Global efforts for development of a COVID-19 vaccine are yielding multiple results including some new and as yet unlicensed technologies.1 Reception of these vaccine candidates by a skeptical public will challenge wide acceptance of new vaccines. Regulatory safety thresholds are a minimum bar that a product must pass to attain regulatory approval, but for the general public, cumulative safety experience will be important. Trust is earned with time, and with repeated experience. Vaccines have a long safety history, but COVID-19 vaccines are new. In this context, Yanjun Zhang and colleagues' report of their phase 1/2 trial of a new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine in The Lancet Infectious Diseases is instructive.2
In their randomised, placebo-controlled trial, Zhang and colleagues assessed two concentrations of the vaccine CoronaVac (Sinovac Life Sciences, Beijing, China), 3 μg and 6 μg per 0·5 mL diluent, in a two-dose regimen, using both 14 and 28 day intervals.2 The phase 1 trial was done in a dose-escalation manner to ensure the safety of dosing in the phase 2 trial. Their rationale for this study design was that extended intervals between doses might result in more durable responses, whereas regimens with shorter intervals between doses might be of use in early outbreak containment. Primary safety results were reported up to day 28 after each dose of study drug, while neutralising immunogenicity data were assessed at 14 days after the second dose for the day 0 and 14 vaccination cohort, and 28 days after the second dose for the days 0 and 28 vaccination cohort.
Zhang and colleagues enrolled 144 participants into the phase 1 trial and 600 participants into the phase 2 trial. 397 (53%) of 743 participants were female, and the mean age in the pooled days 0 and 14 vaccination cohort was 42·6 years (SD 9·4) and in the days 0 and 28 vaccination cohort was 42·1 (9·7). In phase 1, among vaccine recipients, rates of adverse reactions were lower for the lower dose groups, and lower regardless of dose in the days 0 and 28 vaccination cohort than in the days 0 and 14 vaccination cohort (seven [29%] of 24 participants in the 3 μg group vs nine (38%) of 24 in the 6 μg group in the days 0 and 14 vaccination cohort and three [13%] of 24 in the 3 μg group vs four [17%] of 24 in the 6 μg group in the days 0 and 28 vaccination cohort). Seroconversion rates of neutralising antibodies to SARS-CoV-2 were moderate overall, although quite substantially higher 28 days after the second dose than at 14 days after the second dose,2 but the trial design means we cannot assess whether this finding is a function of the regimen or of the timing of testing.
In phase 2, using a different more scalable manufacturing process for the vaccine that resulted serendipitously in more concentrated epitopic presentation, adverse events such as mild injection-site pain, occurred in 81 (17%) of 480 vaccine recipients. Dose made no difference, but the delayed regimen induced fewer adverse reactions overall among vaccine recipients (82 [34%] of 240 in the days 0 and 14 vaccination cohort vs 46 [19%] of 120 in the days 0 and 28 vaccination cohort).2 Geometric mean titre (GMT) for neutralising antibodies was much higher with the phase 2 product, and was broadly similar by dose and regimen, although somewhat higher at higher dose and with longer interval (eg, in the phase 2 trial, the GMT was 23·8 [95% CI 20·5–27·7] for the 3 μg group and 30·1 [26·1–34·7] for the 6 μg group 28 days after the second dose in the days 0 and 14 vaccination cohort, and 44·1 [37·2–52·2] in the 3 μg group and 65·4 [56·4–75·9]) in the 6 μg group 28 days after the second dose in the days 0 and 28 vaccination cohort). However, neutralising titres were substantially lower than those seen in 117 convalescent patients who previously had COVID-19 tested in the same laboratory (in 6 μg group in days 0 and 28 vaccination cohort, 28 days after second dose, GMT was 65·4 [95% CI 56·4–75·9] vs in convalescent patients, 163·7 [128·5–208·6]).2 T-cell responses were low,2 as might be expected with an inactivated vaccine.3 Taken together and in absence of known correlates of protection for COVID-19, efficacy results from phase 3 clinical trials will be all the more important. Although immunogenicity was slightly lower in the low-dose groups than in the high-dose groups, for manufacture to stretch further—ie, more vaccine doses being produced for the same amount of antigen (an important consideration given global need)—phase 3 trials will use the lower dose of 3 μg (eg, NCT04456595).
This COVID-19 vaccine candidate uses β-propriolactone to inactivate SARS-CoV-2 and an alum adjuvant,2 methods also used in influenza and other vaccines and for which safety is well established.4, 5 The alum adjuvant might imply immunogenicity in older people (aged >60 years) too, although these trials did not recruit people older than 60 years. And like for influenza vaccines, a demonstration of longevity of response and of empiric protection from this candidate will be important, even using a two-dose regimen.6
Two lessons arise from this study. First, we can use existing tried and tested platforms to produce vaccines. We know their limitations, but we also know that in previous incarnations they are usually acceptably safe. And second, unexpected things can happen in science as in life. A change in manufacturing process to scale up production can change the performance of a vaccine. It can also affect reactogenicity, although reactogenicity does not seem to have been affected in this study. We should expect the unexpected when considering vaccine safety, and vigilantly observe for unanticipated harms. Like all phase 2 trials, the results must be interpreted with caution until phase 3 results are published. But even then, after phase 3 trial completion and after licensure, we should prudently remain cautious. Pharmacovigilance will be needed long into phase 4 studies, and we should recall that COVID-19 vaccine harms could occur in any of the following ways: real direct harms from adverse events or from disease enhancement; perceived direct harms temporally but not causally associated with receipt of the vaccine (eg, in an older population or among those with excess comorbidities who are already at risk for adverse health events);7 and suboptimal vaccine deployment and unrealistic expectations or inadequate safety communication (eg, a vaccine that reduces disease [the primary outcome in all phase 3 COVID-19 vaccine trials] but not transmission [an unpowered secondary outcome], and that works less well in older individuals or is not taken up by high-risk groups, could allow unmitigated transmission to paradoxically worsen population outcomes for groups at risk, especially if vaccination leads to lower adherence to physical distancing and use of masks). Global and national regulators have declared licensure would be approved for efficacy against disease of 50% with bounds well below that, and unknown efficacy against transmission. Therefore, should such a vaccine be licensed, and without clear protective correlates to allow bridging studies, early licensure could stymie developments of better future candidates, and pose ethical challenges for other trials commencing or that are ongoing.8, 9, 10 Regardless, the trust of the global community is hardwon and achieved through total transparency and realism of expectation, both during and long after vaccine development and deployment.
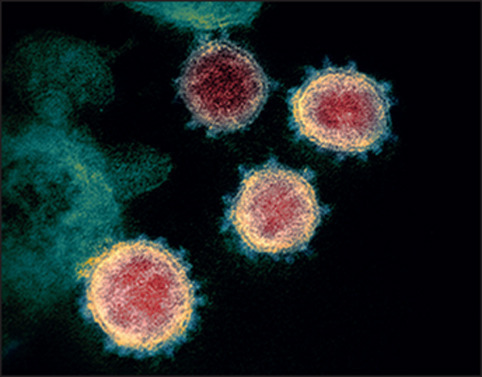
© 2021 Flickr - NIAID
Acknowledgments
NB-Z has previously received investigator-initiated research funding from GlaxoSmithKline, Takeda Pharmaceuticals, and Merck-Sharpe-Dohme. SK declares no competing interests.
References
- 1.Le TT, Cramer JP, Chen R, Mayhew S. Evolution of the COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19:667–668. doi: 10.1038/d41573-020-00151-8. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Zheng G, Pan H, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30843-4. published online Nov 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kochhar S, Excler JL, Kim D, et al. The Brighton Collaboration standardized template for collection of key information for benefit-risk assessment of inactivated viral vaccines. Vaccine. 2020;38:6184–6189. doi: 10.1016/j.vaccine.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fan C, Ye X, Ku Z, et al. Beta-propiolactone inactivation of coxsackievirus A16 induces structural alteration and surface modification of viral capsids. J Virol. 2017;91:e00038–e00117. doi: 10.1128/JVI.00038-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delrue I, Verzele D, Madder A, Nauwynck HJ. Inactivated virus vaccines from chemistry to prophylaxis: merits, risks and challenges. Expert Rev Vaccines. 2012;11:695–719. doi: 10.1586/erv.12.38. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J. How long do vaccines last? The surprising answers may help protect people longer. ScienceMag, AAAS. April 18, 2019. https://www.sciencemag.org/news/2019/04/how-long-do-vaccines-last-surprising-answers-may-help-protect-people-longer
- 7.Kochhar S, Salmon DA. Planning for COVID-19 vaccines safety surveillance. Vaccine. 2020;38:6194–6198. doi: 10.1016/j.vaccine.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krause P, Fleming TR, Longini I, et al. COVID-19 vaccine trials should seek worthwhile efficacy. Lancet. 2020;396:741–743. doi: 10.1016/S0140-6736(20)31821-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peiris M, Leung GM. What can we expect from first-generation COVID-19 vaccines? Lancet. 2020 doi: 10.1016/S0140-6736(20)31976-0. published online Sept 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen J. Early approval of a COVID-19 vaccine could stymie the hunt for better ones. ScienceMag, AAAS. Oct 14, 2020. https://www.sciencemag.org/news/2020/10/early-approval-covid-19-vaccine-could-stymie-hunt-better-ones


