 | 13.39 | 1.36 | 5.62** | 3.51 | to | 7.69 | |
| Norway | 107 (6.6) | 16.58 | 1.36 | 7.17** | 5.11 | to | 9.51 | 16.56 | 1.27 | 6.95** | 4.67 | to | 9.53 | 10.04 | 1.29 | 2.26* | 0.18 | to | 4.52 | |
| Iran | 216 (13.4) | 17.2 | 1.40 | 7.75** | 5.57 | to | 9.76 | 13.99 | 1.37 | 4.38** | 2.51 | to | 6.39 | 11.14 | 1.32 | 3.37** | 1.64 | to | 5.28 | |
| Australia | 130 (8.1) | 16.86 | 1.50 | 7.41** | 5.21 | to | 9.74 | 14.98 | 1.36 | 5.36** | 3.04 | to | 7.70 | 10.71 | 1.32 | 2.93** | 1.06 | to | 5.00 | |
| China | 432 (26.8) | 9.45 | 1.30 | 9.62 | 1.22 | 7.77 | 1.23 | |||||||||||||
| Gender | ||||||||||||||||||||
| Male | 644 (40) | 15.00 | 1.22 | −1.20** | −3.13 | to | −0.99 | 14.03 | 1.11 | −0.98 | −2.10 | to | 0.09 | 10.11 | 1.13 | −0.87 | −1.77 | to | 0.00 | |
| Female | 968 (60) | 17.00 | 1.20 | 15.01 | 1.12 | 10.99 | 1.12 | |||||||||||||
| Declared income | ||||||||||||||||||||
| Low | 190 (11.8) | 16.77 | 1.30 | 2.96 | −1.27 | to | 6.84 | 15.16 | 1.24 | 1.30 | −1.71 | to | 4.29 | 11.44 | 1.19 | 3.76** | 1.50 | to | 6.20 | |
| Medium-low | 358 (22.2) | 16.29 | 1.24 | 2.48 | −1.52 | to | 5.95 | 15.00 | 1.20 | 1.14 | −1.93 | to | 4.09 | 11.54 | 1.19 | 3.87** | 1.78 | to | 6.21 | |
| Medium | 808 (50.1) | 16.90 | 1.14 | 3.09 | −0.45 | to | 6.49 | 14.61 | 1.08 | 0.75 | −1.97 | to | 3.55 | 11.38 | 1.10 | 3.70** | 1.75 | to | 5.86 | |
| Medium-high | 228 (14.1) | 16.22 | 1.28 | 2.41 | −1.36 | to | 5.88 | 13.96 | 1.23 | 0.09 | −2.84 | to | 3.12 | 10.73 | 1.23 | 3.05** | 0.91 | to | 5.30 | |
| High | 28 (1.7) | 13.81 | 2.11 | 13.86 | 1.66 | 7.67 | 1.46 | |||||||||||||
| Education | ||||||||||||||||||||
| No answer | 48 (3) | 15.12 | 1.65 | −0.02 | −2.79 | to | 2.95 | 12.67 | 1.43 | 0.22 | −2.38 | to | 2.81 | 8.81 | 1.36 | −0.96 | −3.29 | to | 1.57 | |
| Primary school | 6 (0.4) | 19.54 | 4.31 | 4.40 | −2.52 | to | 13.79 | 19.87 | 3.48 | 7.42* | 1.74 | to | 14.78 | 15.42 | 4.68 | 5.65 | −2.48 | to | 16.55 | |
| Middle school | 15 (0.9) | 18.68 | 2.45 | 3.54 | −1.61 | to | 8.35 | 17.30 | 3.12 | 4.86 | −1.53 | to | 11.25 | 11.36 | 2.36 | 1.59 | −2.25 | to | 6.79 | |
| High school | 358 (22.2) | 14.74 | 1.06 | −0.40 | −2.31 | to | 1.39 | 13.60 | 0.97 | 1.16 | −0.66 | to | 2.87 | 9.96 | 0.92 | 0.20 | −1.48 | to | 1.73 | |
| Bachelor's degree | 432 (26.8) | 14.78 | 0.97 | −0.36 | −2.06 | to | 1.19 | 13.52 | 0.86 | 1.07 | −0.72 | to | 2.85 | 9.66 | 0.85 | −0.10 | −1.67 | to | 1.22 | |
| Master's degree | 514 (31.9) | 13.98 | 1.06 | −1.16 | −2.84 | to | 0.28 | 12.23 | 0.97 | −0.21 | −1.70 | to | 1.17 | 8.87 | 0.91 | −0.90 | −2.24 | to | 0.39 | |
| Ph.D. or post-graduated school | 239 (14.8) | 15.14 | 1.13 | 12.44 | 1.07 | 9.77 | 1.00 | |||||||||||||
| Employment | ||||||||||||||||||||
| No answer | 44 (2.7) | 15.52 | 1.86 | −0.32 | −3.30 | to | 3.36 | 15.23 | 1.73 | 1.08 | −1.98 | to | 4.24 | 10.52 | 1.74 | 0.33 | −2.86 | to | 3.41 | |
| Unemployed | 117 (7.3) | 16.61 | 1.39 | 0.77 | −1.12 | to | 2.74 | 15.82 | 1.31 | 1.67 | −0.16 | to | 3.52 | 10.76 | 1.33 | 0.58 | −1.27 | to | 2.55 | |
| Student | 732 (45.4) | 15.96 | 1.24 | 0.12 | −1.02 | to | 1.24 | 14.22 | 1.16 | 0.07 | −1.11 | to | 1.32 | 11.01 | 1.18 | 0.82 | −0.25 | to | 1.88 | |
| Student worker | 130 (8.1) | 16.06 | 1.41 | 0.22 | −1.73 | to | 1.97 | 13.19 | 1.29 | −0.96 | −2.76 | to | 0.91 | 10.27 | 1.29 | 0.09 | −1.68 | to | 1.72 | |
| Workers | 589 (36.5) | 15.84 | 1.18 | 14.14 | 1.06 | 10.19 | 1.11 | |||||||||||||
| Do you have children? | ||||||||||||||||||||
| No | 1351 (83.8) | 15.59 | 1.19 | −0.82 | −2.15 | to | 0.56 | 14.90 | 1.07 | 0.77 | −0.58 | to | 2.06 | 10.19 | 1.11 | −0.72 | −1.99 | to | 0.52 | |
| Yes | 261 (16.2) | 16.41 | 1.26 | 14.14 | 1.18 | 10.91 | 1.18 | |||||||||||||
| What is the larger open-air space in your home? | ||||||||||||||||||||
| No open-air spaces | 230 (14.3) | 16.90 | 1.35 | 1.03 | −0.52 | to | 2.56 | 15.78 | 1.27 | 1.49* | −0.02 | to | 3.01 | 11.04 | 1.26 | 1.06 | −0.42 | to | 2.55 | |
| Balconies and terraces | 529 (32.8) | 15.65 | 1.22 | −0.22 | −1.25 | to | 0.98 | 13.90 | 1.14 | −0.38 | −1.42 | to | 0.78 | 10.21 | 1.12 | 0.24 | −0.69 | to | 1.31 | |
| Condominium courtyard | 268 (16.6) | 15.58 | 1.26 | −0.28 | −1.59 | to | 1.28 | 14.11 | 1.12 | −0.17 | −1.47 | to | 1.22 | 10.98 | 1.15 | 1.00 | −0.14 | to | 2.32 | |
| Private garden | 585 (36.3) | 15.86 | 1.23 | 14.28 | 1.14 | 9.98 | 1.16 | |||||||||||||
| Do you know anyone infected with COVID-19? | ||||||||||||||||||||
| Yes | 509 (31.6) | 16.59 | 1.26 | 1.17* | 0.05 | to | 2.21 | 14.78 | 1.16 | 0.53 | −0.57 | to | 1.50 | 11.19 | 1.16 | 1.27* | 0.26 | to | 2.16 | |
| No | 1103 (68.4) | 15.41 | 1.16 | 14.25 | 1.06 | 9.92 | 1.10 |
Note: Results refer to the 3 regression linear models with DASS stress, DASS depression and DASS anxiety as dependent variables, linked to ANCOVA model. Covariates in the model are MAAS, Brief-COPE Avoidant and Brief-COPE Approach. To obtain the group means (ª), covariates are evaluated on the following values: MAAS = 61.16, Brief-COPE Avoidant = 26.15, Brief-COPE Approach = 35.40. Confidence intervals at 95% are obtained with bootstrap standard errors with 500 resamples. T-tests are evaluated at 5% (*p<.05), 1% (**p<.01), and 0.1% (***p<.001).
Table 3.
association between Sociodemographic Characteristics and the psychological impact of the 2019 coronavirus disease (COVID-19) in the PSS10, PHQ-9 and IES-R Scales.
| Variables | n (%) | PSS10 | PHQ-9 | IES-R | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bootstrap | Bootstrap | Bootstrap | ||||||||||||||||||
| Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | |||||||||
| Country | ||||||||||||||||||||
| Italy | 420 (26.1) | 21.14 | 0.76 | 5.15** | 4.01 | to | 6.30 | 10.44 | 0.78 | 4.31** | 3.40 | to | 5.20 | 36.36 | 2.08 | 2.23 | −0.35 | to | 4.76 | |
| United States | 158 (9.8) | 18.52 | 0.84 | 2.53** | 1.34 | to | 3.83 | 9.89 | 0.84 | 3.77** | 2.51 | to | 5.00 | 35.90 | 2.23 | 1.77 | −1.17 | to | 4.82 | |
| Ecuador | 149 (9.2) | 19.25 | 0.80 | 3.27** | 2.06 | to | 4.58 | 8.75 | 0.89 | 2.63** | 1.20 | to | 3.97 | 39.82 | 2.50 | 5.70* | 1.17 | to | 9.65 | |
| Norway | 107 (6.6) | 18.87 | 0.88 | 2.89** | 1.39 | to | 4.61 | 10.13 | 0.81 | 4.01 | 2.65 | to | 5.48 | 29.81 | 2.16 | −4.31* | −7.76 | to | −0.48 | |
| Iran | 216 (13.4) | 17.37 | 0.80 | 1.39* | 0.30 | to | 2.53 | 9.37 | 0.88 | 3.25** | 2.03 | to | 4.53 | 41.75 | 2.23 | 7.62** | 4.97 | to | 10.79 | |
| Australia | 130 (8.1) | 19.65 | 0.84 | 3.67** | 2.42 | to | 5.14 | 9.71 | 0.87 | 3.58** | 2.30 | to | 4.85 | 34.72 | 2.25 | 0.59 | −2.88 | to | 4.38 | |
| China | 432 (26.8) | 15.98 | 0.74 | 6.13 | 0.80 | 34.13 | 2.05 | |||||||||||||
| Gender | ||||||||||||||||||||
| Male | 644 (40) | 17.59 | 0.68 | −2.20** | −2.86 | to | −1.57 | 8.77 | 0.72 | −0.87** | −1.50 | to | −0.27 | 34.41 | 1.93 | −3.32** | −4.89 | to | −1.80 | |
| Female | 968 (60) | 19.78 | 0.68 | 9.64 | 0.75 | 37.73 | 1.90 | |||||||||||||
| Declared income | ||||||||||||||||||||
| Low | 190 (11.8) | 19.69 | 0.71 | 1.79 | −0.62 | to | 4.37 | 10.17 | 0.82 | 1.94* | 0.14 | to | 3.55 | 37.79 | 2.15 | 4.16 | −1.31 | to | 10.60 | |
| Medium-low | 358 (22.2) | 18.89 | 0.71 | 0.99 | −1.24 | to | 3.22 | 9.55 | 0.77 | 1.33 | −0.39 | to | 2.70 | 36.64 | 1.99 | 3.01 | −2.50 | to | 8.70 | |
| Medium | 808 (50.1) | 18.90 | 0.66 | 1.01 | −1.06 | to | 3.32 | 9.35 | 0.71 | 1.12 | −0.39 | to | 2.54 | 36.80 | 1.85 | 3.16 | −2.21 | to | 8.72 | |
| Medium-high | 228 (14.1) | 18.05 | 0.76 | 0.16 | −2.17 | to | 2.52 | 8.73 | 0.80 | 0.50 | −1.14 | to | 2.00 | 35.49 | 2.09 | 1.86 | −3.61 | to | 7.42 | |
| High | 28 (1.7) | 17.89 | 1.26 | 8.22 | 0.97 | 33.63 | 3.11 | |||||||||||||
| Education | ||||||||||||||||||||
| No answer | 48 (3) | 19.38 | 0.86 | −0.16 | −1.50 | to | 1.33 | 8.57 | 0.93 | −0.27 | −1.83 | to | 1.36 | 35.63 | 2.09 | 0.07 | −3.56 | to | 4.00 | |
| Primary school | 6 (0.4) | 18.17 | 2.34 | −1.37 | −5.92 | to | 3.47 | 10.91 | 3.09 | 2.07 | −4.37 | to | 8.95 | 43.42 | 8.61 | 7.87 | −12.62 | to | 24.29 | |
| Middle school | 15 (0.9) | 17.39 | 1.50 | −2.15 | −4.97 | to | 0.45 | 9.75 | 1.47 | 0.91 | −2.10 | to | 3.71 | 33.98 | 4.24 | −1.57 | −9.51 | to | 7.00 | |
| High school | 358 (22.2) | 18.65 | 0.60 | −0.90 | −2.09 | to | 0.17 | 9.12 | 0.60 | 0.28 | −0.74 | to | 1.27 | 34.99 | 1.50 | −0.56 | −3.70 | to | 2.32 | |
| Bachelor's degree | 432 (26.8) | 18.90 | 0.57 | −0.64 | −1.69 | to | 0.39 | 8.92 | 0.56 | 0.08 | −0.89 | to | 1.17 | 34.81 | 1.43 | −0.74 | −3.58 | to | 1.97 | |
| Master's degree | 514 (31.9) | 18.76 | 0.60 | −0.78 | −1.66 | to | 0.10 | 8.31 | 0.62 | −0.53 | −1.42 | to | 0.39 | 34.12 | 1.52 | −1.43 | −3.88 | to | 0.98 | |
| Ph.D. or post-graduated school | 239 (14.8) | 19.54 | 0.66 | 8.84 | 0.67 | 35.55 | 1.71 | |||||||||||||
| Employment | ||||||||||||||||||||
| No answer | 44 (2.7) | 19.02 | 1.07 | 0.82 | −1.14 | to | 3.04 | 9.51 | 1.10 | 0.78 | −1.01 | to | 2.79 | 34.84 | 2.75 | −2.30 | −6.79 | to | 2.70 | |
| Unemployed | 117 (7.3) | 18.39 | 0.82 | 0.18 | −0.97 | to | 1.57 | 9.55 | 0.83 | 0.82 | −0.23 | to | 1.90 | 36.67 | 2.10 | −0.47 | −3.18 | to | 2.13 | |
| Student | 732 (45.4) | 19.26 | 0.71 | 1.05 | 0.30 | to | 1.78 | 8.95 | 0.76 | 0.22 | −0.51 | to | 0.93 | 36.53 | 2.03 | −0.62 | −2.33 | to | 1.31 | |
| Student worker | 130 (8.1) | 18.55 | 0.86 | 0.34 | −1.02 | to | 1.51 | 9.28 | 0.84 | 0.55 | −0.53 | to | 1.64 | 35.16 | 2.36 | −1.99 | −5.26 | to | 0.88 | |
| Workers | 589 (36.5) | 18.21 | 0.64 | 8.73 | 0.73 | 37.15 | 1.92 | |||||||||||||
| Do you have children? | ||||||||||||||||||||
| No | 1351 (83.8) | 18.71 | 0.66 | 0.05 | −0.82 | to | 0.88 | 9.50 | 0.73 | 0.59 | −0.26 | to | 1.36 | 34.63 | 1.89 | −2.88** | −4.77 | to | −0.90 | |
| Yes | 261 (16.2) | 18.66 | 0.71 | 8.91 | 0.76 | 37.51 | 1.99 | |||||||||||||
| What is the larger open-air space in your home? | ||||||||||||||||||||
| No open air spaces | 230 (14.3) | 19.52 | 0.79 | 1.25 | 0.31 | to | 2.16 | 9.86 | 0.82 | 0.84 | −0.09 | to | 1.80 | 36.63 | 2.08 | 0.65 | −1.96 | to | 2.96 | |
| Balconies and terraces | 529 (32.8) | 18.14 | 0.68 | −0.14 | −0.84 | to | 0.59 | 8.96 | 0.73 | −0.06 | −0.64 | to | 0.57 | 35.57 | 1.92 | −0.41 | −2.07 | to | 1.51 | |
| Condominium courtyard | 268 (16.6) | 18.82 | 0.71 | 0.55 | −0.38 | to | 1.58 | 8.96 | 0.75 | −0.07 | −0.84 | to | 0.73 | 36.10 | 2.03 | 0.12 | −2.13 | to | 2.47 | |
| Private garden | 585 (36.3) | 18.26 | 0.68 | 9.03 | 0.74 | 35.98 | 1.99 | |||||||||||||
| Do you know anyone infected with COVID-19? | ||||||||||||||||||||
| Yes | 509 (31.6) | 18.96 | 0.71 | 0.54 | −0.18 | to | 1.23 | 9.41 | 0.76 | 0.42 | −0.20 | to | 1.04 | 37.11 | 1.97 | 2.08* | 0.47 | to | 3.67 | |
| No | 1103 (68.4) | 18.41 | 0.65 | 8.99 | 0.70 | 35.03 | 1.88 | |||||||||||||
Note: Results refer to the 3 regression linear models with PSS10, PHQ-9 and IES-R as dependent variables, linked to ANCOVA model. Covariates in the model are MAAS, Brief-COPE Avoidant and Brief-COPE Approach. To obtain the group means (ª), covariates are evaluated on the following values: MAAS = 61.16, Brief-COPE Avoidant = 26.15, Brief-COPE Approach = 35.40. Confidence intervals at 95% are obtained with bootstrap standard errors with 500 resamples. T-tests are evaluated at 5% (*p<.05), 1% (**p<.01), and 0.1% (***p<.001).
In the DASS-21 Depression Subscale, the scores of the participants in Italy are considerably higher (M = 18.49, SE = 1.23) than in all other countries, except for Norway which has very similar results (M = 16.56, SE = 1.27). Norway has significantly higher depression levels than the United States (MD = 2.30, p = .42, 95% CI: 0.043 to 4.45), Iran (MD = 2.57, p = .04, 95% CI: 0.28 to 5.05) and China (MD = 6.95, p = .002, 95% CI: 4.67 to 9.54). The evaluated depression levels of the Chinese participants are noticeably lower (M = 9.62, SE = 1.22) than those of participants from all other countries. Even in this case the results seem to be confirmed by the PHQ-9 Depression Scale, at least with regards to Italy and China. In fact, it is possible to notice that Italy is the country that suffers from the highest levels (M = 10.44, SE = 0.78), which are significantly higher than Ecuador (MD = 1.68, p = .004, 95% CI: 0.53 to 2.95), Iran (MD = 1.07, p = .042, 95% CI: −0.03 to 2.05) and China (MD = 4.31, p = .002, 95% CI: 3.40 to 5.20). The Chinese participants had the lowest levels (M = 6.13, SE = 0.80) by far in this variable.
With regards to gender in the DASS-21 Stress Subscale, the scores for males (M = 14.50, SE = 1.22) are significantly lower (B = −2.00, p = .002, 95% CI: −3.13 to −0.99) than those for females. Likewise, the difference found between males and females is also substantial in the PSS10 Stress Scale (B = −2.20, p = .002, 95% CI: −2.86 to 1.57), as well as in the PHQ-9 (B = −0.87, p = .006, 95% CI: −1.50 to – 0.27) and IES-R Scales (B = −3.32, p = .002, 95% CI: - 4.89 to −1.80). In particular, the average evaluated scores for males in the PSS-10, PHQ-9 and IES-R Scales are 17.59 (SE =0.68), 8.77 (SE = 0.72) and 34.41 (SE =1.93) respectively. There are no significant differences between males and females in the DASS-21 Anxiety and Depression Subscales.
With regards to income, no significant differences between the sample groups in the IES-R Scale or in the DASS-21 Depression and Stress Subscales are registered. The subjects belonging to the high income bracket, however, have scores in the DASS-21 Anxiety Subscale that are significantly lower (M = 7.67, SE = 1.46) than those in the low (MD = −3.76, p = .002, 95% CI: −6.20 to −1.51), medium-low (MD = −3.87, p = .002, 95% CI: 6.21 to −1.78), medium (MD = −3.70, p = .002, 95% CI: −5.86 to −1.75) and medium-high income brackets (MD = −3.05, p = .006, 95% CI: −5.30 to −0.91). Likewise, the subjects belonging to the lowest income bracket have scores in the PHQ-9 that are significantly higher (M = 10.17 SE = 0.82) than those in the medium-low (MD = 1.44, p = .012, 95% CI: 0.36 to 2.52) and high income brackets (MD = 1.95, p = .018, 95% CI: 0.14 to 3.55).
The level of education is not, however, linked to any significant differences in stress and anxiety levels in the DASS-21, PSS10, PHQ-9 and IES-R Scales. Nevertheless, in the DASS-21 Depression Subscale participants who only have primary school education have higher scores (M = 19.87, SE = 3.48) than participants with high school education (MD = 6.26, p = .028, 95% CI: 0.75 to 13.60), hold a bachelor's degree (MD = 6.35, p = .022, 95% CI: 0.48 to 13.62), a master's degree (MD = 7.63, p = .014, 95% CI: 1.77 to 15.15), a Ph.D. or attend a postgraduate school (MD = 7.42, p = .016, 95% CI: 1.75 to 14.78).
The type of occupation of the participants is not connected to any significant differences in the DASS-21, PSS10, PHQ-9 and IES-R Stress, Anxiety and Depression Subscales.
In the same way, having dependent sons or daughters does not seem to be related to any differences in the scores in the DASS-21, PSS-10 and PHQ-9 subscales. The only exception is in the IES-R Scale where the respondents not having sons or daughters (M = 34.63, SE = 1.89) have significantly lower scores (B = −2.88, p = .008, 95% CI: −4.77 to −0.90) than those who have at least one child.
With regards to the characteristics of the dwelling in which the participants live and they spent their time in quarantine in, there are no important differences relating to the DASS-21, IES-R, and PHQ-9 Stress and Anxiety subscales. On the other hand, the survey participants not having access to open-air spaces (shared or private) had significantly higher scores in the DASS-21 Depression Subscale (M = 15.78, SE = 1.27) than those who had the use of balconies and/or terraces (MD = 1.88, p = .026, 95% CI: 0.25 to 3.55) and private garden (MD = 1.50, p = .05, 95% CI: −0.02 to 3.01). Even in the PSS10 Scale, those who stated that they did not have the use of open-air spaces had significantly higher scores (M = 19.52, SE = 1.79) than those who had the use of balconies and/or terraces (MD = 1.38, p = .01, 95% CI: 0.41 to 2.28) and private garden (MD = 1.25, p = .014, 95% CI: 0.31 to 2.16).
Being acquainted with someone who is infected with COVID-19 is a significant psychological factor in the DASS-21 Stress and Anxiety Subscales and in the IES-R Trauma scale. Considering the DASS-21 Stress subscale, the evaluated average score of subjects who know at least one infected person (M = 16.59, SE = 1.26) is typically higher than those who do not know anyone who is infected (B = 1.17, p = .036, 95% CI: 0.05 to 2.21). In the DASS-21 Anxiety subscale, those who know at least one infected person typically have a higher score (M = 11.19, SE = 1.16) than those who do not know anyone who is infected (B = 1.27, p = .012, 95% CI: 0.26 to 2.16). In the IES-R Trauma Scale, we can see how subjects who know infected people have a higher average score (M = 37.11, SE = 1.97) than those who do not know anyone who is infected (B = 2.07, p = .008, 95% CI: 0.47 to 3.67). On the other hand, no significant differences can be seen in the other scales.
3.2.2. Use of free-time and of means of information and communication
Taking into consideration the activities carried out during quarantine, going out for a walk or for physical exercise and going out for buying non-essential goods were not significantly associated to score differences in the DASS-21, PHQ-9 and PSS10 scales while. On the other hand, those who went out for a walk or for physical exercise showed a significantly higher score (M = 37.36, SE = 1.93) in the IES-R Scale than those who did not (B = 2.57, p = .01, 95% CI: −0.66 to 4.61). Going out for other activities, such as shopping, does not appear to be linked to any significant variation in scores.
With regards to the amount of time spent in searching for information about the virus infection, on the DASS-21 Stress Subscale we can see that those who search for information between two and five times a week have an evaluated average score (M = 14.74, SE = 1.26) that is significantly lower than those who search for information two or three times a day (MD = −1.47, p = .040, 95% CI: −2.84 to −0.01), more than three times a day (MD = −2.13, p = .026, 95% CI: −3.92 to −0.25) less than once a week (MD = −2.06, p = .03, 95% CI: −4.00 to −0.14). Likewise, in the Depression Subscale, the evaluated average score is significantly lower in subjects who search for information between two and five times a week (M = 13.32, SE = 1.14) compared to those who repeat their search for information more than three times a day (MD = −2.06, p = .030, 95% CI: −3.90 to −0.04) or do not search for news at all or less than once a week (MD = −2.07, p = .034, 95% CI: −3.92 to −0.06). In the IES-R Scale, the evaluated average score for subjects who search for information two or three times a day (M = 38.03, SE = 2.08) is significantly higher than those reading news less than once a week (MD = 3.73, p = .032, 95% CI: 0.14 to 6.95) or between two and five times a week (MD = 2.74, p = .014, 95% CI: 0.52 to 4.97). No significant differences can be found in the PSS10 and PHQ-9 Scales.
With regards to the amount of time spent on social networks, there are significant differences in the DASS-21 Stress and Anxiety Subscales. In particular, in the DASS-21 Stress subscale, the scores of those who spend between one and two hours a day on social networks (M = 15.04, SE = 1.22) are considerably lower than those who spend more than five hours a day (B = −1.48, p = .026, 95% CI: −2.68 to −0.22).
With regards to the DASS-21 Anxiety subscale, however, the scores of the subjects who do not use technology for spending time on social networks are significantly higher (M = 15.49, SE = 2.91) compared to the subjects using social networks between three and seven hours a week (MD = 5.62, p = .046, 95% CI: −0.10 to 11.42), for one or two hours a day (MD = 6.72, p = .,024 95% CI: 1.03 to 12.19), between two and five hours a day (MD = 7.14, p = .018, 95% CI: 1.79 to 12.63) and more than five hours a day (MD = 5.62, p = .044, 95% CI: 0.14 to 11.34). In addition, the scores of the subjects who use social networks more than five hours a day (M = 9.87, SE = 1.10) are significantly higher than those who use them between two and five hours a day (B = −1.52, p = .002, 95% CI: −2.61 to −0.54). The PSS10 Stress Subscale results are partially reconfirmed with the evaluated average scores which are significantly higher in people who use social networks for more than five hours a day (M = 19.64, SE = 0.68) compared to those of all other groups, with the exception of those respondents never using social networks (Table 4). In the same manner, with regards to the PHQ-9 Scale, the average evaluated scores of those participants who use technology for more than five hours a day (M = 9.57, SE = 0.68) are considerably higher than those ones who use social networks for one or two hours a day (B = −1.06, p = .004, 95% CI: −1.80 to −0.32) and those ones who use them between two and five hours a day (B = −0.84, p = .018, 95% CI: −1.54 to −0.20). No significant differences can be found in the IES-R Scale.
Table 4.
association between the use of free-time and of means of information and communication and the psychological impact of the COVID-19 in the PSS10, PHQ-9 and IES-R Scales.
| Variables | n (%) | PSS10 | PHQ-9 | IES-R | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bootstrap | Bootstrap | Bootstrap | ||||||||||||||||||
| Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | |||||||||
| During the lockdown period, do you usually go out for a walk or physical exercise? | ||||||||||||||||||||
| No | 1101 (68.3) | 18.65 | 0.69 | −0.07 | −0.95 | to | 0.82 | 9.38 | 0.73 | 0.35 | −0.39 | to | 1.11 | 37.36 | 1.93 | 2.57** | 0.66 | to | 4.61 | |
| Yes | 511 (31.7) | 18.72 | 0.69 | 9.03 | 0.75 | 34.78 | 1.95 | |||||||||||||
| During the lockdown period, do you usually go out for non-essential shopping? | ||||||||||||||||||||
| No | 1360 (84.4) | 18.93 | 0.65 | 0.49 | −0.44 | to | 1.53 | 9.00 | 0.74 | −0.41 | −1.22 | to | 0.42 | 36.40 | 1.92 | 0.67 | −1.36 | to | 2.64 | |
| Yes | 252 (15.6) | 18.44 | 0.75 | 9.41 | 0.75 | 35.74 | 1.96 | |||||||||||||
| What is your main source of information on health and infection? | ||||||||||||||||||||
| Internet | 1215 (75.4) | 19.26 | 0.57 | 0.40 | −1.67 | to | 2.19 | 10.09 | 0.69 | −1.04 | −3.22 | to | 0.89 | 35.48 | 1.71 | −0.65 | −6.26 | to | 4.01 | |
| Television | 297 (18.4) | 18.05 | 0.62 | −0.81 | −3.04 | to | 1.03 | 9.46 | 0.71 | −1.67 | −3.93 | to | 0.19 | 34.60 | 1.83 | −1.54 | −8.02 | to | 3.29 | |
| Radio | 14 (0.9) | 16.51 | 1.19 | −2.36 | −5.25 | to | 0.56 | 6.10 | 1.48 | −5.03** | −8.53 | to | −2.00 | 37.29 | 3.43 | 1.15 | −6.89 | to | 9.12 | |
| Family or friends | 43 (2.7) | 20.73 | 1.05 | 1.86 | −0.93 | to | 4.36 | 9.23 | 1.02 | −1.90 | −4.98 | to | 0.63 | 36.85 | 2.67 | 0.71 | −7.03 | to | 6.72 | |
| Others | 43 (2.7) | 18.87 | 1.13 | 11.13 | 1.20 | 36.14 | 3.15 | |||||||||||||
| How long did you use smartphone and computer to keep in touch and/or stay on social networks before the epidemic? | ||||||||||||||||||||
| Do not use | 16 (1) | 19.37 | 1.12 | −0.27 | −2.39 | to | 1.52 | 10.32 | 2.24 | 0.75 | −4.08 | to | 5.30 | 38.12 | 4.65 | 2.00 | −7.33 | to | 10.91 | |
| Less than 2–3 h per week | 98 (6.1) | 17.34 | 0.88 | −2.30** | −3.53 | to | −0.94 | 9.21 | 0.81 | −0.36 | −1.60 | to | 0.86 | 36.28 | 2.28 | 0.16 | −2.85 | to | 3.47 | |
| 3–7 h a week | 163 (10.1) | 18.42 | 0.77 | −1.22* | −2.44 | to | −0.16 | 8.87 | 0.78 | −0.70 | −1.80 | to | 0.47 | 35.97 | 2.19 | −0.15 | −2.92 | to | 2.81 | |
| 1–2 h a day | 300 (18.6) | 18.48 | 0.75 | −1.16** | −2.01 | to | −0.32 | 8.51 | 0.71 | −1.06** | −1.80 | to | −0.32 | 34.70 | 2.01 | −1.42 | −3.59 | to | 0.83 | |
| 2–5 h a day | 442 (27.4) | 18.85 | 0.69 | −0.79* | −1.57 | to | −0.01 | 8.73 | 0.68 | −0.84* | −1.54 | to | −0.20 | 35.23 | 1.86 | −0.89 | −2.70 | to | 1.02 | |
| more than 5 h/day | 593 (36.8) | 19.64 | 0.68 | 9.57 | 0.68 | 36.12 | 1.91 | |||||||||||||
| How often do you look for information on the progress of the infection? | ||||||||||||||||||||
| Less than once a week | 152 (9.4) | 19.00 | 0.73 | 0.21 | −1.19 | to | 1.62 | 9.83 | 0.84 | 0.91 | −0.63 | to | 2.47 | 34.30 | 2.25 | −2.42 | −6.21 | to | 2.00 | |
| 2 or 5 times a week | 402 (24.9) | 18.38 | 0.73 | −0.41 | −1.54 | to | 0.75 | 9.14 | 0.75 | 0.23 | −0.87 | to | 1.36 | 35.28 | 1.97 | −1.44 | −4.09 | to | 1.61 | |
| once a day | 594 (36.8) | 18.73 | 0.71 | −0.07 | −1.10 | to | 0.90 | 8.77 | 0.74 | −0.15 | −1.21 | to | 0.84 | 36.03 | 1.97 | −0.69 | −3.15 | to | 2.00 | |
| 2 or 3 times a day | 289 (17.9) | 18.52 | 0.72 | −0.28 | −1.35 | to | 0.71 | 9.36 | 0.77 | 0.44 | −0.58 | to | 1.54 | 38.03 | 2.08 | 1.31 | −1.54 | to | 4.03 | |
| more than 3 times a day | 175 (10.9) | 18.79 | 0.81 | 8.92 | 0.86 | 36.72 | 2.22 | |||||||||||||
| MAAS | −0.15** | −0.17 | to | −0.12 | −0.14** | −0.17 | to | −0.12 | −0.32** | −0.39 | to | −0.24 | ||||||||
| Brief-COPE Avoidant | 0.52** | 0.46 | to | 0.58 | 0.43** | 0.36 | to | 0.49 | 1.50** | 1.31 | to | 1.67 | ||||||||
| Brief-COPE Approach | −0.19** | −0.24 | to | −0.13 | −0.12** | −0.17 | to | −0.07 | −0.03 | −0.17 | to | 0.10 | ||||||||
Note: Results refer to the 3 regression linear models with PSS10, PHQ-9 and IES-R as dependent variables, linked to ANCOVA model. Covariates in the model are MAAS, Brief-COPE Avoidant and Brief-COPE Approach. To obtain the group means (ª), covariates are evaluated on the following values: MAAS = 61.16, Brief-COPE Avoidant = 26.15, Brief-COPE Approach = 35.40. Confidence intervals at 95% are obtained with bootstrap standard errors with 500 resamples. T-tests are evaluated at 5% (*p<.05), 1% (**p<.01), and 0.1% (***p<.001).
Based on how technology and other means are employed to retrieve information about the pandemic, people who use the internet have significantly higher scores (M = 17.28, SE = 1.09) in the DASS-21 Stress subscale compared to those who listen to the news on television (MD = 1.49, p = .024, 95% CI: 0.22 to 2.71) or on the radio (MD = 6.63, p = .004, 95% CI: 2.02 to 11.73). Similarly, even in the DASS-21 Depression subscale, the scores of those who use internet are significantly higher (M = 16.08 SE = 0.97) than those who mainly rely on television (MD = 1.96, p = .002, 95% CI: 0.83 to 3.15) and radio (MD = 7.56, p = .002, 95% CI: 2.93 to 11.85) as source of information. The same tendency is also reflected in the DASS-21 Anxiety subscale amongst people who mainly use internet (M = 12.01, SE = 0.98) and those who, on the other hand, make greater use of television (MD = 1.42, p = .008, 95% CI: 0.37 to 2.43) and radio (MD = 5.14, p = .008, 95% CI: 1.09 to 9.20). These results are also confirmed in the PSS10 Scale where those respondents who use internet (M = 19.26 SE = 0.58) have significantly higher scores than those ones who mainly rely on television (MD = 1.21, p = .004, 95% CI: 0.37 to 1.98) and radio (MD = 2.75, p = .012, 95% CI: 0.58 to 5.00). The results deriving from the PHQ-9 scale prove that the participants using internet have an average evaluated score (M = 10.09 SE = 0.69) which is significantly higher than those ones using the radio (MD = 3.99, p = .006, 95% CI: 1.31 to 6.98). No significant differences can be found in the IES-R scale with regards to the means adopted as information source.
With regards to the survey respondents who receive their news from family and friends (M = 18.36, SE =1.66), in the DASS-21 Stress Subscale these individuals have scores that are significantly higher compared to those ones who use the radio (MD = 7.71, p = .006, 95% CI: 2.41 to 13.16). A similar result is achieved in the DASS-21 Depression Subscale with a significant difference in the average evaluated scores between those participants who obtain their information from family and friends (M = 16.71, SE =1.68) and those participants who rely on the radio (MD = 8.19, p = .002, 95% CI: 2.96 to 13.37) as information source. The DASS-21 results are reconfirmed by the stress and depression tests of the PSS10 and PHQ-9. In particular, the subjects who searched for information via family and friends are characterized by higher average PSS10 scores (M = 20.73, SE = 1.05) when compared to those who use television (MD = 2.68, p = .008, 95% CI: 0.64 to 4.54) and radio (MD = 4.22, p = .002, 95% CI: 1.57 to 6.92). In the PHQ-9 Depression scale, the survey participants who receive their information through family and friends (MD = 4.22, p = .002, 95% CI: 1.57 to 6.92) have a higher average evaluated score than those ones who use the radio (MD = 3.13, p = .042, 95% CI: −0.10 to 6.32).
3.2.3. Awareness and coping strategies
By taking into consideration the covariances of this model, the coping and mindful awareness strategies largely explain the average score variations of the dependent variables (Table 2 , Table 4 ). More specifically, the lowest scores in the MAAS scale, relating to reduced awareness, are significantly linked to the highest scores in the DASS-21, PSS10, PHQ-9 and IES-R scales. At the same time, however, the highest scores in avoidance strategies (Brief-COPE Avoidant) relate to considerably higher scores in all of the previous scales. Finally, with regards to Approach Strategies (Brief-COPE Approach), the highest variable scores correspond to significantly lower scores in the DASS21, PSS10 and PHQ-9 Anxiety and Depression subscales.
Table 2.
association between the use of free-time and of means of information and communication and the psychological impact of the COVID-19 in the DASS-21 subscales.
| Variables | n (%) | DASS Stress | DASS Depression | DASS Anxiety | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bootstrap | Bootstrap | Bootstrap | ||||||||||||||||||
| Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | Meanª | SE | B | 95% IC | |||||||||
| During the lockdown period, do you usually go out for a walk or physical exercise? | ||||||||||||||||||||
| No | 1101 (68.3) | 16.27 | 1.23 | 0.55 | −0.85 | to | 1.96 | 14.62 | 1.11 | 0.19 | −1.29 | to | 1.63 | 10.90 | 1.14 | 0.71 | −0.42 | to | 1.99 | |
| Yes | 511 (31.7) | 15.72 | 1.23 | 14.42 | 1.16 | 10.20 | 1.14 | |||||||||||||
| During the lockdown period, do you usually go out for non-essential shopping? | ||||||||||||||||||||
| No | 1360 (84.4) | 16.21 | 1.20 | 0.42 | −1.03 | to | 1.82 | 14.33 | 1.10 | −0.37 | −1.67 | to | 1.05 | 10.44 | 1.11 | −0.22 | −1.38 | to | 1.01 | |
| Yes | 252 (15.6) | 15.79 | 1.25 | 14.70 | 1.16 | 10.66 | 1.16 | |||||||||||||
| What is your main source of information on health and infection? | ||||||||||||||||||||
| Internet | 1215 (75.4) | 17.28 | 1.09 | −0.63 | −4.37 | to | 2.91 | 16.08 | 0.97 | −1.07 | −4.83 | to | 2.24 | 12.01 | 0.98 | −0.80 | −4.01 | to | 2.32 | |
| Television | 297 (18.4) | 15.79 | 1.18 | −2.12 | −5.93 | to | 1.24 | 14.12 | 1.04 | −3.03 | −7.03 | to | 0.43 | 10.59 | 1.06 | −2.22 | −5.87 | to | 0.95 | |
| Radio | 14 (0.9) | 10.65 | 2.49 | −7.26* | −13.44 | to | −1.80 | 8.52 | 2.35 | −8.63** | −13.99 | to | −3.69 | 6.87 | 2.24 | −5.94** | −11.07 | to | −0.94 | |
| Family or friends | 43 (2.7) | 18.36 | 1.66 | 0.45 | −4.46 | to | 4.77 | 16.71 | 1.68 | −0.44 | −5.36 | to | 3.69 | 10.47 | 1.58 | −2.35 | −6.83 | to | 1.46 | |
| Others | 43 (2.7) | 17.91 | 2.02 | 17.15 | 1.90 | 12.81 | 1.84 | |||||||||||||
| How long did you use smartphone and computer to keep in touch and/or stay on social networks before the epidemic? | ||||||||||||||||||||
| Do not use | 16 (1) | 16.71 | 3.18 | 0.19 | −6.31 | to | 6.24 | 16.23 | 2.65 | 1.70 | −3.79 | to | 7.08 | 15.49 | 2.91 | 5.62* | 0.14 | to | 11.34 | |
| Less than 2–3 h per week | 98 (6.1) | 16.16 | 1.42 | −0.36 | −2.29 | to | 1.86 | 14.84 | 1.37 | 0.31 | −1.82 | to | 2.29 | 10.99 | 1.31 | 1.12 | −0.65 | to | 3.02 | |
| 3–7 h a week | 163 (10.1) | 15.69 | 1.29 | −0.83 | −2.59 | to | 0.87 | 14.55 | 1.24 | 0.02 | −1.76 | to | 1.81 | 9.86 | 1.22 | 0.00 | −1.59 | to | 1.60 | |
| 1–2 h a day | 300 (18.6) | 15.04 | 1.22 | −1.48* | −2.68 | to | −0.22 | 13.35 | 1.17 | −1.18 | −2.41 | to | 0.07 | 8.76 | 1.12 | −1.10 | −2.22 | to | −0.01 | |
| 2–5 h a day | 442 (27.4) | 15.86 | 1.15 | −0.66 | −1.93 | to | 0.55 | 13.60 | 1.11 | −0.93 | −2.13 | to | 0.25 | 8.34 | 1.10 | −1.52** | −2.61 | to | −0.54 | |
| more than 5 h/day | 593 (36.8) | 16.52 | 1.13 | 14.53 | 1.12 | 9.87 | 1.10 | |||||||||||||
| How often do you look for information on the progress of the infection? | ||||||||||||||||||||
| Less than once a week | 152 (9.4) | 16.80 | 1.37 | −0.07 | −2.49 | to | 2.41 | 15.39 | 1.32 | 0.01 | −2.54 | to | 2.40 | 10.21 | 1.30 | −1.13 | −3.33 | to | 1.13 | |
| 2 or 5 times a week | 402 (24.9) | 14.74 | 1.26 | −2.19* | −3.92 | to | −0.25 | 13.32 | 1.14 | −2.06* | −3.90 | to | −0.03 | 9.82 | 1.16 | −1.52 | −3.13 | to | 0.16 | |
| once a day | 594 (36.8) | 15.39 | 1.21 | −1.47 | −3.15 | to | 0.38 | 14.05 | 1.15 | −1.33 | −3.05 | to | 0.37 | 9.98 | 1.12 | −1.36 | −2.97 | to | 0.17 | |
| 2 or 3 times a day | 289 (17.9) | 16.20 | 1.28 | −0.66 | −2.45 | to | 1.11 | 14.45 | 1.18 | −0.93 | −2.66 | to | 0.80 | 11.41 | 1.20 | 0.07 | −1.52 | to | 1.68 | |
| more than 3 times a day | 175 (10.9) | 16.87 | 1.44 | 15.38 | 1.33 | 11.34 | 1.30 | |||||||||||||
| MAAS | −0.24** | −0.29 | to | −0.19 | −0.21** | −0.25 | to | −0.17 | −0.18** | −0.22 | to | −0.14 | ||||||||
| Brief-COPE Avoidant | 0.72** | 0.61 | to | 0.83 | 0.77** | 0.66 | to | 0.87 | ||||||||||||
| 0.60** | 0.49 | to | 0.69 | |||||||||||||||||
| Brief-COPE Approach | −0.06 | −0.16 | to | 0.03 | −0.27** | −0.37 | to | −0.19 | −0.12** | −0.20 | to | −0.04 | ||||||||
Note: Results refer to the 3 regression linear models with DASS stress, DASS depression and DASS anxiety as dependent variables, linked to ANCOVA model. Covariates in the model are MAAS, Brief-COPE Avoidant and Brief-COPE Approach. To obtain the group means (ª), covariates are evaluated on the following values: MAAS = 61.16, Brief-COPE Avoidant = 26.15, Brief-COPE Approach = 35.40. Confidence intervals at 95% are obtained with bootstrap standard errors with 500 resamples. T-tests are evaluated at 5% (*p<.05), 1% (**p<.01), and 0.1% (***p<.001).
4. Discussion
In line with literature dealing with the psychological impact of COVID-19 pandemic (Odriozola-González et al., 2020; Sim et al., 2010; Torales et al., 2020; Wang et al., 2020d) and with the more recent systematic review (Xiong et al., 2020), the results of this study show the presence of a strong stress and psychopathological factor during the lockdowns caused by the spread of SARS-CoV-2 disease.
In particular, when summarizing the answers of the online questionnaire, it is possible to notice that between 60% and 80% of the population sample shows stress levels that are above normal and at levels ranging from mild to severe; in particular, between 17% and 36% of the investigated sample shows levels that range from moderate to severe (Fig. 1, Fig. 2). Likewise, between 54% and 69% of the sample indicates levels of depression ranging from mild to severe, of whom between 40 and 44% at a moderate or severe level (Fig. 1; Fig. 3). In the sample, 45% of the interviewed subjects also shows levels of anxiety above average with 39% of cases at a medium or severe level (Fig. 1). Finally, 70% of the sample suffers from the psychological impact and from the risk of PTSD that can be considered as being medium to severe in 55% of cases (Fig. 4).
The prevalence estimates of psychopathology, even with some differences in the range, are in good agreement with the findings derived from the systematic review performed by Xiong and colleagues (Xiong et al., 2020). In this review study, it was documented that prevalence of high stress levels ranged from 8.1% to 81.9%, of high depression levels were from 14.6% to 48.3%, of high anxiety levels were from 6.33% to 50.9% and high scores about PTSD from 7% to 53.8%. The prevalence rates of our results are located at the top of the mentioned ranges.
This same literature also explains how psychological effects during a pandemic can be mitigated by a number of personal, social and environmental factors. These factors include, for example, several types of fears: infection, inadequate psychological and social assistance, loss of income and receiving insufficient information to deal with the pandemic (Brooks et al., 2020; Hawryluck et al., 2004; Odriozola-González et al., 2020; Xiong et al., 2020).
The data collected show a good correlation between the score in the levels of awareness and coping strategies and the psychological impact. More specifically, the lowest scores on the MAAS Awareness scale are estimated to have higher stress levels and a higher risk of PTSD, depression and anxiety; this tendency is also reflected in the Coping Strategy scale. People who have a strategical approach to solve problems, generally being more adaptive, show lower scores in all of the scales taken into consideration, with the exception of the DASS-21 Stress Subscale and of the IES-R Scale. On the other hand, people who more widely adopt avoidance strategies are exposed to higher psychopathological risks on all scales. These results confirm the findings of previous studies (Main et al., 2011; Sim et al., 2010) which also focus on other precarious health conditions (Falgares et al., 2019). A certain correlation is therefore confirmed between negative affectivity, levels of awareness, coping strategies and a certain fragility and predisposition towards types of psychopathology (Meyer, 2001; Watson and Clark, 1984). More contradictory are the results reported in the systematic review by Xiong and colleagues (Xiong et al., 2020). In facts, if on the one hand they confirm the protectivity of a secure attachment and a coping approach, on the other hand they also consider an avoidant style as a protective one, differently from anxious style. According to the authors, this outcome could be explained by people with an avoidant style that might seem calm in a stressful situation or could experiment less distress with social distancing and self-isolation.
The differences between genders reflect the findings of other studies carried out on the COVID-19 pandemic (Li et al., 2020; Liu et al., 2020; Wang et al., 2020d), with the female population appearing to be generally more exposed to the effects of the pandemic with a more severe symptomatology than of the one of the male population. Furthermore, having children seems to be a risk factor only with regards to the IES-R scale which measures the chances of developing PTSD caused by the trauma.
Even a number of social factors are partially linked to an increased psychopathological risk, as already alluded to by other authors (Brooks et al., 2020; Cao et al., 2020; Wang et al., 2020d). In this particular case, this work documented a significant increase in depression in the DASS-21 scale amongst people with an elementary school education compared to the rest of the sample, while in the Anxiety subscale less anxiety was registered amongst those participants belonging to the higher income bracket compared to the other income brackets.
The categories at the highest risk in socio-demographic terms are, therefore, confirmed as being the female population and people with lower education and income (Cao et al., 2020). However, it was not possible to detect any significant differences between various forms of occupation.
Other determining factors in worsening the symptomatology and impact of COVID-19 on the population seem to be, on the one hand, knowing people who are infected and, on the other hand, the characteristics of the place people live in. With regards to the first aspect, people with acquaintances who are infected are at greater risk, especially in relation to the DASS-21 Stress and Anxiety subscale and to the IES-R scale with regards to the risk of PTSD. With regards to the second aspect, those respondents who stated not to have open-air spaces in their homes were in a more critical situation than those ones living in dwelling with balconies, terraces and private gardens in which they could distract themselves during the pandemic.
Curiously enough and contrary to what literature may have led us to expect (Cheval et al., 2020; López-Bueno et al., 2020; Stanton et al., 2020), going out for a walk and performing physical exercise are not useful factors for the prevention of stress, anxiety and depression and can even be worsening factors with regards to the risk of PTSD. This could be explained by the worries caused by leaving the house and by the restrictions imposed during periods of lockdown. At the same time, the study also documented how carrying out other activities, such as non-essential shopping, does not significantly create any greater or lesser psychopathological risk.
Considering that the respondents were located in different countries, no significant random effect on the independent variables of the country groupings was encountered. Moreover, a significant and constant effect was registered with country variables regarding levels of stress, symptoms of depression and of anxiety and with regards to the risk of PTSD. More specifically, countries such as Iran and Ecuador appear to be more closely associated with a greater psychological impact with regards to the risks relating to PTSD, while Norway is the country with the smallest risk. Considering the stress scales, respondents from Italy suffer most from the impact of the pandemic while respondents from China suffer the least with regards to stress levels. Even considering the scores regarding depression and anxiety, Italy is the worst affected country while, according to the DASS-21 Anxiety subscale, Ecuador is the worst hit country. The Chinese participants are the ones who have reacted better than anyone to the emergency with regards to levels of depression and anxiety.
An additional factor, that in literature has already emerged as being relevant in situations of crisis, is the one defined by the means of communication and of information: greater risks are associated with communication and the incessant exposure to potentially traumatic events in the media (Neria and Sullivan, 2011; Roy et al., 2020) and eventual fake news and disinformation (Shuja et al., 2020; Roy et al., 2020; Quinn et al., 2018).
The results obtained in this work partially confirm the findings of previous studies. As a matter of fact, according to our research, those individuals who use internet to search for information about the pandemic situation are associated to higher scores on the stress, depression and PTSD scales compared to those who obtain information via radio or television. These same trend in the results are found when comparing those individuals who obtain their information from friends and family to those ones who mainly use radio and television as their information source. Furthermore, there is a strong association between the amount of time spent to search for information and the relative score. In fact, those ones who only search for information from two to five times a week are less at risk with regards to psychopathological disorders compared to those ones who never do so or to those ones who, quite at the opposite, obstinately look for news about the pandemic several times a day.
Finally, those ones who moderately use social networks by spending an average of one or two hours per day will suffer less from the consequences of the lockdowns caused by COVID-19 compared to those ones excessively use or do not use social networks at all.
These latter results, which are relative to an excessive exposure to news reporting and to the use of technology, shed light on two important implications. On the one hand, the results highlight the dangers of mass information which may be unchecked, biased and organised without adequate public awareness (Shuja et al., 2020; Roy et al., 2020; Quinn et al., 2018), such as through word of mouth from friends and acquaintances. On the other hand the results of this study underline that the use of social media can be considered as being a protective factor, with the aim of distracting oneself and nurturing his or her social network, but on the sole condition that this is done with moderation.
Even in this case, comparing these results with the systematic review of Xiong and colleagues (Xiong et al., 2020), it is noted that being female, belonging to lowest educational background, knowing and being concerned about infected people and being continuously exposed to COVID-19 news are psychopathological risk factors. In addition, while for the systematic review belonging to a poor economic status is predictive of psychopathology, in this study it was observed that people in highest economic status are less vulnerable. Differently, the systematic review also found that occupation is a predictive psychopathological factor; in particular, students and unemployed suffer more severe consequences of COVID-19 pandemic. This difference could be explained by the mediation of different factors such as age, income bracket and education.
When it comes to comparing the respondents located in different countries, both in this study and in the systematic review (Xiong et al., 2020), psychopathological symptoms could be explained by the degree of outbreak severity, government readiness, degree and timing of quarantine measures, national economic situation, disclosure of COVID-19 information and other possible sociocultural elements.
Moreover, as a limitation of this study, this research did not investigate the use of some precautional measures that, according to the current literature, influence psychopathological levels such as hand hygiene and wearing face mask (Wang et al., 2020a, 2020d); for example, Wang and colleagues (Wang et al., 2020a) demonstrated that there are different habits about using face masks between Chinese and Polish subjects. Specifically, the less frequent use of the face mask by Polish individuals is correlated with higher physical and psychopathological symptoms.
5. Conclusions
In this study data regarding the psychological impact on individuals were collected from more than 1600 subjects located in seven countries (Australia, China, Ecuador, Iran, Italy, Norway and the United States) affected by the recent COVID-19 pandemic. A number of differences found in the numerousness of the groups of variables, combined with differences of sociocultural nature and the temporal development of the pandemic, created a plausible source of difficulty in analysing and generalizing the data presented in this study. On the other hand, the model of analysis adopted enables to draw some significant conclusions regarding the psychological effects related to the global pandemic.
Ultimately, during the early months of the pandemic, a considerable portion of the global population appears to have suffered the psychological consequences arising from the enactment of lockdown measures, as depression, anxiety, stress and possible risks of PTSD were encountered in more than half of the sample individuals. Some factors appear to accentuate the onset of these psychopathological problems. More specifically, being a female, having a lower level of education and income, carrying out outdoor activities, being excessively exposed to news reporting or being acquainted with people who are infected seem to be important risk factors. In addition, being a very active user of social networks or being a person not employing technology at all are other risk factors, as well as, to some extent, having children. On the flip side, having the possibility to benefit from an open-air space at home, exposing oneself to news updates regarding the COVID-19 development in a responsible manner and keeping moderate communications with acquaintances in social networks are all elements that offer protection against the psychological impact of the pandemic. Furthermore, a greater mindful awareness and the use of coping strategies generally indicate a higher resistance to the adversities of the pandemic, while a larger use of avoidance strategies is linked to a higher risk of developing psychopathological symptoms.
These results, therefore, become fundamental in determining which of the factors can cause a worsening of psychological symptoms during a pandemic such as COVID-19. At the same time, these findings are invaluable when it comes to demonstrate the importance of intervention to be performed by service institutions and mass-media, which should aim at correctly informing the public in a proper, unbiased and prudent fashion. These results are no less important in highlighting the need to offer psychological support to the population and, above all, to the most vulnerable individuals. In conclusion, in the light of the impact that the pandemic event entails on the global population, it will be imperative and interesting to understand the long-term effects by examining the results of a possible follow-up study which may take place when the global emergency is over. Furthermore, it is also desirable to gather further in-depth analyses encompassing a larger number of countries affected by the pandemic, surveying a larger sample of subjects and evaluating the effect of precautional measures.
Author contributions
Marco Passavanti for his involvement during the statistical analysis phase, for the initial conceptualization of the questionnaire and for drafting the article;
Alessandro Argentieri for the commitment during the statistical analysis phase and for drafting the article as well as for translating the survey into Spanish;
Diego Maria Barbieri for circulating the questionnaire to all the co-authors that took part in this study and managing of authors and co-authors and for the first revision of the article;
Marius Tangerås, Baowen Lou, Seyed Ali Foroutan Mirhosseini and Rosa Garcia Valverde for translating the article respectively into Norwegian, Chinese, Iranian and Spanish;
All authors and co-authors who were involved in circulating the study and in the revision of the article.
Conflict of interest and authorship conformation form
All authors have participated in (a) conception and design, or analysis and interpretation of the data; (b) drafting the article or revising it critically for important intellectual content; and (c) approval of the final version. This manuscript has not been submitted to, nor is under review at, another journal or other publishing venue.
The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
References
- Acter T., Uddin N., Das J., Akhter A., Choudhury T.R., Kim S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.138996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S.F., Quadeer A.A., McKay M.R. Preliminary Identification of Potential Vaccine Targets for the COVID-19 Coronavirus (SARS-CoV-2) Based on SARS-CoV Immunological Studies. Viruses. 2020;12(3):254. doi: 10.3390/v12030254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baiano C., Zappullo I., The LabNPEE Group. Conson M., The LabNPEE Group Tendency to Worry and Fear of Mental Health during Italy’s COVID-19 Lockdown. Int J Environ Res Public Health. 2020;17(16):5928. doi: 10.3390/ijerph17165928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S.R., Bloom N., Davis S.J., Terry S.J. National Bureau of Economic Research; Cambridge, MA: 2020. COVID-induced Economic Uncertainty (NBER Working Paper 26983) [Google Scholar]
- Banerjee D., Rai M. Social isolation in Covid-19: the impact of loneliness. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020922269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbieri D.M., Lou B., Passavanti M., et al. A survey dataset to evaluate the changes in mobility and transportation due to COVID-19 travel restrictions in Australia, Brazil, China, Ghana, India, Iran, Italy, Norway, South Africa, United States. Data Brief. 2020;33 doi: 10.1016/j.dib.2020.106459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbieri D.M., Lou B., Passavanti M., et al. Survey data regarding perceived air quality in Australia, Brazil, China, Ghana, India, Iran, Italy, Norway, South Africa, United States before and during Covid-19 restrictions. Data Brief. 2020;32 doi: 10.1016/j.dib.2020.106169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonaccorsi G., Pierri F., Cinelli M., Flori A., Galeazzi A., Porcelli F., Schmidt A.L., Valensise C.M., Scala A., Quattrociocchi W., Pammolli F. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. U.S.A. 2020;117(27):15530–15535. doi: 10.1073/pnas.2007658117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Aldana D.K., Quintero-Rada K., Montoya-Posada J.P., Ramírez-Ocampo S., Paniz-Mondolfi A., Rabaan A.A., Sah R., Rodríguez-Morales A.J. SARS-CoV, MERS-CoV and now the 2019-novel CoV: have we investigated enough about coronaviruses? - A bibliometric analysis. Travel Med Infect Dis. 2020;33 doi: 10.1016/j.tmaid.2020.101566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K.W., Ryan R.M. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Butler L.D., Blasey C.M., Garlan R.W., McCaslin S.E., Azarow J., Chen X.-.H.…Spiegel D. Posttraumatic Growth Following the Terrorist Attacks of September 11, 2001: Cognitive, Coping, and Trauma Symptom Predictors in an Internet Convenience Sample. Traumatology. 2005;11(4):247–267. doi: 10.1177/153476560501100405. [DOI] [Google Scholar]
- Bystritsky A., Vapnik T., Maidment K., Pynoos R.S., Steinberg A.M. Acute responses of anxiety disorder patients after a natural disaster. Depress Anxiety. 2000;11(1):43–44. doi: 10.1002/(SICI)1520-6394(2000)11:1<43::AID-DA7>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol’s too long: consider the Brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cheval B., Sivaramakrishnan H., Maltagliati S., Fessler L., Forestier C., Sarrazin P.…Boisgontier M.P. 2020. Relationships Between Changes in Self-Reported Physical Activity and Sedentary Behaviours and Health During the Coronavirus (COVID-19) Pandemic in France and Switzerland. April 25. [DOI] [PubMed] [Google Scholar]
- Chew N., Lee G., Tan B., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Williamson G. In: The Social Psychology of Health. Spacapan S., Oskamp S., editors. Sage; Newbury Park, CA: 1988. Perceived Stress in a Probability Sample of the United States. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A Global Measure of Perceived Stress. J Health Soc Behav. 1983;24(4):385–396. www.jstor.org/stable/2136404 Retrieved August 3, 2020, from. [PubMed] [Google Scholar]
- Conversano C., Di Giuseppe M., Miccoli M., Ciacchini R., Gemignani A., Orrù G. Mindfulness, Age and Gender as Protective Factors Against Psychological Distress During COVID-19 Pandemic. Front Psychol. 2020;11:1900. doi: 10.3389/fpsyg.2020.01900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Dawson D.L., Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J Contextual Behav Sci. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vos J. The effect of COVID-19 and subsequent social distancing on travel behavior. Transportation Research Interdisciplinary Perspectives. 2020;5 doi: 10.1016/j.trip.2020.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delucchi K.L., Bostrom A. Methods for analysis of skewed data distributions in psychiatric clinical studies: working with many zero values. Am J Psychiatry. 2004;161(7):1159–1168. doi: 10.1176/appi.ajp.161.7.1159. [DOI] [PubMed] [Google Scholar]
- Deng N., Allison J.J., Fang H.J., et al. Using the bootstrap to establish statistical significance for relative validity comparisons among patient-reported outcome measures. Health Qual Life Outcomes. 2013;11:89. doi: 10.1186/1477-7525-11-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan H., Yan L., Ding X., Gan Y., Kohn N., Wu J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: changes, predictors and psychosocial correlates. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg S.A., Shen B.J., Schwarz E.R., Mallon S. Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. J Behav Med. 2012;35(3):253–261. doi: 10.1007/s10865-011-9358-0. [DOI] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/en/covid-19/latest-evidence/clinical (accessed August 15, 2020).
- Falgares G., Lo Gioco A., Verrocchio M.C., Marchetti D. Anxiety and depression among adult amputees: the role of attachment insecurity, coping strategies and social support. Psychol Health Med. 2019;24(3):281–293. doi: 10.1080/13548506.2018.1529324. [DOI] [PubMed] [Google Scholar]
- Garre-Olmo J., Turró-Garriga O., Martí-Lluch R., Zacarías-Pons L., Alves-Cabratosa L., Serrano-Sarbosa D., Vilalta-Franch J., Ramos R., Girona Healthy Region Study Group Changes in lifestyle resulting from confinement due to COVID-19 and depressive symptomatology: a cross-sectional a population-based study. Compr Psychiatry. 2021;104 doi: 10.1016/j.comppsych.2020.152214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurvich C., Thomas N., Thomas E.H., Hudaib A.R., Sood L., Fabiatos K., Sutton K., Isaacs A., Arunogiri S., Sharp G., Kulkarni J. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. The International Journal of Social Psychiatry. 2020 doi: 10.1177/0020764020961790. 20764020961790. Advance Online Publication. [DOI] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J.D., Crawford J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. The British Journal of Clinical Psychology. 2005;44(Pt 2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Ann. Acad. Med. Singap. 2020;49(3):155–160. https://pubmed.ncbi.nlm.nih.gov/32200399/ [PubMed] [Google Scholar]
- Hosseini S.M., Latifi S., Kelishadi R. Analysis of Factors Affecting the Body Mass Index in a National Sample of Iranian Children and Adolescents: bootstrapping Regression. Adv Biomed Res. 2017;6:152. doi: 10.4103/2277-9175.219417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kar N., Bastia B.K. Post-traumatic stress disorder, depression and generalised anxiety disorder in adolescents after a natural disaster: a study of comorbidity. Clinical Practice and Epidemiology in Mental Health: CP & EMH. 2006;2:17. doi: 10.1186/1745-0179-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamura N., Kim Y., Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry. 2001;158(3):484–486. doi: 10.1176/appi.ajp.158.3.484. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le X., Dang A.K., Toweh J., Nguyen Q.N., Le H.T., Do T., Phan H., Nguyen T.T., Pham Q.T., Ta N., Nguyen Q.T., Nguyen A.N., Van Duong Q., Hoang M.T., Pham H.Q., Vu L.G., Tran B.X., Latkin C.A., Ho C., Ho R. Evaluating the Psychological Impacts Related to COVID-19 of Vietnamese People Under the First Nationwide Partial Lockdown in Vietnam. Front Psychiatry. 2020;11:824. doi: 10.3389/fpsyt.2020.00824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Quéré C., Jackson R.B., Jones M.W., et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat. Clim. Chang. 2020;10:647–653. doi: 10.1038/s41558-020-0797. [DOI] [Google Scholar]
- Leung G.M., Lam T.H., Ho L.M., Ho S.Y., Chan B.H., Wong I.O., Hedley A.J. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. 2003;57(11):857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Wang Y., Xue J., Zhao N., Zhu T. The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: a Study on Active Weibo Users. Int J Environ Res Public Health. 2020;17(6):2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J., Guan Z., Wu P. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R., Calatayud J., Ezzatvar Y., Casajús J.A., Smith L., Andersen L.L., López-Sánchez G.F. Activity and Current Perceived Anxiety and Mood in the Initial Phase of COVID-19 Confinement. Front. Psychiatry. 2020;11:729. doi: 10.3389/fpsyt.2020.00729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotfi M., Hamblin M.R., Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin. Chim. Acta. 2020;508:254–266. doi: 10.1016/j.cca.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main A., Zhou Q., Ma Y., Luecken L.J., Liu X. Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. J Couns Psychol. 2011;58(3):410–423. doi: 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: immediate Psychological Responses and Associated Factors. Int J Environ Res Public Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer B. Coping with severe mental illness: relations of the Brief COPE with symptoms, functioning, and well-being. J Psychopathol Behav Assess. 2001;23(4):265–277. doi: 10.1023/A:1012731520781. [DOI] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morganstein J.C., Ursano R.J. Ecological Disasters and Mental Health: causes, Consequences, and Interventions. Front Psychiatry. 2020;11:1. doi: 10.3389/fpsyt.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y., Sullivan G.M. Understanding the mental health effects of indirect exposure to mass trauma through the media. JAMA. 2011;306(12):1374–1375. doi: 10.1001/jama.2011.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ningthoujam R. COVID 19 can spread through breathing, talking, study estimates. Current medicine research and practice. 2020;10(3):132–133. doi: 10.1016/j.cmrp.2020.05.003. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrozo-Pupo J.C., Pedrozo-Cortés M.J., Campo-Arias A. Perceived stress associated with COVID-19 epidemic in Colombia: an online survey. Cad Saude Publica. 2020;36(5) doi: 10.1590/0102-311x00090520. [DOI] [PubMed] [Google Scholar]
- Quinn K.G., Kelly J.A., Di Francesco W.J., Tarima S.S., Petroll A.E., Sanders C., Lawrence J., Amirkhanian Y.A. The Health and Sociocultural Correlates of AIDS Genocidal Beliefs and Medical Mistrust Among African American MSM. AIDS Behav. 2018;22(6):1814–1825. doi: 10.1007/s10461-016-1657-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapisarda F., Vallarino M., Cavallini E., Barbato A., Brousseau-Paradis C., De Benedictis L., Lesage A. The Early Impact of the Covid-19 Emergency on Mental Health Workers: a Survey in Lombardy. Italy. International Journal of Environmental Research and Public Health. 2020;17(22):8615. doi: 10.3390/ijerph17228615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102083. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM: Monthly Journal of the Association of Physicians. 2020 doi: 10.1093/qjmed/hcaa201. hcaa201Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakil M.H., Munim Z.H., Tasnia M., Sarowar S. COVID-19 and the environment: a critical review and research agenda. Sci. Total Environ. 2020;745 doi: 10.1016/j.scitotenv.2020.141022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuja K.H., Aqeel M., Jaffar A., Ahmed A. COVID-19 Pandemic and Impending Global Mental Health Implications. Psychiatr Danub. 2020;32(1):32–35. doi: 10.24869/psyd.2020.32. [DOI] [PubMed] [Google Scholar]
- Sim K., Huak Chan Y., Chong P.N., Chua H.C., Wen Soon S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res. 2010;68(2):195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim K., Chua H.C. The psychological impact of SARS: a matter of heart and mind. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2004;170(5):811–812. doi: 10.1503/cmaj.1032003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, R., & Adhikari, R. (2020). Age-structured impact of social distancing on the COVID-19 epidemic in India. arXiv preprint arXiv:2003.12055.
- Skapinakis P., Bellos S., Oikonomou A., Dimitriadis G., Gkikas P., Perdikari E., Mavreas V. Depression and Its Relationship with Coping Strategies and Illness Perceptions during the COVID-19 Lockdown in Greece: a Cross-Sectional Survey of the Population. Depress Res Treat. 2020;2020 doi: 10.1155/2020/3158954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Sprang, G., & Silman, M. (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster medicine and public health preparedness, 7(1), 105–110. https://doi.org/10.1017/dmp.2013.22. [DOI] [PubMed]
- Stanton R., To Q.G., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., Fenning A.S., Vandelanotte C. Depression, Anxiety and Stress during COVID-19: associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabata S., Imai K., Kawano S., Ikeda M., Kodama T., Miyoshi K., Obinata H., Mimura S., Kodera T., Kitagaki M., Sato M., Suzuki S., Ito T., Uwabe Y., Tamura K. Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30482-5. S1473-3099(20)30482-5. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan B., Chew N., Lee G., Jing M., Goh Y., Yeo L., Zhang K., Chin H.K., Ahmad A., Khan F.A., Shanmugam G.N., Chan B., Sunny S., Chandra B., Ong J., Paliwal P.R., Wong L., Sagayanathan R., Chen J.T., Ying Ng A.Y.…Sharma V.K. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Annals of internal medicine. 2020:M20–M1083. doi: 10.7326/M20-1083. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tee M.L., Tee C.A., Anlacan J.P., Aligam K., Reyes P., Kuruchittham V., Ho R.C. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Umucu E., Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil Psychol. 2020;65(3):193–198. doi: 10.1037/rep0000328. [DOI] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupała A., Grabowski D., Pan R., Adamus K., Wan X., Hetnał M., Tan Y., Olszewska-Guizzo A., Xu L., McIntyre R.S., Quek J., Ho R., Ho C. The Association Between Physical and Mental Health and Face Mask Use During the COVID-19 Pandemic: a Comparison of Two Countries With Different Views and Practices. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Xia Q., Xiong Z., Li Z., Xiang W., Yuan Y., Liu Y., Li Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: a web-based survey. PLoS ONE. 2020;15(5) doi: 10.1371/journal.pone.0233410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D., Clark L.A. Negative affectivity: the disposition to experience aversive emotional states. Psychol Bull. 1984;96(3):465–490. doi: 10.1037/0033-2909.96.3.465. [DOI] [PubMed] [Google Scholar]
- Wehrens R., Putter H., Buydens L. The bootstrap: a tutorial. Chemometrics and Intelligent Lab Syst. 2000;2000(54):35–52. doi: 10.1016/S0169-7439(00)00102-7. [DOI] [Google Scholar]
- Weiss D.S., Marmar C.R. In: Assessing Psychological Trauma and PTSD. Wilson J., Keane T.M., editors. Guilford; New York: 1996. The Impact of Event Scale - Revised; pp. 399–411. [Google Scholar]
- Wells C.R., Sah P., Moghadas S.M., Pandey A., Shoukat A., Wang Y., Wang Z., Meyers L.A., Singer B.H., Galvani A.P. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc. Natl. Acad. Sci. U.S.A. 2020;117(13):7504–7509. doi: 10.1073/pnas.2002616117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Coronavirus disease (COVID-19) pandemic 2020a. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed August 15, 2020).
- WHO. Coronavirus Disease (COVID-19) Dashboard 2020b. https://covid19.who.int/ (accessed August 15, 2020).
- WHO. COVID-19 – Public Health Emergency of International Concern (PHEIC). Global research and innovation forum. 2020c. https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum (accessed August 15, 2020).
- Wright D.B., London K., Field A.P. Using Bootstrap Estimation and the Plug-in Principle for Clinical Psychology Data. J Exp Psychopathol. 2011:252–270. doi: 10.5127/jep.013611. [DOI] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J Trauma Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan L., Gan Y., Ding X., Wu J., Duan H. The relationship between perceived stress and emotional distress during the COVID-19 outbreak: effects of boredom proneness and coping style. J Anxiety Disord. 2020;77 doi: 10.1016/j.janxdis.2020.102328. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H. The more exposure to media information about COVID-19, the more distressed you will feel. Brain Behav. Immun. 2020;87:167–169. doi: 10.1016/j.bbi.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]