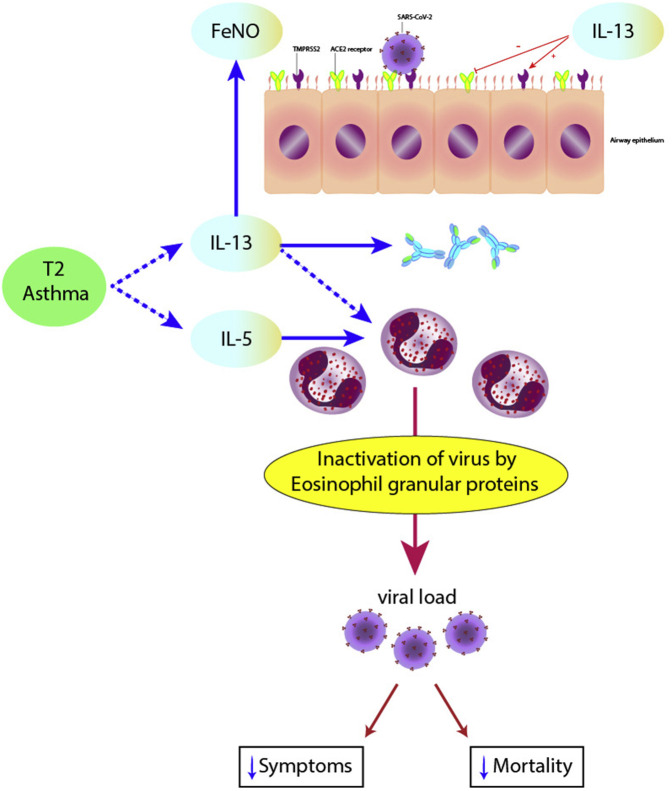
Persistent asthma is typically characterized by activation of proinflammatory cytokines including interleukins (IL)-4, -5, and -13, manifesting as the type 2 (TH2) endotype with raised levels of immunoglobulin E (IgE), eosinophils, and fractional exhaled nitric oxide (FeNO). Patients with severe asthma appear to be more susceptible to viral tiggers including severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), resulting in worse COVID-19 outcomes.1 An observational study found that patients with non-allergic asthma were at higher risk of SARS-CoV2 infection and more severe COVID outcomes compared with those with allergic asthma.2 Activated eosinophils form part of the innate immune response by attenuating viral load. It has been suggested that a degree of eosinophilic antiviral insufficiency may occur in asthma whereby there is a defective virus sink in the lungs with attenuated viral clearance3 (Figure 1 ).
Figure 1.
The paradoxical role of type 2 inflammation in regulation of asthma control and response to infection with SARS-CoV-2. Type 2 activation involves IL-5 with eosinophilia and IL-13 with raised FeNO and IgE. IL13 also acts to downregulate ACE2 and upregulate TMPRSS2 cell entry receptors for SARS-CoV-2. Increased eosinophils are accompanied by worse asthma control but protective against severe COVID-19. In asthma there may a degree of innate eosinophilic antiviral insufficiency resulting in attenuated viral clearance. ACE2, Angiotensin converting enzyme 2; FeNO, fractional exhaled nitric oxide; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TMPRSS2, transmembrane protease serine-2.
The allergic phenotype with IgE sensitization is accompanied by IL-13-mediated differential regulation of SARS-CoV-2 cell entry receptors with decreased expression of angiotensin converting enzyme 2 (ACE2) and increased transmembrane protease serine-2 (TMPRSS2)4 (Figure 1). Moreover, inhaled corticosteroids (ICS) result in reduced expression of both ACE2 and TMPRSS2.5 The United Kingdom OPENSAFELY cohort found that patients with asthma taking high-dose ICS had a 55% (95% confidence interval [CI]: 9-54) increased risk of death from COVID-19, which was interpreted as being due to confounding by disease severity.6
Severe COVID-19 occurring in susceptible individuals may be associated with cytokine-mediated hyperinflammation and associated coagulopathy with multisystem involvement and death.7 Markers of worsening disease include hypoxemia, lymphopenia, thrombocytopenia, and raised levels of IL-6, C reactive protein, ferritin, lactate dehydrogenase, and D-dimers. Eosinopenia may also be part of the overall cytopenic process in the early phase of severe COVID-19, with later resolution of eosinophil counts being associated with clinical recovery.8 The pathogenesis of eosinopenia is complex including suppression of production and release of eosinophils from bone marrow along with interferon-mediated apoptosis and attenuated expression of chemokines. Whether or not eosinopenia is an epiphenomenon or directly related to the COVID-19 disease process is unclear, especially in relation to patients with type 2 asthma.
In this issue of the journal, new data from Ferastraoaru et al9 help to further elucidate the role of eosinophils in asthma patients with severe COVID-19. They performed a retrospective analysis during Spring 2020 among 737 adult asthma patients with COVID-19 seen in the emergency department with severe COVID-19 in the Bronx New York City, of whom 79% were subsequently admitted. Patients with asthma comprised 20% of all patients with COVID-19 in their cohort. The presence of a preadmission mean blood eosinophil count (BEC) ≥150 cells/μL was found in 53.1% of patients with asthma. Patients with asthma who had a mean BEC ≥150 cells/μL before COVID-19 were 54% (95% CI: 2-79) less likely to be admitted, whereas those with comorbid heart failure, chronic kidney disease, or chronic obstructive pulmonary disease (COPD), but not allergic comorbidities, were more likely to be admitted. Forced expiratory volume in 1 second (%) predicted, IgE levels, and use of oral or inhaled corticosteroids were not associated with an increased risk of admission. Notably, hospitalized patients with asthma who had a peak BEC ≥150 cells/μL during admission were much less likely to die compared with those with a BEC <150 cells/μL with respective mortality rates of 9.6% versus 25.8%. Moreover, such patients had a significantly greater BEC before admission amounting to the mean difference of 74 cells/μL, whereas there were no differences in inflammatory markers. There was no such relationship between lymphocyte or platelet counts and mortality in admitted patients. Larger cohorts of patients with asthma and perhaps asthma-COPD overlap will be required to replicate these initial observations.
Taken together, these data suggest that the presence of raised blood eosinophils in asthma appears to be protective against severe COVID-19 outcomes in terms of hospital admission and death. In some respects, this observation may appear to be counterintuitive in that blood eosinophilia is a significant risk factor for worse asthma control and related exacerbations but on the other hand is associated with better outcomes in COVID-19. This paradox might perhaps be explained by the apparent disconnect between TH2 inflammation occurring in asthma and TH1 inflammation in COVID-19. Another point worth making is that levels of circulating and tissue eosinophils may be dissociated in asthma,10 although sputum eosinophils are not measured in routine clinical practice. The presence of raised eosinophils does not inform about eosinophil activation per se, which would require measurement of eosinophil cationic protein or eosinophil-derived neurotoxin. Blood eosinophils are predominantly mediated by IL-5 and in part by IL-13, whereas FeNO is mediated by IL-13 (Figure 1). Consequently, further studies are indicated to explore whether raised FeNO levels in asthma might also be paradoxically related to better COVID-19 outcomes, especially because higher FeNO levels are associated with worse asthma control.
It is also pertinent to speculate whether the use of anti-IL-5 agents such as mepolizumab and benralizumab, which suppress blood eosinophils, might be expected to be accompanied by worsening of COVID-19 outcomes in patients with severe asthma. However, improved asthma control and confounding by disease severity in relation to the use of IL-5 blockers is also likely to be a key factor. By the same token, it would be relevant to know if patients with the type 2 low asthma endotype who have low eosinophils might be more prone to more severe COVID-19 outcomes, in the same way as in non-allergic asthma.2
It remains to be established from much larger cohorts of patients with asthma if there truly is a reciprocal relationship between raised type 2 biomarkers and severity of COVID-19 outcomes. Ultimately clinicians should continue to focus on maintaining optimal long-term asthma control that will reduce exacerbations and potentially confer protection against viral triggers possibly including SARS-CoV-2. In this respect, achieving such therapeutic goals involves suppression of type 2 disease biomarkers including eosinophils and FeNO.
Footnotes
No funding was received for this work.
Conflicts of interest: B. Lipworth reports nonfinancial support (equipment) from GSK; grants, personal fees (consulting, talks, and advisory board), and other support (attending ATS and ERS) from AstraZeneca; grants, personal fees (consulting, talks, and advisory board), and other support (attending ERS) from Teva; personal fees (consulting) from Lupin; personal fees (consulting) from Glenmark; personal fees (consulting) from Vectura; personal fees (consulting) from Dr. Reddy; personal fees (consulting) from Sandoz, in relation to the submitted work; and grants, personal fees (consulting, talks, and advisory board), and other support (attending BTS) from Boehringer Ingelheim; grants and personal fees (advisory board and talks) from Mylan; grants and personal fees (consulting) from Sanofi, outside of the submitted work; and the son of B. Lipworth is presently an employee of AstraZeneca. R. Chan declares no relevant conflicts of interest. C. R. Kuo reports personal fees (talks) from AstraZeneca, personal fees (advisory board) from Circassia, personal fees (talks) in relation to the submitted work, and other support from Chiesi (attending BTS) outside of the submitted work.
References
- 1.Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang J.M., Koh H.Y., Moon S.Y., Yoo I.K., Ha E.K., You S. Allergic disorders and susceptibility to and severity of COVID-19: a nationwide cohort study. J Allergy Clin Immunol. 2020;146:790–798. doi: 10.1016/j.jaci.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jesenak M., Schwarze J. Lung eosinophils-A novel "virus sink" that is defective in asthma? Allergy. 2019;74:1832–1834. doi: 10.1111/all.13811. [DOI] [PubMed] [Google Scholar]
- 4.Kimura H., Francisco D., Conway M., Martinez F.D., Vercelli D., Polverino F. Type 2 inflammation modulates ACE2 and TMPRSS2 in airway epithelial cells. J Allergy Clin Immunol. 2020;146:80–88.e8. doi: 10.1016/j.jaci.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peters M.C., Sajuthi S., Deford P., Christenson S., Rios C.L., Montgomery M.T. COVID-19-related genes in sputum cells in asthma. Relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020;202:83–90. doi: 10.1164/rccm.202003-0821OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schultze A., Walker A.J., MacKenna B., Morton C.E., Bhaskaran K., Brown J.P. Risk of COVID-19-related death among patients with chronic obstructive pulmonary disease or asthma prescribed inhaled corticosteroids: an observational cohort study using the OpenSAFELY platform. Lancet Respir Med. 2020;8:1106–1120. doi: 10.1016/S2213-2600(20)30415-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipworth B., Chan R., Kuo C.R. Predicting severe outcomes in COVID-19. J Allergy Clin Immunol Pract. 2020;8:2582–2584. doi: 10.1016/j.jaip.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindsley A.W., Schwartz J.T., Rothenberg M.E. Eosinophil responses during COVID-19 infections and coronavirus vaccination. J Allergy Clin Immunol. 2020;146:1–7. doi: 10.1016/j.jaci.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferastraoaru D., Hudes G., Jershow E., Jariwala S., Karagic M., de Vos G. Eosinophilia in asthma patients is protective against severe COVID-19 illness. J Allergy Clin Immunol Pract. 2021;9:1152–1162. doi: 10.1016/j.jaip.2020.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hastie A.T., Moore W.C., Li H., Rector B.M., Ortega V.E., Pascual R.M. Biomarker surrogates do not accurately predict sputum eosinophil and neutrophil percentages in asthmatic subjects. J Allergy Clin Immunol. 2013;132:72–80. doi: 10.1016/j.jaci.2013.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]