Abstract
The spread of SARS-CoV-2 by contact (direct or indirect) is widely accepted, but the relative importance of airborne transmission is still controversial. Probability of outdoor airborne transmission depends on several parameters, still rather uncertain: virus-laden aerosol concentrations, viability and lifetime, minimum dose necessary to transmit the disease. In this work, an estimate of outdoor concentrations in northern Italy (region Lombardia) was performed using a simple box model approach, based on an estimate of respiratory emissions, with a specific focus for the cities of Milan and Bergamo (Italy). In addition, the probability of interaction of virus-laden aerosol with pre-existing particles of different sizes was investigated. Results indicate very low (<1 RNA copy/m3) average outdoor concentrations in public area, excluding crowded zones, even in the worst case scenario and assuming a number of infects up to 25% of population. On average, assuming a number of infects equal to 10% of the population, the time necessary to inspire a quantum (i.e. the dose of airborne droplet nuclei required to cause infection in 63% of susceptible persons) would be 31.5 days in Milan (range 2.7–91 days) and 51.2 days in Bergamo (range 4.4–149 days). Therefore, the probability of airborne transmission due to respiratory aerosol is very low in outdoor conditions, even if it could be more relevant for community indoor environments, in which further studies are necessary to investigate the potential risks. We theoretically examined if atmospheric particles can scavenge virus aerosol, through inertial impact, interception, and Brownian diffusion. The probability was very low. In addition, the probability of coagulation of virus-laden aerosol with pre-existing atmospheric particles resulted negligible for accumulation and coarse mode particles, but virus-laden aerosol could act as sink of ultrafine particles (around 0.01 μm in diameter). However, this will not change significantly the dynamics behaviour of the virus particle or its permanence time in atmosphere.
Keywords: SARS-CoV-2, COVID-19, Airborne virus transmission, Coronavirus, Aerosol, Coagulation
Highlights
-
•
Concentrations of SARS-CoV-2 in outdoor air were estimated using a box model.
-
•
Probability of interactions with pre-existing aerosol particles was investigated.
-
•
Average outdoor concentration was <1 RNA copy/m3 even in the worst case scenario.
-
•
Probability of outdoor airborne transmission was extremely low.
-
•
Virus-laden aerosol could act as a sink of ultrafine particles.
1. Introduction
The COVID-19 is the disease associated to the SARS-CoV-2 virus, that was initially reported in Wuhan (China), and successively it spread all over the world and was declared Public Health Emergency of International Concern by the World Health Organization (WHO). COVID-19 produces an acute respiratory disease and the main clinical manifestations are fever, cough, and dyspnoea. The spread of SARS-CoV-2 by contact (direct or indirect through contaminated surfaces) is widely accepted (WHO, 2020), but the relative importance of airborne transmission is controversial (Asadi et al., 2020; Bontempi 2020; Domingo et al., 2020; Jiang et al., 2020; Klompas et al., 2020; Morawksa et al., 2020; Prather et al., 2020; Zhang et al., 2020).
Viral respiratory infections are an important cause of morbidity and mortality worldwide. They may range from asymptomatic to acute diseases, in some cases life-threatening. Breathing, talking, coughing or sneezing release droplets, which can contain viral particles, in case of infected individuals. Airborne transmission of disease could occur by means of large droplets (>5 μm) released during respiration, coughing, and sneezing by contagious persons, or by solid residuals (called droplet nuclei or aerosol) of small droplets (<5 μm). Generally large droplets settle faster than they evaporate, contaminating the immediate vicinity of the infected individuals. In contrast, small droplets evaporate faster than they settle, leaving a residual which might contain virus aggregates, proteins, and mineral salts (Bourouiba, 2020; Asadi et al., 2020). They have a longer permanence time in atmosphere and can be transported and dispersed, by winds, over longer distances compared to large droplets.
Probability of airborne transmission depends on several parameters, still rather uncertain, such as virus-laden aerosol concentrations, viability and lifetime, and minimum dose necessary to transmit the disease (Contini and Costabile, 2020; Buonanno et al., 2020). This probability could be significantly different in outdoor and indoor community environments (such as hospitals, quarantine areas, commercial centres and so on) because there could be more intense sources (number of infected individuals) and negligible dispersion and transport conditions. In addition, the influence of meteorological parameters, such as UV radiation, that could deteriorate the virus reducing its lifetime in atmosphere (Ratnesar-Shumate, 2020) is significantly different when indoors and outdoors are compared. The analysis of Nishiura et al. (2020) in eleven COVID-19 clusters in Japan showed that the odds that a primary case transmitted COVID-19 in a closed environment was 18.7 times greater compared to an open-air environment. The analysis of Arav et al. (2020) showed that indoor airborne transmission in pre-symptomatic cases has a minor role compared to other transmission mechanisms.
Some studies (Conticini et al., 2020; Setti et al., 2020a, 2020b) suggested that outdoor airborne transmission could have played an important role during COVID-19 outbreak in northern Italy in winter 2020. The mechanism hypothesized is that virus-laden aerosol could interact with atmospheric particles creating clusters with pre-existing particles acting as carriers enhancing the persistence of the virus in atmosphere. This lead to the suggestion that atmospheric particulate matter concentrations is a kind of proxy to track virus dispersion in the atmosphere. There are not, up to now, specific data on the interaction of SARS-CoV-2 with pre-existing particles. However, it is known that atmospheric aerosols could contain biological material (bacteria and viruses) in certain conditions (Verreault et al., 2008; Deprés et al., 2012) and that the interaction between viruses and atmospheric particles could influence (increasing or decreasing) their infectivity (Groulx et al., 2018). Concentration and size distribution of both virus-laden aerosol and pre-existing particles strongly influence the probability of interaction.
Measurements of SARS-CoV-2 concentration in air (in both outdoor and indoor conditions) are relatively limited and some contrasting results were observed. In Liu et al. (2020) outdoor air samples collected in public areas in Wuhan (China) during the COVID-19 pandemic gave negative results, when tested for the presence of SARS-CoV-2 RNA with the exclusion of some specific crowded areas. Similar results were obtained from the measurements reported in Hu et al. (2020). Outdoor air samples collected in northern Italy (in the city of Bergamo) during the COVID-19 outbreak were positive to the presence of SARS-CoV-2 RNA in 23% of the measurement days, but no determination of concentration was provided (Setti et al., 2020a). Outdoor air samples simultaneously collected in Venice (northern Italy) and in Lecce (southern Italy) in May 2020 tested negative for the presence of SARS-CoV-2 RNA (Chirizzi et al., 2020). In indoor conditions, larger concentrations of virus-laden aerosols, compared to outdoor environments, were measured in some hospitals and quarantine areas (Hu et al., 2020; Liu et al., 2020; Santarpia et al., 2020). However, other studies reported negative results for indoor SARS-CoV-2 RNA detection even near COVID-19 confirmed patients (Faridi et al., 2020; Ong et al., 2020). In none of these studies was possible to ascertain the viability of collected viral particles.
This demonstrates that further studies, also using multidisciplinary approaches (Bontempi et al., 2020), are needed to investigate the role of virus airborne transmission in the spread of COVID-19. This work presents a study, using simple box models, of the average concentration of virus-laden aerosol due to respiratory emissions, in outdoor air in Lombardia region (northern Italy, severely hit by COVID-19) during winter 2020. In addition, the probability of interactions of virus-laden aerosol with pre-existing particles, an aspect previously not addressed in published papers, is investigated.
2. Characterisation of emissions
Sneezing, coughing, and respiration lead to release of large droplets and smaller aerosols. Conventionally, a distinctive size of 5 μm is used (Anderson et al., 2020) to separate droplets and aerosols. These emissions are saliva and secretions expelled (atomisation) from the upper airway, through the mouth or the nose (Morawska et al., 2009; Han et al., 2013; Bourouiba et al., 2014; Asadi et al., 2019; Bake et al., 2019; Hsiao et al., 2020; Martano, 2020). Large droplets tend to be removed quickly by dry deposition processes, and this is the reason of the suggested physical distance to minimise the risk of short distance contagion. Instead, small aerosols have a relevant fraction in the size range of the accumulation mode and they, or the droplet nuclei after evaporation (Asadi et al., 2020), could remain in suspension in air for longer time span compared to large droplets (Stadnytskyi et al., 2020).
Sneezing, mainly associated to symptomatic individuals, produces relevant number of large droplets. In Han et al. (2013) sneezing tests from human participants were performed and two size distributions including unimodal (aerosol geometric mean: 360.1 μm) and bimodal (aerosol geometric mean: 74.4 μm) were observed. Coughing is mainly associated to symptomatic individuals; however, it could also involve occasional coughs from asymptomatic individuals. Lindsley et al. (2012) showed that the amount of particles emitted in a cough varies widely from patient to patient in a range between 900 and 300,000 particles/cough with an average of 75,400 particle/cough (standard deviation 97,300) in patients with influenza and an average of 52,200 particles/cough (standard deviation 98,600) after recovery from influenza. In general, 63% of droplets emitted during coughing are in the respirable size range (Lindsley et al., 2012). Respiration and speaking, that are relevant also for asymptomatic individuals, are a source of fine aerosol (Morawska et al., 2009; Asadi et al., 2019), even if the intensity of the source is more limited compared to singing, shouting, coughing or sneezing. In Asadi et al. (2019), measurements during breathing showed a typical emissions from mouth and nose, in normal and fast breathing, lower than 3000 particles/h, with geometric mean diameter around 0.8 μm. Emissions during speaking and vocalisations are larger, between 3000 and 36,000 particles/h, with a geometric mean diameter (around 1 μm). Furthermore, emission intensity increases during loud speaking compared to whispering (Morawska et al., 2009; Asadi et al., 2019).
Respiratory droplets and aerosols released by infected individuals could contain viral particles. There are limited experimental evidences for the SARS-CoV-2, however, viral RNA in respiratory droplets and aerosols was observed for other respiratory viruses including other coronavirus (Milton et al., 2013; Yan et al., 2018; Leung et al., 2020). Milton et al. (2013) found a median emission of about 1200 RNA copies/h in respiration of influenza infected individuals, at one day from the onset of the disease, in aerosols (<5 μm) and about 50 copies/h in the coarse fraction (>5 μm) with a decrease in the successive days. Leung et al. (2020) found emissions, in the aerosol size fraction (<5 μm), in the range 4–4000 copies/h for other coronaviruses (NL63, OC43, 229E, and HKU1), 4–2000 copies/h for influenza, and 4–1200 copies/h for rhinovirus.
Another important aspect is the fraction of these respiratory virus-laden particles that are effectively viable and able to transmit the contagion. There are no information regarding SARS-CoV-2. However, the study of Yan et al. (2018) for the influenza virus found a small but statistically significant correlation among viable virus counting and RNA copies concentration in respiratory aerosols. The only study relative to the lifetime of SARS-CoV-2 in air is from van Doremalen et al. (2020) that found a half-life of about 1 h and that the virus can remain viable in air for about 3 h in laboratory controlled conditions. In outdoor conditions, the effective lifetime could depend from meteorological conditions, like temperature, humidity, and solar radiation that could degrade the virus (Ratnesar-Shumate et al., 2020).
The emissions of viral RNA copies can be estimated following the approach proposed in Buonanno et al. (2020): using mass balance between the viral load in mouth (sputum) and the volume of particles emitted during respiration and speaking. Specifically, the emission rate (E) is evaluated as:
| (1) |
where IR is the inspiration rate, CV the viral load in the mouth (in sputum), Nj the particle number concentration in the size range j, and Vj the volume of particle in the same size range. We considered four aerosol size ranges, as done in Morawska et al. (2009), and reported in Table 1 . These were differentiated for diurnal and nocturnal hours. In diurnal hours, the particle concentrations are the average between unmodulated vocalization and voiced counting as done in Buonanno et al. (2020), instead, in nocturnal hours the particle concentrations refer to breathing activity.
Table 1.
Particle concentrations (cm−3) for different size ranges separated for diurnal and nocturnal hours.
| Diam. 0.8 μm | Diam. 1.8 μm | Diam. 3.5 μm | Diam. 5.5 μm | |
|---|---|---|---|---|
| Diurnal hours | 0.4935 | 0.1035 | 0.073 | 0.035 |
| Nocturnal hours | 0.084 | 0.009 | 0.003 | 0.002 |
The inhalation rates, averaged between females and males, are equal to 0.49 (resting), 0.54 (standing), 1.38 (light exercise), 2.35 (moderate exercise), and 3.30 m3/h (heavy exercise) (Adams, 1993). For nocturnal hours the value at rest (0.49 m3/h) was used, while, for diurnal hours the values of light exercise 1.38 m3/h was used. The average of the two conditions (i.e. the daily average considering 12 h at rest and 12 h of activity) was 0.94 m3/h. In order to develop a worst case scenario (WCS from now on), an increased inhalation rate (1.08 m3/h) obtained considering 8 h per day at rest and 16 h per day of activity was also used.
Recent research studies investigated values of viral load in the mouth of COVID-19 confirmed patients finding highly variability, also related to the number of days from the onset of the disease. Wölfel et al. (2020) found an average viral load in sputum (CV) of 7 × 106 copies/mL, with a maximum of 2.35 × 109 copies/mL in COVID-19 patients. Rothe et al. (2020) investigate one case of transmission from an asymptomatic individual, finding a high viral load in sputum of 108 copies/mL, confirming that asymptomatic individuals could be a potential source. A study on 82 SARS-CoV-2 infected individuals (Pan et al., 2020) found highly variable viral load in sputum with several cases having values between 108 copies/mL and 109 copies/mL and one case arriving up to 1011 copies/mL. Therefore, in this work, we consider a median value of CV equal to 109 copies/mL.
With the assumptions discussed, the probability that a 10 μm droplet, prior to dehydration, contains one RNA copy is about 52% and this probability decrease to about 0.05% for a 1 μm droplet. The average estimated emission is 3613 RNA copies/h per infected individual. With the WCS assumptions, the estimated emission is 4770 RNA copies/h.
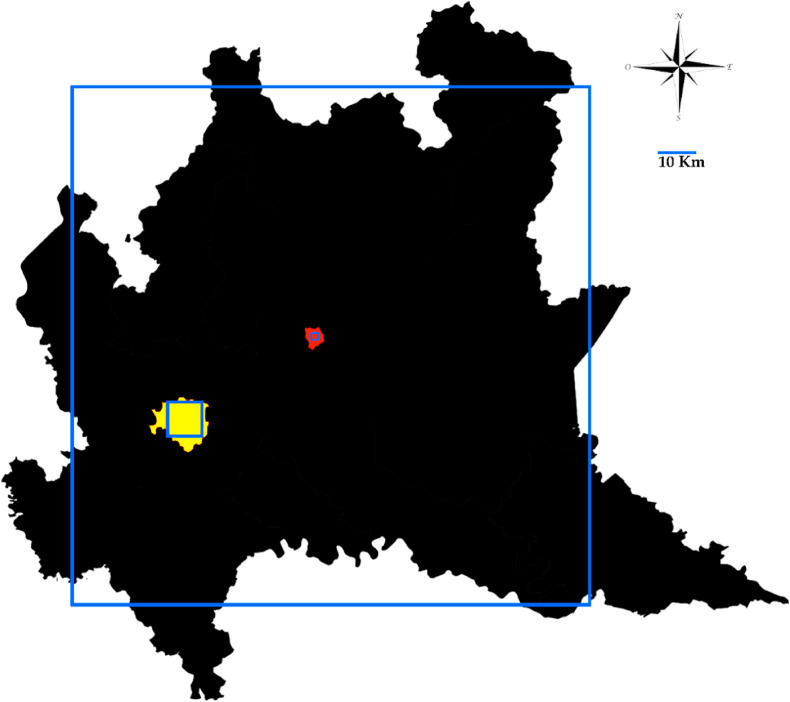
3. Estimate of outdoor concentrations using a box model
We used a simple box model approach to estimate average outdoor atmospheric concentrations of RNA copies of SARS-CoV-2 in the Region Lombardia as function of the number of infected individuals and using the average emissions estimated in Section 2. This model could give information regarding long-term averages and the effect of mixing height and ventilation (wind speed). Sophisticated models are available for analysis of pollutant transport and dispersion with high spatial and temporal resolution. However, they need, as input, data on emissions with high details on spatial and temporal resolutions. These details are not available for virus-laden aerosol emissions released during respiration and speaking, for this reason we choose to apply a simple box model. The box model is based on a large square of 150 km by 150 km covering almost all region Lombardia (Fig. 1 ) and having a height equal to the average mixing layer height. The mixing layer over the city of Milan (the largest city of Lombardia) was analysed in Ferrero et al. (2010) for the period 2005–2008 showing values, in winter, between 50 m and 500 m with typical median values around 250 m. The vertical profiles of particulate matter showed that 70% (for PM1) and 80% (for PM10) of particles were inside the mixing layer with rather uniform profiles. The analysis of the mixing layer height in Milan, done using measurements taken with the Sonic Detection and Ranging (SODAR) approach (Argentini et al., 1999), showed similar figures for the mixing layer height generally between 200 m and 300 m. Data provided by Arpa Lombardia, at the Milano Linate airport for the period February–April 2020, showed a median value of the mixing height of 240 m in February and an increase in March and April. Therefore, for the modelling purposes, we assumed an average mixing layer height of 250 m containing 75% of the RNA copies as a uniform profile. For the sake of simplicity and as precaution, coagulation and deposition processes were neglected.
Fig. 1.
Map of the region Lombardia with indication of the box model domain. In yellow the area of the city of Milan with the second box domain and in red the location of the city of Bergamo with the third box domain. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Wind velocity near the ground (at 10 m height) in the area near Milan could be relatively small. Average winter value of 0.84 m/s was observed in Ferrero et al. (2010) and values between 0.5 m/s and 2.5 m/s were observed in Silibello et al. (2008). The analysis of the data from three meteorological stations in Milan, managed by the Regional Environmental Agency (Arpa Lombardia), gave a median wind velocity near the ground of 1.1 m/s in the period February–April 2020. Therefore, for the model, we assumed an average wind velocity of 2.2 m/s at a height of 125 m above the ground (i.e. in the middle of the mixing layer). This was obtained using the typical factor 2 for the ratio between the wind velocity at 125 m and that at 10 m in long-term average wind velocity profile in suburban areas (Contini et al., 2009). For the worst case scenario, we used a lower mixing height (60 m), about the minimum values (range 50 m–70 m) observed over Milan (Ferrero et al., 2010) in winter period, and a lower wind velocity of 1.2 m/s. The latter obtained as the first quartile (25th percentile) of the wind velocities measured at the different stations (0.9 m/s) multiplied by a factor 1.36 for the ratio between the middle of the mixing height (30 m) and the measurement height (10 m). A best case scenario (BCS from now on) was also analysed. This refers to better dispersion conditions compared to average or to WCS values. Specifically, in this case the mixing height selected was 400 m corresponding to the third quartile (75th percentile) of the measurements at the Milano Linate airport in February and roughly around the maximum values measured in Ferrero et al. (2010) and in Argentini et al. (1999). The wind speed selected was 4 m/s chosen as the third quartile of the wind velocities measured at the different stations (1.7 m/s) multiplied by a factor 2.35 for the ratio between the middle of the mixing height (200 m) and the measurement height (10 m).
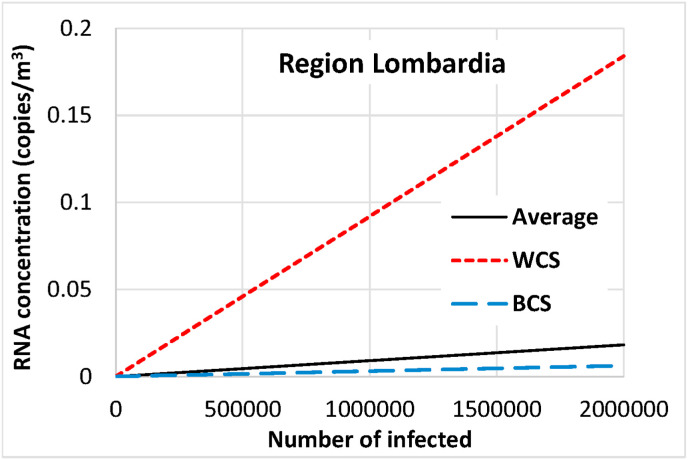
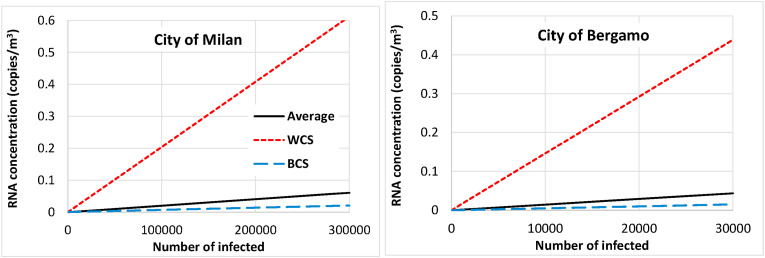
Estimated average concentrations are reported in Fig. 2 as function of the number of infected individuals (including asymptomatic) for the entire region Lombardia (about 23,844 km2 and 10 million inhabitants). These results have been used as boundary condition for the application of two other box models (Fig. 1): one of 10 km by 10 km covering the earth of the Milan town (about 1.4 million inhabitants); the second with an extension of 2 km by 2 km centred above the town of Bergamo (about 120,000 inhabitants) in which there was an epidemic outbreak. The results are reported in Fig. 3 , again including the average, the WCS, and the BCS results. To put in perspective these results, it is useful to consider the officially counted cases furnished by the Italian Ministry of Health (www.salute.gov.it). It must be said that the numbers could be underestimated because they are related to the capacity of performing nasal/mouth swabs and to the absence of systematic testing on asymptomatic individuals. In the region Lombardia, the maximum number of active cases (i.e. the currently positive individuals) was 37,305 achieved on May 04, 2020. At the same date, the total number of cases in the region was 78,105. Data was not available at city level but total number of cases is available for each Italian province. The total number of cases in the province of Milan at May 04, 2020 was 20,254 and in the province of Bergamo 11,538 cases were counted on the same date.
Fig. 2.
Estimated average outdoor concentration as function of the number of infected individuals for the Region Lombardia. WCS is the worst case scenario calculated with larger emissions and lower wind speed and mixing height compared to average. BCS is the best case scenario calculated with larger wind speed and mixing height compared to average.
Fig. 3.
Estimated average outdoor concentration as function of the number of infected individuals for the Milan and Bergamo cities. WCS is the worst case scenario calculated with larger emissions and lower wind speed and mixing height compared to average. BCS is the best case scenario calculated with larger wind speed and mixing height compared to average.
Estimated outdoor average concentrations are relatively small; this is in agreement with the few measurements available. Aerosols samples were collected in Wuhan (China) in February 2020 and found no detectable concentration of SARS-CoV-2 (<3 copies/m3) with the exclusion of crowded sites, in which concentrations up to 11 copies/m3 were observed. In the preprint of Hu et al. (2020), aerosol samples were collected in Wuhan (China) in outdoor public areas and in different hospitals (indoor), and no virus copies were found in outdoor samples in residential and public areas. In a recent work (Setti et al., 2020a), it is reported that traces of viral RNA were observed in 8 cases out of 34 (about 23% of positive cases) in PM10 daily samples collected in Bergamo (Northern Italy) during the spread of COVID-19 in the period between February and March 2020 even if concentrations were not quantified.
According to the data reported in Fig. 3, considering the average inspiration rate discussed in the previous Section and a number of infected individuals equal to 10% of the population (about 140,000 people for Milan and 12,000 people for Bergamo), it would be necessary, on average, 38 h in Milan (range calculated from BCS and WCS scenarios: 3.2–109 h) and 61 h in Bergamo (range 5.3–179 h) to inspire a single virus particle. Furthermore, it must be considered that a single virus particle could be not sufficient to transmit the infection. It can be used the concept of quantum, defined as the dose of airborne droplet nuclei required to cause infection in 63% of susceptible individuals. The conversion factor Ci defined as the ratio between one infectious quantum and the infectious dose expressed in viral RNA copies is not defined for SARS-CoV-2 in current scientific literature. However, referring to SARS-CoV-1, that has similar characteristics (van Doremalen et al., 2020), Watanabe et al. (2010) estimated the SARS-CoV-1 infectious doses received by residents in Hong Kong, corresponding to a Ci between 0.01 and 0.1 (Li et al., 2005; Yu et al., 2004). An average value equal to 0.05 was used for this work, as done in Buonanno et al. (2020). In the conditions stated above, the average time necessary to inspire a quantum would be 31.5 days in Milan (range calculated using BCS and WCS scenarios: 2.7–91 days) and 51.2 days in Bergamo (range 4.4–149 days). Therefore, the possibility to have airborne transmission in outdoor is low, almost negligible, if crowded areas and large gatherings of people are avoided.
The situation is different in specific community indoor environments in which there is the possibility to have several infected individuals in restricted spaces. In these environments, the transport and dispersion, and consequently the dilution of airborne viral particles is more limited so that concentrations could be larger. In addition, the indoor environmental conditions (temperature, humidity, and absence of solar radiation) could be more suitable for virus survival compared to outdoors. Santarpia et al. (2020) observed the presence of viral RNA in the air in isolation rooms where patients with SARS-CoV-2 were treated. The analysis by Liu et al. (2020) of aerosol samples in two hospitals in Wuhan (China), during COVID-19 outbreak, showed high concentrations in patient care areas (up to 19 copies/m3 in toilet facility) as well as in medical staff areas (18–42 copies/m3). Liu et al. (2020) also performed size-segregated analysis of indoor virus in air showing that a relevant fraction of these virus-laden aerosols was in the fine size range (0.2–1 μm) that could remain in air for a longer time compared to the coarse fractions, thus being more suitable for airborne transmission. Faridi et al. (2020) collected ten air samples in the major hospital in Iran but detection of SARS-CoV-2 in air inside patient rooms was unsuccessful. In Hong Kong (Cheng et al., 2020) air samples taken near the mouth of an established COVID-19 patients tested negative for the presence of SARS-CoV-2, although the statistics was very limited. In Singapore, in an isolation area (with 12 air changes per hour) that housed three COVID-19 patients, samples were collected from surfaces and in the air (for 2 days). The air samples were negative even if traces of SARS-CoV-2 were found on the surfaces (Ong et al., 2020). Therefore, there are contrasting results that could likely arise also from the different measurement conditions and the different methodological approaches used. However, community indoor environments could represent a larger risk compared to outdoor (Contini and Costabile, 2020; Buonanno et al., 2020) and further studies are necessary to ascertain this aspect. It is advisable to use masks and frequent ventilation in these indoor environments to minimise risks.
In Setti et al. (2020b) it is hypothesized that the presence of SARS-CoV-2 RNA in outdoor air samples could represent a potential early indicator of COVID-19 diffusion. According to the results presented here, to have a probability of 50% of collecting a RNA copy in a standard 24 h air sample (55 m3), it would be necessary a number of infected individuals, including asymptomatic, equal to about 45,000 in the city of Milan (3.2% of the population) and to about 6300 in the city of Bergamo (5.2% of population). Sporadically, RNA copies could be detected on filters for periods with low dispersion conditions as those of the worst case scenario. Therefore, it is doubtful that this approach could be efficiently used as an early indicator of COVID-19 diffusion or an early indicator of a recrudescence of the pandemic.
4. Interaction of virus-laden aerosol with pre-existing atmospheric particles
Johnson et al. (2011) showed that droplets size distribution emitted via coughing, sneezing, speaking and breathing are multimodal, with modes diameters around 200 μm and 2 μm. The small droplets evaporate rapidly leaving droplet residuals (virions) consisting of virus aggregates, proteins and mineral salts. At 50% relative humidity (RH), a 10 μm pure water droplet evaporates in about 0.15 s (Hinds, 1999). Xie et al. (2007) numerically calculated the evaporation and dispersion of respiratory droplets with a salinity of 0.9% w/v at ambient air temperature and different RH. A 20 μm droplet evaporates in less than 1 s. Redrow et al. (2011) carried out simulations on sputum droplets and numerical results indicate that a 10 μm sputum droplet will evaporate to become a droplet nucleus (3.5 μm) in 0.55 s at 80% RH and in 0.3 s at 50% RH. These virions have low sedimentation velocities and can remain suspended in atmosphere and, eventually, interact with pre-existing atmospheric particulate matter (PM). Setti et al. (2020a) suggested that SARS-CoV-2 RNA can be present on outdoor PM and in conditions of atmospheric stability and high concentrations of PM, SARS-CoV-2 could create clusters with outdoor PM and, by reducing their diffusion coefficient, enhance the persistence of the virus in the atmosphere. However, this preliminary result must be confirmed. We theoretically examined if atmospheric particles can scavenge virions.
4.1. Selected atmospheric particles and virions number concentrations and sizes
We estimate the atmospheric particles number concentration in winter in Bergamo, one of the most relevant COVID-19 outbreak in northern Italy, through the air quality measurements carried out by the Regional Protection Agency (ARPA-Lombardia). In winter 2020, the highest PM10 (94 μg/m3) and PM2.5 (70 μg/m3) concentrations were measured in Bergamo at Via Garibaldi and Via Meucci air quality monitoring stations, respectively (Supplement information S1 shows daily PM10 and PM2.5 concentrations). Unfortunately, the PM1 fraction were not available for that period. However, Vecchi et al. (2008) measured in winter (December 2003–March 2004) a PM1/PM2.5 ratio of 0.6–0.9 and PM1/PM10 ratio of 0.4–0.6 in three cities (Milano, Genoa, and Florence) with an average PM1 value 0f 48.8 μg/m3 in Milan, which would give an average estimate of PM2.5 of 65 μg/m3 (average ratio PM1/PM2.5 of 0.75) and a PM10 of 94 μg/m3 (average ratio PM1/PM10 of 0.5). Therefore, the obtained concentration values are in agreement with the highest measured concentrations obtained by ARPA in the 2020 winter period.
Rodriguez et al. (2007) obtained the particle number concentration in the ultrafine size range in Milan in the period November 2003–December 2003 with a Differential Mobility Analyzer connected to a Condensation Particle Counter. They found, in the ultrafine mode (N10–N100), about 1.5 × 1010 #/m3 and about 5.5 × 109 #/m3 in the accumulation mode (N100–N800) in agreement with results from Lonati et al. (2011) obtained during the cold season. The particle number concentration in the coarse fraction is obtained by adapting particle size distributions collected by an OPC (Grimm 107, Envirocheck model) in the urban area of Milan during 2011 and 2012 in winter and summer months (Cugerone et al., 2018) (see Fig. S2). Table 2 shows the estimated particle number concentrations in the three size modes: ultrafine, accumulation, and coarse. The last column gives the size intervals considered in each mode.
Table 2.
Atmospheric particle number concentrations for different size ranges: ultrafine, accumulation and coarse modes.
| Mode | Urban particle number concentration (m−3) | Size range |
|---|---|---|
| Ultrafine | 2 × 1010 | 0.01–0.1 μm |
| Accumulation | 6 × 109 | 0.1–0.8 μm |
| Coarse | 3 × 106 | 1–3 μm |
We consider the following sizes representative of the virions: 200 μm (large droplets), 2 μm (dry evaporated residuals) and 0.1 μm (single virus aerosol). Liu et al. (2020) detected peaks both in sub-micrometric and super-micrometric regions of virus particle concentrations in Wuhan (China). We also assume a number concentration of viral particles in the atmosphere of 10 copies/m3 in each mode, which was the maximum concentration observed in crowded public areas in Wuhan (Liu et al., 2020).
4.2. Collision process
We theoretically examined if PM atmospheric particles can scavenge virus aerosol, through inertial impact, interception, and Brownian diffusion. We calculated the scavenging coefficients of a 10 μm settling particle by using Fuchs' formula (Fuchs, 1964) for the interception and Brownian diffusion scavenging efficiencies, and Park et al. (2005) formulation for impaction. The probability of the virions to be scavenged due to coarse PM10 settling particles resulted negligible because the total scavenging kernel was very low. In addition, the volume swept by falling atmospheric coarse particles will contain a limited number of virions particles, thereby lowering the probability of collisions to a negligible value even in the unrealistic condition of a fall of 1000 m. Detailed information is provided in Supplemental Information S2.
Attachment of virions to PM10 particles could also be possible by thermal coagulation (governed by Brownian diffusion) or by kinematic coagulation (governed by external forces). We will consider only thermal coagulation. The dry residual droplets of the second mode (2 μm) could be a sink for PM aerosols from the accumulation and ultrafine modes, because of thermal coagulation. The rate of collision of an atmospheric particle of size di with a fixed particle of size dj (the dry residual droplet, which is supposed to have a negligible Brownian displacement) in the stationary case, is given by (Friedlander, 2000):
| (2) |
where F is the number of particles colliding per second, N0 is the PM aerosol number concentration, di is the PM aerosol size (assumed 0.1 μm for accumulation mode and 0.01 μm for ultrafine mode), dj is the droplet residual (2 μm) and D is the PM diffusion coefficient (5.2 10−8 m2/s and 6.8 10−10 m2/s for particle size of 0.01 μm and 0.1 μm respectively – Hinds (1999)). Results show a collision rate of about 5 × 10−5 collisions per second in the accumulation mode and 10−2 in the ultrafine mode. It would take more than one day for a collision to take place between a virion and an atmospheric aerosol particle in the accumulation mode, and only about 100 s for an ultrafine particle (0.01 μm). However, in this case the added mass to the virion would be negligible, as well as the changes in its size.
Finally, we consider the monodisperse coagulation of a single virus particle (0.1 μm) in the accumulation mode. For a monodisperse aerosol, the rate of change in number concentration is given by the Smoluchowski equation (Supplemental Information S2). The coagulation kernel of a 0.1 μm monodisperse aerosol is about 7.2 × 10−16 m3/s, considering also the Fuchs correction (Hinds, 1999). Figure S4 (supplementary material) shows the particle size increase as a function of time. Even after 8000 s the particle diameter increase would be only 1.2% without consequences in the dynamic behaviour of virus-laden aerosol in the atmosphere.
Therefore, scavenging and thermal coagulation processes have negligible effect in the attachment of virions to atmospheric aerosol particles in the considered conditions. Other processes, like electrostatic attractive forces or turbulent coagulation, not taken into account in this study, could eventually be responsible for inclusion of virions into atmospheric particles.
5. Conclusions
Average outdoor SARS-CoV-2 virus-laden aerosol concentrations, due to respiratory emissions of infected individuals in the Lombardia region (Northern Italy, Po valley pollution hot-spot), were investigated as function of the number of infected individuals (including asymptomatic). This was done using three simple box models: one covering all region, the second centred on the city of Milan, and the third centred on the city of Bergamo, where a COVID-19 outbreak was observed in March 2020. Emissions were estimated using a mass balance model for respiratory droplets and aerosols and the typical values of viral load observed in sputum. Calculations were done for average conditions and for best and worst case scenarios using different dispersion and ventilation assumptions compared to the average.
Outdoor concentrations in public area, excluding crowds, were very low, < 1 RNA copy/m3, even in the worst case scenario and assuming a number of infects up to 25% of local population. In average terms, assuming a number of infects equal to 10% of the population, the time necessary to inspire a quantum would be 31.5 days in Milan (range calculated using BCS and WCS scenarios: 2.7–91 days) and 51.2 days in Bergamo (range 4.4–149 days). Therefore, the probability of airborne transmission due to respiratory aerosol is very low in outdoor conditions excluding public crowded areas. This transmission mechanism could be more relevant for indoor community environments, in which further studies are necessary to investigate the potential risks. Therefore, it is advisable to mitigate the risk for vulnerable people via frequent ventilation, air exchanges, and disinfection of exposed surfaces including those of air conditioning systems.
The probability of the viral particles to be scavenged from atmospheric aerosol particles, due to inertial, interception and Brownian capture mechanisms, was negligible. The probability of coagulation of virus-laden aerosol with pre-existing particles was very low for accumulation and coarse mode particles, even considering the maximum RNA copies concentrations observed in crowded public areas, and large concentrations of pre-existing particles typically observed in winter conditions in the Lombardia area. The virus-laden aerosol particles eventually present in atmosphere are dry residual of evaporated droplets (i.e. droplet nuclei) rather than agglomerate with pre-existing particles. There is a small, but not negligible, probability that virus-laden aerosol could act as sink of ultrafine particles (around 0.01 μm in diameter). However, this will not change significantly the dynamics of the virus particles or their permanence time in atmosphere.
Authors credit statement
F. Belosi and D. Contini conceptualized the study design; M. Conte, G. Santachiara, and V. Gianelle contributed to data post-processing and calculations. All authors collaborated to interpretation of results, wrote, read, commented, and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Authors wish to thank Dr. Cinzia Perrino (IIA-CNR), Dr. Paolo Monti (University of Rome La Sapienza), and Dr. Paolo Martano (ISAC-CNR) for useful discussion on the different topics treated in this work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110603.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adams W.C. Final Report. Human Performance Laboratory, Physical Education Department, University of California; Davis: 1993. Measurement of breathing rate and volume in routinely performed daily activities. Human Performance Laboratory, Physical Education Department, University of California, Davis. Prepared for the California Air Resources Board, Contract No. A033-205, April 1993. [Google Scholar]
- Anderson E.L., Turnham P., Griffin J.R., Clarke C.C. 2020. Consideration of the Aerosol Transmission for COVID-19 and Public Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arav Y., Klausner Z., fatal E. 2020. Understanding the Indoor Pre-symptomatic Transmission Mechanism of COVID-19.https://www.medrxiv.org/content/10.1101/2020.05.12.20099085v1 [Google Scholar]
- Argentini S., Mastrantonio G., Lena F. Case studies of the wintertime convective boundary-layer structure in the urban area of Milan, Italy. Boundary-Layer Meteorol. 1999;93:253–267. [Google Scholar]
- Asadi S., Wexler A.S., Cappa C.D., Barreda S., Bouvier N.M., Ristenpart W.D. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 2019;9:2348. doi: 10.1038/s41598-019-38808-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi S., Bouvier N., Wexler A.S., Ristenpart W.D. The coronavirus pandemic and aerosols: does COVID-19 transmit via expiratory particles? Aerosol. Sci. Technol. 2020;54(6):635–638. doi: 10.1080/02786826.2020.1749229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bake B., Larsson P., Ljungkvist G., Ljungström E., Olin A.C. Exhaled particles and small airways. Respir. Res. 2019;20:8. doi: 10.1186/s12931-019-0970-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: more efforts are necessary to address interdisciplinary research. Environ. Res. 2020;188:109775. doi: 10.1016/j.envres.2020.109775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E., Vergalli S., Squazzoni F. Understanding COVID-19 diffusion requires an interdisciplinary, multi-dimensional approach. Environ. Res. 2020;188:109814. doi: 10.1016/j.envres.2020.109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourouiba L., Dehandschoewercker E., Bush J.W.M. Violent expiratory events: on coughing and Sneezing. J. Fluid Mech. 2014;745:537–563. doi: 10.1017/jfm.2014.88. [DOI] [Google Scholar]
- Borouiba L. Turbulent gas clouds and respiratory pathogen emissions, potential implications for reducing transmission of COVID-19. J. Am. Med. Assoc. 2020;323(18):1837–1838. doi: 10.1001/jama.2020.4756. [DOI] [PubMed] [Google Scholar]
- Buonanno G., Stabile L., Morawska L. Estimation of airborne viral emission: quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020;141 doi: 10.1016/j.envint.2020.105794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y., Sridhar S., Chan J.F.W., Ho P.L., Yuen K.Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Contr. Hosp. Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirizzi D., Conte M., Feltracco M., Dinoi A., Gregoris E., Barbaro E., La Bella G., Ciccarese G., La Salandra G., Gambaro A., Contini D. SARS-CoV-2 concentrations and virus-laden aerosol size distributions in outdoor air in north and south of Italy. Environ. Int. 2020;146 doi: 10.1016/j.envint.2020.106255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contini D., Cava D., Martano P., Donateo A., Grasso F.M. Comparison of indirect methods for the estimation of Boundary Layer height over flat-terrain in a coastal site. Meteorol. Z. 2009;18(3):309–320. [Google Scholar]
- Contini D., Costabile F. Does air pollution influence COVID-19 outbreaks? Atmosphere. 2020;11:377. doi: 10.3390/atmos11040377. [DOI] [Google Scholar]
- Cugerone K., De Michele C., Ghezzi A., Gianelle V., Gilardoni S. On the functional form of particle number size distributions: influence of particle source and meteorological variables. Atmos. Chem. Phys. 2018;18:4831–4842. [Google Scholar]
- Després V.R., Huffman A., Burrows S.M., Hoose C., Safatov A.S., Buryak G., Fröhlich-Nowoisky J., Elbert W., Andreae M.O., Pöschl U., Jaenicke R. Primary biological aerosol particles in the atmosphere: a review. Tellus B. 2012;64:15598. [Google Scholar]
- Domingo J.L., Marquès M., Rovira J. Influenec of airborne transmission of SARS-CoV-2 in COVID-19 pandemic. A review. Environ. Res. 2020;188:109861. doi: 10.1016/j.envres.2020.109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faridi S., Niazi S., Sadeghi K., Naddafi K., Yavarian J., Shamsipour M., Jandaghi N.Z.S., Sadeghniiat K., Nabizadeh R., Yunesian M., Momeniha F., Mokamel A., Hassanvand M.S., MokhtariAzad T. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 2020;725:138401. doi: 10.1016/j.scitotenv.2020.138401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrero L., Perrone M.G., Petraccone S., Sangiorgi G., Ferrini B.S., Lo Porto C., Lazzati Z., Cocchi D., Bruno F., Greco F., Riccio A., Bolzacchini E. Vertically-resolved particle size distribution within and above the mixing layer over the Milan metropolitan area. Atmos. Chem. Phys. 2010;10:3915–3932. [Google Scholar]
- Friedlander S.K. Oxford University Press; 2000. Smoke, Dust, and Haze. [Google Scholar]
- Fuchs N.A. Pergamon Press; 1964. The Mechanics of Aerosol; p. 202. [Google Scholar]
- Groulx N., Urch B., Duchaine C., Mubareka S., Scott J.A. The Pollution Particulate Concentrator (PoPCon): a platform to investigate the effects of particulate air pollutants on viral infectivity. Sci. Total Environ. 2018;628–629:1101–1107. doi: 10.1016/j.scitotenv.2018.02.118. [DOI] [PubMed] [Google Scholar]
- Han Z.Y., Weng W.G., Huang Q.Y. Characterizations of particle size distribution of the droplets exhaled by sneeze. J. R. Soc. Interface. 2013;10:20130560. doi: 10.1098/rsif.2013.0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds W.C. John Wiley & Sons, Inc; 1999. Aerosol Technology. [Google Scholar]
- Hsiao T.C., Chuang H.C., Griffith S.M., Chen S.J., Young L.H. COVID-19: an aerosol's point of view from expiration to transmission to viral-mechanism. Aerosol and Air Quality Research. 2020;20:905–910. [Google Scholar]
- Hu J., Lei C., Chen Z., Liu W., Hu X., Pei R., Su Z., Deng F., Huang Y., Sun X., Cao J., Guan W. Airborne SARS-CoV-2 and the use of masks for protection against its spread in Wuhan, China. Preprints. 2020;2020:2020050464. https://www.preprints.org/manuscript/202005.0464/v1 [Google Scholar]
- Jiang J., Fu Y.V., Liu L., Kulmala M. Transmission via aerosols: plausible differences among emerging coronaviruses. Aerosol. Sci. Technol. 2020;54(8):865–868. doi: 10.1080/02786826.2020.1769020. [DOI] [Google Scholar]
- Johnson G.R., Morawska L., Ristovski Z.D., Hargreaves M., Mengersen K., Chao C.Y.H., Wan M.P., Li Y., Xie X., Katoshevski D., Corbett S. Modality of human expired aerosol size distributions. J. Aerosol Sci. 2011;42:839–851. doi: 10.1016/j.jaerosci.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klompas M., Baker M.A., Rhee C. Airborne transmission of SARS-CoV-2. Theoretical considerations and available evidence. J. Am. Med. Assoc. 2020;324(5):441–442. doi: 10.1001/jama.2020.12458. [DOI] [PubMed] [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P., Yen H.L., Li Y., Ip D.K.M., Peiris J.S.M., Seto W.H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face mask. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Duan S., Yu I.T.S., Wong T.W. Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air. 2005;15:96–111. doi: 10.1111/j.1600-0668.2004.00318.x. [DOI] [PubMed] [Google Scholar]
- Lindsley W.G., Pearce T.A., Hudnall J.B., Davis K.A., Davis S.M., Fisher M.A., Khakoo R., Palmer J.E., Clark K.E., Celik I., Coffey C.C., Blachere F.M., Beezhold D.H. Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J. Occup. Environ. Hyg. 2012;9:443–449. doi: 10.1080/15459624.2012.684582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K., Sun L., Duan Y., Cai J., Westerdahl D., Liu X., Xu K., Ho K., Kan H., Fu Q., Lan K. 2020. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals Nature. [DOI] [PubMed] [Google Scholar]
- Lonati G., Crippa M., Gianelle V., Van Dingenen R. Daily patterns of the multi-modal structure of the particle number size distribution in Milan, Italy. Atmos. Environ. 2011;45:2434–2442. [Google Scholar]
- Martano P. Droplet fate in a cough puff. Atmosphere. 2020;11(8):841. doi: 10.3390/atmos11080841. [DOI] [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9(3) doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Johnson G.R., Ristovski Z.D., Hargreaves M., Mengersen K., Corbett S., Chao C.Y.H., Li Y., Katoshevski D. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J. Aerosol Sci. 2009;40:256–269. doi: 10.1016/j.jaerosci.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H., Oshitani H., Kobayashi T., Saito T., Sunagawa T., Mutsui T., Wakita T., MHLW COVID-19 Response Team. Suzuki M. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19) 2020. https://www.medrxiv.org/content/10.1101/2020.02.28.20029272v2
- Ong S.Y., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., YenWong M.S., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. J. Am. Med. Assoc. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan Y., Zang D., Yang P., Poon L.M., Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet. 2020;20:411–412. doi: 10.1016/S1473-3099(20)30113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.H., Jung C.H., Jung K.R., Lee B.K., Lee K.W. Wet scrubbing of polydisperse aerosols by freely falling droplets. Aerosol Science. 2005;36:1444–1458. [Google Scholar]
- Prather K.A., Wang C.C., Schooley R.T. 2020. Reducing Transmission of SARS-COV-2. [DOI] [PubMed] [Google Scholar]
- Ratnesar-Shumate S., Williams G., Green B., Krause M., Holland B., Wood S., Bohannon J., Boydston J., Freeburger D., Hooper I., Beck K., Yeager J., Altamura L.A., Biryukov J., Yolitz J., Schuit M., Wahl V., Hevey M., Dabisch P. Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces. J. Infect. Dis. 2020;222(2):214–222. doi: 10.1093/infdis/jiaa274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redrow J., Mao S., Celik I., Posada J.A., Feng Z.G. Modeling the evaporation and dispersion of airborne sputum droplets expelled from a human cough. Build. Environ. 2011;46:2042–2051. [Google Scholar]
- Rodríguez S., Van Dingenen R., Putaud J.-P., Dell'Acqua A., Pey J., Querol X., Alastuey A., Chenery S., Ho K.-F., Harrison R., Tardivo R., Scarnato B., Gemelli V. A study on the relationship between mass concentrations, chemistry and number size distribution of urban fine aerosols in Milan, Barcelona and London. Atmos. Chem. Phys. 2007;7:2217–2232. [Google Scholar]
- Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Guggemos W., Seilmaier M., Drosten C., Vollmar P., Zwirglmaier K., Zange S., Wölfel R., Hoelscher M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarpia J.L., Rivera D.N., Herrera V., Morwitzer M.J., Creager H., Santarpia G.W., Crown K.K., Brett-Major D., Schnaubelt E., Broadhurst M.J. Transmission potential of SARS-CoV-2 in viral shedding observed at the university of Nebraska medical center. 2020. https://www.medrxiv.org/content/10.1101/2020.03.23.20039446v2 Available online:
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., Palmisani J., Di Gilio A., Torboli V., Fontana F., Clemente L., Pallavicini A., Ruscio M., Piscitelli P., Miani A. SARS-Cov-2 RNA found on particulate matter of Bergamo in northern Italy: first evidence. Environ. Res. 2020;188:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Pallavicini A., Ruscio M., Piscitelli P., Colao A., Miani A. Searching for SARS-COV-2 on particulate matter: a possible early indicator of COVID-19 epidemic recurrence. Int. J. Environ. Res. Publ. Health. 2020;17:2986. doi: 10.3390/ijerph17092986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silibello C., Calori G., Brusasca G., Giudici A., Angelino E., Fossati G., Peroni E., Buganza E. Modelling of PM10 concentrations over Milano urban area using two aerosol modules. Environ. Model. Software. 2008;23:333–343. [Google Scholar]
- Stadnytskyi V., Bax C.E., Bax A., Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-COV-2 transmission. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(22):11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vecchi R., Chiari M., D'Alessandro A., Fermo P., Lucarelli F., Mazzei F., Nava S., Piazzalunga A., Prati P., Silvani S., Valli G. A mass closure and PMF source apportionment study on the sub-micron sized aerosol fraction at urban sites in Italy. Atmos. Environ. 2008;42:2240–2253. https://doi:10.1016/j.atmosenv.2007.11.039 [Google Scholar]
- Verreault D., Moineau S., Duchaine C. Methods for sampling of airborne viruses. Microbiol. Mol. Biol. Rev. 2008;72(3):413–444. doi: 10.1128/MMBR.00002-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe T., Bartrand T.A., Weir M.H., Omura T., Haas C.N. Development of a dose-response model for SARS coronavirus. Risk Anal. 2010;30:1129–1138. doi: 10.1111/j.1539-6924.2010.01427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations, World Health Organization, Scientific brief. 2020. https://www.who.int/newsroom/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipcprecaution-recommendations available at:
- Wölfel R., Corman V.M., Guggemos W., Seilmaier M., Zange S., Müller M.M., Niemeyer D., Jones T.C., Vollmar P., Rothe C., Hoelscher M., Bleicker T., Brünink S., Schneider J., Ehmann R., Zwirglmaier K., Drosten C., Wendtner C. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- Xie X., Li Y., Chwang A.T.Y., Ho P.L., Seto W.H. How far droplets can move in indoor environments – revisiting the Wells evaporation–falling curve. Indoor Air. 2007;17:211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- Yan J., Grantham M., Pantelic J., Bueno de Mesquita P.J., Albert B., Liu F., Ehrman S., Milton D.K., EMIT Consortium Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc. Natl. Acad. Sci. Unit. States Am. 2018;115(5):1081–1086. doi: 10.1073/pnas.1716561115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu I.T.S., Li Y., Wong T.W., Tam W., Chan A.T., Lee J.H.W., Leung D.Y.C., Ho T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N. Engl. J. Med. 2004;350:1731–1739. doi: 10.1056/NEJMoa032867. [DOI] [PubMed] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(26):14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.