Abstract
Long-term care facilities (LTCFs), retirement homes (RHs), and other congregate care settings in Canada and worldwide have experienced significant COVID-19 outbreaks. As a health system response, our acute care hospital in Toronto, Ontario, Canada, developed and mobilized an onsite Infection Prevention and Control (IPAC) SWAT team (IPAC-SWAT) to regional settings on outbreak and implemented a strategy of support through education, training, and engagement.
Between April 28, 2020, and June 30, 2020, IPAC-SWAT assessed 7 LTCFs and 10 RHs for IPAC preparedness and actively managed 10 of 13 COVID-19 outbreaks (LTCF n=5; RH n=5). IPAC-SWAT strategies were multi-interventional and intended to mitigate further viral transmission or prevent outbreaks. Dedicated training of local “IPAC champions” was facilitated at 7 sites (LTCF = 5; RH = 2) using a “train-the-trainer” approach to promote local knowledge, autonomy, and site-led audits and feedback.
Keywords: IPAC, COVID-19, coronavirus, long-term care, outbreak, champion
Following Infection Prevention and Control (IPAC)-SWAT interventions, outbreaks were declared over at a mean of 20.6 days (range = 7-43). After 80 days following cessation of outbreaks (range = 80-160), no new COVID-19 transmission occurred in the 13 settings with previous incidence. No positive cases occurred in the 4 settings without initial outbreaks after 110 days following initial assessment (range = 110-116). Anonymous surveys were sent to all 17 supported sites 60 days postintervention. Among responders, 93.5% (29/31) felt IPAC-SWAT improved their ability to manage their COVID-19 outbreak and benefited from onsite support.
The creation and implementation of an IPAC-SWAT team mobilized to long-term care facilities (LTCFs) and retirement homes (RHs) during the COVID-19 pandemic was a successful health system initiative to manage institutional outbreaks and promote preparedness through education and training. It is hoped that the development of local IPAC knowledge and leadership through training of IPAC champions will additionally create a sustainable model of best routine IPAC practices and local independence for potential further waves of COVID-19.
Problem and Significance
Widespread COVID-19 outbreaks have occurred in LTCFs, RHs, and other congregate care settings in Canada and worldwide. Resident and environmental vulnerabilities, lack of supplies, staff shortages, and inadequate infection control/surveillance practices make these settings susceptible to outbreaks and rapid viral transmission.1, 2, 3, 4 As with other infectious diseases, the elderly population is particularly susceptible to severe coronavirus disease.
As of September 24, 2020, a total of 147,753 cases of COVID-19 have occurred in Canada, with 48,496 in Ontario.5 , 6 Within Ontario, 339 LTCFs have experienced outbreaks, with 64.5% (1829/2836) of all deaths occurring in LTCFs.7 In response to these outbreaks, the Government of Ontario requested that acute care hospitals provide LTCFs with Infection Prevention and Control (IPAC) assistance. Our community teaching hospital in Toronto, Ontario, Canada, created and mobilized an onsite IPAC “SWAT” team (IPAC-SWAT) to LTCFs and RHs to actively manage COVID-19 outbreaks and promote sustainable IPAC practices through engagement, education, and training.
Innovation
In April 2020, a strategy team led by a hospital vice president and the IPAC medical director initiated IPAC support to local LTCFs and RHs, aided by 2 relationship managers to facilitate engagement and communication. At the outset, 5 of 7 regionally partnered LTCFs and 5 of 10 RHs were on COVID-19 outbreak. The strategy team determined that onsite IPAC presence was urgently required. IPAC-SWAT was thus created, consisting of 11 health care professionals, led by 2 physicians and 1 nurse practitioner, to assess settings on active outbreak. Additional team members included 8 registered nurses (emergency, geriatrics, and nursing resource).
Relationship managers engaged with Toronto Public Health to determine the settings that were linked to our hospital and to understand outbreak characteristics. Sites were subsequently contacted (telephone and e-mail) to offer IPAC-SWAT onsite assessments, using the Public Health Ontario IPAC checklist.8 The IPAC-SWAT co-leads created written guidelines for outbreak management, adopted from best practices literature and regional guidelines, which were distributed to partnered homes to inform interventions. IPAC-SWAT was initially deployed to settings in greatest need of support based on the duration and size of outbreak.
Implementation
Prior to deployment, IPAC-SWAT team members were trained on appropriate hand hygiene practices, donning and doffing of personal protective equipment (PPE), and fundamentals of COVID-19. IPAC-SWAT used its own PPE supplies consisting of level 1 procedure masks, face shields, and alcohol-based hand rub. Gowns and gloves were only used for direct patient care. Universal masking was practiced in all settings. N95 respirators were not used by any IPAC-SWAT members.
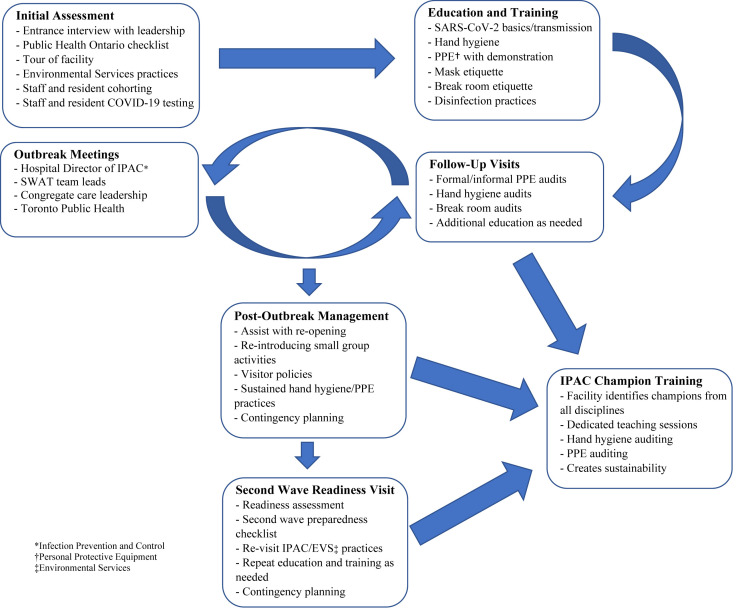
Between April 28, 2020, and June 30, 2020, IPAC-SWAT assessed 7 LTCFs and 10 RHs on IPAC practices and preparedness. Active outbreak management was provided to 10 of 13 settings (LTCF n = 5; RH n = 5) with COVID-19 outbreaks. One LTCF declined outbreak assistance and 2 RH outbreaks were over before IPAC-SWAT assessment. The strategies implemented were multi-interventional and aimed at mitigating further transmission or preventing outbreaks (Figure 1 ). In all settings, IPAC-SWAT provided formal education or training to all available staff regarding COVID-19 epidemiology, hand hygiene, mask and eye protection, PPE donning and doffing, and cleaning of shared medical equipment.
Fig. 1.
Multidimensional interventions by IPAC-SWAT to LTCFs and RHs during the COVID-19 pandemic. A downloadable PDF of this form is available at www.sciencedirect.com.
Strategy of support and interventions provided to LTCFs and RHs to aid COVID-19 outbreak management and preparedness through engagement, education, and training with a strong focus on sustainability of best IPAC practices through training of IPAC champions.
Assessment of disinfection practices and education and training were additionally provided to Environmental Services (EVS) managers and staff. Our hospital formally deployed EVS supervisors and cleaners in 5 outbreak settings (LTCF n = 2; RH n = 3) because of inadequate staffing, inappropriate disinfectants and technique, and lack of knowledge and training.
In addition to onsite visits, regular virtual “huddles” were conducted for sites on outbreak, which included members from the hospital IPAC team, LTCFs and RHs, and Toronto Public Health. Huddles were focused on tenets of outbreak management and aimed to promote relationship building and collaboration. In nonoutbreak settings, 1 or more huddles occurred after the initial IPAC-SWAT visit to clarify any questions from the site management team and to support outbreak preparedness.
To promote sustainability of best IPAC practices, dedicated training of “IPAC champions” was encouraged and facilitated using a “train the trainer” approach at 7 sites (LTCF = 5; RH = 2). Relevant guidelines and audit tools were created by IPAC-SWAT and distributed to site leadership. IPAC champions included personal support workers, nurses (across all shifts), maintenance, housekeeping, and dietary staff. IPAC champions were taught to audit compliance with hand hygiene, PPE donning and doffing, cleaning of shared medical equipment, and staff-room behaviors, including physical distancing. Regular meetings between site leadership and IPAC champions were encouraged with audit data to be used to inform future interventions.
Finally, between August 24 and September 21, 2020, IPAC-SWAT reassessed 16 of 17 affiliated LTCFs and RHs for future preparedness using a formal checklist auditing IPAC, EVS, Human Resources, Outbreak Management, Swabbing, and Medical Care (Supplementary Material 1). One LTCF opted to complete the checklist independently. This exercise was intended to identify outstanding issues to prevent future outbreaks. LTCFs overall met or were actively addressing all 48 items, missing only 2 to 4 points. Nearly all RHs however had continued IPAC concerns, missing a mean of 8 points (range = 4-18). Most notably, a lack of point-of-care hand sanitizer, missing or inappropriate donning and doffing stations, and lack of eye protection in droplet and contact isolation rooms. All LTCFs and RHs were provided a report outlining written recommendations including “immediate action items.”
Evaluation
During our intervention period, 10 of 17 affiliated LTCFs and RHs were assisted with outbreak management by IPAC-SWAT, commonly defined as a single resident case or ≥2 staff cases of COVID-19 (without clear community spread). Mean outbreak duration in these facilities was 46.3 days (range = 14-82). Following IPAC-SWAT interventions, outbreaks were declared over at a mean of 20.6 days (range = 7-43).
Relationships and close communication with all partnered homes have continued following initial interventions. After 80 days following cessation of outbreaks (range = 80-160), no new COVID-19 transmission occurred in the 13 settings with previous cases. The 4 sites without initial outbreaks likewise had no positive cases after 110 days following initial IPAC-SWAT assessment (range = 110-116).
Anonymous surveys were sent to all 17 partnered LTCFs and RHs for IPAC-SWAT feedback 60 days postintervention. Medical directors, directors of care, administrators, general managers, and IPAC leads across all sites were provided the survey. Among 31 of 37 responses, 93.5% (29/31) felt IPAC-SWAT improved their ability to manage their COVID-19 outbreak, and they benefited from onsite training and education. Regarding virtual huddles, 83.9% (26/31) believed these discussions improved the ability of the site to manage. Overall, all responders (100%; 31/31) felt the support provided from our hospital-based IPAC team positively impacted their LTCF or RH.
Comments
The creation and implementation of a hospital-based IPAC strategy and IPAC-SWAT team, mobilized to LTCFs and RHs during the COVID-19 pandemic, was a successful health system initiative to manage institutional outbreaks and promote preparedness through education, training and resource provision. Sites were receptive and appreciative of IPAC interventions, and this engagement policy has created community partnerships for ongoing support during this pandemic. The IPAC-SWAT outreach program and training of dedicated IPAC champions is ongoing and deemed imperative to promote local knowledge and autonomy. Engagement of multidisciplinary health care staff is hoped to encourage best routine IPAC practices. Site-led audits by trained IPAC champions will allow for trends of compliance and provide a platform for further education and discussion, which is expected to create a sustainable IPAC model for potential further waves of COVID-19.
The pragmatic innovation described in this article may need to be modified for use by others; in addition, strong evidence does not yet exist regarding efficacy or effectiveness. Therefore, successful implementation and outcomes cannot be assured. When necessary, administrative and legal review conducted with due diligence may be appropriate before implementing a pragmatic innovation.
Acknowledgments
We would like to thank Stacey Daub for her exceptional leadership and innovation as well as Maja McGuire for her clinical expertise and oversight.
Footnotes
The authors declare no conflicts of interest.
Supplementary Material 1. Long-Term Care Facility (LTCF) and Retirement Home (RH) COVID-19 Infection Prevention and Control (IPAC) “Second Wave” Preparedness Checklist
This checklist is based on the framework produced by Ontario Health. It will be used to conduct preparedness assessments at both Long-Term Care and Retirement Homes and in the future to support provincial and regional decisions and supports.
IPAC
-
❑
All recommendations made in the IPAC Assessment Report and/or previously identified Public Health Ontario checklist deficiencies addressed
-
❑
Staff and physicians receiving ongoing IPAC training and education
-
❑
Personal protective equipment (PPE) donning and doffing videos have been provided to staff
-
❑
PPE donning and doffing posters are up on the walls
-
❑
Appropriate use of PPE is followed and observed (universal mask use for all staff with goggles or visors for direct resident care and interactions)
-
❑
IPAC champions have been identified and have received dedicated training
-
❑
IPAC champion checklists have been created and regular auditing being completed
-
❑
Active screening in place for all staff twice daily
-
❑
Residents are being actively screened with temperatures checked twice daily
-
❑
Dining set up appropriately with physical distancing of at least 6 feet among residents and cohorting of residents
-
❑
Visitor policy in place
-
❑
Laboratory technicians visitation policy in place
-
❑
Diagnostic imaging technicians visitation policy in place
PPE
-
❑
Understanding of appropriate PPE with regular auditing of compliance
-
❑
48-h supply of gown on hand (disposable or launderable) based on calculated burn-rate
-
❑
Face shields or goggles are being used for all resident interactions with adequate supplies (plan for reusables in place)
-
❑
Universal use of surgical masks with adequate supply
-
❑
Gloves supply in different sizes available
-
❑
Hand sanitizer available at point of care
-
❑
Appropriate PPE stocked or supply chain in place
-
❑
Understanding of the Ontario Health request process
Environmental Services (EVS)
-
❑
Hospital-grade cleaning products being used with appropriate disinfectant contact time being adhered to
-
❑
High-touch surfaces being cleaned at increased frequency and minimum twice daily
-
❑
Manager or supervisor with outbreak management knowledge and training
-
❑
Sufficient ratio of EVS clearers to residents
Outbreak Management
-
❑
Tracking sheet for line lists and positive cases set up
-
❑
Cohorting plan for residents
Notes (Infection Prevention and Control):
Human Resourcing
-
❑
Emergency staffing plan and recruitment strategy in place
-
❑
Staff supports in place (eg, mental health resources, wellness support, appreciation)
-
❑
Staffing plan in place (clinical and support services)
-
❑
One location per staff person policy during outbreak in place
Notes (Human Resourcing):
Partnerships and Sustained Operations
Swabbing
-
❑
Nasopharyngeal (NP) swabs available
-
❑
Plan to acquire NP swabs if required
-
❑
Understanding of the swabbing process (eg, where to send the swabs)
-
❑
Physicians or nurses identified and trained to perform the swabbing
-
❑
Family physician consent to order swabs (RH only)
-
❑
Mobile swab team access lines are communicated
Medical Care
-
❑
Medical director or attending physician has plans to provide on-site care when appropriate
-
❑
Administration to plan for policy whether to allow on-site cross-coverage of physicians between facilities prior to outbreak
-
❑
Vaccination plan in place (influenza, pneumococcal, oseltamivir, updated creatinine)
-
❑
General internal medicine and palliative care 24/7 consult lines are communicated
-
❑
Advance care plans are in place for all residents
-
❑
Adequate supply of diagnostic equipment (blood pressure devices) for cohorting during outbreak
-
❑
STAT laboratory testing availability addressed
-
❑
External medical consultants to plan for continuation of on-site visits when possible (psychiatry, dermatology, wound care, dentistry, optometry, audiology, physio, chiropody, etc)
-
❑
Emergency supplies box ramped up to manage COVID-19 symptoms and to minimize transfers to emergency department
-
❑
Prescription order sets and readily available references for COVID-19 symptom management and end-of-life care in place
-
❑
Death pronouncement protocol—plan in place during outbreak
Notes (Partnerships and Sustained Operations):
References
- 1.McMicheal T.M., Currie D.W., Clark S. Epidemiology of COVID-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quigley D.D., Dick A., Agarwal M. COVID-19 Preparedness in nursing homes in the midst of the pandemic. J Am Geriatr Soc. 2020;68:1164–1166. doi: 10.1111/jgs.16520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zoutman D.E., Ford B.D., Gauthier J. A cross-Canada survey of infection prevention and control in long-term care facilities. Am J Infect Control. 2009;37:358–363. doi: 10.1016/j.ajic.2008.10.029. [DOI] [PubMed] [Google Scholar]
- 4.Li Y., Temkin-Greener H., Gao S. COVID-19 infections and deaths among Connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68:1899–1906. doi: 10.1111/jgs.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government of Canada Coronavirus disease 2019 (COVID-19): Epidemiology update; c2020b. https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html Available at:
- 6.Government of Ontario How Ontario is responding to COVID-19. https://www.ontario.ca/page/how-ontario-is-responding-covid-19#section-0 Available at:
- 7.Public Health Ontario Daily Epidemiologic Summary: COVID-19 in Ontario: January 15, 2020 to September 24, 2020. Toronto, ON: Queen’s Printer for Ontario, 2020. https://www.publi-chealthontario.ca/-/media/documents/ncov/epi/2020/covid-19-daily-epi-summary-re-port.pdf?la=en Available at:
- 8.Public Health Ontario COVID-19: Infection Prevention and Control Checklist for Long-Term Care and Retirement Homes. Toronto, ON: Queens’s Printer for Ontario, 2020. https://www.publichealthontario.ca/-/media/documents/ncov/ipac/covid-19-ipack-checklist-ltcrh.pdf?la=en Available at: