Highlights
-
•
We compared OHCA presentations in London during March and April 2019 and 2020
-
•
There was an 81% increase in OHCAs during the first peak of the COVID-19 pandemic
-
•
This increase was closely related to SARS-CoV-2 infection rates in London
-
•
We report an increase in the rate of bystander CPR in London during the pandemic
-
•
Outcomes following OHCA were significantly poorer during the COVID-19 pandemic
Keywords: Out of Hospital Cardiac Arrest, EMS, COVID-19, SARS-CoV-2, Coronavirus, London
Abstract
Aim
There is an emerging potential link between the COVID-19 pandemic and incidence and outcomes from out-of-hospital cardiac arrest (OHCA). We aimed to describe the incidence, characteristics and outcomes from OHCA in London, UK during the first wave of the pandemic.
Methods
We examined data for all OHCA patients attended by the London Ambulance Service from 1st March to 30th April 2020 and compared our findings to the previous year. We also compared OHCA characteristics and short-term outcomes for those suspected or confirmed to have COVID-19 with those who were not. Additionally, we investigated the relationship between daily COVID-19 cases and OHCA incidents.
Results
We observed an 81% increase in OHCAs during the pandemic, and a strong correlation between the daily number of COVID-19 cases and OHCA incidents (r = 0.828, p < 0.001). We report an increase in OHCA occurring in a private location (92.9% vs 85.5%, p < 0.001) and an increased bystander CPR (63.3% vs 52.6%, p < 0.001) during the pandemic, as well as fewer resuscitation attempts (36.4% vs 39.6%, p = 0.03) and longer EMS response times (9.3 vs 7.2 min, p < 0.001). Survival at 30 days post-arrest was poorer during the pandemic (4.4% vs 10.6%, p < 0.001) and amongst patients where COVID-19 was considered likely (1.0% vs 6.3%, p < 0.001).
Conclusions
During the first wave of the COVID-19 pandemic in London, we saw a dramatic rise in the incidence of OHCA, accompanied by a significant reduction in survival. The pattern of increased incidence and mortality closely reflected the rise in confirmed COVID-19 infections in the city.
Introduction
London was the first city in the UK to experience the novel coronavirus SARS-CoV-2 (COVID-19) infection at scale. The first case of COVID-19 was reported in London on 12th February 2020 and by 1st March, there was on average 7 new laboratory confirmed infections every day, a figure that rose rapidly during March. On 11th March 2020, the WHO classified the outbreak as a pandemic1 and, on 23rd March 2020, the UK went into full lockdown in an attempt to control the spread of the disease. COVID-19 infections in London peaked on 4th April when there was an average of 892 new cases per day in the city. During this time, there was also an increase in the number of patients admitted to hospital with a confirmed COVID-19 infection, and the number who died within 28 days of testing positive.2
Globally, there is an emerging potential link between the COVID-19 pandemic and incidence and outcomes from out of hospital cardiac arrest (OHCA). Whilst two recent studies found no differences,3, 4 data from the Lombardia Region of Northwest Italy,5, 6 Paris,7 New York City,8 and two counties in the Western States of the USA9 all reported increased incidence of OHCA along with local rises in COVID-19 infections, and poorer outcomes for patients sustaining OHCA during the pandemic. A significant increase in mortality was also observed in Victoria, Austrailia,10 although no difference in OHCA incidence was reported. Increased Emergency Medical Service (EMS) response times,5, 6, 7, 9, 10, 11, 12 fewer resuscitations,7, 10, 11, 12 fewer shockable rhythms6, 7, 8 and lower rates of bystander CPR5, 6, 7, 9, 12 are some of the characteristics of OHCA during the pandemic that are being reported. There is growing concern that these findings represent both direct and indirect impacts of the pandemic, with indirect influences potentially relating to healthcare system reorganisation, the reluctance of individuals to access healthcare, and an unwillingness of bystanders to render aid due to the fear of virus transmission.
To date, no studies have been published from the UK reporting OHCA during COVID-19. In this paper, we aim to describe the incidence, characteristics and outcomes from OHCA in London during the first wave of the COVID-19 pandemic in early 2020.
Methods
Study design
This retrospective, observational study reports all OHCA incidents from 1st March to 30th April 2020 (COVID-19 period) attended by the London Ambulance Service NHS Trust (LAS) and compares these data to the same period of the previous year (1st March to 30th April 2019; the pre-COVID-19 period). We used fully anonymised data routinely collected as part of an on-going clinical audit programme and ethical approval was not required.
Patient population
All OHCA patients who, during the study periods, received an EMS response from LAS (irrespective of whether a resuscitation attempt was made) were included in our analysis. Those who were successfully resuscitated prior to EMS arrival and so did not receive resuscitation from our clinicians were excluded.
Study setting
LAS is the primary provider of prehospital emergency care in Greater London, UK, serving an estimated population of 8.96 million.13 Over 3500 clinicians are employed by the LAS in frontline patient facing roles, attending more than 1.2 million face-to-face incidents per year, over 10,000 of which are cardiac arrest, with resuscitative efforts being provided to 39%. Emergency calls are triaged using the advanced Medical Priority Dispatch System (MPDS v.13.0 in 2019 and v.13.1 in 2020; IAED, Salt Lake City, Utah, USA). OHCAs receive the highest priority response with a minimum of two emergency vehicles dispatched carrying at least one advanced life support (ALS) trained paramedic. Initial rhythm analysis and defibrillation is undertaken in semi-automatic mode in line with local procedures; all other clinical training and practices are in accordance with 2015 Resuscitation Council (UK) guidelines.14 The LAS also has Advanced Paramedic Practitioners who receive additional prehospital critical care training and are targeted to the most critically ill and injured patients, including OHCA.
During the pandemic, the LAS followed infection prevention and control guidance published by Public Health England (PHE) requiring clinicians to don Level 2 personal protective equipment (PPE) for most patient contacts (disposable gloves and aprons, fluid resistant surgical mask and, where there was a splash risk, eye protection). Where COVID-19 was suspected, Level 3 PPE (disposable gloves, fluid repellent coverall or gown, FFP3 mask and eye protection) was required during resuscitation.15 From 18th March 2020, updated guidance from PHE, required EMS clinicians to don Level 3 PPE for any resuscitation regardless of COVID-19 suspicion. PPE was donned after arrival on-scene and before any patient contact.
The number of emergency calls received by LAS rose sharply during the pandemic, this, along with significant staff absences, led to call answering times (the time between the call for help being placed and the call being answered by the EMS) rising from 7 s in March 2019 to an average of 3 min 20 s in March 2020.
Data collection
Anonymised data were extracted from the LAS’s Out-of-Hospital Cardiac Arrest Registry that uses multiple sources to collate information about call triage and dispatch, EMS response times, demographic and patient details, clinical care and treatment, and short-term clinical outcomes (ROSC at any point, ROSC sustained to hospital, and survival to 30 days post-event). Data were collected in accordance with the Utstein methodology. Aetiology was based on the suspected cause, with ‘presumed cardiac’ assigned when there was no other obvious cause for the cardiac arrest. A clinical suspicion or a confirmed diagnosis of COVID-19 infection was also collected from attending EMS clinicians’ records.
To establish the number of laboratory confirmed SARS-CoV-2 infections in the local population, data on the number of positive PCR tests (by specimen date) were obtained from the UK Government’s coronavirus data portal2 (last accessed 15th September 2020). We used mid-2019 residential population estimates published by the Office for National Statistics13 to calculate incidence rates per 100,000 population.
Data analysis
Patients were grouped and analysed according to the period in which they had their cardiac arrest (pre-COVID-19 period: 1st March to 30th April 2019 vs. COVID-19 period: 1st March to 30th April 2020). Basic demographic data and response times are reported for all OHCAs attended, with more detailed characteristics provided for those who had resuscitation attempted.
Patients from the COVID-19 period were also grouped and compared according to whether there was clinical suspicion/confirmed diagnosis of SARS-CoV-2 infection (for simplicity this is called the ‘COVID-19’ group) or not (‘non-COVID-19’ group).
Data were summarised using descriptive statistics. Continuous data are presented as means and standard deviations (SD) or medians and inter-quartile ranges (IQR), as appropriate, and categorical data as counts with percentages. Statistical analyses were performed using Chi-Squared tests for categorical data and one-way analysis of variance for continuous data.
The 7-day moving average of OHCA incidents were plotted as a function of time along with the 7-day moving average of the number of positive SARS-CoV-2 PCR tests in Greater London for the COVID-19 period. To investigate correlations, we plotted the daily number of positive SARS-CoV-2 PCR tests in Greater London against the daily number of OHCA incidents attended. We used Pearson's product-moment correlation and linear regression to analyse the correlation between variables in our plots.
Data were analysed using Excel (Microsoft, Redmond, WA) and SPSS v26 (IBM, Armonk, NY).
Results
COVID-19 period vs pre-COVID period—all OHCAs
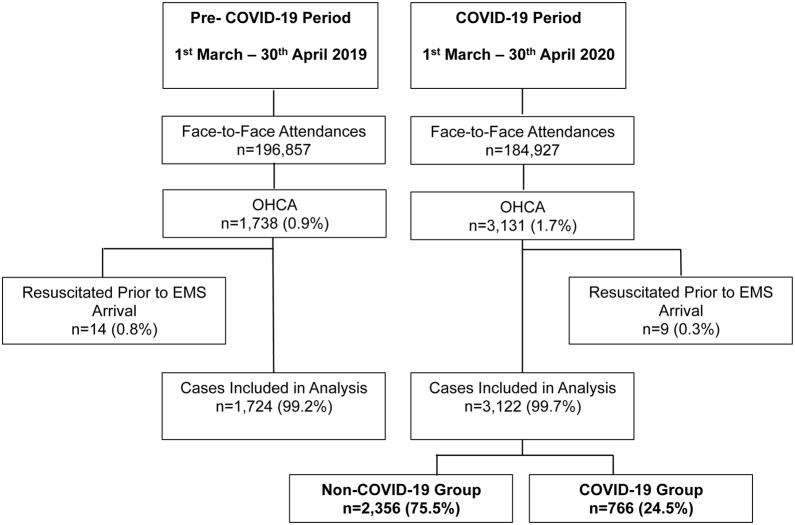
During the COVID-19 period, EMS clinicians attended 3122 patients in cardiac arrest, which compares with 1724 OHCAs during the same two-month period of the previous year. This represents an 81% absolute increase in OHCA incidents, rising from 19.2 to 34.8 OHCAs per 100,000 population of London. The total number of calls for EMS help increased by 14% (from 320,709 to 366,039), but face-to-face attendances decreased by 11,930 (6%), meaning that OHCA accounted for a larger proportion of call-outs during COVID-19 (increasing from 0.9% to 1.7%). Fig. 1 shows the total number of face-to-face incidents and OHCAs attended during both time periods.
Fig. 1.
Patients Included in the Study with Comparison Groups.
Patient characteristics differed between the two periods: OHCA patients were older (mean age 71 vs 68; p < 0.001), less likely to be of white ethnic origin (50.4% vs 60.6%; p < 0.001) and less likely to be male (59.0% vs 62.0%; p = 0.04) during the COVID-19 period. OHCAs were also significantly more likely to occur in a private location during the pandemic (92.9% vs 85.5%; p < 0.001) (Table 1).
Table 1.
Characteristics of all OHCA patients.
| Characteristics | Pre-COVID-19 Period (n = 1724) | COVID-19 Period (n = 3122) | p-value | Non-COVID-19 Group (n = 2356) | COVID-19 Group (n = 766) | p-value | Total (n = 4869) |
|---|---|---|---|---|---|---|---|
| Age (years), Mean ± SD | 68 ± 20 | 71 ± 19 | <0.001 | 71 ± 19 | 70 ± 18 | 0.03 | 70 ± 19 |
| Gendera (male), n (%) | 1069 (62.0) | 1839 (59.0) | 0.04 | 1371 (58.3) | 468 (61.2) | 0.12 | 2908 (60.1) |
| Ethnicity, n (%) | |||||||
| White | 1044 (60.6) | 1573 (50.4) | <0.001 | 1276 (54.2) | 297 (38.8) | <0.001 | 2617 (54.0) |
| Asian/British Asian | 86 (5.0) | 221 (7.1) | 135 (5.7) | 86 (11.2) | 307 (6.3) | ||
| Black/Black British | 111 (6.4) | 244 (7.8) | 166 (7.0) | 78 (10.2) | 355 (7.3) | ||
| Other | 58 (3.4) | 130 (4.2) | 77 (3.3) | 53 (6.9) | 188 (3.9) | ||
| Unknown | 425 (24.7) | 954 (30.6) | 702 (29.8) | 252 (32.9) | 1379 (28.5) | ||
| Location, n (%) | |||||||
| Private address | 1474 (85.5) | 2899 (92.9) | <0.001 | 2164 (91.9) | 735 (96.0) | <0.001 | 4373 (90.2) |
| Public | 249 (14.4) | 223 (7.1) | 192 (8.1) | 31 (4.0) | 472 (9.7) | ||
| Unknown | 1 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (<0.1) | ||
| Response times (min), Median (IQR) | |||||||
| EMS call to scene | 7.2 (5.4−9.8) | 9.3 (6.4−15.3) | <0.001 | 9.0 (6.3−14.3) | 10.0 (6.4−17.4) | <0.001 | 8.2 (5.9−12.9) |
| Time spent on sceneb | 52.3 (39.5−70.6) | 61.8 (47.7−81.0) | <0.001 | 61.1 (47.1−78.8) | 67.0 (49.0−90.0) | 0.03 | 57.1 (42.5−75.1) |
| EMS Call to hospital arrivalb | 74.4 (59.9−94.5) | 86.4 (68.7−109.1) | <0.001 | 84.6 (68.5−105.5) | 98.5 (70.3−148.3) | <0.001 | 80.6 (64.1−101.1) |
| EMS resuscitation attempt, n (%) | 683 (39.6) | 1135 (36.4) | 0.03 | 742 (31.5) | 393 (51.3) | <0.001 | 1818 (37.5) |
Percentages exclude cases where gender is unknown (n = 6).
Where the patient was conveyed to hospital.
In addition, fewer resuscitations were attempted during the COVID-19 period (36.4% vs 39.6%; p = 0.03), decreasing from 12.7 to 7.6 per 100,000 population. The response intervals from 999 call to EMS arrival on-scene, total time spent on-scene, and the time from 999 call to arrival at hospital were all longer during COVID-19 (9.3 vs 7.2 min, p < 0.001; 61.8 vs 52.3 min, p < 0.001; and 86.4 vs 74.4 min, p < 0.001 respectively) (Table 1).
COVID-19 vs pre-COVID period—resuscitation attempted cases
The proportion of public access defibrillator (PAD) deployments more than halved during the COVID-19 period (4.1% vs 8.9%, p < 0.001), and significantly more patients received bystander CPR (63.3% vs 52.6%, p < 0.001). Fewer patients who had EMS resuscitative efforts undertaken presented with a presumed cardiac aetiology (66.7% vs 76.4%, p < 0.001) and more presented in asystole (56.5% vs 31.6%, p < 0.001). There were no differences in whether or not EMS defibrillation was provided, nor the number of shocks delivered, but patients treated during the COVID-19 period were significantly more likely to be administered adrenaline (87.6% vs 82.3%, p = 0.002) (Table 2)
Table 2.
Characteristics and outcomes of patients with OHCA where resuscitation was attempted.
| Characteristics | Pre-COVID-19 Period (n = 683) | COVID-19 Period (n = 1135) | p-value | Non-COVID-19 Group (n = 742) | COVID-19 Group (n = 393) | p-value | Total (n = 1818) |
|---|---|---|---|---|---|---|---|
| Witnessed arrest, n (%) | |||||||
| Bystander | 339 (49.6) | 606 (53.4) | 0.27 | 390 (52.6) | 216 (55.0) | 0.20 | 945 (52.0) |
| EMS clinician | 104 (15.2) | 168 (14.8) | 120 (16.2) | 48 (12.2) | 272 (15.0) | ||
| Not witnessed | 240 (35.1) | 361 (31.8) | 232 (31.3) | 129 (32.8) | 601 (33.1) | ||
| Bystander CPR, n (%) | 359 (52.6) | 718 (63.3) | <0.001 | 461 (62.1) | 257 (65.4) | 0.28 | 1077 (59.2) |
| Aetiology, n (%) | |||||||
| Presumed cardiac | 522 (76.4) | 757 (66.7) | <0.001 | 540 (72.8) | 217 (55.2) | <0.001 | 1279 (70.4) |
| Other medical | 124 (18.2) | 350 (30.8) | 174 (23.5) | 176 (44.8) | 474 (26.1) | ||
| Trauma | 37 (5.4) | 28 (2.5) | 28 (3.8) | 0 (0.0) | 65 (3.6) | ||
| Initial rhythma, n (%) | |||||||
| Asystole | 321 (31.6) | 638 (56.5) | <0.001 | 371 (50.1) | 267 (68.5) | <0.001 | 959 (53.1) |
| VF/VT | 142 (21.0) | 168 (14.9) | 144 (19.5) | 24 (6.2) | 310 (17.2) | ||
| PEA | 214 (31.6) | 324 (28.7) | 225 (30.4) | 99 (25.4) | 538 (29.8) | ||
| Unknown, n (%) | 6 (0.9) | 5 (0.4) | 2 (0.3) | 3 (0.8) | 11 (0.6) | ||
| PAD deployed, n (%) | 61 (8.9) | 47 (4.1) | <0.001 | 39 (5.3) | 8 (2.0) | 0.01 | 108 (5.9) |
| EMS defibrillation, n (%) | 244 (35.7) | 372 (32.8) | 0.20 | 288 (38.8) | 84 (21.4) | <0.001 | 616 (33.9) |
| Number of shocks, Median (IQR)b | 2 (1−5) | 2 (1−5) | 0.77 | 2 (1−5) | 1 (1−3) | 0.001 | 2 (1−5) |
| Adrenaline administered, n (%) | 562 (82.3) | 994 (87.6) | 0.002 | 628 (84.6) | 366 (93.1) | <0.001 | 1556 (85.6) |
| Total dose of adrenaline (mg), Median (IQR)c | 6 (3−8) | 5 (4−7) | 0.16 | 5 (4−7) | 5 (4−7) | 0.71 | 5 (4−7) |
| ROSC achieved, n (%) | 332 (48.6) | 429 (37.8) | <0.001 | 314 (42.3) | 115 (29.3) | <0.001 | 761 (41.9) |
| ROSC sustained to hospital, n (%) | 224 (32.8) | 213 (18.8) | <0.001 | 179 (24.1) | 34 (8.7) | <0.001 | 437 (24.0) |
| Resuscitation terminated on scene, n (%) | 318 (46.6) | 798 (70.3) | <0.001 | 467 (62.9) | 331 (84.2) | <0.001 | 1116 (61.4) |
| Alive at 30 Daysd, n (%) | 70 (10.6) | 49 (4.4) | <0.001 | 45 (6.3) | 4 (1.0) | <0.001 | 119 (6.7) |
| Unknown, n (%) | 25 (3.7) | 27 (2.4) | 25 (3.4) | 2 (0.5) | 52 (2.9) |
Percentages exclude cases with an unknown initial rhythm.
Excludes patients who were not defibrillated by EMS clinicians.
Excludes patients who were not administered intra-arrest adrenaline.
Percentages exclude cases with unknown outcome at 30 day.
Short-term outcomes were poorer during the pandemic, with more resuscitation efforts terminated on-scene (70.3% vs 46.6%, p < 0.001), fewer patients achieving ROSC at any point (37.8% vs 48.6%, p < 0.001), sustaining ROSC to hospital (18.8% vs 32.8%, p < 0.001) or surviving to 30 days post-event (4.4% vs 10.6%, p < 0.001) (Table 2).
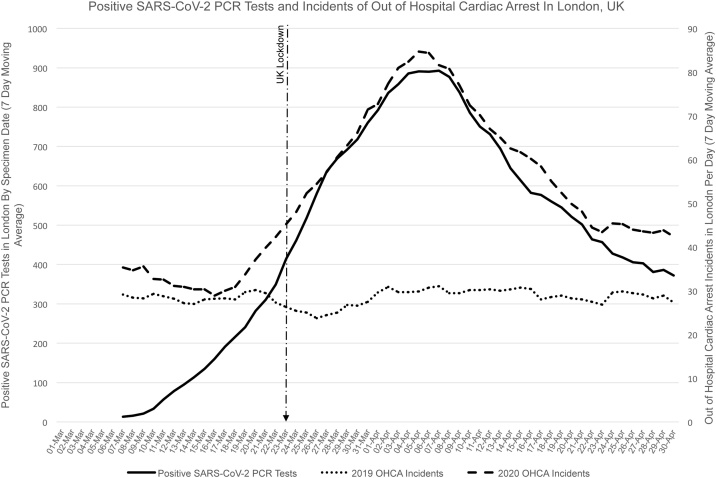
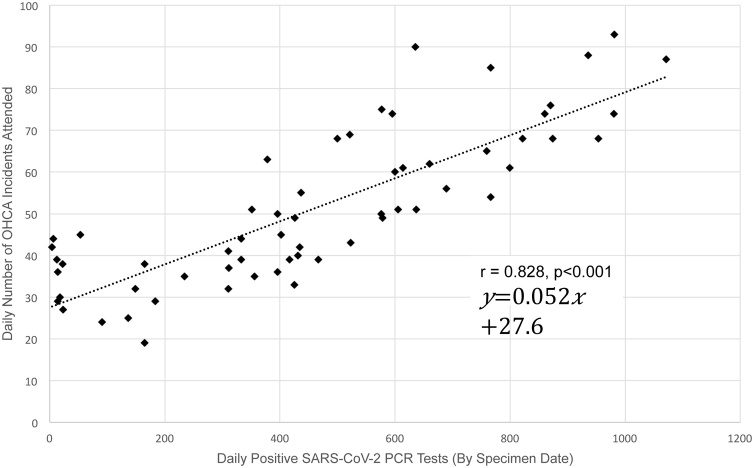
Associations between SARS-CoV-2 PCR tests and cardiac arrest incidence
The increasing incidence of OHCA in London clearly corresponded with the number of positive SARS-CoV-2 PCR tests, with the peak of both occurring during early April (Fig. 2). We observed a strong and statistically significant correlation between the daily number of positive SARS-CoV-2 PCR tests in London and OHCA incidents attended by LAS (Fig. 3, r = 0.828, p < 0.001). Linear regression analysis showed a daily increase of 100 positive SARS-CoV-2 PCR tests to be associated with an average daily increase of 5 OHCA incidents (95% CI: 4.3–6.1, p < 0.001).
Fig. 2.
Daily Number of Positive SARS-CoV-2 PCR Tests and OHCA Incidents in London during March and April 2019 and 2020 (7 Day Moving Average).
Fig. 3.
Correlation between Daily Positive SARS-CoV-2 PCR Tests and OHCA Incidents in London in March and April 2020.
Resuscitation and outcomes of confirmed or suspected COVID-19 cases
766 (24.5%) OHCA patients had either a confirmed diagnosis of SARS-CoV-2 infection (n = 66) or displayed clinical signs (n = 700) consistent with COVID-19 (together defined as the COVID-19 group).
As reported in Table 1, patients in the COVID-19 group were significantly less likely to be white, and more often from a black and ethnic minority background, more often arrested in private, had longer responses times, and resuscitation was more likely. For the subgroup who had resuscitation attempted (Table 2), in the COVID-19 group there were fewer arrests of a presumed cardiac aetiology, and more of a medical cause, (55.2% vs 72.8% and 44.8% vs 23.5%; p < 0.001), PAD deployment was lower (2.0% vs 5.3%, p = 0.01), bystander CPR was higher (65.4% vs 62.1%, p = 0.28), and patients were more likely to present in asystole (68.5% vs 50.1%, p < 0.001), less likely to require defibrillation (21.4% vs 38.8%; p < 0.001), and received fewer shocks (1 vs 2 shocks; p = 0.001). This group of patients were also more often administered adrenaline (93.1% vs 84.6%, p < 0.001), although the total number of doses given did not differ between the two groups.
Outcomes were poorer amongst the suspected COVID-19 group, with fewer achieving ROSC at any point (29.3% vs 42.3%, p < 0.001) or sustaining ROSC to hospital (8.7% vs 24.1%, p < 0.001) and resuscitation efforts were more likely to be terminated on-scene (84.2% vs 62.9%, p < 0.001).
Discussion
We observed an absolute increase of 81% in OHCA incidence, representing an additional 15 cardiac arrests per 100,000 population, during the first two months of the COVID-19 pandemic in London. We also found a clear correlation between the rise in incidents and progression of the pandemic, with an average daily increase of 5 cardiac arrests for every 100 confirmed infections. Similar patterns of increased OHCA incidence during COVID-19 have been reported from the USA, Paris, and Lombardia.5, 6, 7, 8, 9 Taken together with the observation that a quarter of our OHCA patients either had, or were clinically suspected to have, COVID-19 our findings strongly support a link between COVID-19 and the occurrence of OHCA. Whether such a link is the direct result of the pathophysiology of the disease, or more widely related to indirect factors, such as a reluctance to access medical assistance for conditions pre-empting cardiac arrest, changes to healthcare provision and infrastructure, or even the societal restrictions that accompanied the pandemic, remains to be ascertained.16
Alongside the pandemic-related rise in incidence, we found a decrease in favourable outcomes from OHCA, with more resuscitations terminated on-scene, reduced ROSC rates, and fewer patients surviving. While the current literature provides a mixed picture regarding resuscitation rates and ROSC, five of the six studies published to date that have measured survival to hospital discharge, have reported decreases during COVID-19.6, 7, 9, 10,12
To protect the public and EMS responders during the pandemic, some changes to cardiac arrest management were made. With a decreased likelihood of OHCA occurring in public due to the lockdown, and the need to assume that all patients were potentially COVID-19 positive, the dispatch of Community First Responders was suspended and, on the 23rd March, GoodSam (a mobile phone alerting system that activates volunteers trained in CPR and defibrillator use to the nearest OHCA17) was switched off, affording fewer opportunities for community based rapid intervention. EMS responders were required to wear PPE, inevitably adding minutes to the time to reach the patient, potentially reducing the quality of CPR18 and impairing non-technical skills.19 These necessary precautions, along with an unprecedented increase in call volumes (>45,000 additional calls across the 2 month period) and extended call answering times, may have contributed to the longer response times seen, which may adversely affect outcome.20, 21 A delayed EMS response during COVID-19 is not specific to London, but has also been reported by six of the eight cities and provinces that have published data so far.5, 6, 7, 9, 10, 11, 12
We report a reduction in shockable rhythms during the pandemic period, and also amongst the COVID-19 sub-group. This finding may be a consequence of extended EMS response times, as it took longer to arrive on-scene both during the COVID-19 period and for the COVID-19 subgroup. The studies from Lombardia and Paris6, 7 also report extended response times along with fewer shockable rhythms. However, in New York City8 they found fewer instances of VF/VT, but response times were unchanged. We also observed, in line with other studies,4, 5, 6, 10 differences in the aetiology of cardiac arrests. Both during the overall COVID-19 period and within the COVID-19 subgroup, we found fewer presumed cardiac cases and an increase in medical causes. Aetiology is not something that would be impacted by response times, raising the possibility that the characteristics of OHCA are influenced by the infection itself.
Bystander CPR rates in London were higher during COVID-19 compared to the previous year, which was also seen in Victoria,10 but not reported elsewhere.3, 4, 5, 6, 7, 8, 9, 11, 12, 22 As the number of OHCAs in residential locations also increased, it is likely that bystander CPR occurred more often because it was provided by someone known to the patient and motivated to help, regardless of any potential fear over virus transmission.
That fewer arrests occurred in public is unsurprising given the social restrictions imposed and with the full UK lockdown occurring part-way through the studied period. This would also account for the halving of PAD deployment. Lower PAD use specifically amongst the COVID-19 subgroup can be further explained by the government guidelines that anyone infected, or suspected to have COVID-19, should stay at home and isolate.
We identified increased OHCA amongst black and ethnic minority (BAME) patients, and a decrease amongst those of white ethnic origin, compared to the previous year. This pattern was also evident when comparing the COVID-19 group to those not suspected to be infected. However, as there was also an increase in unknown ethnicity, we do not know the true distribution of White and BAME patients amongst our cohort and this questions the robustness of these findings Nonetheless, they cautiously lend support to emerging evidence that BAME populations may be particularly susceptible to COVID-19,23 the reasons for which are currently not understood.
There are a number of limitations to our study, one being that our incidence rates use mid-2019 population estimates, which relate to the residents of the city and do not take into account temporal fluctuations in the population during the working week, at weekends, or during the pandemic itself. Another notable limitation is that the identification of cases with a confirmed/suspected COVID-19 relied on the documentation of this information by EMS clinicians. This, combined with the absence of a widespread SARS-CoV-2 testing programme, means that the likely incidence of COVID-19 in our cohort could be very different to that which we report. The existence of asymptomatic presentations could mean that more patients were infected and the potential link between COVID-19 and OHCA is even stronger than our data shows. Equally, as those clinically suspected to have COVID-19 were not formally tested or diagnosed, the infection rate amongst our cohort could be much lower. Even so, our reported rate of 24.5% confirmed/suspected infections closely aligns with that reported from Italy (25.5% and 28.5%).5, 6 Access to patient level testing data and/or post-mortem data would have allowed us to report the true proportion of patients with SARS-CoV-2 infection who suffered OHCA and draw firmer conclusions of the direct and indirect impact of the pandemic.
Conclusion
During the first wave of the COVID-19 pandemic in London, we saw a dramatic rise in OHCA incidence accompanied by a significant reduction in survival. The pattern of increased incidence and mortality closely reflected the rise in confirmed COVID-19 infections in the city. These results have important implications with further surges of COVID-19 infection expected. EMS systems will need to prepare for potentially further considerable increases in OHCA, and the wider healthcare system will need to ensure adequate attention is paid to preventing indirect deaths.
Credit author statement
RF and AS conceived the study idea and designed the protocol. AS performed the statistical analysis. RF and AS drafted the manuscript. All authors commented on the draft manuscript and approved the final manuscript.
Declarations of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Rachael T. Fothergill, Email: rachael.fothergill@londonambulance.nhs.uk.
Adam L. Smith, Email: adam.smith@londonambulance.nhs.uk.
Fenella Wrigley, Email: fenella.wrigley@londonambulance.nhs.uk.
Gavin D. Perkins, Email: G.D.Perkins@warwick.ac.uk.
References
- 1.World Health Organisation . 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 . Accessed 23/09/2020. [Google Scholar]
- 2.UK Government . 2020. Coronavirus (COVID-19) in the UK.https://coronavirus.data.gov.uk/ . Accessed 15/09/2020. [Google Scholar]
- 3.Semeraro F., Gamberini L., Tartaglione M., Iarussi B., Descovich C., Picoco C. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: system response to preserve performances. Resuscitation. 2020;157:1–2. doi: 10.1016/j.resuscitation.2020.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elmer J., Okubo M., Guyette F.X., Martin-Gill C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. 2020;156:282–283. doi: 10.1016/j.resuscitation.2020.08.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldi E., Sechi G.M., Mare C., Canevari F., Brancaglione A., Primi R. Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. New Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C., Canevari F., Brancaglione A., Primi R. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marikon E., Karam N., Jost D., Perrot D., Frattini B., Derkenne C. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai P.H., Lancet E.A., Weiden M.D., Webber M.P., Zeig-Owens R., Hall C.B. Characteristics associated with out-of-Hospital Cardiac Arrests and Resuscitations During the Novel Coronavirus Disease 2019 Pandemic in New York City. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uy-Evanado A., Chugh H.S., Sargsyan A., Nakamura K., Mariani R., Hadduck K. Out-of-Hospital Cardiac Arrest Response and Outcomes During the COVID-19 Pandemic. JACC: Clin Electrophysiol. 2020 doi: 10.1016/j.jacep.2020.08.010. 2020/08/14/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.J. Ball, Z. Nehme, S. Bernard, D. Stub, M. Stephenson, K. Smith, M. Stephenson, K. Smith. Collateral damage: hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. [DOI] [PMC free article] [PubMed]
- 11.Paoli A., Brischigliaro L., Scquizzato T., Favaretto A., Spagna A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation. 2020;154:47–49. doi: 10.1016/j.resuscitation.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.F.R. Ortiz, P.F. del Valle, E.C. Knox, X.J. Fabrega, J.M.N. Pascual, I.M. Rodriguez, et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. [DOI] [PMC free article] [PubMed]
- 13.Office for National Statistics . 2020. Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2019.https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2019estimates . Accessed 15/09/2020. [Google Scholar]
- 14.Resuscitation Council UK . 2015. 2015 Resuscitation Guidelines.https://www.resus.org.uk/library/2015-resuscitation-guidelines . Accessed 15/09/2020. [Google Scholar]
- 15.Couper K., Taylor-Phillips S., Grove A., Freeman K., Osokogu O., Court R. COVID-19 in cardiac arrest and infection risk to rescuers: a systematic review. Resuscitation. 2020;151:59–66. doi: 10.1016/j.resuscitation.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perkins G.D., Couper K. COVID-19: long-term effects on the community response to cardiac arrest? Lancet Public Health. 2020;5:e415–e416. doi: 10.1016/S2468-2667(20)30134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith C.M., Wilson M.H., Ghorbangholi A., Hartley-Sharpe C., Gwinnutt C., Dicker B. The use of trained volunteers in the response to out-of-hospital cardiac arrest; the GoodSAM experience. Resuscitation. 2017;121:123–126. doi: 10.1016/j.resuscitation.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 18.Sahu A.K., Suresh S., Mathew R., Aggarwal P., Nayer J. Impact of personal protective equipment on the effectiveness of chest compression—a systematic review and meta-analysis. Am J Emerg Med. 2020;(Oct 1) doi: 10.1016/j.ajem.2020.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parush A., Wacht O., Gomes R., Frenkel A. Human factor considerations in using personal protective equipment in the COVID-19 pandemic context: binational survey study. J Med Internet Res. 2020;22 doi: 10.2196/19947. e19947-e19947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nichol G., Cobb L.A., Yin L., Maynard C., Olsufka M., Larsen J. Briefer activation time is associated with better outcomes after out-of-hospital cardiac arrest. Resuscitation. 2016;107:139–144. doi: 10.1016/j.resuscitation.2016.06.040. [DOI] [PubMed] [Google Scholar]
- 21.Grunau B., Kawano T., Scheuermeyer F., Tallon J., Reynolds J., Besserer F. Early advanced life support attendance is associated with improved survival and neurologic outcomes after non-traumatic out-of-hospital cardiac arrest in a tiered prehospital response system. Resuscitation. 2019;135:137–144. doi: 10.1016/j.resuscitation.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Sayre M.R., Barnard L.M., Counts C.R., Drucker C.J., Kudenchuk P.J., Rea T.D. Prevalence of COVID-19 in Out-of-Hospital Cardiac Arrest. Circulation. 2020;142:507–509. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed M.H. Black and Minority Ethnic (BAME) Alliance Against COVID-19: One Step Forward. J Rac Ethnic Health Disparit. 2020;7:822–828. doi: 10.1007/s40615-020-00837-0. 2020/10/01. [DOI] [PMC free article] [PubMed] [Google Scholar]