Abstract
This study investigated the presence of SARS-CoV-2 in air of public places such as shopping centers, a post office, banks, governmental offices, and public transportation facilities including an airport, subways, and buses in Tehran, Iran. A total of 28 air samples were collected from the eight groups of public and transportation locations. The airborne particle samples were collected on PTFE or glass fiber filters using two types of samplers with flow rates of 40 and 3.5 L/min, respectively. The viral samples were leached and concentrated, and RNA was extracted from each. The presence of viral RNA was evaluated using novel coronavirus nucleic acid diagnostic real time PCR kits. In 64% of the samples, SARS-CoV-2 RNA (62% and 67% from the public places and transportation, respectively) was detected. Positive samples were detected in banks (33%), shopping centers (100%), governmental offices (50%), the airport (80%), subway stations (50%), subway trains (100%), and buses (50%). Logistic regression showed that number of people present during the sampling and the sampled air volume were positively associated with presence of SARS-CoV-2; while the percentage of people with masks, air temperature, and sampling site's volume were negatively related to SARS-CoV-2's presence. However, none of these associations were statistically significant. This study showed that most public places and transportation vehicles were contaminated with SARS-CoV-2. Thus, strategies to control the spread of COVID-19 should include reducing the number of people in indoor spaces, more intense disinfection of transport vehicles, and requiring people to wear masks.
Keywords: COVID-19, Airborne transmission, PCR, Aerosol
Graphical abstract
1. Introduction
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has affected millions of people worldwide since its first emergence in December 2019 in Wuhan, China. Initial reports indicated that the disease can be transmitted through respiratory droplets and contact with contaminated surfaces (Public Health England, 2020). However, from the beginning, various researchers raised concerns about the airborne transmission of SARS-CoV-2. They argued that the past experience from the similar viruses such as influenza and SARS-CoV-1 (Cowling et al., 2013) supported the hypothesis of transmissibility of the novel virus through air. In addition, coughing, sneezing, and even normal speaking are known to produce many particles in size distributions that can transfer viruses (Han et al., 2013; Johnson et al., 2011). These were the theoretical reasons supporting the airborne transmission hypothesis of SARS-CoV-2.
Several field studies have found the presence of SARS-CoV-2 in clinical and public locations in medical centers. Chia et al. (2020) sampled airborne infection isolation rooms and reported that the novel coronavirus were found in particle sized >4 μm and 1–4 μm, but not in <1 μm particles. SARS-CoV-2 was detected in the intensive care unit (ICU) of a hospital in Milan (Razzini et al., 2020a). In addition to the positive results from the samples taken in clinical settings such as intensive care units (ICU), isolation rooms, etc. (Guo et al., 2020; Lednicky et al., 2020a,b), some studies reported that SARS-CoV-2 was observed in the public locations in hospitals such as department stores associated with the hospital (Liu et al., 2020), the entrance and public areas (Zhou et al., 2020), and hallways (Santarpia et al., 2020). However, some studies or samples have reported negative results on the presence of this virus in clinical settings and public areas of hospitals (Cheng et al., 2020; Faridi et al., 2020; Guo et al., 2020). Some factors such as sampling method and the total volume of air sampled can affect the results of such studies (Hadei et al., 2020).
To our knowledge, only one study has been reported that investigated the presence of SARS-CoV-2 in public places in cities. In that study, SARS-CoV-2 was detected in 94% of the ambient particulate matter samples taken from an industrialized area of Bergamo (Italy) (Setti et al., 2020). Combining these results with the existing literature, there was a strong possibility for airborne transmission of COVID-19. Therefore, there is a need to perform a study on the presence of this virus in public places and transportation systems where many people are in contact with each other on a daily basis. Such a study will provide additional information on the potential for airborne transmission of COVID-19 and determine high-risk places in the urban environment.
Iran has been experiencing a high rate of COVID-19 incidence and prevalence with more than 920,000 and 47,000 confirmed cases and deaths, respectively, through the end of November 2020. This period was after the end of the lockdown previously imposed to control COVID-19. Almost all professions were allowed to restart, and public areas were crowded with people. This return to more normal life provided a high potential for spreading COVID-19. This study was conducted to explore the presence of SARS-CoV-2 in the public places such as shopping centers, a post office, banks, offices, and public transportation facilities including airport, subways, and buses in Tehran, Iran.
2. Methods
2.1. Study design and sampling
This cross-sectional study was conducted in Tehran, the capital of Iran. Samples were taken during June and July 2020. A total of 28 air samples were collected from the sites located in different parts of the city. Sampling was limited because of the difficulties in obtaining permission and the general aversion for administrators to learn about potential problems. The sampling sites can be categorized into two major groups: I) public places, and II) public transportation systems.
Table 1 shows the description of sampling sites in public places and public transportation systems. The public places included banks (3 locations, 1 sample each), shopping centers (5 locations, 1 sample each), post office (1 location, 1 sample), and a governmental office building (one location, 4 samples). The sampling sites in public transportation systems were in Mehrabad airport (one location, 5 samples), subway stations (4 locations, 1 sample each), subway trains (2 locations, 1 sample each), and buses (4 locations, 1 sample each). Three different banks and one post office were sampled. The shopping centers included four places in Tehran's bazaar, and one shopping mall for electronic devices (Alaedin Commercial Complex). In case of the governmental offices, different areas of one building were sampled: client section at the first floor, inside gate at the first floor, and two office rooms. In addition, five spots in Mehrabad airport were sampled: three inspection gates, a transit lounge, and a waiting lounge. Various characteristics of sampling sites such as surface area, height, type of ventilation (natural, forced), temperature, the approximate number of people, and the approximate percentage of people wearing face mask were recorded. The number of people and percentage of those wearing face mask were estimated using the pictures taken every 10 min during the sampling. The numbers of people in each picture were averaged to obtain an overall estimated population.
Table 1.
Description of sampling sites in public places and public transportation systems.
| Site | Sample size | Description |
|---|---|---|
| Bank | 3 | Three different banks, one sample from each. |
| Shopping center | 5 | Four samples from Tehran's bazaar, and one sample from Alaedin mall. |
| Post office | 1 | One post office. |
| Office | 4 | Four samples from 1 office building: clients section, entrance, and inside two office rooms. |
| Airport | 5 | Five samples from Mehrabad Airport: transit lounge, and waiting lounge, and three inspection gates. |
| Subway station | 4 | Four different stations, one sample from each. |
| Subway train | 2 | Two different trains, one sample from each. |
| Bus | 4 | Four different buses, one sample from each. |
For all of the samples except for the buses and one of the subway train samples, an AV1000 sampler (China) with an average flow rate of 40 L/min and polytetrafluoroethylene (PTFE, diameter = 9 cm, pore size = 0.2 μm) filters were used. The AV1000 sampler collects total suspended particles (TSP). PTFE filters are reported to have suitable performance for sampling viruses such as SARS-CoV-1 (Rahmani et al., 2020). Sampling in the buses and one of the subway trains (total of 5 samples) was performed using an SKC pump (Universal PCXR4, SKC, South Korea) with an average flow rate of 3.5 L/min and glass fiber filters (diameter = 2 cm). Sampling duration was 1–1.5 h, depending on the site's limitations. The total volume of sampled air ranged from 200 to 240 and 1270–3496 L for the places sampled by SKC pump and AV1000 sampler, respectively. The samplers were placed at the height of 0.9–1.6 m above the ground. The minimum distance from the physical barriers and human individuals ranged 0.1–3.0 and 0.3–2.5 m. The high variation in these values originates from the site-specific characteristics, so that the distances in some cases such as buses, subway trains, and highly crowded places were small.
2.2. Virus concentration
The filters were shipped in well-sealed containers at 4 °C to the Virology Laboratory (RIGLD, Shahid Beheshti University of Medical Sciences). The samples were placed in 50 mL plastic centrifuge tubes containing 20 mL of Tris-glycine-beef extract buffer (TGBE, 100 mM Tris, 50 mM glycine, 3% (wt/vol) beef extract, pH = 9.5) followed by gently shaking of the tubes for 20 min at room temperature. Subsequently, the filters were removed from the tubes and 12.5% PEG-6000 and 2.5% NaCl at final concentration were added. The eluate was stirred at 4 °C for 2 h, and centrifuged at 11,000 g for 30 min (Alonso et al., 2017; Zuo et al., 2013). The pellet was suspended in 0.2 mL of PBS (pH = 7.2). The final pellet eluate was stored at −80 °C until further analyses.
To calculate the efficiency of the virus isolation method from the filter, attenuated live Infectious Bronchitis Virus (IBV), strain H-120, Massachusetts serotype, a virus of the coronaviridea family, which is a member of gamma-coronavirus, was selected as the SARS-CoV-2 model virus. Both viruses are from the same family, and very similar in structure and target tissue, although IBV causes infectious bronchitis in poultry. To calculate the efficiency, the virus solution was inoculated into the filter surface at separate points, and placed in a biosafety cabinet for 2 h to dry. After that, the concentration method was performed. Then, along with this sample, 20 μL of the vaccine, which was dissolved in 120 μL of water, was extracted and RT-qPCR test was performed on the resulting RNA. The result of the qPCR test showed that the recovery percentage is about 20% compared to the initial value.
2.3. Viral RNA extraction
Viral nucleic acids were extracted from 140 μL of the final eluate obtained from the second concentration step using a QIAamp RNA Mini Kit (Qiagen, Germany) to produce a final volume of 60 μL according to the manufacturer's protocol. The extracted nucleic acids were stored at −20 °C until further analysis.
2.4. SARS-CoV-2 RNA detection
The presence of Viral RNA was evaluated by novel coronavirus nucleic acid diagnostic real time PCR kit (Sansure Biotech, China) according to the manufacturer's instruction. The test utilized specific sequences of ORF1ab and nulceocapsid protein N genes as the target regions for amplification and detection. A RotorGene Q instrument (Qiagen, Germany) was used to perform the tests.
2.5. Quality assurance/quality control (QA/QC)
During the study, positive control samples (spiked IBV filters) along with the negative control samples were used as the quality control of the experiment to ensure the absence of false positive (possible cross-contaminations) and false negative (possible recovery failure). In addition, RT-PCR test was performed with positive and negative controls.
2.6. Statistical analyses
Logistic regression modeling was used to explore the effects of the parameters including air temperature, number of people, percentage of people wearing face masks, the sampling site volumes, and sampled air volume on the presence of SARS-Cov-2. These parameters were used as continuous independent variables, and the presence/absence of SARS-CoV-2 was entered to the model as a binary variable of zero and one. Due to low sample size, separate models were developed for the effect of each variable on SARS-CoV-2 presence. The association between the variables were expressed as odds ratios (ORs) with 95% confidence intervals (CIs). The modeling was performed using R programming software v. 3.6.3.
3. Results and discussion
Twenty-eight air samples were collected from nine public places and transportation system components. The detailed results for each sampling site are presented in Table 2 . Overall, 64% of the samples were positive for SARS-CoV-2 RNA. Characteristics of sampling sites such as the approximate room volume, air temperature, approximate number of people present during the sampling period, approximate percentage of people wearing face mask, and type of ventilation are also provided in Table 2. The sampled air volume at different sites ranged from 200 L in buses to 3496 L in subway trains. The sampled volume is a critical factor for these studies (Baghani et al., 2019; Hadei et al., 2018), since collecting a small air volume could produce a false negative result (Hadei et al., 2020). The average (±standard deviation) of air temperature was 27.3 (±3.4) °C. The number of people at the sampling site varied significantly based on the type of location. The percentage of people in Tehran's bazaars (shopping centers 1–4) who wore masks (3–20%) was markedly lower than in other locations (70–100%) except for the post office where only 10% of those present wore masks.
Table 2.
Presence of SARS-CoV-2 in sampling sites.
| Site | Sampling volume (m3) | Site volume (m3) | Temp. | No. of people | % of people wearing mask | Ventilationa | SARS-CoV-2 |
|---|---|---|---|---|---|---|---|
| Bank 1 | 1.453 | 810 | 30.4 | 150 | 85 | F | Negative |
| Bank 2 | 1.472 | 150 | 28.9 | 30 | 70 | N & F | Negative |
| Bank 3 | 1.271 | 525 | 29.3 | 80 | 80 | N & F | Positive |
| Shopping center 1b | 1.74 | 1350 | 29.6 | 550 | 5 | N | Positive |
| Shopping center 2b | 1.589 | 1350 | 27.6 | 700 | 3 | N | Positive |
| Shopping center 3b | 1.675 | 1000 | 23.9 | 350 | 20 | F | Positive |
| Shopping center 4b | 1.683 | 1350 | 28.1 | 600 | 3 | N | Positive |
| Shopping center 5b | 3.469 | 700 | 29.9 | 500 | 90 | N | Positive |
| Post office | 1.556 | 4000 | 25.2 | 250 | 10 | F | Negative |
| Office 1c | 2.11 | 280 | 24.4 | 80 | 80 | F | Positive |
| Office 2c | 1.626 | 504 | 23.2 | 250 | 80 | F | Positive |
| Office 3c | 1.786 | 84 | 24.3 | 25 | 80 | N & F | Negative |
| Office 4c | 1.787 | 70 | 23.8 | 20 | 85 | F | Negative |
| Airport 1d | 3.396 | 256 | 19.3 | 150 | 90 | F | Positive |
| Airport 2d | 3.359 | 2800 | 24.1 | 300 | 90 | F | Negative |
| Airport 3d | 3.413 | 270 | 24.7 | 180 | 100 | F | Positive |
| Airport 4d | 2.972 | 270 | 22.9 | 60 | 100 | F | Positive |
| Airport 5d | 3.491 | 1500 | 25.9 | 250 | 95 | F | Positive |
| Subway station 1 | 3.496 | 5600 | 29.8 | 390 | 95 | N & F | Negative |
| Subway station 2 | 3.451 | 2100 | 31.8 | 370 | 95 | N & F | Positive |
| Subway station 3 | 3.545 | 5000 | 28.3 | 450 | 97 | N & F | Negative |
| Subway station 4 | 3.495 | 1125 | 31.5 | 300 | 90 | N & F | Positive |
| Subway train | 0.24 | 125 | 27.6 | 80 | 95 | N & F | Positive |
| Subway train | 2.353 | 125 | 25 | 80 | 95 | N & F | Positive |
| Bus 1 | 0.2 | 88 | 31.3 | 30 | 90 | N & F | Negative |
| Bus 2 | 0.2 | 88 | 29.9 | 70 | 80 | N | Positive |
| Bus 3 | 0.2 | 88 | 31.8 | 80 | 100 | N & F | Positive |
| Bus 4 | 0.2 | 88 | 32.3 | 50 | 85 | N & F | Negative |
Ventilation type: N: natural, F: forced, N & F: combination of natural and forced ventilation.
Shopping center 1: Tehran's bazaar, Shopping center 2: Tehran's bazaar, Shopping center 3: Tehran's bazaar, Shopping center 4: Tehran's bazaar, Shopping center 5: Alaedin mall.
Inside a governmental office including office 1: clients section, office 2: entrance, office 3: inside office 1, office 4: inside office 2.
Airport 1: inspection gate, airport 2: transit lounge, airport 3: inspection gate, airport 4: inspection gate, airport 5: waiting lounge.
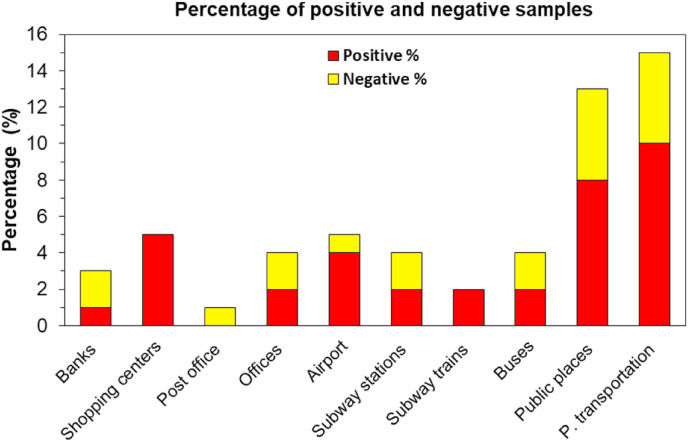
Fig. 1 presents the percentages of positive and negative samples for each of the eight groups of public and transport locations. In total, 62% and 67% of the samples collected from the public places and transportation were positive, respectively. Positive samples were detected in banks (33%), shopping centers (100%), the governmental office building (50%), the airport (80%), subway stations (50%), subway trains (100%), and buses (50%). Due to the permission limitations, only one post office was sampled, and the sample was negative. It is possible that if there were more samples in more buildings, SARS-CoV-2 could also have been detected in post offices. In case of the airport, all the samples at the inspection gates (n = 3) and the sample from the waiting lounge (n = 1) were positive; while the transit lounge's sample was negative. In the government building, SARS-CoV-2 was found in the two samples collected from the first floor (client section and inside gate), where there were higher numbers of people (80 and 250 people) than inside the office rooms (20–25 people) that had negative samples.
Fig. 1.
Percentage of positive and negative samples based on the group of sampling sites.
Only one other study has been reported that explored the presence of SARS-CoV-2 in non-medical environments. Setti et al. (2020) explored the presence of SARS-CoV-2 in particulate matter in an industrial area in Italy and found that 94% of the samples were positive. Liu et al. (2020) found SARS-CoV-2 in PM samples in department stores located in a hospital, but not in other public areas such as a supermarket, residential building, etc. (Liu et al., 2020). In another study in a hospital in London, the virus were found in an entrance, toilet, and lift area (Zhou et al., 2020). Despite these studies, some other studies have not identified SARS-CoV-2 RNA in public places and clean areas in hospitals (Razzini et al., 2020b; Wu, 2020). Even in clinical settings, some studies have not found the presence of airborne virus (Cheng et al., 2020; Faridi et al., 2020; Guo et al., 2020). This inconsistency could be due to the various parameters (Rahmani et al., 2020), which have been partly investigated in our study. Due to experimental limitations common to this type of study, only the presence of SARS-CoV-2 viral RNA was investigated, which may not represent the presences of viable virus. Detecting viable viruses needs culture methods. It was expected that concentration of viral RNA would be lower than that of its viable forms (Lednicky et al., 2020a,b). Therefore, these results should be interpreted with caution.
The effects of the number of people present during sampling, the percentage of people wearing masks, air temperature, sampled volume, and sampling site volume on the presence of SARS-CoV-2 in air are presented in Table 3 . The number of people during the sampling and sampled volume were positively associated with presence of SARS-CoV-2; while the percentage of people with masks, air temperature, and sampling site volume were negatively related to SARS-CoV-2 presence. However, none of the associations were statistically significant. Our results are similar to the current knowledge about COVID-19. Liu et al. (2020) reported that the presence of SARS-CoV-2 in public places could be related to the number of people. Thus, more people leads to higher concentrations of this virus. Face masks can reduce the transmissibility of the virus by reducing transmission of respiratory droplets in both laboratory and clinical contexts (Howard et al., 2020). Several factors such as using face masks, coughing, and sneezing during the sampling, air movement and conditioning, sampler type, sampling conditions, storage and transferring conditions can influence the results of an environmental surveillance of SARS-CoV-2 (Rahmani et al., 2020). In our study, some of the samples (in buses and a subway train) were collected using a low flow pump with total sample volumes of 200–240 L. However, the results of three out of these five samples were positive, indicating that a likely higher concentration of SARS-CoV-2 in these places. Previous studies have stated that survival of SARS-CoV-2 decreases with temperature reduction in various environments (Chan et al., 2020; Yao et al., 2020) and may explain the negative association with temperature. However, the relationship between air temperature and SARS-CoV-2 is currently not well-known. More experimental studies on this issue are needed including the interactions among multiple factors such as relative humidity, ventilation systems, ultraviolet radiation, susceptibility of virus, etc. (ECDC, 2020; Riddell et al., 2020).
Table 3.
Results of the logistic regression models for the effects of different parameters on the presence of SARS-CoV-2 in air.
| Independent variables | Odds ratio (95% CI) | p-value |
|---|---|---|
| Number of people | 1.00 (0.99, 1.01) | 0.23 |
| People with mask (%) | 0.99 (0.96, 1.02) | 0.61 |
| Temperature | 0.93 (0.72, 1.17) | 0.54 |
| Sampling site's volume | 0.99 (0.99, 0.99) | 0.08 |
| Sampled volume | 1.20 (0.61, 2.41) | 0.59 |
In the set of indoor locations, there were also offices with low traffic and they had little or no viral RNA. Thus, viral RNA associated with ambient particulate pollution was not likely to be spread to a significant extent within the office building or the airport lounges. Thus, although it is likely that airborne transmission of COVID-19 occurs in buildings with HVAC systems with low quality filters like commonly used MERV-8, the more important source is the direct aerosolization of material expelled by infected individuals. Thus, higher occupancy likely produced higher levels of viral RNA contamination. In transport facilities like buses and subway trains, ventilation rates are relatively high with doors frequently opening and people entering and leaving. Thus, again it is likely that direct exhalation of viral bearing droplets are the likely source of the observed viral RNA and the relationship between occupancy and viral RNA concentrations could be anticipated. It would be in locations without significant populations and still finding viral RNA that aerosol transmission would become a major source of infection such as what likely happened on the Diamond Princess when docked in Yokohama. (Nakazawa et al., 2020).
4. Conclusions
In this study, airborne particle samples were collected from eight types of public places and transport vehicles in Tehran (Iran), and analyzed for the SARS-CoV-2. A majority of samples from these groups were identified to be positive for the presence of the virus. Positive association of SARS-CoV-2 with number of people during the sampling and sampled volume were found while negative associations were found with percentage of people with masks, air temperature, and sampling site volume. Although the number of samples per types of environment was small and thus statistically less significant, it did show that the majority of the sampled public places and public transport vehicles were contaminated with SARS-CoV-2. Thus, these contaminated spaces pose a significant risk to public health. Given the end of lockdown periods in many countries, more attention should be paid to control the spread of COVID-19 in public places and gatherings. Based on the present work, strategies need to continue to limit the number of people in public indoor spaces and require people to wear masks.
Funding sources
This study was funded by Shahid Beheshti University of Medical Sciences, Tehran, Iran (grant number #23256).
CRediT authorship contribution statement
Mostafa Hadei: Conceptualization, Methodology, Writing - review & editing, Formal analysis. Seyed Reza Mohebbi: Methodology, Writing - review & editing, Validation, Formal analysis. Philip K. Hopke: Conceptualization, Methodology, Writing - review & editing. Abbas Shahsavani: Conceptualization, Methodology, Writing - review & editing, Supervision, Resources. Shahriyar Bazzazpour: Investigation, Methodology, Writing - review & editing. Mohammadreza Alipour: Investigation, Methodology, Writing - review & editing. Ahmad Jonidi Jafari: Conceptualization, Methodology, Writing - review & editing. Anooshiravan Mohseni Bandpey: Resources, Writing - review & editing, Conceptualization. Alireza Zali: Conceptualization, Resources, Writing - review & editing. Maryam Yarahmadi: Investigation, Methodology, Writing - review & editing. Mohsen Farhadi: Resources, Writing - review & editing. Masoumeh Rahmatinia: Resources, Investigation, Writing - review & editing. Vajihe Hasanzadeh: Investigation, Resources, Writing - review & editing. Seyed Saeed Hashemi Nazari: Methodology, Writing - review & editing, Formal analysis. Hamid Asadzadeh-Aghdaei: Methodology, Resources, Writing - review & editing. Mohammad Tanhaei: Methodology, Writing - review & editing, Validation. Mohammad Reza Zali: Methodology, Writing - review & editing, Validation. Majid Kermani: Methodology, Writing - review & editing. Mohmmad Hossien Vaziri: Methodology, Resources, Writing - review & editing. Hamid Chobineh: Methodology, Resources, Writing - review & editing, Formal analysis.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors wish to thank Shahid Beheshti University of Medical Sciences for their support of this study.
Footnotes
Peer review under responsibility of Turkish National Committee for Air Pollution Research and Control.
References
- Baghani A.N. A case study of BTEX characteristics and health effects by major point sources of pollution during winter in Iran. Environ. Pollut. 2019;247:607–617. doi: 10.1016/j.envpol.2019.01.070. [DOI] [PubMed] [Google Scholar]
- Chan K.H. Factors affecting stability and infectivity of SARS-CoV-2. J. Hosp. Infect. 2020;106:226–231. doi: 10.1016/j.jhin.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C. Infection Control and Hospital Epidemiology. 2020. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia P.Y. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020;11:1–7. doi: 10.1038/s41467-020-16670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling B.J. Aerosol transmission is an important mode of influenza A virus spread. Nat. Commun. 2013;4:1935. doi: 10.1038/ncomms2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC . European Centre for Disease Prevention and Control; 2020. Heating, Ventilation and Air-Conditioning Systems in the Context of COVID-19: First Update. [Google Scholar]
- Faridi S. Science of the Total Environment; 2020. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran; p. 138401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z.-D. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020;26:10–3201. doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadei M. Indoor and outdoor concentrations of BTEX and formaldehyde in Tehran, Iran: effects of building characteristics and health risk assessment. Environ. Sci. Pollut. Control Ser. 2018;25:27423–27437. doi: 10.1007/s11356-018-2794-4. [DOI] [PubMed] [Google Scholar]
- Hadei M. A letter about the airborne transmission of SARS-CoV-2 based on the current evidence. Aerosol and Air Quality Research. 2020;20:911–914. [Google Scholar]
- Han Z. Characterizations of particle size distribution of the droplets exhaled by sneeze. J. R. Soc. Interface. 2013;10:20130560. doi: 10.1098/rsif.2013.0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard J. 2020. Face Masks against COVID-19: an Evidence Review. [Google Scholar]
- Johnson G. Modality of human expired aerosol size distributions. J. Aerosol Sci. 2011;42:839–851. [Google Scholar]
- Lednicky J.A. Vol. 20. Aerosol and Air Quality Research; 2020. Collection of SARS-CoV-2 virus from the air of a clinic within a university student health care center and analyses of the viral genomic sequence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lednicky J.A. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. Int. J. Infect. Dis. 2020;100:476–482. doi: 10.1016/j.ijid.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Nakazawa E. Disaster Medicine and Public Health Preparedness. 2020. Chronology of COVID-19 cases on the Diamond princess cruise ship and ethical considerations: a report from Japan; pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health England . In: COVID-19: Infection Prevention and Control Guidance. England P.H., editor. 2020. England. [Google Scholar]
- Rahmani A.R. Science of the Total Environment; 2020. Sampling and detection of corona viruses in air: a mini review; p. 740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razzini K. Science of The Total Environment; 2020. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy; p. 140540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razzini K. Science of the Total Environment; 2020. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy; p. 742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riddell S. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol. J. 2020;17:145. doi: 10.1186/s12985-020-01418-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarpia J.L. University of Nebraska Medical Center; MedRxIV: 2020. Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the. [Google Scholar]
- Setti L. SARS-Cov-2RNA found on particulate matter of Bergamo in northern Italy: first evidence. Environ. Res. 2020;188:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S. Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease 2019. Am. J. Infect. Contr. 2020;48(8):910–914. doi: 10.1016/j.ajic.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao M. Vol. 731. Science of The Total Environment; 2020. On airborne transmission and control of SARS-Cov-2; p. 139178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J. medRxiv; 2020. Investigating SARS-CoV-2 Surface and Air Contamination in an Acute Healthcare Setting during the Peak of the COVID-19 Pandemic in London. [Google Scholar]
- Zuo Z., de Abin M., Chander Y., Kuehn T., Goyal S. Comparison of spike and aerosol challenge tests for the recovery of viable influenza virus from non-woven fabrics. Influenza other respir. Viruses. 2013;7(5):637–644. doi: 10.1111/irv.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]