Abstract
There is a serious concern over the variation of case fatality of COVID-19 patients that reflects the preparedness of the medical care system in response to the surge of pneumonia patients. We aimed to quantify the disease spectrum of COVID-19 on which we are based to develop a key indicator on the probability of progression from pneumonia to acute respiratory disease syndrome (ARDS) for fatal COVID-19. The retrospective cohort on 12 countries that have already experienced the epidemic of COVID-19 with available open data on the conformed cases with detailed information on mild respiratory disease (MRD), pneumonia, ARDS, and deaths were used. The pooled estimates from three countries with detailed information were 73% from MRD to pneumonia and 27% from MRD to recovery and the case-fatality rate of ARDS was 43%. The progression from pneumonia to ARDS varied from 3% to 63%. These key estimates were highly associated with the case fatality rates reported for each country with a statistically significant positive relationship (adjusted R2 = 95%). Such a quantitative model provides key messages for the optimal medical resources allocation to a spectrum of patients requiring quarantine and isolation at home, isolation wards, and intensive care unit in order to reduce deaths from COVID-19.
Keywords: Acute respiratory distress syndrome, Fatal, COVID-19, Predictor, Pandemic
Introduction
The global pandemic of COVID-19 cause by the SARS-CoV-2 [1] has expanded from the epidemic center of Wuhan, China to the countries worldwide in the first three months of 2020 [[1], [2], [3]]. While COVID-19 spread across the globe, it has a wide variation in case-fatality, ranging from 10% in Italy to less than 1% in Germany [4]. The spectrum of clinical severity is the crucial factor to gauge the severity of this pandemic in addition to affected population and disease transmission [5]. Current evidence has demonstrated the association between disease progression of COVID-19 and relevant factors pertaining to clinical characteristics [6,7], environmental factors [8,9], and medical resource allocation [10,11]. Whether COVID-19 is fatal or not is highly dependent on the odds of progression from mild disease to severe disease and sufficient capacity of isolation wards and intensive care units to reduce its progression from pneumonia to severe acute respiratory disease syndrome (ARDS) [11]. By quantifying the progression of the entire disease spectrum of COVID-19 from mild symptoms to death from publicly available clinical data, we provide evidence-based explanation for difference in case-fatalities among affected countries.
Material and methods
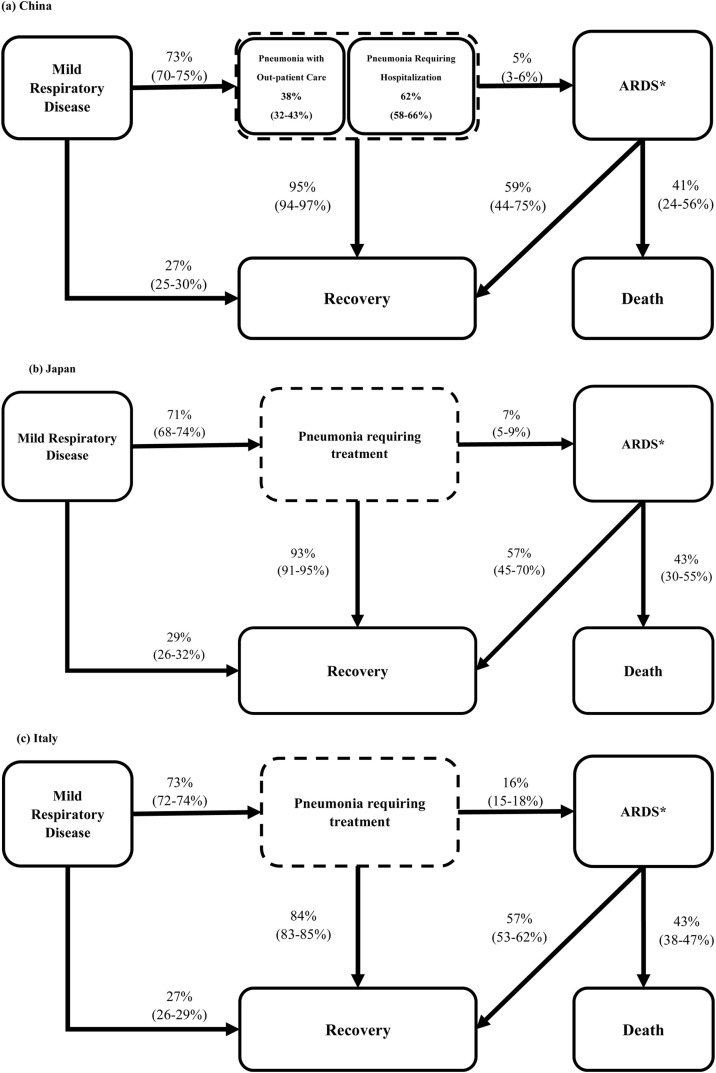
We have developed a quantitative model as shown in Fig. 1 for evaluating the disease progression of COVID-19 through three main categories of severity, from mild respiratory disease (MRD) to pneumonia and then to severe pneumonia with ARDS. The key indicator accounting for the variation in case-fatality rate is the progression rate from pneumonia to ARDS. To estimate these progression rates, published data from China, Japan, and Italy have been abstracted [7,12,13]. The aggregate numbers abstracted from the publicly available data provide information on the frequencies of MRD, pneumonia, ARDS in need of intensive care, recovery, and death. Only three countries (China, Italy, and Japan) have so far provided fully available information on the progression of disease severity as shown in Fig. 1. Regarding information on China, the aggregated tabular data abstracted from the original article are listed in Table A.1, including clinical characteristics of 1099 patients from 552 hospitals covering 30 provinces in China [7]. Information was available from February 6 to March 13 2020 for Japan [12], and March 3 to March 6 for Italy [13]. Information on other countries was retrieved from open data sources during the current epidemic period until March 17 [4].
Fig. 1.
Disease progression model for COVID-19 from mild respiratory disease to pneumonia, ARDS and the terminal events of recovery and death.
* ARDS: acute respiratory distress syndrome
The probability of each progression following the binomial distribution was first estimated on the basis of the frequencies on each state using the empirical data from three countries (China, Japan, and Italy). The pooled probabilities for disease progression from MRD to pneumonia, from MRD to recovery, and from ARDS to death were estimated by combining the data from three countries. These pooled estimates were further applied to imputing the key indicator for progression from pneumonia to ARDS for other eight countries with only information on total pneumonia cases and deaths from ARDS. The case-fatality rate was regressed on the estimated probability of progression from pneumonia to ARDS by using a linear regression equation model to calculate the adjusted R2.
Results
The probabilities of disease progression in China, Japan and Italy
During the outbreaks in China, 27 % (95% CI: 25-30%) of infected persons with MRD recovered and the remaining 73% (95% CI: 70-75%) progressed to pneumonia. Of those with pneumonia, 38% (302/800, 95% CI: 32-43%) were treated as outpatients and the remaining 62% (498/800, 95% CI: 58-66%) required hospitalization. The recovery rate of the hospitalized patients was 95% (95% CI: 94-97%), and the remaining 5% (95% CI: 3-6%) deteriorated to ARDS with a death rate of 41% (95% CI: 25-56%) (Fig. 1(a), Table A.1). The pooled estimates for disease progression from these three countries were 73% from MRD to pneumonia and 27% from MRD to recovery (Table 1 ). It should be noted that the combined fatality rate of ARDS (43%) by pooling the estimates across three countries was comparable to that reported in a systematic review article based on meta-analysis (44%) [14]. The remarkable difference in case fatality rates among these three countries was attributable to their difference in the probability of progression from pneumonia to ARDS, which was 7% (95% CI: 5-9%) and 16% (95% CI: 15-18%) for Japan and Italy, respectively (Fig. 1 (b) and (c), Table 1).
Table 1.
Disease progression rates of COVID-19 for countries with more than 20 fatal cases.
| Country | Mild Respiratory Disease to Pneumonia | Mild Respiratory Disease to Recovery | Pneumonia to ARDSb | Pneumonia to Recoveryb | ARDS to Death | ARDS to Recovery |
|---|---|---|---|---|---|---|
| China | 73% | 27% | 5% | 95% | 41% | 59% |
| Japan | 71% | 29% | 7% | 93% | 43% | 57% |
| Italy | 73% | 27% | 16% | 84% | 43% | 57% |
| Iran | 73%a | 27%a | 21% | 79% | 43%a | 57%a |
| Spain | 39% | 61% | ||||
| UK | 49% | 51% | ||||
| Netherlands | 42% | 58% | ||||
| France | 63% | 37% | ||||
| US | 20% | 80% | ||||
| South Korea | 8% | 92% | ||||
| Germany | 15% | 85% | ||||
| Taiwan | 3% | 97% |
Based on the results derived from China, Japan, and Italy.
Derived by using data on total cases and deaths reported by WHO, updated from February 4 to May 9, 2020 [4].
The probability of progression from pneumonia to ARDS
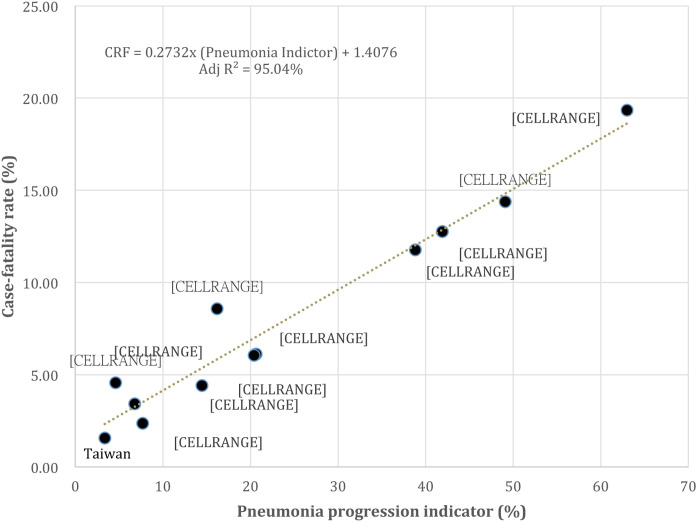
The probability of progression from pneumonia to ARDS was the highest in France with 63%, followed by 50% in UK, 42% in Netherlands, and the lowest, 3%, in Taiwan (Table 1). These estimates were highly associated with all the case fatality rates reported for each country with a statistically significant positive relationship (adjusted R2 = 95%, Figure A.1).
External validation
We have performed an external validation of the parameters of Fig. 1 (a), calculated with data from China, using data from countries other than China but in the same epidemic wave as the China epidemic, such as the reported cases and deaths from South Korea up to March 20 and the Diamond Princess up to February 27, all available from open data allowing for a three-day delay for the COVID-19 death count [4]. Supplemental Table A.2 shows the observed and predicted deaths for these two sets of empirical data. The number of expected deaths was 118 and 9.62 for South Korea and the Diamond Princess Cruise Ship, respectively, which were consistent with the observed data (P = 0.82 by the chi-square test, = 1.79).
Discussion and conclusion
In response to the soaring number of COVID-19 cases reported in previous studies and reports [4,12,13] and in the absence of approved anti-viral therapy and vaccination, a variety of non-pharmaceutical mitigation strategies have been implemented in most countries and regions attacked by COVID-19. With the rapid transmission and subsequent propagation of the COVID-19 pandemic, the ultimate goal of these containment strategies have shifted from transmission prevention centered on border control and contact tracing to plans aimed at the reduction of case fatality with the preservation of intensive care capacity. Our quantitative model should assist in planning for the upcoming demand for healthcare personnel and facilities in order to minimize the consequences of COVID-19, particularly by reducing the progression from pneumonia to ARDS.
This quantitative disease progression model can assist in estimating the proportion of each of the three stages of the disease and the chances of recovery from each state, for the purpose of efficient allocation of medical resources. These include medical and paramedical personnel, isolation wards and ICUs in designated hospitals responsible for COVID-19 patients, and more importantly, guidance in triaging those identified as COVID-19 cases. Based on the disease progression parameters derived from the outbreak in China, more than half (55%) of the COVID-19 cases can be treated as outpatients and be expected to recover. The remaining patients will require hospital-based treatment with a conservative estimate of an ICU demand of 3% of all confirmed COVID-19 cases.
To sum up, our finding provides a new insight into a wide variation of case-fatality rate of COVID-19 patients across countries. In contrast to more consistent estimates noted in the progression rates from MRD to pneumonia requiring hospitalization (73%) and also the death rate of the severest ARDS (43%), the progression rate from pneumonia to ARDS varied considerably among the countries examined here with a range > 20-fold (3% to 63%). Therefore, it is the key factor responsible for the variation of case-fatality rate of COVID-19. This was further supported by highly positive association between progression rate from pneumonia to ARDS and fatal COVID-19, accounting for up to 95% variation of association. Serious efforts need to be made to reduce this rate, among which the optimal allocation of medical resources should play a major role. Preventing the progression of pneumonia to ARDS should be the management strategy given the highest priority, and the strategies employed by counties with low rates of progression should be carefully studied. Our quantitative disease progression model can assist in this process.
The progression rate from pneumonia to ARDS, the key determinant of fatal outcome from COVID-19, varies considerably among the countries examined here with a range from 3% to 63%. The highly positive association between progression rate from pneumonia to ARDS and fatal COVID-19 was demonstrated. Serious efforts need to be made to reduce this rate, among which the optimal allocation of medical resources should play a major role. Preventing the progression of pneumonia to ARDS should be the management strategy given the highest priority, and the strategies employed by counties with low rates of progression should be carefully studied. Our quantitative disease progression model can assist in this process.
Financial support
The study has financial support by Ministry of Science and Technology, Taiwan (MOST 107-3017-F-002-003; MOST 108-2118-M-002-002-MY3), Ministry of Education, Taiwan (NTU-107L9003) and also the in-depth discussion and opinion provided by Professor Hsien-Ho Lin from the Institute of Epidemiology and Preventive Medicine, College of Public Health, National Taiwan University, Taipei, Taiwan. This work was financially supported by the “Innovation and Policy Center for Population Health and Sustainable Environment (Population Health Research Center, PHRC), College of Public Health, National Taiwan University” from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan.
Conflicts of interests
We declare no competing interests.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jiph.2020.12.026.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Zhou P., Yang X., Wang X., Zhang L., Zhang W., Si H.R., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;26(382):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2020. Coronavirus disease (COVID-2019) situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Accessed on May 29, 2020. [Google Scholar]
- 5.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19 - studies needed. N Engl J Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 6.Chang M.C., Park Y.K., Kim P.O., Park D. Risk factors for disease progression in COVID-19 patients. BMC Infect Dis. 2020;20:445. doi: 10.1186/s12879-020-05144-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., Hee J.X., et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yao Y., Pan J., Wang W., Liu Z., Kan H., Qiu Y., et al. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci Total Environ. 2020;741 doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeung D.W., Zhang Y., Bo Y., Hossain M.S., Zeng Y., Lao X.Q. A mechanism-based parameterisation scheme to investigate the association between transmission rate of COVID-19 and meteorological factors on plains in China. Sci Total Environ. 2020;737:140348. doi: 10.1016/j.scitotenv.2020.140348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dondorp A.M., Hayat M., Aryal D., Beane A., Schultz M.J. Respiratory support in COVID-19 patients, with a focus on resource-limited settings. Am J Trop Med Hyg. 2020;102(6):1191–1197. doi: 10.4269/ajtmh.20-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peng Y., Xu B., Sun B., Han G., Zhou Y.H. Importance of timely management of patients in reducing fatality rate of coronavirus disease 2019. J Infect Public Health. 2020;13(6):890–892. doi: 10.1016/j.jiph.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Japan: Ministry of Health, Labor, and Welfare. About Coronavirus Disease 2019 (COVID-19). 2020. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/newpage_00032.html (Accessed on April 15, 2020).
- 13.Ministero della Salute, Italy . 2020. Nuovo Coronavirus Cosa C’é da sapere.http://www.salute.gov.it/portale/home.html (Accessed on April 15, 2020. [Google Scholar]
- 14.Phua J., Badia J.R., Adhikari N.K.J., Friedrich J.O., Fowler R.A., Singh J.M., et al. Has mortality from acute respiratory distress syndrome decreased over time? A systematic review. Am J Respir Crit Care Med. 2008;179(3):220–227. doi: 10.1164/rccm.200805-722OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.