Abstract
This commentary will summarize the evidence on face masks for COVID-19 from both the infectious diseases and physical science viewpoints; standardize recommendations on types of masks that afford the best protection to the public; and provide guidelines on messaging for this important non-pharmaceutical intervention as we await widespread vaccine distribution.
This commentary will summarize the evidence on face masks for COVID-19 from both the infectious diseases and physical science viewpoints; standardize recommendations on types of masks that afford the best protection to the public; and provide guidelines on messaging for this important non-pharmaceutical intervention as we await widespread vaccine distribution.
Main Text
Epidemiologic Evidence for the Importance of Masking during COVID-19
The Centers for Disease Control and Prevention (CDC) advised the U.S. population to wear cloth face coverings in public on April 3, 2020, initially citing the reasoning that masks would protect others during the COVID-19 pandemic. However, mask wearing prevalence in the U.S. has been variable across regions of the country, compared to 95% adherence in countries where cultural norms or mandates facilitated the practice.1 In the U.S., there has not yet been a federal mask mandate, although individual counties and states have successively (but not uniformly) instituted individual mandates.
Epidemiologic and observational evidence for the importance of mask wearing in reducing COVID-19 transmission has been accumulating, much of which was recently summarized in a scientific brief by the CDC, including a case control study from Thailand and data from Beijing households and commercial airplanes.2 Table 1 outlines the seminal studies. For instance, impressive reductions in COVID-19 transmission were seen during the summer 2020 surge with institution of a state-wide mask mandate, among other interventions, in Arizona.3 Similarly, when Kansas counties imposed mask mandates unevenly during the summer surge, COVID-19 incidence decreased in the counties with mask mandates, but continued to increase in those without.4 A recent paper showed a 47% reduction in new COVID-19 transmissions (estimate between 15% and 75%) over a period of 20 days after the institution of regional mask mandates in Germany.5
Table 1.
Epidemiologic and Observational Studies Showing the Effectiveness of Masks in Reducing COVID-19 Transmission
| Setting | Exposure of interest | Effect |
|---|---|---|
| USS Theodore Roosevelt aircraft carrier | face coverings during an outbreak | service members who wore face coverings had lower infection rate than those who did not (55.8% versus 80.8%) |
| Hair salons in Missouri | two masked hair stylists infected with COVID-19 exposed 139 clients, all masked | none of the 139 clients developed symptoms with 67 testing negative for SARS-CoV-2 |
| Boston health care settings | institution of universal surgical masking with provision in hospitals | significantly lower rate of SARS-CoV-2 positivity among health care workers after masking |
| Arizona during summer surge | mask mandates, limiting large crowds, social distancing | transmission rates were up by 151% prior to these measures and then stabilized and decreased by 75% with continued application |
| Kansas counties during summer surge | state mask mandate with option for counties to opt-out in Kansas | COVID-19 incidence decreased in 24 counties with mask mandates after July 3, but continued to increase in 81 counties without mask mandates4 |
| Tennessee counties | mask requirements | areas with mask requirements had a slower growth rate in hospitalizations for COVID-19 (without controlling for cases) than those without mask requirements6 |
| States in the U.S. | mask mandates in 15 states and Washington, DC over summer | reduction in COVID-19 transmission rates in states mandating face mask use in public compared to those without mandates |
| Germany | regional mandates for mandatory mask wearing in public transport and shops | face masks reduced the number of new COVID-19 infections 45% (between 15% and 75%) over a period of 20 days after the mandates5 |
∗Unless indicated, all references are found in the CDC Scientific Brief2
In contrast, a recent study in Denmark randomized individuals to an arm where surgical masks were recommended and provided versus a standard-of-care arm and demonstrated only a modest benefit in limiting COVID-19 transmission.7 However, several design limitations of the trial—including low incidence at the time of the trial, inadequate sample size, randomization at the level of the individual instead of a community, and issues with adherence to mask-wearing and outcome ascertainment—likely hindered its ability to more substantially show the benefits of mask-wearing for COVID-19,8 making the epidemiologic and implementation evidence more compelling.
Beyond the impact on COVID-19 transmission rates, our group9 and others have hypothesized that facial masking could reduce the size of the viral inoculum to which people are exposed and, if they become infected, decrease the severity of the resultant COVID-19 disease. The association between inoculum size and disease severity has been seen in a Syrian hamster model with SARS-CoV-2, and surgical mask partitions were shown to reduce infections and disease severity in another hamster model. By reducing inhalation of viral particles by the mask wearer, masks can protect the individual from COVID-19 acquisition2 or, if acquired, possibly lead to a milder or asymptomatic infection.
Laboratory Evidence on How Surgical and Cloth Masks Protect the Wearer and Others from COVID-19
Initial guidance from the CDC on the use of cloth face coverings was focused on the protection this would afford to others (an approach termed source control). In a scientific brief published November 9, 2020, the CDC reiterated the benefit of face coverings to protect others, while emphasizing that masks also protect the wearer (filtration for personal protection).2
Masks work by blocking or filtering out viruses that are carried in aerosols. Filtering is not sieving out things that are too large to pass through holes in the material. Rather, air must curve as it flows around individual, tightly packed fibers of the material, like a race car swerving around cones of an obstacle course. As the air curves, the aerosols it carries cannot make the sharp bends and therefore slam into the fibers, or they come too close to the fibers and stick to them. Very small aerosols acquire random motion from air molecules bouncing off them and end up crashing into the fibers. This process works in both directions as air flows through a mask. With those principles in mind, we will now discuss evidence from the physical sciences about how masks block both transmission and acquisition of SARS-CoV-2 in order to reinforce this message that masks protect you and others. We also provide recommendations on specific face coverings that maximize protection.
Laboratory studies have demonstrated the ability of surgical masks to block SARS-COV-2 and other viruses. Viruses are carried in respiratory droplets and aerosols that, even when fully dried, contain far more salts and proteins than virus, so the size of concern is much larger than that of a naked virus. Surgical masks are made of melt-blown, non-woven polypropylene, similar to N95 masks. Researchers tested surgical masks on two manikins that were facing each other. SARS-CoV-2 virions were nebulized out the mouth of one manikin and were sampled through the mouth of the opposite manikin. The masks were 60%–70% effective at protecting others and 50% effective at protecting the wearer.10 The mechanism by which masks block viruses depends purely on the physical characteristics of the carrier droplet or aerosol and not the virus itself, so evidence for other viruses can be extended to SARS-COV-2 with careful consideration of the size of the droplets and aerosols involved. For instance, in a study of patients with documented infections with either seasonal coronaviruses or influenza virus, surgical masks blocked coronaviruses released into the air to undetectable levels and partially blocked influenza virus.11 Testing of eight different surgical masks on a manikin exposed to influenza virus in droplets and aerosols found that they protected the wearer by an average of 80%.12 The protective ability of cloth masks is more variable. Studies of dozens of materials have found material filtration efficiencies of <10% for polyurethane foam to nearly 100% for a vacuum cleaner bag.13 , 14 According to fit tests on humans, homemade masks are 50%–60% efficient at protecting the wearer against air pollution particles.15
Our group recently tested ten different types of face coverings for their effectiveness at protecting others as well as the wearer.14 Masks in our study protected the wearer more than others but this difference was not statistically significant. Based on our and others’ results, we recommend a high-quality surgical mask or a fabric mask of at least two layers with high thread count for basic protection (Figure 1 , top panel) for the public. For maximal protection (Figure 1, bottom panel), members of the public can either (1) wear a cloth mask tightly on top of a surgical mask where the surgical mask acts as a filter and the cloth mask provides an additional layer of filtration while improving the fit; or (2) wear a three-layer mask with outer layers consisting of a flexible, tightly woven fabric that can conform well to the face and a middle layer consisting of a non-woven high-efficiency filter material (e.g., vacuum bag material). If the masks fit well, these combinations should produce an overall efficiency of >90% for particles 1 μm and larger, which corresponds to the size of respiratory aerosols that we think are most important in mediating transmission of COVID-19.14
Figure 1.
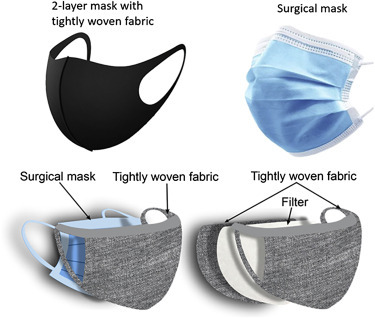
Recommended Masks for Public
Top: basic; bottom: maximal protection.
Ways to Effectively Provide Public Health Messaging on the Importance of Facial Masks during COVID-19
Finally, we recommend a variety of techniques to more effectively communicate the importance of facial masking in the U.S. to control COVID-19. Modeling of public health guidelines—such as facial masking—by leaders can encourage the populace to adopt this recommendation. Under new Presidential leadership as of January 2021, we suspect that mask modeling will gain in prominence as we enter the second year of the pandemic. For instance, President-Elect Biden has urged Americans to wear masks for the first 100 days of his administration as we await widespread vaccine distribution. Mask provision in essential workplaces can encourage mask adherence. Mask mandates, with enforcement strategies as needed, can be highly effective in expanding mask wearing prevalence.1
Finally, we recommend a harm reduction-based, non-stigmatizing approach to our public health messaging on face masking. Harm reduction—when applied to disease prevention for infectious diseases—is the principle of advising individuals how to mitigate risk while acknowledging the real-world conditions that may lead individuals to take some risks. Mask-shaming or calling individuals selfish for not wearing a mask is the most ineffective way to achieve trust in public health officials and should not be part of our messaging. We are recommending a new non-pharmacological intervention (NPI) for the American public that was not previously a part of our cultural norms. This NPI will be necessary to adhere to for some time as we achieve equitable and widespread distribution of a safe and effective vaccine.
Although the recent news that the Moderna and Pfizer/BioNTech mRNA vaccines are more than 94% efficacious in protecting against symptomatic COVID-19 is very encouraging, asymptomatic infection could not be ruled out in either trial among vaccine recipients. Moreover, the duration of vaccine protection is not yet known and widespread vaccination to reach an appropriate level of population-level immunity (60%–70%) will take some time. Therefore, mask wearing will need to continue until the cessation of this pandemic and may be required if there is another. We recommend messaging on the importance of facial masks with kindness, evidence, and empathy and a nationwide mask mandate1 to encourage adherence and get through this pandemic together.
Acknowledgments
Funding for this work was provided by the National Institute of Allergy and Infectious Diseases/National Institutes of Health (NIAID/NIH) R01AI158013 (PI: Gandhi) and the National Science Foundation (NSF) CBET-1438103 and ECCS-1542100 (PI: Marr). Artwork by Jasper Marr Hester.
Declaration of Interests
The authors declare no competing interests.
References
- 1.Leffler C.T., Ing E., Lykins J.D., Hogan M.C., McKeown C.A., Grzybowski A. Association of Country-wide Coronavirus Mortality with Demographics, Testing, Lockdowns, and Public Wearing of Masks. Am. J. Trop. Med. Hyg. 2020;103:2400–2411. doi: 10.4269/ajtmh.20-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) 2020. Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2. Accessed November 10, 2020.https://www.cdc.gov/coronavirus/2019-ncov/more/masking-science-sars-cov2.html [Google Scholar]
- 3.Gallaway M.S., Rigler J., Robinson S., Herrick K., Livar E., Komatsu K.K., Brady S., Cunico J., Christ C.M. Trends in COVID-19 Incidence After Implementation of Mitigation Measures - Arizona, January 22-August 7, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1460–1463. doi: 10.15585/mmwr.mm6940e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Dyke M.E., Rogers T.M., Pevzner E., Satterwhite C.L., Shah H.B., Beckman W.J., Ahmed F., Hunt D.C., Rule J. Trends in County-Level COVID-19 Incidence in Counties With and Without a Mask Mandate - Kansas, June 1-August 23, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1777–1781. doi: 10.15585/mmwr.mm6947e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitze T., Kosfeld R., Rode J., Wälde K. Face masks considerably reduce COVID-19 cases in Germany. Proc. Natl. Acad. Sci. USA. 2020 doi: 10.1073/pnas.2015954117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lowary J. 2020. Study finds areas without mask requirements have larger increase in COVID-19 hospitalizations. Vanderbilt Center for Economic Health Modeling. October 27, 2020.https://news.vumc.org/2020/10/27/study-finds-areas-without-mask-requirements-have-larger-increase-in-covid-19-hospitalizations/ Accessed November 10, 2020. [Google Scholar]
- 7.Bundgaard H., Bundgaard J.S., Raaschou-Pedersen D.E.T., von Buchwald C., Todsen T., Norsk J.B., Pries-Heje M.M., Vissing C.R., Nielsen P.B., Winsløw U.C., et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers : A Randomized Controlled Trial. Ann. Intern. Med. 2020 doi: 10.7326/M20-6817. Published online November 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gandhi M. 2020. Perspective on DANMASK Study. November 18, 2020. Healio Infection Control online.https://www.healio.com/news/primary-care/20201118/study-covid19-risk-slightly-lower-for-mask-wearers [Google Scholar]
- 9.Gandhi M., Beyrer C., Goosby E. Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer. J. Gen. Intern. Med. 2020;35:3063–3066. doi: 10.1007/s11606-020-06067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ueki H., Furusawa Y., Iwatsuki-Horimoto K., Imai M., Kabata H., Nishimura H., Kawaoka Y. Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. MSphere. 2020;5:5. doi: 10.1128/mSphere.00637-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P., Yen H.L., Li Y., Ip D.K.M., Peiris J.S.M., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Makison Booth C., Clayton M., Crook B., Gawn J.M. Effectiveness of surgical masks against influenza bioaerosols. J. Hosp. Infect. 2013;84:22–26. doi: 10.1016/j.jhin.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Drewnick F., Pikmann J., Fachinger F., Moormann L., Sprang F., Bormann S. Aerosol filtration efficiency of household materials for homemade face masks: Influence of material properties, particle size, particle electrical charge, face velocity, and leaks. Aerosol Sci. Technol. 2020;55:63–79. [Google Scholar]
- 14.Pan J., Harb C., Leng W., Marr L.C. Inward and outward effectiveness of cloth masks, a surgical mask, and a face shield. medRxiv. 2020 doi: 10.1101/2020.11.18.20233353. [DOI] [Google Scholar]
- 15.van der Sande M., Teunis P., Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS ONE. 2008;3:e2618. doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]


