Abstract
Background
Coronavirus disease 2019 (COVID-19) has caused an unprecedented change in the apparent epidemiology of acute coronary syndromes (ACS). However, the interplay between this disease, changes in pollution, climate, and aversion to activation of emergency medical services represents a challenging conundrum. We aimed at appraising the impact of COVID-19, weather, and environment features on the occurrence of ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI) in a large Italian region and metropolitan area.
Methods and results
Italy was hit early on by COVID-19, such that state of emergency was declared on January 31, 2020, and national lockdown implemented on March 9, 2020, mainly because the accrual of cases in Northern Italy. In order to appraise the independent contribution on changes in STEMI and NSTEMI daily rates of COVID-19, climate and pollution, we collected data on these clinical events from tertiary care cardiovascular centers in the Lazio region and Rome metropolitan area. Multilevel Poisson modeling was used to appraise unadjusted and adjusted effect estimates for the daily incidence of STEMI and NSTEMI cases.
The sample included 1448 STEMI and 2040 NSTEMI, with a total of 2882 PCI spanning 6 months. Significant reductions in STEMI and NSTEMI were evident already in early February 2020 (all p<0.05), concomitantly with COVID-19 spread and institution of national countermeasures. Changes in STEMI and NSTEMI were inversely associated with daily COVID-19 tests, cases, and/or death (p<0.05). In addition, STEMI and NSTEMI incidences were associated with daily NO2, PM10, and O3 concentrations, as well as temperature (p<0.05). Multi-stage and multiply adjusted models highlighted that reductions in STEMI were significantly associated with COVID-19 data (p<0.001), whereas changes in NSTEMI were significantly associated with both NO2 and COVID-19 data (both p<0.001).
Conclusions
Reductions in STEMI and NSTEMI in the COVID-19 pandemic may depend on different concomitant epidemiologic and pathophysiologic mechanisms. In particular, recent changes in STEMI may depend on COVID-19 scare, leading to excess all-cause mortality, or effective reduced incidence, whereas reductions in NSTEMI may also be due to beneficial reductions in NO2 emissions in the lockdown phase.
Keywords: Acute coronary syndrome, Climate, COVID-19, Environment, Pollution, Weather
1. Introduction
Recent months have seen a dramatic change in worldwide mortality, morbidity and healthcare delivery fundamentals due to the coronavirus disease 2019 (COVID-19) pandemic [[1], [2], [3], [4]]. This infectious disease has created unprecedented challenges to healthcare systems and societies at large, with most governments proceedings to intense containment and mitigation efforts, often repeatedly [5]. These actions, which in the most intense fashion have been actual regional or national lockdowns, have also been mirrored by substantial individual and collective scare, such that “potential” patients have tended to avoid, especially in the most dangerous times, to seek medical care despite moderate or severe symptoms or signs of disease [[6], [7], [8]].
In particular, it has been shown in several series from different countries with diverse healthcare systems that the incidence of acute coronary syndromes (ACS) and ST-elevation myocardial infarction (STEMI) have apparently decreased in the early months of 2020, together with the highest daily reported cases of COVID-19 and COVID-19-related infections [3,4,6,9,10]. Most recently, leading investigations have highlighted that in many cases ACS and STEMI have not actually decreased universally, but instead in many instances they have shifted in presentation, in the sense that patients with ACS have preferred in several cases to present later rather than early, or to avoid presenting at all [4,10,11].
Another intriguing piece of the puzzle has been the overreaching decrease in environmental pollution during regional and national lockdowns, given the significative reduction or actual stop of many human sources of pollutants, ranging from traffic to factories [12]. Despite such apparently favorable effects of COVID-related lockdowns, pollution has been purportedly associated with more adverse effects of COVID-19, in particular for nitrogen-related pollutants, and even with the possibility (to date never proved though) that the virus can be carried by particulate matter (PM) with potentially dramatic effects on contagion rate [[13], [14], [15], [16], [17]].
Given the importance of exploring in detail the complex interplay between environment and weather features, on one hand [18], and COVID-19, on the other hand, on changes in the incidence of ACS, we conducted a region-wide multicenter retrospective analysis aiming at disentangling the independent impact of COVID-19 and pollution on ACS incidence.
2. Methods
Details of this research project have been reported already in detail elsewhere [19,20]. Specifically, we queried all healthcare institutions with 24/7 catheterization laboratory activity in the Lazio region for detailed data on daily STEMI and non-ST-elevation myocardial infarction (NSTEMI), distinguishing those requiring angiography (irrespective of subsequent revascularization), and those requiring percutaneous coronary intervention (PCI). The periods of time of interest were January 1, 2019-March 30, 2019, and January 1, 2020-March 30, 2020.
COVID-19 data were obtained from the Italian Protezione Civile service website [21,22], distinguishing new cases, new deaths, and new tests, per day. Additional COVID-19-related initiatives were also sought and collected, such as the date of in which the national state of emergency was declared (January 31, 2020), and when national lockdown had been implemented (March 9, 2020), mainly because the exponential accrual of cases in Northern Italy. Weather features were obtained from Agenzia Regionale Per l'Ambiente (ARPA) Lazio, yielding daily details on temperature (measured as Celsius degrees), humidity (measured as percentage), and rainfall (measured as mm) at the province level [23]. Finally, ARPA also provided detailed data on benzene, nitric oxide (NO), nitrogen dioxide (NO2), nitrogen oxides (NOX), ozone (O3), sulfur dioxide (SO2), PM with a diameter ≤2.5 μm (PM2.5), and PM with a diameter ≤10 μm (PM10). All pollution features were expressed as μm/m3.
Descriptive analysis was based on mean and standard deviation, either per month or per day, whereas graphical depiction was based on time series analysis and scatterplots with generalized additive model smoothing. Inferential analysis was based, as in prior works from our research team, on a mixed effect model with Poisson likelihood and log link, accounting for center and province clustering [19,20]. Independent variables of interest were year, COVID-19 features (including days of governmental actions such as declaration of state of emergency), pollutants, and weather features. After such unadjusted analysis, sequentially expanding modeling steps were carried out to explore the independent impact of COVID-19, environment, and weather variables, for exploratory purposes. Computations were performed with R 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) and Stata 13 (StataCorp, College Station, TX, USA).
3. Results
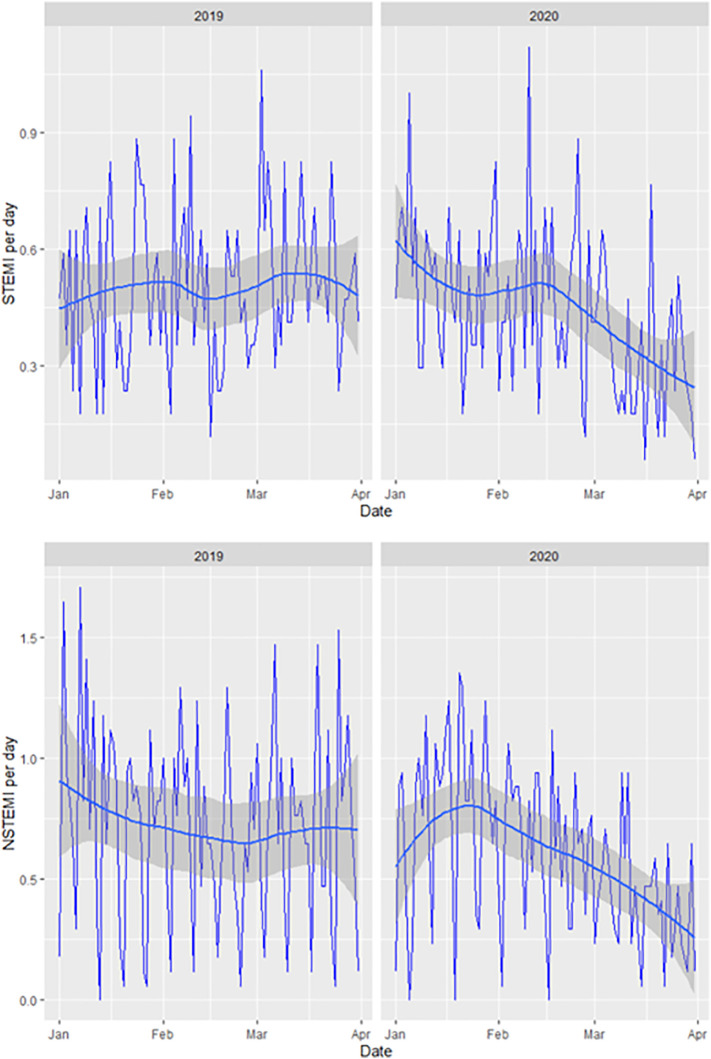
The sample included 1448 STEMI and 2040 NSTEMI, with a total of 2882 PCI spanning 6 months (Table 1 ), showing a significant decrease in both types of ACS since mid-February 2020 (Fig. 1 ). These changes were mirrored by decreases in some but not all pollution features, including NO, NO2, NOX, and SO2 (all p<0.05).
Table 1.
Descriptive analysis, according to year and month, of ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), coronavirus disease 2019 (COVID-19), environmental pollution, and weather features.
| Feature | January |
February |
March |
|||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| STEMI per day | 0.4896 | 0.5256 | 0.4643 | 0.4746 | 0.5503 | 0.3187 |
| STEMI requiring PCI per day | 0.4782 | 0.5085 | 0.4433 | 0.4462 | 0.5256 | 0.3169 |
| NSTEMI per day | 0.7742 | 0.7647 | 0.6722 | 0.6410 | 0.7191 | 0.4061 |
| NSTEMI requiring PCI per day | 0.5275 | 0.5439 | 0.4622 | 0.4442 | 0.5019 | 0.2979 |
| STEMI/NSTEMI per day ratio | 0.3733 | 0.3862 | 0.4774 | 0.3997 | 0.4311 | 0.2685 |
| STEMI/NSTEMI requiring PCI per day ratio | 0.4334 | 0.362 | 0.4874 | 0.4284 | 0.4019 | 0.2152 |
| COVID-19 | ||||||
| Cases | 0 | 0 | 0 | 0.17±0.65 | 0 | 99.65±77.71 |
| Deaths | 0 | 0 | 0 | 0 | 0 | 5.23±5.13 |
| Tests | 0 | 0 | 0 | 23.41±81.19 | 0 | 1096.71±1274.65 |
| Environmenta | ||||||
| Benzene | 1.825±0.682 | 2.303±0.689 | 1.479±0.587 | 1.341±0.421 | 1.047±0.256 | 0.917±0.272 |
| Nitric oxide | 29.30±18.55 | 41.54±20.70 | 21.05±12.14 | 19.69±12.25 | 11.60±5.12 | 5.09±3.03 |
| Nitrogen dioxide | 34.25±9.83 | 42.25±11.51 | 33.63±11.97 | 32.44±10.69 | 28.97±7.93 | 17.93±7.09 |
| Nitrogen oxides | 92.09±41.20 | 118.64±44.53 | 76.03±31.21 | 70.18±29.29 | 55.45±15.77 | 28.97±12.33 |
| Ozone | 31.29±10.69 | 22.39±9.74 | 43.11±13.00 | 39.20±13.42 | 55.22±11.22 | 55.33±9.76 |
| Sulfur dioxide | 1.25±0.43 | 2.64±7.65 | 1.32±0.52 | 3.27±10.83 | 0.86±0.42 | 4.31±14.72 |
| Particulate matter <2.5 μm | 17.209±8.288 | 26.589±10.055 | 17.902±9.305 | 15.760±7.451 | 13.221±4.529 | 13.267±6.827 |
| Particulate matter <10 μm | 25.621±10.729 | 39.185±11.008 | 28.397±11.195 | 27.028±9.671 | 24.623±7.581 | 23.638±11.214 |
| Weather | ||||||
| Temperature (°C) | 6.46±2.22 | 7.81±2.26 | 9.51±1.70 | 10.66±2.18 | 12.44±1.56 | 11.32±2.16 |
| Humidity (%) | 74.66±17.39 | 80.45±9.50 | 66.50±20.39 | 74.68±15.21 | 68.58±17.84 | 74.35±11.52 |
| Rainfall (mm) | 2.29±4.71 | 1.59±8.11 | 0.64±5.16 | 1.10±2.43 | 0.27±1.10 | 2.88±6.33 |
All pollutants are expressed as μg/m3; PCI=percutaneous coronary intervention; PM=particulate matter.
Fig. 1.
Changes in the daily incidence of ST-elevation myocardial infarction (STEMI, top panel) and non-ST-elevation myocardial infarction (NSTEMI, bottom panel) in the first three months of 2019 and of 2020.
Unadjusted analysis showed that year, declaration of emergency, national lockdown, daily cases, deaths and tests were all negatively and significantly associated with STEMI and NSTEMI rates, as a whole or limiting the analysis to those requiring PCI (all p<0.05, Table 2 , Table 2S, Table 3S). Conversely, only benzene, NO, NO2, NOX, SO2, and PM10 were nominally associated with changes in STEMI or NSTEMI rates (all p<0.05). Temperature was associated with fewer NSTEMI (p<0.001) and NSTEMI requiring PCI (p=0.002). Notably, STEMI to NSTEMI ratios were not associated with any feature (all p>0.05).
Table 2.
Unadjusted analysis.a
| Features | STEMI per day | STEMI requiring PCI per day | NSTEMI per day | NSTEMI requiring PCI per day | STEMI/NSTEMI per day ratio | STEMI/NSTEMI requiring PCI per day ratio |
|---|---|---|---|---|---|---|
| Year | −0.1355 (−0.2385; −0.0325), p=0.010 | −0.1331 (−0.2382; −0.0279), p=0.013 | −0.1821 (−0.2690; −0.0950), p<0.001 | −0.1478 (−0.2519; −0.0438), p=0.005 | −0.0929 (−0.2661; 0.0802), p=0.293 | −0.1193 (−0.3121; 0.0735), p=0.225 |
| COVID-19 | ||||||
| Declaration of emergency | −0.2548 (−0.3697; −0.1399), p<0.001 | −0.2558 (−0.3729; −0.1388), p<0.001 | −0.3455 (−0.4441; −0.2470), p<0.001 | −0.3269 (−0.4446; −0.2092), p<0.001 | −0.1087 (−0.3049; 0.0874), p=0.277 | −0.2114 (−0.4355; 0.0127), p=0.064 |
| National lockdown | −0.2651 (−0.3846; −0.1456), p<0.001 | −0.2630 (−0.3861; −0.1400), p<0.001 | −0.3940 (−0.4999; −0.2881), p<0.001 | −0.3614 (−0.4867; −0.2360), p<0.001 | −0.0882 (−0.2962; 0.1199), p=0.406 | −0.2081 (−0.4469; 0.0304), p=0.087 |
| Cases | −0.0033 (−0.0047; −0.0020), p<0.001 | −0.0031 (−0.0044; −0.0018), p<0.001 | −0.0048 (−0.0060; −0.0035), p<0.001 | −0.0046 (−0.0061; −0.0031), p<0.001 | −0.0026 (−0.0053; 0.0002), p=0.069 | −0.0027 (−0.0058; 0.0003), p=0.080 |
| Deaths | −0.0457 (−0.0684; −0.0230), p<0.001 | −0.0414 (−0.0640; −0.0188), p<0.001 | −0.0732 (−0.0937; −0.0511), p<0.001 | −0.0744 (−0.1010; −0.0478), p<0.001 | −0.0208 (−0.0645; 0.0228), p=0.351 | −0.0241 (−0.0732; 0.0249), p=0.336 |
| Tests | −0.0003 (−0.0004; −0.0002), p<0.001 | −0.0003 (−0.0004; −0.0002), p<0.001 | −0.003 (−0.0004; −0.0002), p<0.001 | −0.0003 (−0.0005; −0.0002), p<0.001 | −0.0002 (−0.0004; 0.0000), p=0.053 | −0.002 (−0.0005; 0.0000), p=0.100 |
| Environmentb | ||||||
| Benzene | 0.0393 (−0.0362; 0.1147), p=0.308 | 0.0395 (−0.0369; 0.1159), p=0.311 | 0.1921 (0.1321; 0.2520), p<0.001 | 0.1817 (0.1077; 0.2557), p<0.001 | −0.0465 (−0.1715; 0.0784), p=0.465 | −0.0444 (−0.1854; 0.0965), p=0.537 |
| Nitric oxide | 0.0027 (−0.0005; 0.0059), p=0.100 | 0.0025 (−0.0007; 0.0057), p=0.127 | 0.0100 (0.0075; 0.0125), p<0.001 | 0.0097 (0.0067; 0.0127), p<0.001 | −0.0032 (−0.0086; 0.0022), p=0.248 | −0.0005 (−0.0065; 0.0053), p=0.845 |
| Nitrogen dioxide | 0.0074 (0.0024; 0.0123), p=0.004 | 0.0069 (0.0018; 0.0120), p=0.008 | 0.0183 (0.0140; 0.0225), p<0.001 | 0.0163 (0.0112; 0.0213), p<0.001 | 0.0020 (−0.0065; 0.0105), p=0.645 | 0.0034 (−0.0061; 0.0130), p=0.477 |
| Nitrogen oxides | 0.0015 (0.0001; 0.0029), p=0.027 | 0.0014 (0.0000; 0.0029), p=0.044 | 0.0049 (0.0038; 0.0060), p<0.001 | 0.0047 (0.0034; 0.0059), p<0.001 | −0.0009 (−0.0033; 0.0015), p=0.464 | 0.0000 (−0.0026; 0.0026), p=0.983 |
| Ozone | −0.0032 (−0.0067; 0.0002), p=0.068 | −0.0032 (−0.0067; 0.0040), p=0.082 | −0.0087 (−0.0116; −0.0057), p<0.001 | −0.0083 (−0.0118; −0.0048), p<0.001 | −0.0001 (−0.0059; 0.0058), p=0.984 | −0.0021 (−0.0086; 0.0044), p=0.528 |
| Sulfur dioxide | −0.0011 (−0.0065; 0.0043), p=0.679 | −0.0011 (−0.0064; 0.0043), p=0.687 | −0.0082 (−0.0138; −0.0026), p=0.004 | −0.0047 (−0.0123; 0.0030), p=0.232 | −0.0007 (−0.0095; 0.0080), p=0.868 | 0.0010 (−0.0010; 0.0109), p=0.845 |
| Particulate matter <2.5 μm | 0.0013 (−0.0048; 0.0074), p=0.687 | 0.0015 (−0.0047; 0.0077), p=0.636 | 0.0048 (−0.0025; 0.0099), p=0.063 | 0.0034 (−0.0026; 0.0095), p=0.263 | −0.0044 (−0.0147; 0.0060), p=0.407 | −0.0054 (−0.0166; 0.0058), p=0.348 |
| Particulate matter <10 μm | 0.020 (−0.0029; 0.0068), p=0.429 | 0.0020 (−0.0030; 0.0069), p=0.435 | 0.0047 (0.0006; 0.0087), p=0.024 | 0.0037 (−0.0011; 0.0085), p=0.129 | −0.0020 (−0.0103; 0.0061), p=0.623 | −0.0025 (−0.0115; 0.0065), p=0.590 |
| Weather† | ||||||
| Temperature (°C) | −0.0089 (−0.0279; 0.0102), p=0.362 | −0.0101 (−0.0294; 0.0092), p=0.304 | −0.0317 (−0.0474; −0.0159), p<0.001 | −0.0290 (−0.0477; −0.0102), p=0.002 | 0.0014 (−0.0309; 0.0336), p=0.934 | −0.0117 (−0.0481; 0.0245), p=0.526 |
| Humidity (%) | 0.0004 (−0.0030; 0.0037), p=0.820 | 0.0003 (−0.0031; 0.0037), p=0.878 | 0.0015 (−0.0012; 0.0043), p=0.279 | 0.0025 (−0.0008; 0.0058), p=0.150 | 0.0037 (0.0020; 0.0094), p=0.205 | 0.0049 (−0.0011; 0.0109), p=0.112 |
| Rainfall (mm) | −0.0037 (−0.0130; 0.0057), p=0.442 | −0.0028 (−0.0120; 0.0063), p=0.543 | −0.0083 (−0.0177; 0.0011), p=0.082 | −0.0062 (−0.0175; 0.0051), p=0.283 | −0.0004 (−0.0122; 0.0114), p=0.953 | −0.0002 (−0.0210; 0.0205), p=0.985 |
Bold type highlights statistically significant results; COVID-19=coronavirus disease 2019; NSTEMI=non-ST-elevation myocardial infarction; STEMI=ST-elevation myocardial infarction.
All pollutants are expressed as μg/m3
All environment and weather features are expressed as daily mean, with the exception of total daily rainfall.
Table 3.
Adjusted analysis with sequentially expanding models.⁎
| Outcome | Stage 1: including only selected COVID-19 variables | Stage 2: including only selected environment variables | Stage 3: including only selected weather variables | Stage 4: including only selected variables from stages 2 and 3 | Stage 5: including only selected variables from stages 1 and 4 |
|---|---|---|---|---|---|
| STEMI per day | Emergency: p>0.05 Lockdown: p=0.009 Cases: p>0.05 Deaths: p=0.017 Tests: p>0.05 |
NO2 (mean): p=0.026 NOX (mean): p>0.05 O3 (min): p>0.05 |
– | – | Deaths: p<0.001 NO2 (mean): p=0.430 |
| STEMI requiring PCI per day | Emergency: p>0.05 Lockdown: p=0.045 Cases: p>0.05 Deaths: p>0.05 Tests: p<0.001 |
NO2 (mean): p=0.037 NOX (mean): p>0.05 O3 (min): p>0.05 |
– | – | Tests: p<0.001 NO2 (mean): p>0.05 |
| NSTEMI per day | Emergency: p>0.05 Lockdown: p<0.001 Cases: p<0.001 Deaths: p>0.05 Tests: p>0.05 |
Benzene (min): p>0.05 NO (min): p>0.05 NO2 (mean): p<0.001 NOX (min): p>0.05 O3 (min): p>0.05 SO2 (min): p>0.05 PM10: p<0.001 |
Temperature (mean): p<0.001 | NO2 (mean): p<0.001 PM10 (mean): p>0.05 Temperature (mean): p>0.05 |
Cases: p<0.001 NO2 (mean): p<0.001 |
| NSTEMI requiring PCI per day | Emergency: p>0.05 Lockdown: p=0.012 Cases: p<0.001 Deaths: p>0.05 Tests: p>0.05 |
Benzene (min): p>0.05 NO (min): p>0.05 NO2 (min): p=0.036 NOX (min): p>0.05 O3 (min): p=0.013 |
Temperature (mean): p=0.002 | NO2 (mean): p<0.001 O3 (min): p>0.05 Temperature (mean): p>0.05 |
Cases: p<0.001 NO2 (mean): p<0.001 |
min=minimum; COVID-19=coronavirus disease 2019; NO=nitric oxide; NOX=nitrogen oxides; NO2=nitric dioxide; O3=ozone; PM10=particulate matter <10 μm; NSTEMI=non-ST-elevation myocardial infarction; PM=particulate matter; SO2=sulfur dioxide; STEMI=ST-elevation myocardial infarction.
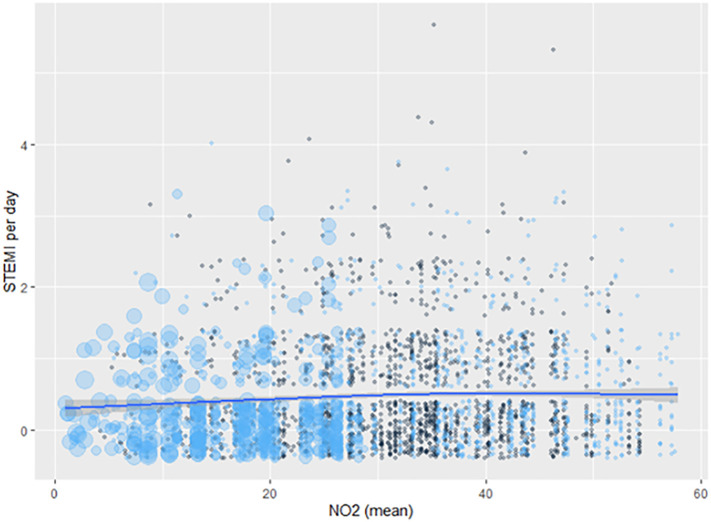
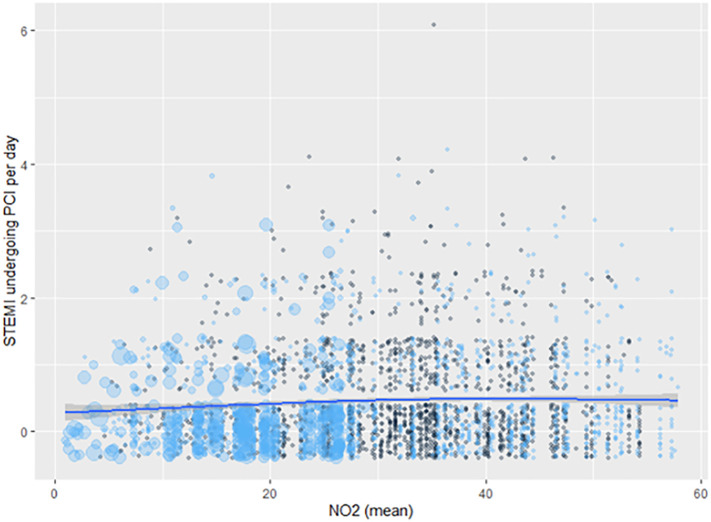
Reported as p values
Sequential modeling steps aimed at disentangling the independent contribution of the various factors potentially impacting on the incidence of ACS showed that lockdown date and daily COVID-19 deaths were the most impactful COVID-19-related factors, and NO2 was the most important pollutant (all p<0.05, Table 3, Fig. 2 ). However, eventually daily COVID-19 deaths were the only feature associated independently with STEMI rates. Similar findings were obtained for STEMI requiring PCI, with the notable difference that focusing on this subtype of STEMI, daily COVID-19 tests were more strongly associated with events than daily COVID-19 deaths (Fig. 3 ).
Fig. 2.
Association between mean daily nitric dioxide (NO2) concentration and risk of ST-elevation myocardial infarction (STEMI): black dots show the first 3 months of 2019, and blue dots the first 3 months of 2020, and dot size represents the number of same day coronavirus disease 2019 (COVID-19) deaths; the smooth line was computed using a generalized additive model. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
Association between mean daily nitric dioxide (NO2) concentration and risk of ST-elevation myocardial infarction (STEMI) undergoing percutaneous coronary intervention (PCI): black dots show the first 3 months of 2019, and blue dots the first 3 months of 2020, and dot size represents the number of same day coronavirus disease 2019 (COVID-19) tests; the smooth line was computed using a generalized additive model. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
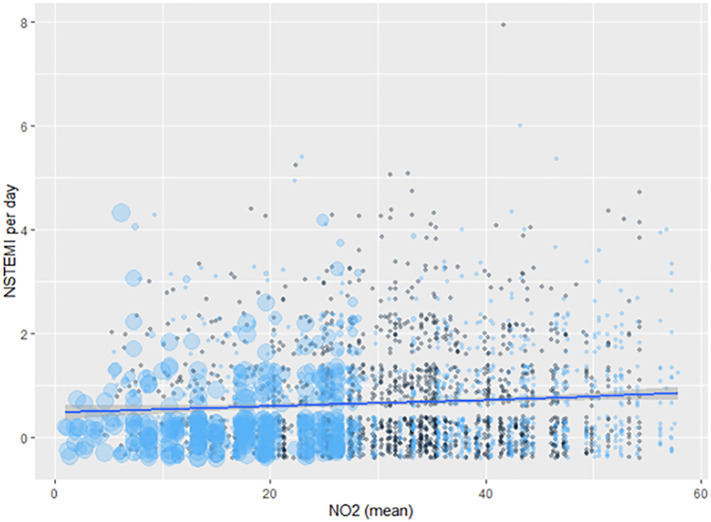
Analyses focusing on NSTEMI confirmed the importance of lockdown date and daily COVID-19 cases, on one hand, and NO2, O3, and PM10, on the other (all p<0.05). However, multivariable modeling, also including temperature, showed that daily COVID-19 cases and NO2 were the only variables significantly associated with NSTEMI, irrespective of management (both p<0.05, Fig. 4 ). Additional graphs were obtained to highlight the complex interplay between COVID-19 features, pollutants, and weather features on ACS trends (Fig. 1S, Fig. 2S, Fig. 3S, Fig. 4S, Fig. 5S).
Fig. 4.
Association between mean daily nitric dioxide (NO2) concentration and risk of non-ST-elevation myocardial infarction (NSTEMI): black dots show the first 3 months of 2019, and blue dots the first 3 months of 2020, and dot size represents the number of same day coronavirus disease 2019 (COVID-19) cases; the smooth line was computed using a generalized additive model. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
This observational study, aiming at appraising the multidimensional mechanisms impacting on recent trends in ACS incidence, has the following implications: a) as detailed also in many other reports, early 2020 has seen a significant reduction in ACS admissions, with similar improvements in the concentration of many pollutants given widespread anti-COVID-19 mitigation efforts; b) reductions in STEMI differ in features and mechanisms from reductions in NSTEMI; c) the decrease in STEMI admissions appears strongly associated with COVID-19-related variables, including lockdown measures, suggesting that such changes may depend on individual scare, avoidance or delay in seeking healthcare support, and may thus be counteracted by excesses in STEMI not admitted to hospitals (including fatal STEMI at home) or to an effective reduction of STEMI incidence; d) the decrease in NSTEMI recognizes different mechanisms, including COVID-19-related features (such as daily cases), but also the beneficial effects of anti-COVID-19 countermeasures on environmental pollution (especially on NO2).
Containment measures are appropriate to impede the diffusion of an infectious agent, for instance between countries or communities. However, this approach failed with COVID-19 for many reasons, including the globalized society, incubation period, common lack of symptoms, and limited point-of-care testing capabilities [21]. Accordingly, mitigation was chosen by many countries as a countermeasure for COVID-19, ranging from social distancing, use of personal protection equipment, closure of specific activities and venues (eg clubs and spas), to actual almost universal closure of leisure, education, and work activities (ie lockdown) [5,8,24]. While the benefits of imposing persistent and general lockdowns are being debated, it is apparent that in most countries lockdowns and other mitigation efforts were associated with favorable reductions in COVID-19 cases as well as deaths [5,7]. However, it has been shown that during such efforts, especially in March and April 2020, substantial decreases in ACS incidence occurred [3,4,9]. Accordingly, physicians, patients and decision makers have questioned the actual impact of COVID-19 on cardiovascular disease, notwithstanding the evident direct pathophysiologic role that SARS-CoV-2 may have on cardiovascular health. Further complicating the scenario, environmental pollution has shown significant improvements following widespread and forceful mitigation efforts. Indeed, Huang et al. have estimated that the benefits of reduced pollution due to mitigation strategies such as lockdown on fatality rates may be substantial, including 40% reduction in fatal stroke, 33% reduction in fatal ACS, and 18% reduction in fatal pulmonary disease [25]. Another important piece of the puzzle, integrating the apparent “silver lining” of reduced pollution due to lockdowns, is the evidence that pollution and COVID-19 may synergistically interact to exponentially increase mortality and morbidity, especially in frail subjects [26].
Accordingly, we aimed at exploring and attempted to disentangle the complex interplay between COVID-19 trends, ensuing countermeasures, environmental pollution, weather, and ACS incidence in a large urban Italian region. To the best of our knowledge, we originally found that that COVID-19 incidence, as well as accompanying scare and countermeasures, were associated with significant reductions in the concentration of many pollutants, as well as lower incidence of STEMI and NSTEMI. Adjusted analysis suggested that STEMI reductions were largely associated with COVID-19-related variables, including delayed presentation with ensuing increased out-of-hospital cardiac arrest, suggesting that reduced pollution may have contributed only in part, if at all, to such trends [27]. Conversely, we found that NSTEMI trends were more complex and depended on both COVID-19-related features and the beneficial effects of anti-COVID-19 countermeasures on environmental pollution (especially on NO2). This is not surprising, as, indeed, the potentially crucial role of NO2 in COVID-19-related cardiovascular morbidity and mortality has already been reported in an international ecological analysis encompassing France, Germany, Italy, and Spain [13]. Similarly, the hypothesis that COVID-19 countermeasures could be, at least in part, causing the evident reduction in ACS incidence in early 2020 has already been proposed by other investigators, such as Claeys and colleagues [4], who documented a nationwide 26% reduction in STEMI admissions in Belgium during a 3-week period in March 2020, for instance due to changes in traffic patterns [28].
The main novelties of our work concern the impact of COVID-19-related improvements in pollution on NSTEMI, such that, awaiting for additional studies on this topic, dedicated risk prediction tools (eg smartphone apps) could be developed and refined to predict patients at risk of all cause, COVID-19, and cardiovascular morbidity and mortality encompassing several multidimensional features, ranging from patient characteristics, to local COVID-19 features, governmental countermeasures, pollution, and climate data [3,29,30]. Risk stratification based on these tools could lead to substantial clinical benefits at population as well as individual level [31]. Furthermore, high-quality, international, and prospective studies are direly needed to confirm and expand our present findings, especially focusing on the complex effort needed to disentangle patient impact (ie secondary prevention) from subject impact (ie primary prevention), as well as moving from individual tailored approaches to collective ones [32,33]. Without being overly provocative, we suggest that controlled trials could be envisioned to identify the best management strategy for future recurrences of COVID-19 outbreaks, for instance comparing in nearby provinces or counties more vs less forceful mitigation efforts, while measuring clinical, environmental and economic consequences of such actions [34,35]. Finally, without supporting any effort at reducing acute cardiac care capabilities, it is clear that local COVID-19 epidemics could be managed by temporarily repurposing cardiovascular units devoted to elective or semi-urgent cases, especially when improvements in pollution are expected, given the expected need for intensive care management of high-risk COVID-19 patients [36,37].
4.1. Limitations
This work has several important limitations. First, being an observational retrospective study of daily institution-level data it cannot adjust for individual features (eg age, comorbidities, door to balloon or extent of multivessel disease), which may potentially impact on ACS. Second, no procedural data were obtained (eg time to admission) nor outcome data were collected (eg case fatality rate, hospital stay or other clinically relevant outcomes) [[38], [39], [40]]. Third, COVID-19 data are subject to selective reporting (eg depending on daily test rates and targets), and COVID-19-related deaths represent an adjudication challenge. Fourth, our modeling approach (multilevel Poisson regression), while established for similar analytical goals, has been challenged and may not capture all data complexities. Fifth, and most important, our results do not imply causation but simply association, and several potentially biasing effects (eg regression to the mean and confounding by unmeasured features) should be borne in mind. Finally, while forceful mitigation efforts such as lockdowns may clearly reduce pollution, some complex interactions have been reported to date, including a paradoxical increase in O3, PM10, and SO2 during lockdown in China and/or USA [35,41].
4.2. Future directions
Several avenues for future clinical practice and research can be hypothesized, based on the present study findings. First, individualized risk prediction apps could be used to predict patients at risk of clinical events based on environment, weather, and epidemiologic features. Second, in case of resurgence of COVID-19 or similarly dire infectious disease threats, temporary repurposing of cardiovascular units devoted to elective or semi-urgent cases could be considered, for instance by admitting patients with pneumonia or acute respiratory distress syndrome to coronary care units or semi-intensive cardiac care units. Third, physicians could consider informing their patients on the competing risk of COVID-19 and NSTEMI, in light of the relatively favorable changes in pollution features, without discounting the need to activate and manage STEMI proactively even in COVID-19 times.
5. Conclusions
Our observational study suggests that reductions in STEMI and NSTEMI in the COVID-19 pandemic may depend on different concomitant epidemiologic and pathophysiologic mechanisms, including changes in pollution associated with COVID-19. In particular, recent changes in STEMI may depend on COVID-19 scare or excess all cause mortality, whereas reductions in NSTEMI may also be due to beneficial reductions in NO2 emissions in the lockdown phase.
Author statement – International Journal of Cardiology
Francesco Versaci, Giuseppe Biondi-Zoccai: study design, data analysis, manuscript drafting, final approval.
Achille Gaspardone, Alessandro Danesi, Fabio Ferranti, Massimo Mancone, Enrica Mariano, Francesco L. Rotolo, Carmine Musto, Igino Proietti, Andrea Berni, Carlo Trani, Sonia Cristina Sergi, Giulio Speciale, Gaetano Tanzilli, Fabrizio Tomai, Alessandro Di Giosa, Giada Marchegiani, Enrico Romagnoli: data collection, manuscript revision for intellectual content, final approval.
Elena Cavarretta, Roberto Carnevale, Giacomo Frati: data analysis, manuscript revision for intellectual content, final approval.
Funding
None
Declaration of Competing Interest
Prof. Biondi-Zoccai has consulted for Cardionovum, Bonn, Germany, InnovHeart, Milan, Italy, Meditrial, Rome, Italy, and Replycare, Rome, Italy.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcard.2020.12.059.
Appendix A. Supplementary data
Supplementary material
References
- 1.Kulkarni P., Mahadevappa M. COVID-19 pandemic and the reduction in ST-elevation myocardial infarction admissions. Postgrad. Med. J. 2020;96:436–437. doi: 10.1136/postgradmedj-2020-137895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mafham M.M., Spata E., Goldacre R., Gair D., Curnow P., Bray M., Hollings S., Roebuck C., Gale C.P., Mamas M.A., Deanfield J.E., de Belder M.A., Luescher T.F., Denwood T., Landray M.J., Emberson J.R., Collins R., Morris E.J.A., Casadei B., Baigent C. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Versaci F., Scappaticci M., Calcagno S., Del Prete A., Romeo F., Peruzzi M., Cavarretta E., Frati G. ST-elevation myocardial infarction in the COVID-19 era. Minerva Cardioangiol. 2020 May 29 doi: 10.23736/S0026-4725.20.05343-8. [DOI] [PubMed] [Google Scholar]
- 4.Claeys M.J., Argacha J.F., Collart P., Carlier M., Van Caenegem O., Sinnaeve P.R., Desmet W., Dubois P., Stammen F., Gevaert S., Pourbaix S., Coussement P., Beauloye C., Evrard P., Brasseur O., Fierens F., Marechal P., Schelfaut D., Floré V., Hanet C. Impact of COVID-19-related public containment measures on the ST elevation myocardial infarction epidemic in Belgium: a nationwide, serial, cross-sectional study. Acta Cardiol. 2020 Jul;30:1–7. doi: 10.1080/00015385.2020.1796035. [DOI] [PubMed] [Google Scholar]
- 5.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., Brown T.S., Der Nigoghossian C., Zidar D.A., Haythe J., Brodie D., Beckman J.A., Kirtane A.J., Stone G.W., Krumholz H.M., Parikh S.A. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Filippo O., D’Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A., Secco G.G., Campo G., Gallone G., Verardi R., Gaido L., Iannaccone M., Galvani M., Ugo F., Barbero U., Infantino V., Olivotti L., Mennuni M., Gili S., Infusino F., Vercellino M., Zucchetti O., Casella G., Giammaria M., Boccuzzi G., Tolomeo P., Doronzo B., Senatore G., Grosso Marra W., Rognoni A., Trabattoni D., Franchin L., Borin A., Bruno F., Galluzzo A., Gambino A., Nicolino A., Truffa Giachet A., Sardella G., Fedele F., Monticone S., Montefusco A., Omedè P., Pennone M., Patti G., Mancone M., De Ferrari G.M. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kulkarni P., Mahadevappa M., Alluri S. COVID-19 pandemic and the impact on the cardiovascular disease patient care. Curr. Cardiol. Rev. 2020 Jun 21 doi: 10.2174/1573403X16666200621154842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavarretta E., Biondi-Zoccai G., Frati G., Versaci F. Veneto’s successful lesson for a world shocked by COVID-19: think globally and act locally. J. Cardiothorac. Vasc. Anesth. 2020;34:2346–2348. doi: 10.1053/j.jvca.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Braiteh N., Rehman W.U., Alom M., Skovira V., Breiteh N., Rehman I., Yarkoni A., Kahsou H., Rehman A. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am. Heart J. 2020;226:147–151. doi: 10.1016/j.ahj.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia S, Stanberry L, Schmidt C, Sharkey S, Megaly M, Albaghdadi MS, Meraj PM, Garberich R, Jaffer FA, Stefanescu Schmidt AC, Dixon SR, Rade JJ, Smith T, Tannenbaum M, Chambers J, Aguirre F, Huang PP, Kumbhani DJ, Koshy T, Feldman DN, Giri J, Kaul P, Thompson C, Khalili H, Maini B, Nayak KR, Cohen MG, Bangalore S, Shah B, Henry TD. Impact of COVID-19 pandemic on STEMI care: An expanded analysis from the United States. Catheter Cardiovasc Interv 2020 Aug 7: 10.1002/ccd.29154 [DOI] [PMC free article] [PubMed]
- 11.Gluckman T.J., Wilson M.A., Chiu S.T., Penny B.W., Chepuri V.B., Waggoner J.W., Spinelli K.J. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. AMA Cardiol. 2020 Aug;7 doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodríguez-Urrego D., Rodríguez-Urrego L. Air quality during the COVID-19: PM2.5 analysis in the 50 most polluted capital cities in the world. Environ. Pollut. 2020;266:115042. doi: 10.1016/j.envpol.2020.115042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020 Jul 15;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.He S., Han J. Electrostatic fine particles emitted from laser printers as potential vectors for airborne transmission of COVID-19. Environ. Chem. Lett. 2020:1–8. doi: 10.1007/s10311-020-01069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wathore R., Gupta A., Bherwani H., Labhasetwar N. Understanding air and water borne transmission and survival of coronavirus: insights and way forward for SARS-CoV-2. Sci. Total Environ. 2020;749:141486. doi: 10.1016/j.scitotenv.2020.141486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jüni P., Rothenbühler M., Bobos P., Thorpe K.E., da Costa B.R., Fisman D.N., Slutsky A.S., Gesink D. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ. 2020;192:E566–E573. doi: 10.1503/cmaj.200920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frontera A., Cianfanelli L., Vlachos K., Landoni G., Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J. Inf. Secur. 2020;81:255–259. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garg P.K., Jorgensen N., Moore K., Soliman E.Z., Heckbert S.R. Neighborhood environments and risk of incident atrial fibrillation: the multi-ethnic study of atherosclerosis. Eur. J. Prev. Cardiol. 2020;27:1440–1441. doi: 10.1177/2047487319885196. [DOI] [PubMed] [Google Scholar]
- 19.Versaci F., Biondi-Zoccai G., Giudici A.D., Mariano E., Trivisonno A., Sciarretta S., Valenti V., Peruzzi M., Cavarretta E., Frati G., Scappaticci M., Federici M., Romeo F. Climate changes and ST-elevation myocardial infarction treated with primary percutaneous coronary angioplasty. Int. J. Cardiol. 2019;294:1–5. doi: 10.1016/j.ijcard.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Biondi-Zoccai G., Frati G., Gaspardone A., Mariano E., Di Giosa A.D., Bolignano A., Dei Giudici A., Calcagno S., Scappaticci M., Sciarretta S., Valenti V., Casati R., Visconti G., Penco M., Giannico M.B., Peruzzi M., Cavarretta E., Budassi S., Cosma J., Federici M., Roever L., Romeo F., Versaci F. Impact of environmental pollution and weather changes on the incidence of ST-elevation myocardial infarction. Eur. J. Prev. Cardiol. 2020 Jun;2 doi: 10.1177/2047487320928450. 2047487320928450. [DOI] [PubMed] [Google Scholar]
- 21.Biondi Zoccai G., Landoni G., Carnevale R., Cavarretta E., Sciarretta S., Frati G. SARS-CoV-2 and COVID-19: facing the pandemic together as citizens and cardiovascular practitioners. Minerva Cardioangiol. 2020;68:61–64. doi: 10.23736/S0026-4725.20.05250-0. [DOI] [PubMed] [Google Scholar]
- 22.Protezione Civile: Emergenza Coronavirus: la risposta nazionale. Available at: http://www.protezionecivile.gov.it/attivita-rischi/rischio-sanitario/emergenze/coronavirus (last accessed on September 7, 2020).
- 23.Agenzia Regionale Protezione Ambientale (ARPA) Lazio. Available at: http://www.arpalazio.gov.it/ (last accessed on September 7, 2020).
- 24.Anderez D.O., Kanjo E., Pogrebna G., Kaiwartya O., Johnson S.D., Hunt J.A. A COVID-19-based modified epidemiological model and technological approaches to help vulnerable individuals emerge from the lockdown in the UK. Sensors (Basel) 2020;20 doi: 10.3390/s20174967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang L, Liu Z, Li H, Wang Y, Li Y, Zhu Y, Ooi MCG, An J, Shang Y, Zhang D, Chan A, Li L. The silver lining of COVID-19: estimation of short-term health impacts due to lockdown in the Yangtze River Delta region, China. Geohealth 2020 Jul 7:e2020GH000272. doi: 10.1029/2020GH000272. [DOI] [PMC free article] [PubMed]
- 26.Coker E.S., Cavalli L., Fabrizi E., Guastella G., Lippo E., Parisi M.L., Pontarollo N., Rizzati M., Varacca A., Vergalli S. The effects of air pollution on COVID-19 related mortality in northern Italy. Environ Resour Econ (Dordr) 2020 Aug;4:1–24. doi: 10.1007/s10640-020-00486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mountantonakis S.E., Saleh M., Coleman K., Kuvin J., Singh V., Jauhar R., Ong L., Qiu M., Epstein L.M. Out-of-hospital cardiac arrest and acute coronary syndrome hospitalizations during the COVID-19 surge. J. Am. Coll. Cardiol. 2020;76:1271–1273. doi: 10.1016/j.jacc.2020.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Versaci F, Gaspardone A, Danesi A, Ferranti F, Mancone M, Mariano E, Rotolo F, Musto C, Proietti I, Berni A, Trani C, Sergi SC, Speciale G, Tanzilli G, Tomai F, Di Giosa A, Marchegiani G, Calcagno S, Romagnoli E, Frati G, Biondi-Zoccai G. Impact of temporary traffic bans on the risk of acute coronary syndromes in a large metropolitan area. Panminerva Med 2020 Oct 6. doi: 10.23736/S0031-0808.20.04161-0. [DOI] [PubMed]
- 29.Salas R.N., Shultz J.M., Solomon C.G. The climate crisis and Covid-19 - a major threat to the pandemic response. N. Engl. J. Med. 2020 Jul 15 doi: 10.1056/NEJMp2022011. [DOI] [PubMed] [Google Scholar]
- 30.Calcagno S., Di Pietro R., Dei Giudici A., Del Prete A., Sciarretta S., Versaci F. Air pollution, climate changes and cardiovascular diseases: a nightmare threesome! Minerva Cardioangiol. 2020;68:282–284. doi: 10.23736/S0026-4725.20.05122-1. [DOI] [PubMed] [Google Scholar]
- 31.Nudi R, Campagna M, Parma A, Nudi A, Biondi-Zoccai G. Breakthrough healthcare technologies in the COVID-19 era: a unique opportunity for cardiovascular practitioners and patients. Panminerva Med 2020 Nov 9. doi: 10.23736/S0031-0808.20.04188-9. (Epub ahead of print). [DOI] [PubMed]
- 32.Cabrini L, Ageno W, Balbi S, Baruzzi F, Candeloro E, Capra C, Carimati F, Castiglioni B, Conti V, De Ponti R, Franchi D, Gini G, Giorgianni A, Sartorelli M, Landoni G, Locatelli D, Maffioli L, Pradella R, Severgnini P, Tozzi M, Versino M, Zocchi G, Zoli A. Caring for acute coronary syndrome and other time-sensitive medical emergencies during the coronavirus disease 2019 pandemic in Northern Italy: report from a hub centre. Minerva Cardioangiol 2020 Dec 1. doi: 10.23736/S0026-4725.20.05384-0. [DOI] [PubMed]
- 33.Saglietto A, D'ascenzo F, Cavarretta E, Frati G, Anselmino M, Versaci F, Biondi-Zoccai G, De Ferrari GM. Excess all-cause mortality during COVID-19 outbreak: potential role of untreated cardiovascular disease. Minerva Cardioangiol. 2020 Sep 30. doi: 10.23736/S0026-4725.20.05349-9. [DOI] [PubMed]
- 34.Gluckman T.J., Wilson M.A., Chiu S.T., Penny B.W., Chepuri V.B., Waggoner J.W., Spinelli K.J. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020 Aug;7 doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang L., Li M., Yu S., Chen X., Li Z., Zhang Y., Jiang L., Xia Y., Li J., Liu W., Li P., Lichtfouse E., Rosenfeld D., Seinfeld J.H. Unexpected rise of ozone in urban and rural areas, and sulfur dioxide in rural areas during the coronavirus city lockdown in Hangzhou, China: implications for air quality. Environ. Chem. Lett. 2020:1–11. doi: 10.1007/s10311-020-01028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marullo A.G., Cavarretta E., Biondi Zoccai G., Mancone M., Peruzzi M., Piscioneri F., Sartini P., Versaci F., Morelli A., Miraldi F., Frati G. Extracorporeal membrane oxygenation for critically ill patients with coronavirus-associated disease 2019: an updated perspective of the European experience. Minerva Cardioangiol. 2020:68368–68372. doi: 10.23736/S0026-4725.20.05328-1. [DOI] [PubMed] [Google Scholar]
- 37.Novelli L, Raimondi F, Ghirardi A, Pellegrini D, Capodanno D, Sotgiu G, Guagliumi G, Senni M, Russo FM, Lorini FL, Rizzi M, Barbui T, Rambaldi A, Cosentini R, Grazioli LS, Marchesi G, Sferrazza Papa GF, Cesa S, Colledan M, Civiletti R, Conti C, Casati M, Ferri F, Camagni S, Sessa M, Masciulli A, Gavazzi A, Falanga A, Da Pozzo LF, Buoro S, Remuzzi G, Ruggenenti P, Callegaro A, D’ Antiga L, Pasulo L, Pezzoli F, Gianatti A, Parigi P, Farina C, Bellasi A, Solidoro P, Sironi S, Di Marco F, Fagiuoli S; HPG23 Covid-19 Study Group. At the peak of Covid-19 age and disease severity but not comorbidities are predictors of mortality. Covid-19 burden in Bergamo, Italy. Panminerva Med 2020 Nov 27. doi: 10.23736/S0031-0808.20.04063-X.
- 38.Yang W.Y., Zhang Z.Y., Thijs L., Bijnens E.M., Janssen B.G., Vanpoucke C., Lefebvre W., Cauwenberghs N., Wei F.F., Luttun A., Verhamme P., Van Hecke E., Kuznetsova T., D’hooge J., Nawrot T.S., Staessen J.A. Left ventricular function in relation to chronic residential air pollution in a general population. Eur. J. Prev. Cardiol. 2017;24:1416–1428. doi: 10.1177/2047487317715109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kwon OK, Kim SH, Kang SH, Cho Y, Oh IY, Yoon CH, Kim SY, Kim OJ, Choi EK, Youn TJ, Chae IH. Association of short- and long-term exposure to air pollution with atrial fibrillation. Eur J Prev Cardiol 2019;26:1208–1216. [DOI] [PubMed]
- 40.Hennig F., Moebus S., Reinsch N., Budde T., Erbel R., Jöckel K.H., Lehmann N., Hoffmann B., Kälsch H., Heinz Nixdorf Recall Study Investigative Group Investigation of air pollution and noise on progression of thoracic aortic calcification: results of the Heinz Nixdorf recall study. Eur. J. Prev. Cardiol. 2020;27:965–974. doi: 10.1177/2047487319854818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shakoor A., Chen X., Farooq T.H., Shahzad U., Ashraf F., Rehman A., Sahar N.E., Yan W. Fluctuations in environmental pollutants and air quality during the lockdown in the USA and China: two sides of COVID-19 pandemic. Air Qual. Atmos. Health. 2020:1–8. doi: 10.1007/s11869-020-00888-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material