Highlights
-
•
This is the first few studies exploring the perceptions of Bangladeshi students towards the COVID-19 pandemic.
-
•
Female students showed higher stress levels, greater anxiety symptoms and, depressive symptoms.
-
•
Younger students had a greater psychological impact due to COVID-19 than senior students.
-
•
The psychological impact is higher among those students who have at least one COVID-19 like symptoms.
Keywords: Mental health, Student, Perception, COVID-19, Bangladesh
Abstract
Although the COVID-19 pandemic triggered commination on both physical and mental wellbeing since its outbreak, the impact of the pandemic on mental health difficulties among Bangladeshi students is still lack in substantial evidence. The study aimed to explore such an impact on mental health among Bangladeshi students and their perception towards the COVID-19 pandemic. A web-based cross-sectional study was conducted among 589 students from Bangladesh in between April 29th to 7th May 2020. Data was collected by using an online questionnaire on demographic status, perceptions towards COVID-19, and mental health symptoms by using the Depression, Anxiety and Stress Scale (DASS 21). About 26.66% and 61.97% of students reported mild to extremely severe anxiety symptoms, and depressive symptoms, respectively, and 57.05% reported mild to extremely severe levels of stress. Multivariate logistic regression reported that students’ age, gender, family income, residence, and family size are associated with mental health difficulties. Negative perceptions on the effect of the pandemic on life events, mental health, disruptions in education, and health care system, existing physical health conditions, and COVID-19 like symptoms were significantly associated with poor mental outcomes. It is suggested that students' mental health difficulties should be monitored to provide adequate support and services during this ongoing pandemic.
1. Introduction
The novel coronavirus disease (COVID-19) was first identified at the end of 2019 in Wuhan City, Hubei Province, China (Odriozola-González et al., 2020, Temsah et al., 2020) and became a universal threat within a few weeks (Shen et al., 2020), leading to the declaration of a global pandemic by the World Health Organization (WHO) on 11 March 2020 (Kapasia et al., 2020). The COVID-19 pandemic triggered a combination of both physical and mental wellbeing since its first outbreak (Cooper et al., 2020, Hasan and Bao, 2020). The pandemic is not only causing deaths worldwide, but also initiating negative consequences on mental health, and worsens pre-existing conditions such as anxiety, depression, stress, etc. (Khan et al., 2020, Wang et al., 2020c, Xiao, 2020).
The COVID-19 case fatality rate has been increasing rapidly in Bangladesh since the first identification of the first case in early March 2020 (IEDCR, 2020). In order to flatten the curve, on March 16, 2020, the Government of Bangladesh restricted the active functioning of all educational institutions and public gatherings (Banna et al., 2020), and on March 25, 2020, Bangladesh declared a lockdown measure suggesting stay at home (Anwar, Nasrullah, & Hosen, 2020). To follow this procedure, citizens, as well as students, were bound to stay at home for a long period (Khan et al., 2020), which might have heightened the risk of developing mental health difficulties (Ravesloot et al., 2016). The high prevalence of negative mental health issues in Bangladeshi students has already been reported in different contemporary studies (Anjum et al., 2019, Hossain et al., 2019, Sayeed et al., 2020). A recent study conducted among Bangladeshi college and university students during the COVID-19 pandemic has also described a higher prevalence of depressive symptoms, anxiety, stress symptoms and identified that COVID-19 like symptoms and fear of infection were two strong predictors of this high pervasiveness of mental consequences (Khan et al., 2020). Another study in Bangladesh during the COVID-19 pandemic found a significant correlation between negative perception and poor mental health (Banna et al., 2020). To the best of our knowledge, very few studies have been conducted in Bangladesh exploring the mental health of home-quarantined students (Khan et al., 2020), though we need more evidence to describe the mental health difficulties of Bangladeshi students during this pandemic to address this research gap adequately. Additionally, very few studies have reported the perception of students towards the pandemic and the potential association with mental health difficulties. This study aimed to explore the mental health difficulties of Bangladeshi students and their perception towards the COVID-19 pandemic.
2. Methods
2.1. Study type & population
This was a cross-sectional web-based survey among Bangladesh students during the COVID-19 pandemic. 50% response rate, 5% significance level, and 5% margin of error were used to calculate the required sample size of 385 to achieve 80% power. We received responses from 589 students and we included all in the analysis.
2.2. Data collection
The survey was conducted from April 29th to 7th May 2020. Since a community-based sampling survey was not feasible during this period, data were collected online. A structured questionnaire link using ‘Google form’ was sent to students via social media using snowball sampling. Eligibility criteria included the ability to read Bangla, being a student, staying at home during the pandemic, and living in Bangladesh for the duration of the government-mandated lockdown.
2.3. Procedure
The questionnaire was provided in native Bangla. The survey questionnaire was first written in English and then translated into Bangla. We did the translation first by a bilingual translator, checked by an independent researcher, and then back-translated by another bilingual translator to check the consistencies and avoiding any bias. The questionnaire was piloted in a small, randomly selected group of online users to confirm clarity and understanding. The online survey provided a brief description of the study and nature of the study, eligibility requirements, procedures, e-consent form, and how to answer the questionnaire. Clicking on the survey link directed the respondents automatically to the study summary and electronic informed consent page. An electronic consent form was collected from all participants. The parent’s/ legal guardian’s electronic consent form was collected in case of under 18 participants. This study followed the guidance of the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines (Eysenbach, 2004), as well as the 2013 revision of the Helsinki Declaration (Williams, 2008).
2.4. Survey questions
The questionnaire was divided into four sections: demographics, perception towards COVID-19, reported physical symptoms, and mental health assessments. The self-rated survey approximately took fifteen minutes, and there was no compensation for the participants. Participants were asked for their perceptions on the pandemic disrupting normal life events, health care systems, mental health, challenges in education, and concern on existing physical problems. A symptom checklist (fever, headache, dry cough, breathing difficulties, sore throat, and fatigue, etc.) within the last 14 days was used. Mental health was assessed using a validated Bangla version of the Depression, Anxiety, and Stress Scale (DASS-21) (Alim et al., 2020), with scores measured according to previous research (Banna et al., 2020, Wang et al., 2020a). The DASS-21 contains 21 total self-report items distributed among three factors aimed at evaluating the negative emotion of depressive symptoms, anxiety symptoms and stress symptoms experienced during the last week (Lovibond & Lovibond, 1995). Every item score is on a Likert scale of four points ranging from zero to three, with higher scores suggesting a higher frequency or severity of the item. The total scores for depressive symptoms were categorized into normal (0–9), mild depression (10–12), moderate depression (13–20), severe depression (21–27), and extremely severe depression (28–42) (Banna et al., 2020, Wang et al., 2020a). The total anxiety subscale score was categorized into normal (0–6), mild anxiety (7–9), moderate anxiety (10–14), severe anxiety (15–19), and extremely severe anxiety (20–42) (Banna et al., 2020, Wang et al., 2020a). The total stress subscale score was categorized into normal (0–10), mild stress (11–18), moderate stress (19–26), severe stress (27–34), and extremely severe stress (35–42) (Banna et al., 2020, Wang et al., 2020a). The Bangla DASS-21 has proven to be a reliable and relevant test for the assessment of mental health in the Bangladeshi population (Alim et al., 2015, Khan et al., 2020, Sadiq et al., 2019). The Cronbach’s alpha coefficient for this study was 0.92 for the DASS-21, indicating acceptable internal consistency.
2.5. Statistical analysis
Chi-square test, Pearson Correlation Matrix (PCM), and Hierarchical Cluster Analysis (CA) were applied to know the association between variables. A multivariate logistic regression model was fitted to see the effect of all variables on the mental health condition. Multicollinearity was checked with the variance inflation factor (VIF). The final model selection was done by using Hosmer and Lemeshow goodness of fit test and the significance of variables were assessed with the Wald test. Odds ratio (OR) and 95% confidence interval (CI) were used to represent the model. All analyses were done using the statistical software SAS 9.3 version, and SPSS 23.0 version. P value < 0.05 with two-tailed tests was considered throughout the analysis.
3. Results
3.1. Demographic characteristics
Two-thirds (65.7%) of the students were male. Nearly half (45%) were under or equivalent to the age of 22 years, 81.0% were undergraduate students, and 60.6% lived in rural areas. Most of the participants (71.6%) were Muslims and almost half (45.7%) of the participants’ families comprised of 4 or more members. The prevalence of mental health symptoms varied among subgroups. The rates of different stress levels were significantly higher in females (79.7%), aged 22 years or less (70.9%), and having under five children (59.8%) and adults over 50 years of age (59.7%) in the household. Varied rates of anxiety symptoms were reported in females (40.6%), aged 22 years or less (38.5%), secondary level education (83.3%) and urban residents (35.3%). The higher prevalence of depressive symptoms was significantly associated with females (72.8%), secondary education (2%) and families having under five children (64.0%) (Table 1 ).
Table 1.
Prevalence of stress, anxiety and depressive symptoms across socio-demographic variables (n = 589).
| Parameters | Category | % in the sample | % Stress (>10) | % Anxiety (>6) | % Depression (>9) |
|---|---|---|---|---|---|
| All | 57.0 | 26.7 | 62.0 | ||
| Age (years) | ≤22 | 45.0 | 70.9*** | 38.5*** | 65.3 |
| >22 | 55.0 | 45.7 | 17.0 | 59.3 | |
| Gender | Male | 65.7 | 45.2*** | 19.4*** | 56.3*** |
| Female | 34.3 | 79.7 | 40.6 | 72.8 | |
| Marital status | Married | 2.0 | 83.3 | 33.3 | 83.3 |
| Unmarried | 98.0 | 56.5 | 26.5 | 61.5 | |
| Education level | Secondary | 2.0 | 100** | 83.3*** | 100* |
| Higher secondary | 11.2 | 47.0 | 24.2 | 66.6 | |
| Undergraduate | 81.0 | 56.2 | 24.9 | 61.2 | |
| Graduate and higher | 5.8 | 73.5 | 35.3 | 50.0 | |
| Monthly income | ≤27,000 BDT | 51.8 | 56.1 | 30.8* | 61.0 |
| >27,000 BDT | 48.2 | 58.1 | 22.2 | 63.0 | |
| Residence | Rural | 60.6 | 55.7 | 21.0*** | 62.7 |
| Urban | 39.4 | 59.1 | 35.3 | 60.8 | |
| Religion | Muslim | 71.6 | 56.6 | 27.5 | 64.7 |
| Hindu | 27.3 | 59.0 | 25.5 | 55.9 | |
| Others† | 1.0 | 33.3 | 0.00 | 33.3 | |
| Family size | ≤ 4 | 54.3 | 59.4 | 29.1 | 60.0 |
| > 4 | 45.7 | 54.3 | 23.8 | 64.3 | |
| Child < 5 in family | Yes | 11.4 | 59.8*** | 26.6 | 64.0** |
| No | 88.6 | 35.8 | 26.9 | 46.3 | |
| Elderly > 50 in family | Yes | 80.0 | 59.7* | 26.1 | 62.4 |
| No | 20.0 | 46.6 | 28.8 | 60.2 |
p < 0.001, **p < 0.01, *p < 0.05.
Others included Buddhists, Christians etc. ‡Others included farmers, fisherman etc.
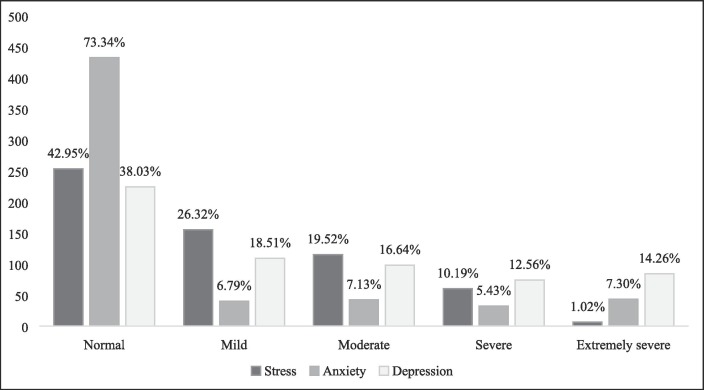
3.2. Prevalence of stress level, anxiety symptoms, and depressive symptoms
Among the participants, 57.05% had mild to extremely severe symptoms of stress. One-fourth (26.6%) of participants reported mild to extremely severe anxiety symptoms; among them, 7.13% had moderate symptoms of anxiety and 5.43% and 7.30% had severe and extremely severe anxiety symptoms. Over half of the respondents (61.97%) reported mild to extremely severe depressive symptoms, including mild (18.51%), moderate (16.64%), severe (12.56%), and extremely severe (14.26) levels (Fig. 1 ).
Fig. 1.
Severities of stress, anxiety and depression symptoms of the participants by using DASS-21 scale (n = 598).
3.3. Student’s perception towards the COVID-19
Nearly half of students (42.8%) claimed that their lives were disrupted ‘a lot’ by the COVID-19 pandemic. More than one third (37.0%) believed that this pandemic had a ‘medium’ mental health effect on them. More than half of the students (57.0%) believed the COVID-19 would disrupt the health care system. For this outbreak in Bangladesh, a majority (84.2%) predicted that “the worst is yet to come”. A majority (80.8%) also believed that their education would have a negative effect due to the pandemic. Over half (58.1%) were also worried that the pandemic would adversely affect their mental health due to a current physical health problem. Negative perceptions on this pandemic were significantly correlated with worse mental health scores (Table 2 ).
Table 2.
Prevalence of stress, anxiety and depressive symptoms based on perceptions of COVID-19 (n = 589).
| Perceptions | Response | % in the sample | % Stress (>10) | % Anxiety (>6) | % Depression (>9) |
|---|---|---|---|---|---|
| 1 | A lot | 42.8 | 59.1** | 29.0 | 63.9** |
| Medium | 34.1 | 52.7 | 24.9 | 63.7 | |
| Some | 19.9 | 65.8 | 25.6 | 61.5 | |
| Not at all | 3.2 | 21.1 | 21.1 | 21.1 | |
| 2 | A lot | 23.0 | 63.6*** | 39.3*** | 65.0*** |
| Medium | 37.0 | 61.9 | 28.4 | 73.4 | |
| Some | 29.4 | 57.8 | 22.0 | 59.0 | |
| Not at all | 9.8 | 20.7 | 3.4 | 20.7 | |
| 3 | I think so | 57 | 63.7*** | 23.2 | 65.5* |
| I don’t think so | 26 | 40.5 | 30.7 | 53.6 | |
| Don’t know | 17 | 60.0 | 32.0 | 63.0 | |
| 4 | The worst is behind us | 4.2 | 59.1 | 25.2 | 65.1 |
| The worst is yet to come | 84.2 | 60.0* | 40.0* | 56.0*** | |
| Covid-19 is/will not be a major problem for Bangladesh | 2.7 | 25.0 | 12.5 | 12.5 | |
| Don’t know | 8.8 | 46.2 | 38.5 | 50.0 | |
| 5 | Yes | 80.8 | 62.2*** | 29.0* | 69.1*** |
| No | 14.1 | 31.3 | 13.3 | 36.1 | |
| Somewhat | 5.1 | 46.7 | 26.7 | 20.0 | |
| 6 | Yes | 58.1 | 61.4*** | 23.7*** | 70.8*** |
| No | 11.5 | 26.5 | 11.8 | 20.6 | |
| Somewhat | 30.4 | 63.3 | 38.0 | 60.9 | |
1. How much has your life been disrupted by the COVID-19 pandemic?
2. How much the COVID-19 pandemic has negatively affected your mental health?
3. Do you think the country’s healthcare system will be overrun and people will not be able to get medical care?
4. Which of the following do you suspect about the trajectory of COVID-19 in Bangladesh?
5. Do you think COVID-19 will have a negative impact on your education?
6. Do you think COVID-19 will have a negative impact on the existing health conditions which effects on mental health?
p < 0.001, **p < 0.01, *p < 0.05.
In this study, the Pearson correlation coefficient matrix was used to describe the relationship among the student's perception in between towards the COVID-19 pandemic. Almost all the perceptions of participants towards COVID-19 were positively correlated in between (Table 3 ).
Table 3.
Pearson correlation coefficient matrix for perception of students towards the COVID-19 pandemic.
| P1 | P2 | P3 | P4 | P5 | P6 | |
|---|---|---|---|---|---|---|
| P1 | 1 | |||||
| P2 | 0.297** | 1 | ||||
| P3 | 0.241** | 0.187** | 1 | |||
| P4 | 0.059 | 0.003 | 0.252** | 1 | ||
| P5 | 0.076 | 0.215** | 0.189** | 0.237** | 1 | |
| P6 | 0.244** | 0.139** | 0.349** | 0.088* | 0.200** | 1 |
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.05 level (2-tailed).
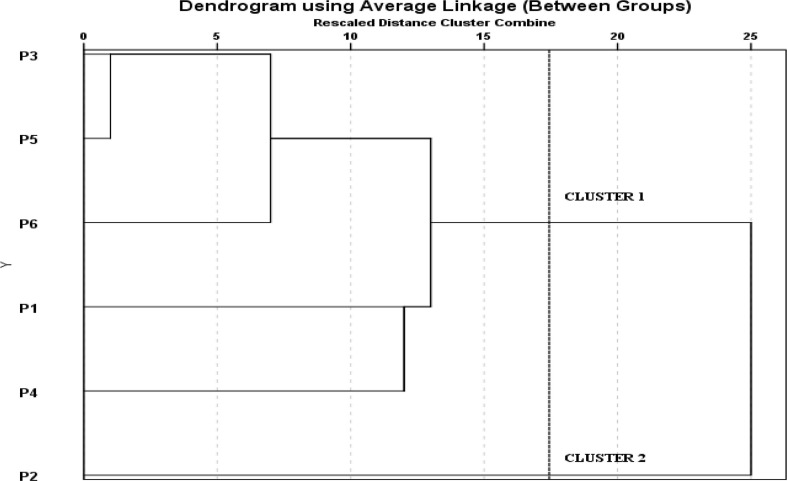
Cluster analysis (CA) divided perceptions into clusters/groups based on the reaction of students towards COVID-19. CA results are divided into two main clusters or groups. Cluster 1 was formed with five perceptions (P1, P3-P6), and Cluster 2 was formed with only one perception (P2) (Fig. 2 ).
Fig. 2.
Dendrogram clustering of students perceptions towards the COVID-19 pandemic.
3.4. Association between COVID-19 related symptoms and social stressors, and mental health of students
About 30% of the participants had at least one COVID-19 like symptom. The stress level was significantly higher in individuals with a single symptom (61.5%) and more than one symptom (74.8%). The stress level was also significantly associated with those who contacted the confirmed case of COVID-19 (84.6%) or suspected case (71.4%). Anxiety symptoms were higher in respondents with a single symptom (37.5%) and more than one symptom (48.8%). Anxiety symptoms were also associated with those who were quarantined in the last 14 days (53.8%) and contacted the confirmed case of COVID-19 (76.9%). No significant association was found between depressive symptoms and COVID-19 related social stressors and symptoms (Table 4 ).
Table 4.
Association among perceived COVID-19 related symptoms and social stressors, and mental health impact (n = 589).
| Parameter | % in the sample | % Stress (>10) | % Anxiety (>6) | % Depression (>9) |
|---|---|---|---|---|
| COVID-19 like symptom# | ||||
| Single symptom | 16.3 | 61.5*** | 37.5*** | 59.4 |
| More than one symptom | 20.9 | 74.8 | 48.8 | 69.9 |
| No symptom | 62.8 | 50.0 | 16.5 | 60.0 |
| Recent quarantine in last 14 days | ||||
| Yes | 2.2 | 69.2 | 53.8* | 84.6 |
| No | 97.8 | 56.8 | 26.0 | 61.5 |
| Contact with individuals with confirmed cases of COVID-19 | ||||
| Yes | 4.4 | 84.6** | 76.9*** | 61.5 |
| No | 95.6 | 55.8 | 26.8 | 62.0 |
| Contact with individuals with suspected COVID-19 or infected materials | ||||
| Yes | 11.9 | 71.4* | 24.3 | 72.9 |
| No | 88.1 | 55.1 | 27.0 | 60.5 |
Symptoms including Fever for at least one day, Headache, Dizziness, Myalgia, Cough, Runny Nose, Breathing Difficulty, etc.
p < 0.001, **p < 0.01, * p < 0.05.
3.5. Impact of socio-demographic variables on mental health
Multivariate logistic regression models fitted between demographic characteristics and students’ mental health outcomes. A Hosmer and Lemeshow test statistic of stress (χ2 = 5.28, p = 0.51), anxiety (χ2 = 12.30, p = 0.14) and depressive symptoms (χ2 = 13.24, p = 0.10) indicated a good fit the model with the observed data. Regarding stress, after adjusting for other confounding variables, age and gender were significantly associated with stress. The results indicated that > 22 years of age, in contrast to ≤ 22 years, was a protective factor against stress level (OR = 3.01; CI: 2.07–4.35). Male respondents had lower odds of stress level (OR = 0.22; CI: 0.14–0.33) than females. For anxiety, after adjusting for other confounding variables, age, gender, education, family income, residence, and family size were significantly associated. Age ≤ 22 years (vs. > 22 years; OR = 4.46, CI: 2.80–7.11), secondary level education (vs. graduate level; OR = 11.03; CI: 1.81–67.33), family monthly income ≤ 27000 BDT (vs. > 27000 BDT; OR = 2.56; CI: 1.631–4.00) and, having family size ≤ 4 (vs. > 4; OR = 1.89; CI: 1.15–3.06) had the higher odds of anxiety symptoms. Male (vs. female; OR = 0.29; CI: 0.19–0.46) and rural residence (vs. urban; OR = 0.31; CI: 0.20–0.49) had the lower odds of anxiety symptoms. For depressive symptoms, age, gender, education, family income, family size, residence, and under 5 children were significantly associated after controlling for other confounding variables. Age ≤ 22 years (vs. > 22 years; OR = 4.49, CI: 2.81–7.17), secondary level education (vs. graduate level; OR = 11.15; CI: 1.82–68.21), family monthly income ≤ 27000 BDT (vs. > 27000 BDT; OR = 2.62; CI: 1.65–4.18) and having family size ≤ 4 (vs. > 4; OR = 1.91; CI: 1.16–3.15) had the higher odds. Male (vs. female; OR = 0.29; CI: 0.18–0.45), rural residence (vs. urban; OR = 0.31; CI: 0.21–0.49), and having no under 5 children (vs. yes; OR = 0.43; CI: 0.21–0.87) had the lower odds of depressive symptoms (Table 5 ).
Table 5.
Effects of socio-demographic variables on mental health (n = 589).
| Variables | Stress | Anxiety | Depression |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age group (ref.: >22 years) | |||
| ≤22 | 3.01 (2.07–4.35)*** | 4.46(2.80–7.11)*** | 4.49(2.81–7.17)*** |
| Gender (ref.: female) | |||
| Male | 0.22 (0.14–0.33)*** | 0.29 (0.19–0.46)*** | 0.29(0.18–0.45)*** |
| Marital status (ref: no) | |||
| Yes | 2.89(0.56–14.95) | 1.38(0.34–5.59) | 1.39 (0.35–5.65) |
| Education (ref.: graduate and higher) | |||
| Secondary | – | 11.03(1.81–67.33)** | 11.15(1.82–68.21)*** |
| Higher secondary | – | 0.428(0.147–1.245) | 0.44(0.15–1.29) |
| undergraduate | – | 0.559(0.231–1.35) | 0.58(0.24–1.41) |
| Family income (ref.: >BDT) | |||
| ≤27000 | – | 2.56(1.63–4.00)*** | 2.62(1.65–4.18)*** |
| Residence (ref.: urban) | |||
| Rural | – | 0.31(0.20–0.49)*** | 0.31(0.21–0.49)*** |
| Religion (ref.: Muslim) | |||
| Hindu | 3.07(0.43–21.98) | – | – |
| Others | 2.813(0.35–20.55) | – | – |
| Family size (ref.: >4) | |||
| ≤ 4 | – | 1.89 (1.15–3.06)* | 1.91(1.16–3.15)* |
| Under 5 children (ref.: yes) | |||
| No | 1.42(0.98–2.04) | 0.42(0.20–1.88) | 0.43(0.21–0.87)* |
| Over 50 year adults (ref.: yes) | |||
| No | – | – | 0.89 (0.51–1.53) |
***p < 0.001, **p < 0.01, *p < 0.05.
OR = Odds Ratio; CI = Confidence Interval.
3.6. Impact of COVID-19 perceptions on mental health
Multivariate logistic regression models on perceptions towards COVID-19 and mental health outcomes were modeled and Hosmer and Lemeshow test for stress (χ2 = 7.06, p = 0.53), anxiety (χ2 = 14.77; p = 0.06) and depression (χ2 = 14.29, p = 0.07) showed the good fit of the data. After adjusting the confounders, perception 1, 2, and 3 were associated with stress and perception 2, and 4 with anxiety. Depressive symptoms were associated with perception 1, 4, 5, and 6. Participants who perceived that some events of life would be disrupted (OR = 5.47; CI: 1.56–19.22) had higher odds of stress level than those who believed that life would not be disrupted for the pandemic. The respondents who perceived that the COVID-19 pandemic had ‘a lot’ (OR = 6.06; CI: 2.60–14.11) or 'medium' (OR = 5.28; CI: 2.37–11.75) or 'some' (OR = 4.10; CI: 1.84–9.11) negative effect on mental health had the higher odds of stress level than those who denied any negative effect. Participants who were uncertain about the fate of the healthcare system (OR = 2.51; CI: 1.38–4.59) had higher odds of stress level than those that believed the healthcare system would withstand the pandemic. Students who believed that pandemic had ‘a lot’ (OR = 17.58; CI: 3.68–83.90) or ‘medium’ (OR = 8.73; CI: 1.87–40.89) effect on mental health had higher odds of anxiety symptoms than those who did not perceive mental health effects. Respondents who were unaware of the pandemic (OR = 9.54; CI: 1.63–55.73) had higher odds of anxiety symptoms than those who did not consider the COVID-19 pandemic as a major concern for Bangladesh. Students who agreed that COVID-19 disrupted the life events ‘a lot’ (OR = 7.66; CI: 2.25–26.08) or ‘medium’ (OR = 7.67; CI: 2.25–26.08) or ‘some’ (OR = 5.03; CI: 1.46–17.28) had higher odds of depressive symptoms than those who replied as 'not at all'. Respondents who perceived that the worst crisis of pandemic is yet to come (OR = 7.45; CI: 1.43–38.83) had higher odds of anxiety symptoms than those who did not consider the COVID-19 pandemic as a major problem for Bangladesh. Those who admitted that the COVID-19 pandemic would have a negative effect on the economy and education were more likely to have depressive symptoms (OR = 3.45; CI: 2.01–5.93) than those who denied any negative impacts. Respondents who fully disagreed that COVID-19 had no negative mental health impact on those with physical health conditions had lower chances (OR = 0.258; CI: 0.12–0.54) of depressive symptoms than those who claimed that COVID-19 would have “somewhat” negative impact (Table 6 ).
Table 6.
Effects of COVID-19 perceptions on mental health (stress, anxiety and depression).
| Parameters | Stress | Anxiety | Depression |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Perception 1 (ref.: not at all) | |||
| A lot | 3.39 (0.97–11.79) | 1.82 (0.49–6.80) | 7.66 (2.25–26.08)** |
| Medium | 3.19 (0.93–10.96) | 1.56 (0.42–5.73) | 7.67 (2.25–26.08)** |
| Some | 5.47 (1.56–19.22)** | 1.06 (0.28–3.96) | 5.03 (1.46–17.28)** |
| Perception 2 (ref.: not at all) | |||
| A lot | 6.06 (2.60–14.11)** | 17.58 (3.68–83.90)*** | – |
| Medium | 5.28 (2.37–11.75)** | 8.73 (1.87–40.89)* | – |
| Some | 4.10 (1.84–9.11)** | 6.12 (1.29–29.01) | – |
| Perception 3 (ref.: I don’t think so) | |||
| I think so | 2.19 (1.37–3.50) | 0.51 (0.30–1.06) | 0.74 (0.45–1.21) |
| Don’t know | 2.51 (1.38–4.59)* | 0.87 (0.47–1.62) | 1.13 (0.61–2.09) |
| Perception 4 (ref.: COVID-19 is/will not be a major problem for Bangladesh) | |||
| The worst is behind us | 3.09 (0.63–14.96) | 8.51 (1.27–56.76) | 5.85 (0.91–37-64) |
| The worst is yet to come | 3.44 (0.92–12.90) | 5.49 (1.01–29.69) | 7.45 (1.43–38.83)* |
| Don’t know | 2.55 (0.62–10.41) | 9.54 (1.63–55.73)* | 7.96 (1.38–45-88) |
| Perception 5 (ref.: no) | |||
| Yes | 2.51 (1.44–4.37) | 2.65 (1.26–5.58) | 3.45 (2.01–5.93)*** |
| Somewhat | 2.98 (1.08–8.26) | 2.44 (0.75–7.91) | 0.572 (0.19–1.70) |
| Perception 6 (ref.: somewhat) | |||
| Yes | 0.81 (0.52–1.27) | 0.46 (0.29–1.74) | 1.327 (0.85–2.07) |
| No | 0.53 (0.25–1.13) | 0.35 (0.13–1.60) | 0.258 (0.12–0.54)*** |
*p < 0.05; **p < 0.01; ***p < 0.001; OR = Odds Ratio; CI = Confidence Interval
1. How much has your life been disrupted by the COVID-19 pandemic?
2. How much the COVID-19 pandemic has negatively affected your mental health?
3. Do you think the country’s healthcare system will be overrun and people will not be able to get medical care?
4. Which of the following do you suspect about the trajectory of COVID-19 in Bangladesh?
5. Do you think COVID-19 will have a negative impact on your education?
6. Do you think COVID-19 will have a negative impact on the mental health of those with existing health conditions?
3.7. Impact of COVID-19 related symptoms and social stressors on mental health
Multivariate logistic regression models on COVID-19 related symptoms and social stressors, and mental health outcomes were modeled and Hosmer and Lemeshow test for stress (χ2 = 8.72, p = 0.391), anxiety (χ2 = 12.21; p = 0.124) and depression (χ2 = 11.29, p = 0.147) showed the good fit of the data. Having at least one COVID-19 related symptom (OR = 1.60; CI: 1.002–2.54) and more than one symptom (OR = 3.06; CI: 1.94–4.85) had higher odds of stress level. Individuals contacted with confirmed cases of COVID-19 had higher odds of stress level (OR = 3.99; CI: 1.29–12.35) compared to those who did not contact. Students with a single COVID-19 related symptom (OR = 3.02; CI: 1.83–4.99) and more than one symptom (OR = 4.96, CI: 3.16–7.80) were more anxious compared to those without any symptoms. The quarantined students were more anxious (OR = 3.67; CI: 1.14–11.81) than those who were not quarantined. Individuals contacted with confirmed cases of COVID-19 had higher odds of anxiety symptoms (OR = 3.17, CI: 1.41–3.30) (Table 7 ).
Table 7.
Effects of perceived COVID-19 related symptoms and social stressors on mental health.
| Variables | Stress | Anxiety | Depression |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| COVID-19 like symptom (ref.: No symptom) | |||
| Single symptom | 1.60 (1.002–2.54)* | 3.02 (1.83–4.99)*** | 0.93 (0.59–1.48) |
| More than one symptom | 3.06 (1.94–4.85)*** | 4.96 (3.16–7.80)*** | 1.53 (0.99–2.38) |
| Recent quarantine in last 14 days (ref.: No) | |||
| Yes | 1.73 (0.51–5.83) | 3.67 (1.14–11.81)* | 3.33 (0.73–15.29) |
| Contact with individuals with confirmed cases of COVID-19 (ref.: No) | |||
| Yes | 3.99 (1.29–12.35)* | 3.17 (1.41–3.30)** | 0.73 (0.30–1.78) |
| Contact with individuals with suspected COVID-19 or infected materials (ref.: No) | |||
| Yes | 1.54 (0.85–2.77) | 0.73 (0.38–1.39) | 1.85 (0.99–3.38) |
***p < 0.001, **p < 0.01, *p < 0.05.
OR = Odds Ratio; CI = Confidence Interval.
4. Discussion
This study investigated students' mental health (stress, anxiety and depression) at the time of the COVID-19 crisis in Bangladesh. Findings indicate that 57.05% of students suffered from mild to extremely severe stress levels, similar to a study among adults in Bangladesh (60%) (Banna et al., 2020). This finding can potentially be compared with the study by Khan et al. 2020 which reported 28.50% moderate to extremely severe stress levels among Bangladeshi students during the pandemic whereas we categorized and reported mild to extremely severe levels of stress (Khan et al., 2020). The study suggests that 26.66% of students reported mild to extremely severe levels of anxiety, which is lower than the Bangladeshi study (33.28% having moderate to extremely severe levels of anxiety) (Khan et al., 2020) and higher than the China study (7.7%) (Wang et al., 2020c), but somehow comparable to another China study (24.9%) (Cao et al., 2020). In the study, 61.97% of students reported mild to extremely severe depressive symptoms that were higher than Bangladesh (46.92% having moderate to extremely severe depressive symptoms) (Khan et al., 2020) and China (12.2%) (Wang et al., 2020c). Studies suggest that students might develop mental health difficulties during public health emergencies like this, but we found fewer mental health difficulties among students in China. This might be due to the festive survey time, as the study was conducted during the Chinese biggest traditional 'Chinese New Year' festival (Wang et al., 2020c). Disrupted educational activity due to the COVID-19 pandemic might be a reason for emerging mental health difficulties in students which can be potentially supported by necessary & adequate arrangements for online classes (Kapasia et al., 2020, Roy et al., 2020).
Students of less/equal to 22 years had a greater psychological impact than students of over 22 years of age. This finding is contrary to an earlier study that shows a higher psychological impact for older age (Khan et al., 2020). This may be due to the higher COVID-19 knowledge among higher aged university students (Wang et al., 2020c). In females, higher stress levels, anxiety symptoms and depressive symptoms were observed, which is consistent with previous findings in Bangladeshi students (Khan et al., 2020). The potential explanation for female showing higher psychological impact due to the easily negatively affected nature of the female while keeping other variables constant (Elmer, Mepham, & Stadtfeld, 2020). However, female students in all student groups were a minority group which may lead to their potentially higher vulnerability in our study. We found more anxiety and depression among the students with a lower economic status. Economic stressors have also been found to be positively associated with anxiety in Chinese college students during the epidemic (Cao et al., 2020) which calls for further research. The pandemic also affects the family economy and students might be anxious to maintain the ongoing study & associated cost.
Students from the rural areas showed lower anxiety symptoms and depressive symptoms and this result is in line with a Bangladeshi study among adults. This may be due to the lower affected rate in rural areas (IEDCR, 2020). We interestingly found that students from those families which had equal or less than four members showed higher anxiety symptoms and depressive symptoms. Further investigation is required to understand the findings.
Respondents who claimed that the COVID-19 pandemic had a negative impact on his mental health had a substantial association with negative psychological effects and this result is similar among adults in Bangladesh (Banna et al., 2020). 82.4% of the student believed that “the worst of COVID-19 is yet to come”, which is quite identical among Bangladeshi (Banna et al., 2020) and American adults (KFF, 2020). More than half of the students assume that “the health care system will overrun,” and this proportion is consistent with the previous study among adults in Bangladesh (Banna et al., 2020). A recent study reproached that Bangladesh doesn't have the economic or systemic capacity to address COVID-19 adequately, reflecting public perceptions of Bangladesh's rudimentary healthcare systems (Islam & Siddika, 2020).
In this study, 37.2% of students reported having at least one symptom like headache, dizziness, myalgia, cough, runny nose, and breathing difficulty, etc. which is marginally higher than the previous study (29.7%) (Khan et al., 2020). The psychological impact is higher among those students who have at least one COVID-19 like symptoms and this outcome is identical to the previous study in Bangladeshi students (Khan et al., 2020). Previous studies in China during the COVID-19 also showed that physical symptoms can affect the psychological response significantly (Wang et al., 2020b). Bangladeshi residents with COVID-19-like symptoms are struggling to access adequate healthcare in a hospital setting. A daily newspaper has reported an increase in deaths from symptoms similar to COVID-19, likely due to too few testing facilities and the resulting hospital refusals (NEW AGE, 2020). This may be the reason for the higher psychological distress among the respondents with COVID-19 like symptoms. This finding suggests that health professionals should provide psychological support with treatment for those who have those COVID-19 like symptoms in the pandemic situation.
This study is among the first few studies in Bangladesh context on the mental health impacts of the COVID-19 pandemic among students. This study included students from all divisions across Bangladesh. These results warrant consideration of easily accessible, low-intensity interventions to support mental health for students during and after this pandemic.
However, this study has several limitations to acknowledge, including the snowball sampling method for recruiting students online, which may suggest sampling bias by excluding those who do not have access to the internet. This also limits the generalizability of the findings. This recruitment strategy may also have contributed to the skewed demographic distribution of gender, with the current sample comprised of larger proportions of male students while data from female students are scarce. Limited research on this novel topic hinders the robustness of the conclusion of the study. Additionally, anxiety, depression & stress symptoms were determined by self-reported data and subjected to response bias. The present study does not provide any qualitative information regarding preventive measures and coping strategies of the students which are warranted in future studies. No causality cannot be established due to the cross-sectional study design. In addition, some important confounding factors were overlooked such as part-time employment, physical comorbidity, pre-existing mental illnesses of the students. Lastly, all data were based on self-reported and could have been affected by memory recall of social desirability biases.
5. Conclusion
During the COVID-19 pandemic, a high prevalence of depression symptoms, anxiety & stress symptoms among students was observed in this study. The findings also reported that students’ age, gender, income, location of residence, and family size are associated with mental health difficulties. Negative perceptions on the effect of the pandemic on life events, mental health, disruptions in education, health care system, existing physical health conditions, and COVID-19 like symptoms were significantly associated with poor mental outcomes. It is suggested that students ' mental health difficulties should be monitored carefully to provide adequate support during this ongoing pandemic. We will echo with what Khan et al. (2020) suggested, improving the delivery of low intensity psychological intervention, especially community-based, aligning with the clinical field of the health system should be the key. Additionally, educating youth on COVID-19 may improve the perception of this group to fight against a global threat in these trying times.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Abu Sayeed: Conceptualization, Methodology, Project administration. Satyajit Kundu: Formal analysis, Software, Writing - review & editing. Md. Hasan Al Banna: Writing - review & editing, Investigation, Validation, Writing - original draft. M. Tasdik Hasan: Validation, Writing, review & editing. Musammet Rasheda Begum: Formal analysis, Software. Md. Shafiqul Islam Khan: Methodology, Validation, Investigation.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgments
Acknowledgment
The authors thank all the participants of the study.
Ethics
The research protocol was reviewed and approved by the Research Ethical Committee (REC) of the Department of Food Microbiology, Patuakhali Science and Technology University, Bangladesh (Approval no: FMB:22/04/2020:02). This study complied with the most recent revision of the Helsinki Declaration and followed the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines.
References
- Alim S.M.A.H., Ahmed M.N., Mullick M.S.I., Chowdhury N.F., Akhter F., Alam M.S. Validation of the Bangla version of Beck Depression Inventory-II. Brain and Behavior. 2020;10(3) doi: 10.1002/brb3.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alim S.M.A.H.M., Rabbani M.G., Karim E., Mullick M.S.I., Al Mamun A., Khan M.Z.R. Assessment of depression, anxiety and stress among first year MBBS students of a public medical college, Bangladesh. Bangladesh Journal of Psychiatry. 2015;29(1):23–29. [Google Scholar]
- Anjum A., Hossain S., Sikder T., Uddin M.E., Rahim D.A. Investigating the prevalence of and factors associated with depressive symptoms among urban and semi-urban school adolescents in Bangladesh: A pilot study. International Health. 2019 doi: 10.1093/inthealth/ihz092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anwar S., Nasrullah M., Hosen M.J. COVID-19 and Bangladesh: Challenges and how to address them. Frontiers Public Health. 2020;8 doi: 10.3389/fpubh.2020.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banna M.H., Sayeed A., Kundu S., Christopher E., Hasan M.T., Begum M.R.…Khan M.S.I. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: A nationwide cross-sectional study. International Journal of Environmental Health Research. 2020 doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;112934 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper I., Mondal A., Antonopoulos C.G. A SIR model assumption for the spread of COVID-19 in different communities. Chaos, Solitons & Fractals. 2020:110057. doi: 10.1016/j.chaos.2020.110057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. 2020;15(7) doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) Journal of Medical Internet Research. 2004;6(3) doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan N., Bao Y. Impact of “e-Learning Crack-up” perception on psychological distress among college students during COVID-19 pandemic: A mediating Role of “Fear of Academic Year Loss”. Children and Youth Services Review. 2020;105355 doi: 10.1016/j.childyouth.2020.105355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain S., Anjum A., Uddin M.E., Rahman M.A., Hossain M.F. Impacts of socio-cultural environment and lifestyle factors on the psychological health of university students in Bangladesh: A longitudinal study. Journal of Affective Disorders. 2019;256:393–403. doi: 10.1016/j.jad.2019.06.001. [DOI] [PubMed] [Google Scholar]
- IEDCR Covid-19 Status Bangladesh. 2020. https://www.iedcr.gov.bd/ Retrieved from.
- Islam, M. D., & Siddika, A. (2020). COVID-19 and Bangladesh: A study of the public perception on the measures taken by the government.
- Kapasia N., Paul P., Roy A., Saha J., Zaveri A., Mallick R.…Chouhan P. Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal, India. Children and Youth Services Review. 2020;116 doi: 10.1016/j.childyouth.2020.105194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KFF. (2020). The Implications of COVID-19 for Mental Health and Substance Use: Available at: https://www.kff.org/health-reform/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/?fbclid=IwAR0PqOL5KBohMQgOoFbj3FFr-rV5gn1DoyhbUMTHikSmpr8jTWxlN.
- Khan, A. H., Sultana, M. S., Hossain, S., Hasan, M. T., Ahmed, H. U., & Sikder, M. T. (2020). The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. [DOI] [PMC free article] [PubMed]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- NEW AGE. (2020). 1,010 die with COVID-19 symptoms in 70 days in Bangladesh. [Online]. Available in: https://www.newagebd.net/article/106772/1010-die-with-covid-19-symptoms-in-70-days-in-bangladesh [accessed on 17 June 2020].
- Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Research. 2020;113108 doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravesloot C., Ward B., Hargrove T., Wong J., Livingston N., Torma L., Ipsen C. Why stay home? Temporal association of pain, fatigue and depression with being at home. Disability and Health Journal. 2016;9(2):218–225. doi: 10.1016/j.dhjo.2015.10.010. [DOI] [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020;102083 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadiq M.S., Morshed N.M., Rahman W., Chowdhury N.F., Arafat S.M.Y., Mullick M.S.I. Depression, anxiety, stress among postgraduate medical residents: A cross sectional observation in Bangladesh. Iranian Journal of Psychiatry. 2019;14(3):192. [PMC free article] [PubMed] [Google Scholar]
- Sayeed A., Hassan M.N., Rahman M.H., El Hayek S., Al Banna M.H., Mallick T.…Kundu S. Facebook addiction associated with, internet activity, depression and behavioral factors among university students of Bangladesh: A cross-sectional study. Children and Youth Services Review. 2020:105424. [Google Scholar]
- Shen M., Peng Z., Guo Y., Rong L., Li Y., Xiao Y.…Zhang L. Assessing the effects of metropolitan-wide quarantine on the spread of COVID-19 in public space and households. International Journal Of Infectious Diseases. 2020 doi: 10.1016/j.ijid.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temsah M.-H., Al-Sohime F., Alamro N., Al-Eyadhy A., Al-Hasan K., Jamal A.…Barry M. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. Journal of Infection and Public Health. 2020 doi: 10.1016/j.jiph.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Sharma V.K. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.-H., Yang H.-L., Yang Y.-Q., Liu D., Li Z.-H., Zhang X.-R.…Song W.-Q. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. Journal of Affective Disorders. 2020 doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J.R. The Declaration of Helsinki and public health. Bulletin of the World Health Organization. 2008;86:650–652. doi: 10.2471/BLT.08.050955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: Structured letter therapy. Psychiatry Investigation. 2020;17(2):175. doi: 10.30773/pi.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]