Abstract
Background
Despite the COVID-19 infection is more frequently related to acute respiratory distress but there is an increasing evidence of a heterogeneous spectrum of multi-system involvement including the central nervous system. Thromboembolic events after COVID-19 infection have been reported mainly in the pulmonary vasculature however; thromboembolic complications of the nervous system with subsequent cerebrovascular stroke have been increasingly reported. The most common cerebrovascular complication after COVID-19 infection is ischemic stroke however there is also reported cases of cerebral venous sinus thrombosis in such patients as well. In the current report we present two cases with extensive cerebral venous sinus thrombosis as a potential complication for COVID-19 infection.
Objective
Increase the awareness of neurological complications in patient with COVID-19 virus disease.
Methods
Reporting two cases with confirmed cerebral venous sinus obstruction in patient with confirmed COVID-19 infection.
Results
Two young adult males less than 30 years old have no other risk factors of hypercoagulable state apart from being COVID-19 infection victims complicated by CVST. Both of them had progressive course of deterioration in conscious level, right hemiplegia and only one seizures attack has been reported in (Case-1). Both patients in the current report died within one week of their initial symptoms in spite the aggressive medical and surgical treatment.
Conclusion
CVST is a devastating complication when associated with COVID-19 infection and early investigations for cerebrovascular integrity by using MRA, MRV whenever there are unexplained neurological manifestations in patient with COVID-19 disease.
Keywords: COVID-19, Cerebral venous sinus thrombosis, Stroke
1. Introduction
The new coronavirus (COVID-19) is one of the human β-coronaviruses, which also includes SARS-CoV-1 and Middle East respiratory syndrome (MERS)-CoV [1]. Acute respiratory syndrome due to COVID-19 infection was primary identified in Wuhan city, china on January 2020 [1]. The coronavirus disease (COVID-19) has been declared a pandemic in March 2020 [2]. Despite the COVID-19 infection is more frequently related to acute respiratory distress but there is an increasing evidence of a heterogeneous spectrum of multisystem involvement including the neurological complications [3]. Thromboembolic events after COVID-19 infection have been reported mainly in the pulmonary vasculature however; thromboembolic complications of the nervous system with subsequent cerebrovascular stroke have been increasingly reported [4]. The most common cerebrovascular complication after COVID-19 infection is ischemic stroke however there is also reported cases of cerebral venous sinus thrombosis in such patients as well [5], [6]. In the current report we present two cases with extensive cerebral venous sinus thrombosis as a potential complication for COVID-19 infection. To the best of our knowledge, this case series is the only case series to date on patients with Covid-19 infection who developed CVST in Arab region. Moreover, in our two cases; both patients presented to the health care facility by neurological manifestations initially and not COVID 19 common symptoms.
2. Case 1
A 22-year-old gentle man who was brought to the emergency department with deterioration in his conscious level after an attack of convulsion and fall down from four meters height. On arrival to the hospital; his GCS was 4/15, so the patient was immediately intubated, connected to the ventilator and anti-epileptic medication was given. After stabilization of his condition; radiological survey was completed; the initial CT scan of the brain (Fig. 1 A) revealed left cerebral small subdural hematoma with mild brain edema, pneumocephalus and fissure fracture of the skull. Later, the patient was admitted to the surgical ICU for conservative treatment and follow up. Over the following couple of days, his neurological condition showed notable improvement.
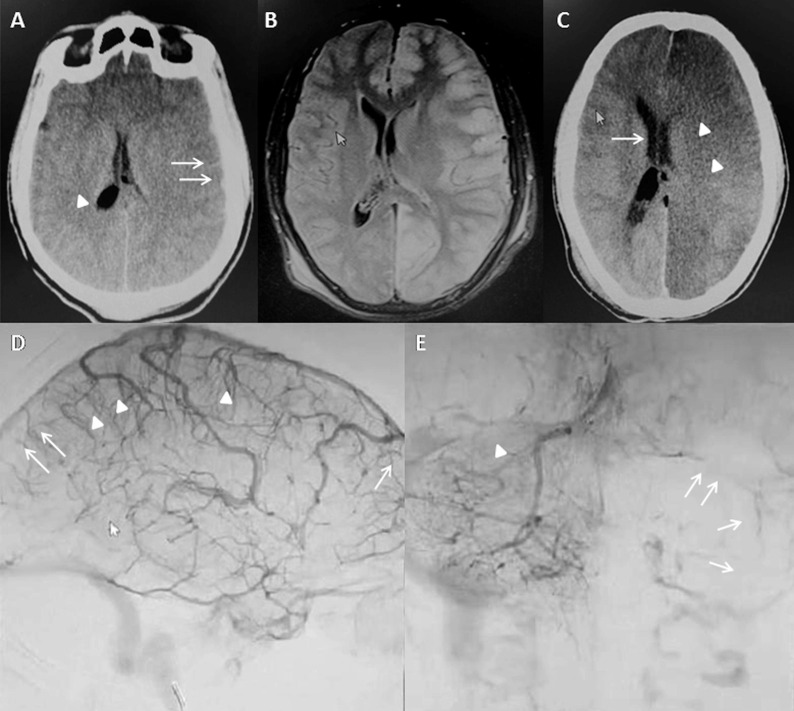
Fig. 1.
Case 1; preoperative findings. Initial CT brain (Fig. 1A) showed left cerebral small SDH with mild brain edema, pneumocephalus. On the 3rd day, MRI brain (Fig. 1B) showed left cerebral recent ischemic insult with stationary thin rim SDH. On the 4th day FU CT brain (Fig. 1C), showed progressive left hemispheric ischemic changes with midline shift. Cerebral angiogram showed partial SSS thrombosis and complete thrombosis of the left transverse-sigmoid sinus (Fig. 1D&E).
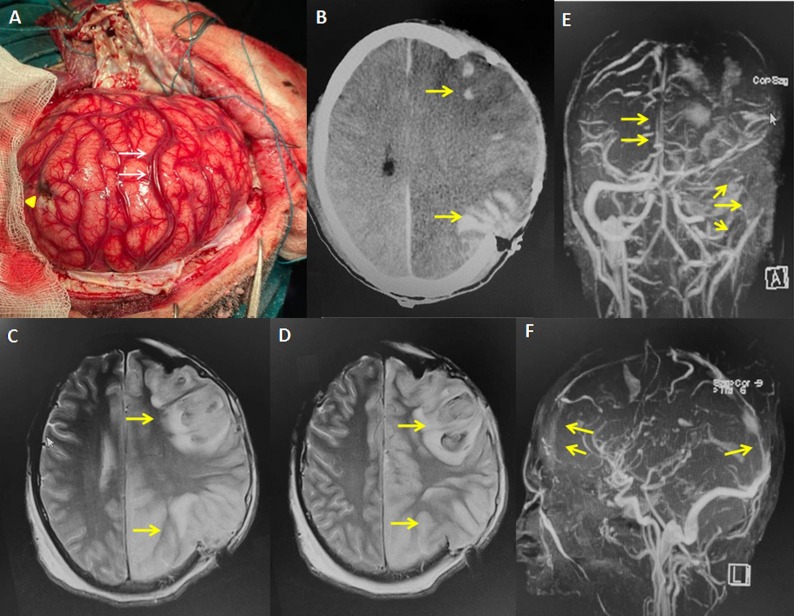
Unfortunately, on the 3rd day of ICU admission, he developed a new neurological deficit in the form of right sided hemiparesis. In response, an MRI of the brain (Fig. 1B) was performed and showed left cerebral recent ischemic insult with stationary left sided small subdural hematoma. On the 4th day of ICU admission decline in the sensorium was observed and a new CT scan of the brain (Fig. 1C), was performed on urgent basis that reveled; progressive left hemispheric ischemic changes with mid line shift. Intern, Diagnostic cerebral angiography was performed in order to exclude carotid dissection which showed patent both anterior and posterior arterial trees with partial SSS thrombosis and complete thrombosis of the left transverse sigmoid sinus (Fig. 1D&E). The patient was shifted immediately from the Angio suite to the operating room, where decompressive craniectomy was performed. Intraoperatively, congested cortical veins were observed (Fig. 2 A). Early postoperative neurological improvement was observed (GCS was improved from 4 to 9/15). On the second postoperative day, the patient conscious level started to decline again, where CT scan of the brain (Fig. 2B) and MRI/MRV scan of the brain (Fig. 2C,D,E,F) were performed and revealed notable increased obstruction of left transverse sinus, and markedly diminished flow on superior sagittal sinus, sigmoid sinus, straight sinus (progressive course of dural sinus thrombosis). Based on this finding, therapeutic anticoagulation (enoxaparin) was started. Even though, the patient condition showed progressive deterioration together with development of respiratory distress and high-grade fever. In response to the new respiratory clinical findings, CT scans of the chest was requested which revealed bilateral basal ground glass opacities & centrilobular thickening and concomitant nasopharyngeal swab confirmed the COVID-19 infections.
Fig. 2.
Case 1; operative and post-operative findings. Intraoperative picture during DC with congested cortical vein (Fig. 2A, arrow head). On the 2nd postoperative day CT (Fig. 2B) and MRI/MRV brain (Fig. 2C,D,E,F) showed picture of progressive multiple dural sinus thrombosis.
Despite all the above measures and efforts exerted to save the patient life, he did not show notable response with progressive deterioration in his neurological status and respiratory parameters and finally he developed cardiopulmonary arrest on the third postoperative day.
3. Case 2
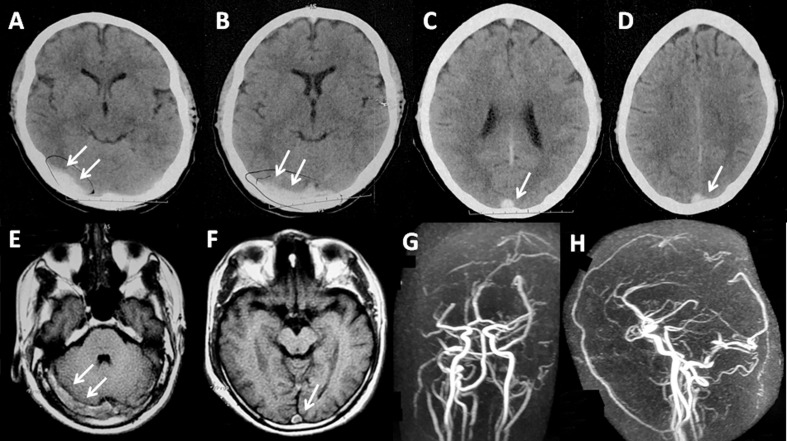
A-28-year old male previously healthy patient has a history of mild fever and generalized bony ache for 3 days. Patient asked for medical advice and treated symptomatically with antibiotic and anti-pyretic by general practitioner doctor at his village with no improvement. The Patient started to develop increasing headache associated with slightly disturbed conscious level that mandate the admission to emergency department where CT scan of the brain was performed and showed hyper-dense transverse sinus (Fig. 3 A&B) and positive delta sign (Fig. 3 C&D) raising the possibility of venous sinus thrombosis which was confirmed by MRI brain (Fig. 3E,F) and MRV confirmed the extensive sinus thrombosis as shown in (Fig. 3G&H).
Fig. 3.
Case 2. Initial CT brain showed hyperdense transverse sinus (Fig. 3A,B) and positive delta sign (Fig. 3 C&D). MRI brain (Fig. 3E,F) and MRV confirmed the extensive sinus thrombosis (Fig. 3G,H).
As per-recent protocol in Covid-19 pandemic, complementary CT scan of the chest and routine laboratory investigations were requested. The results of his investigations raised the possibility of Covid-19 infection that was confirmed by the result of the nasopharyngeal swab. Patient treated at the isolation unit with the routine protocol for Covid-19 disease in addition to, therapeutic low- molecular-weight heparin (enoxaparin), and prophylactic levetiracetam infusion.
Despite the above treatment protocol was strictly followed at the isolation unit, rapid progressive deterioration in his general and neurological status happened and he died on the 5th day of admission.
4. Discussion
The most frequent clinical manifestations of COVID-19 infection are cough, fever, dyspnea, diarrhea, and fatigue associated with radiological lung abnormalities [7]. Moreover, the neurologic manifestations such as seizures, headache, and loss of smell are not uncommon [5], [8]. The neurotropism of covid-19 virus was confirmed by the presence of the virus in cerebrospinal fluid [9], [10] and its neuroinvasive potential could happen through the retrograde neuronal route as similar to the MERS-CoV and SARS-CoV-1 [10], [11].
A wide spectrum of neurological complications has been reported with the new version of corona virus (Covid-19) [3], which could involve the acute cerebrovascular insult [8].
COVID-19 disease shows a state of hypercoagulability with a high prevalence of venous thromboembolism associated with thrombotic complications mostly related to the pulmonary vasculature [6], [12], [13], [14]. However; these thrombotic complications may involve the brain vasculature as well in 2% of patient with confirmed COVID-19 infection [3].
The mechanism of thrombophilic state with COVID-19 infection has not been fully elucidated. However, the severe inflammatory response after COVID-19 infection leads a cytokine storm that intern can induce a pro-coagulable state [15], [16]. In addition, the virus itself has its specific pro-coagulant effect [16].
Covid 19 infection induces widespread endothelial dysfunction (endotheliopathy) and inflammation [17]. Von Willebrand factor (VWF) and factor VIII (FVIII) are known to be elevated COVID-19 patients [18], [19]. FVIII and VWF are not only related to inflammation and risk of thrombosis but also associated with endothelial damage [20]. A decrease in FVIII/VWF ratio values on COVID 19 patients’ admission could determine which patient will be at higher risk of worsening respiratory status, and subsequently shows an increase in oxygen requirements [20].
Ultra large VWF (ULVWF) has a higher adhesive ability to platelets than VWF [21]. Exocytosis of ULVWF stored at endothelial Weibel-Palade bodies (WPB) into the circulation can be triggered by hypoxia, Interleukin (IL)-1, as well as, tumor necrosis factor (TNF)-alpha. Moreover, IL-6 can inhibit the cleavage of ULVWF–platelet strings [22]. Tremblay et al showed that there is no difference in the outcome of COVID 19 patients who were receiving anti-platelet or anti- coagulants compared to those who were not [23].
So, preventing the binding of platelets to ULVWF at the glycoprotein IX-Ib receptor through agents like; caplacizumab [22] or anfibatide [22], recombinant ADAMTS13 concentrate [24], or dissolving the ULVWF multimers by using N Acetylcysteine [25] might represent an attractive way to prevent microthrombosis formation.
The most frequent cerebrovascular disease after COVID-19 infection is ischemic stroke as demonstrated in the series of Helms et al., [5] where, one sub-acute and two acute ischemic strokes out of 13 patients with confirmed covid-19 infection were reported. Moreover there are reported cases of cerebral venous sinus thrombosis among COVID-19 infected patients [6].
Cerebral venous sinus thrombosis is a rare thrombotic disease and has a relatively good outcome when treated promptly although it could be fatal if not [26]. The use of oral contraceptive pills Pregnancy & puerperium, presence of genetic predisposition, malignancy, connective tissue disease and local infections of the head & neck are considered risk factors for development of CVST [26], [27], [28].
The CVST manifestation includes symptoms and signs of intracranial hypertension, encephalopathy or focal neurological deficit and can cause cerebral infarction and/or hemorrhage [26]. Heparin anticoagulation is the initial treatment of CVST even in the presence of intracerebral hemorrhage [29]. Despite limited reports in the literature described the association between COVID-19 infection and CVST [4], [30], the current report demonstrates two patients with confirmed COVID-19 infection complicated by CVST.
In the current report both patients are young adult males and have no other risk factors of hypercoagulable state apart from being COVID-19 infection victims which could support the association between COVID-19 infection and CVST. Both patients in the current report died within one week of their initial symptoms in spite the aggressive medical and surgical treatment. Seizures attack was reported in few cases with COVID-19 infection [3]. The attacks of convulsion after COVID-19 infection may be due to blood–brain barrier breakdown with excessive release of pro-inflammatory cytokine leading to cortical irritation and seizures [31], [32]. In the current report only one seizures attack has been reported in (Case-1).
In our both cases, no antiviral protocol was administrated.
5. Conclusion
The devastating consequences of CVST associated with COVID-19 infection whenever diagnosis is delayed should initiate high index of suspicion among clinicians in order to start early investigations for cerebrovascular integrity by using MRA, MRV whenever there are unexplained neurological manifestations. Moreover whenever there is unexplained thrombogenicity in a neurological case presented with CVST, one showed think about associated COVID 19 infection even in the absence of classic constitutional symptoms.
This study has several limitations. It has only two cases; however it can still raise the suspicion among CVST cases presented only with neurological manifestation without clear predisposing factors being possibly COVID 19 cases in the recent pandemic era. And the possible association could be related to the known COVID 19 associated thrombogenicity that has been proven recently in many literatures. There were several missing laboratory data among our patients, because of their ambiguous initial presentation, not classic to COVID 19 patient and the rapid progressive deterioration scenarios in both of cases.
Funding
No funding was received for this research.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
For this type of study formal consent is not required “This article does not contain any studies with human participants performed by any of the authors.”
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- 1.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L.i. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease 2019 (COVID-19) situation report. (accessed April 20, 2020).
- 3.Di Carlo D.T., Montemurro N., Petrella G., Siciliano G., Ceravolo R., Perrini P. Exploring the clinical association between neurological symptoms and COVID-19 pandemic outbreak: a systematic review of current literature. J. Neurol. 2020;1–9 doi: 10.1007/s00415-020-09978-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cavalcanti D.D., Raz E., Shapiro M., Dehkharghani S., Yaghi S., Lillemoe K., Nossek E., Torres J., Jain R., Riina H.A., Radmanesh A., Nelson P.K. Cerebral Venous Thrombosis Associated with COVID-19. AJNR Am. J. Neuroradiol. 2020;41(8):1370–1376. doi: 10.3174/ajnr.A6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., Collange O., Boulay C., Fafi-Kremer S., Ohana M., Anheim M., Meziani F. Neurologic Features in Severe SARS-CoV-2 Infection. N. Engl. J. Med. 2020;382(23):2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolaji P., Kukoyi B., Ahmad N., Wharton C. Extensive cerebral venous sinus thrombosis: a potential complication in a patient with COVID-19 disease. BMJ Case Rep. 2020;13(8):e236820. doi: 10.1136/bcr-2020-236820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y.i., Zhang L.i., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L.i., Xie J., Wang G., Jiang R., Gao Z., Jin Q.i., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mao L., Jin H., Wang M., Hu Y.u., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Li Y., Hu B.o. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.P. Xiang, X.M. Xu, L.L. Gao, et al., First case of 2019 novel coronavirus disease with encephalitis. ChinaXiv. 202003 (2020) 15.
- 10.Li Y.-C., Bai W.-Z., Hashikawa T. The neuroinvasive potential of SARS-CoV2 may be at least partially responsible for the respiratory failure of COVID-19 patients. J. Med. Virol. 2020 doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L., Liu C., Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cui S., Chen S., Li X., Liu S., Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18(6):1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., Endeman H. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb. Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. The Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.J.M. Connors, J.H. Levy, COVID-19 and its implications for thrombosis and anticoagulation. Blood 135 (2020) 2033–2040. [DOI] [PMC free article] [PubMed]
- 17.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. The Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Helms J., Tacquard C., Severac F., Leonard-Lorant I., Ohana M., Delabranche X., Merdji H., Clere-Jehl R., Schenck M., Fagot Gandet F., Fafi-Kremer S., Castelain V., Schneider F., Grunebaum L., Anglés-Cano E., Sattler L., Mertes P.-M., Meziani F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panigada M., Bottino N., Tagliabue P., Grasselli G., Novembrino C., Chantarangkul V., Pesenti A., Peyvandi F., Tripodi A. Hypercoagulability of COVID‐19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J. Thromb. Haemost. 2020;18(7):1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rauch A., Labreuche J., Lassalle F., Goutay J., Caplan M., Charbonnier L., Rohn A., Jeanpierre E., Dupont A., Duhamel A., Faure K., Lambert M., Kipnis E., Garrigue D., Lenting P.J., Poissy J., Susen S. Coagulation biomarkers are independent predictors of increased oxygen requirements in COVID‐19. J. Thromb. Haemost. 2020;18(11):2942–2953. doi: 10.1111/jth.15067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhogal P., Jensen M., Collins G., Spooner O., Makalanda L., Hart D., Jaffer O. Letter in response to: Coagulation markers are independent predictors of increased oxygen requirements and thrombosis in COVID‐19. J. Thromb. Haemost. 2020;18(12):3382–3384. doi: 10.1111/jth.15080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.A. Bernardo, C. Ball, L. Nolasco, J.F. Moake, J.-F. Dong, Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von Willebrand factor multimers under flow. Blood. 104 (2004) 100–106. [DOI] [PubMed]
- 23.Tremblay D., van Gerwen M., Alsen M., Thibaud S., Kessler A., Venugopal S., Makki I., Qin Q., Dharmapuri S., Jun T., Bhalla S., Berwick S., Feld J., Mascarenhas J., Troy K., Cromwell C., Dunn A., Oh W.K., Naymagon L. Impact of anticoagulation prior to COVID-19 infection: a propensity score–matched cohort study. Blood. 2020;136(1):144–147. doi: 10.1182/blood.2020006941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.B. Plaimauer, J.A. Kremer Hovinga, C. Juno, et al., Recombinant ADAMTS13 normalizes von Willebrand factor-cleaving activity in plasma of acquired TTP patients by overriding inhibitory antibodies. J. Thromb. Haemost. 9 (2011) 936–944. [DOI] [PubMed]
- 25.Martinez de Lizarrondo S., Gakuba C., Herbig B.A., Repessé Y., Ali C., Denis C.V., Lenting P.J., Touzé E., Diamond S.L., Vivien D., Gauberti M. Potent Thrombolytic Effect of N -Acetylcysteine on Arterial Thrombi. Circulation. 2017;136(7):646–660. doi: 10.1161/CIRCULATIONAHA.117.027290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saposnik G., Barinagarrementeria F., Brown R.D., Jr, Bushnell C.D., Cucchiara B., Cushman M., deVeber G., Ferro J.M., Tsai F.Y. Diagnosis and Management of Cerebral Venous Thrombosis: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158–1192. doi: 10.1161/STR.0b013e31820a8364. [DOI] [PubMed] [Google Scholar]
- 27.Deschiens M.-A., Conard J., Horellou M.H., Ameri A., Preter M., Chedru F., Samama M.M., Bousser M.-G. Coagulation Studies, Factor V Leiden, and Anticardiolipin Antibodies in 40 Cases of Cerebral Venous Thrombosis. Stroke. 1996;27(10):1724–1730. doi: 10.1161/01.str.27.10.1724. [DOI] [PubMed] [Google Scholar]
- 28.Ameri A., Bousser M.-G. Cerebral Venous Thrombosis. Neurol. Clin. 1992;10(1):87–111. [PubMed] [Google Scholar]
- 29.Ferro J., Bousser M., Canhão P. European stroke organization guideline for the diagnosis and treatment of cerebral venous thrombosis – endorsed by the European Academy of Neurology. Eur. J. Neurol. 2017;2:195–221. doi: 10.1177/2396987317719364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hughes C., Nichols T., Pike M. Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur. J. Case Rep. Intern. Med. 2020;7 doi: 10.12890/2020_001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.M. Hepburn, N. Mullaguri, P. George, et al., Acute symptomatic seizures in critically Ill patients with COVID-19: is there an association? Neurocrit. Care. (2020). [DOI] [PMC free article] [PubMed]
- 32.Moriguchi T., Harii N., Goto J., Harada D., Sugawara H., Takamino J., Ueno M., Sakata H., Kondo K., Myose N., Nakao A., Takeda M., Haro H., Inoue O., Suzuki-Inoue K., Kubokawa K., Ogihara S., Sasaki T., Kinouchi H., Kojin H., Ito M., Onishi H., Shimizu T., Sasaki Y.u., Enomoto N., Ishihara H., Furuya S., Yamamoto T., Shimada S. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int. J. Infect. Diseases. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]