Abstract
The COVID-19 pandemic has had far-ranging consequences for general physical and mental health. Country-specific research reveals a general reduction in mental and physical well-being, due to measures undertaken to stop the spread of COVID-19 disease. However, research is yet to examine the impact of the pandemic on global psychological distress and its effects upon vulnerable groups. Exploration of the factors that potentially mediate the relationship between stress and mental health during this period is needed, to assist in undertaking concrete measures to mitigate psychological distress and support vulnerable groups. Therefore, this study examined the impact of the COVID-19 pandemic on psychological distress globally, and identified factors that may exacerbate decline in mental health. N = 1653 participants (mean age 42.90 ± 13.63 years; 30.3% males) from 63 countries responded to the survey. Depression and anxiety were assessed using the Patient Health Questionnaire and State Trait Anxiety Inventory, respectively. Other measures included the Perceived Stress Scale, the Pittsburgh Sleep Quality Index, 3-item UCLA Loneliness Scale and the Brief Resilient Coping Scale. Globally, consistently high levels of stress, anxiety, depression and poor sleep were observed regardless of number of COVID-19 cases. Over 70% of the respondents had greater than moderate levels of stress, with 59% meeting the criteria for clinically significant anxiety and 39% reporting moderate depressive symptoms. People with a prior mental health diagnosis experienced greater psychological distress. Poor sleep, lower levels of resilience, younger age and loneliness significantly mediated the links between stress and depression, and stress and anxiety. Age-based differences revealed that younger age-groups were more vulnerable to stress, depression and anxiety symptoms. Results show that these vulnerable individuals need more support. Age-specific interventions for modifiable factors that mediate the psychological distress need to urgently deployed to address the global mental health pandemic.
Keywords: Young adults, Perceived stress, Depression, Anxiety, Sleep, Resilience, Loneliness
1. Introduction
The emergence of the SARS-CoV-2 pandemic (COVID-19) in December 2019 has led to unprecedented changes to our lives, with profound consequences for physical and mental well-being. Apart from the physical toll of the disease itself, people across the globe are experiencing heightened anxiety and stress due to financial distress, social distancing, quarantining and stay-at-home orders.(Li et al., 2020; McGinty et al., 2020; Pierce et al., 2020; Hetkamp et al., 2020) These restrictions have dramatically impacted our personal, social and occupational functioning. The psychological effect of these changes and uncertainty is expected to be significant.(Holmes et al., 2020)
It is anticipated that we will be faced with a mental health pandemic that will continue for years to come, even after effective treatments have been developed. Increases in rates of severe mental illnesses have often followed in the aftermath of other global crises, such as the Great Depression and the Spanish Flu pandemic of 1919. In fact, studies emerging from early 2020 have shown an increase in internet mental health symptom searches(Jacobson et al., 2020) and an increased demand for mental health services.(Titov et al., 2020) Country specific data has revealed high levels of stress, depression and anxiety symptoms, increased loneliness and suicidal ideation.(Killgore et al., 2020a; Reger et al., 2020; Zhang et al., 2020; Rossell et al., 2020; Serafini et al., 2020) While it is clear that the pandemic has resulted in greater psychological distress, it is important to determine whether this experience is globally consistent. It is also crucial to examine factors that may mediate the relationship between stress and mental health.
Several mediating factors are linked with stress and mental health. For instance, poor sleep has a well-known bidirectional relationship with depression and anxiety.(Bartlett and Jackson, 2016) Indeed, disrupted routines during the pandemic has resulted in significant changes in sleep.(Blume et al., 2020; Wright et al., 2020) Consequently, reduced sleep quantity and quality during the pandemic is related to poor mental health outcomes.(Ernstsen and Havnen, 2020; Janati Idrissi et al., 2020) Poor sleep can degrade neurocognitive functioning, impacting mood and emotion regulation.(Konjarski et al., 2018; Palmer and Alfano, 2017) Factors such as a previous psychiatric diagnosis, isolation, financial distress, hopelessness, loneliness and uncertainty due to COVID-19 outbreaks can also increase the risk of psychiatric conditions and suicide.(Killgore et al., 2020a; Serafini et al., 2020; Xin et al., 2020; Serafini et al., 2012) In contrast, resilience and perception of social support can be protective against psychiatric disorders.(Serafini et al., 2020) Psychological resilience – a construct representing ability to withstand set-backs and adapt positively in the face of adversity(Luthar and Cicchetti, 2000) – is linked to better mental health outcomes during the pandemic.(Killgore et al., 2020b) It appears that both sleep and resilience are modifiable factors, with the latter associated with more daily exercise and perceived social support.(Killgore et al., 2020b) Examining their influence can help design and implement public health strategies that directly addresses these modifiable, mediating factors.
While recognising mediating factors is the key to developing a consistent public health approach, understanding whether some groups are more vulnerable will help with targeted treatments. For instance, the social, economic and psychological effects of the pandemic may disproportionately impact different age groups. Early evidence from the UK, US, Korea and Australia indicates that younger people have had the greatest increase in rates of psychological distress during the pandemic.(McGinty et al., 2020; Pierce et al., 2020; Rossell et al., 2020; Jung et al., 2020) On the other hand, older adults may also be at risk of poor mental health outcomes as a result of isolation and anxieties about infection risk, particularly those with comorbid health conditions or cognitive impairment.(World Health Organization, 2020) As we move through different phases of the pandemic, identifying vulnerable age-groups will help us modify and design better treatments. Such information is paramount to inform intervention strategies to assist in reducing the psychological burden of the pandemic in the months and years to come.
While country-specific prevalence of mental health issues have been reported previously, this study aimed to 1) examine levels of perceived stress, anxiety and depression during the pandemic between differentcountries; 2) explore the factors that mediate the relationship between stress and poor mental health (i.e., anxiety and depression); and 3) determine whether certain age groups are differentially affected by the pandemic in terms of depression, anxiety, stress, resilience and sleep quality. Specifically, it is hypothesized that younger age groups will be more adversely affected during the pandemic.
2. Methods
A global online survey was disseminated between April 9 and May 25, 2020 through social media channels, targeting adults over 18 years of age. The study was approved by the Monash University Human Research Ethics Committee and conducted in accordance with the Declaration of Helsinki. The survey was conducted via Qualtrics and contained a series of demographic items (age, sex, education, employment/student status, country of residence, ethnicity, marital status, and number and age of dependents), questions on health behaviours (e.g., sunlight exposure, exercise), and questions regarding risk of COVID-19, or pandemic related changes in personal, social or occupational functioning.
Depression was assessed using the Patient Health Questionnaire (PHQ-9(Kroenke et al., 2001)), where scores ≥10 recommended cut-off for moderate depression. State anxiety, which refers to transitory emotional state due to apprehension or fear, was assessed using the 6-item State Trait Anxiety Inventory (STAI(Marteau and Bekker, 1992)), with scores >40 indicating probable levels of clinical anxiety. Perceived Stress Scale (PSS) was used to assess current stress state, with scores >14 indicating moderate levels of stress. Sleep was assessed using the Pittsburgh Sleep Quality Index (PSQI(Buysse et al., 1989)). Scores >5 were considered indicative of poor sleep quality. Loneliness was examined using the 3-item UCLA Loneliness Scale.(Russell, 1996) The 4-item Brief Resilient Coping Scale (BRCS(Sinclair and Wallston, 2004)) was used to measure resilience, which captures tendencies to cope with stress in a highly adaptive manner.
2.1. Data analysis
Data was analyzed using IBM SPSS v.26. ANCOVA and Chi-square tests were used to assess differences in reported prevalence of poor mental health, based on number of regional COVID cases and between countries with most survey responses, with post-hoc testing using Bonferroni correction.
Correlation analysis was used to explore potential mediating variables that may explain the relationship between stress, depression and anxiety. Following this, PROCESS v3.5 for SPSS by Hayes (2013), Model 6 (bootstrapped for 10,000) was used to examine the effects of these mediating factors. To explore age-based differences in mental health, participants were divided into three age groups – 18-34 years (n = 492), 35–54 years (n = 665), and 55 years or above (n = 270). ANCOVA was used to examine differences age based differences in mental health. Multiple regression models were performed within each group to examine predictors of both depression in anxiety across different age-groups.
3. Results
3.1. Participant characteristics
A total of 2555 individuals from 63 countries opened the survey. Of these, 902 participants did not complete all of the mental health outcome measures. Therefore, 1653 participants were included in the final analysis. Participant characteristics are summarized in Table 1 . The vast majority of respondents were currently in lockdown (89%), with 61% working from home. In this sample, 18% of individuals were diagnosed with a mental health condition prior to the COVID-19 pandemic. Commonly reported diagnoses were anxiety and depression, followed by Attention Deficit Hyperactivity Disorder, Bipolar disorder and Post-traumatic Stress Disorder. A majority of the participants shared their household with at least one other person, and 39% had at least one child.
Table 1.
Participant characteristics (N = 1653).
| Demographics | Mean (Standard Deviation) or Frequencies (%) |
|---|---|
| Age | 42.90 ± 13.63 years (18-82)a |
| Gender | |
| Males | 509 (30.3%)b |
| Females | 1090 (67.7%)b |
| Self-describe | 12 (0.7%)b |
| Regions | |
| Australia | 598 (35.6%) |
| India | 262 (15.6%) |
| United Kingdom | 323 (19.05%) |
| South Africa | 119 (7.1%) |
| USA | 56 (3.4%) |
| Spain | 51 (3%) |
| Other | 211 (12.76%) |
| Ethnicity | |
| Caucasian or Caucasian mixed | 1028 (61.2%) |
| Asian or Asian Indian | 339 (20.2%) |
| Hispanic or Latino | 60 (3.6%) |
| African or African American | 28 (1.7%) |
| Self-described | 33 (2.0%) |
| In Lockdown | 1476 (89.10%) |
| Education (n = 1631) | |
| Bachelor's degree or higher | 1322 (81.54%) |
| Vocational college or trade diploma | 265 (16.24%) |
| Less than high school | 19 (0.1%) |
| Other | 25 (3%) |
| Employment status (n = 1631) | |
| Employed full-time | 819 (50.2%) |
| Self-employed | 182 (11.2%) |
| Employed part-time | 143 (8.8%) |
| Retired | 114 (7.0%) |
| Unemployed (looking for work) | 72 (4.3%) |
| Disabled | 13 (0.8%) |
| Student | 150 (9.2%) |
| Other | 138 (8.4%) |
| Working from home | 1003 (60.67%) |
| Total members in household(including housemates) | 2.20 ± 1.70 (0–25)a |
| Dependents | 1.00 ± 0.34 (0−10)a |
| Children(n = 655) | 1.50 ± 1.01 (0–7)a |
| Change in financial status (n = 1269) | |
| No | 545 (42.94%) |
| Yes (negative financial change) | 329 (25.92%) |
| Yes (positive financial change) | 236 (18.59%) |
| Anticipating (negative future change) | 159 (12.52%) |
| Financial distress (n = 1506) | |
| None at all – a little | 947 (58.01%) |
| A moderate amount | 247 (15%) |
| A lot – a great deal | 312 (19.34%) |
| Weekly exercise (n = 1617) | |
| No exercise | 355 (22%) |
| Less than 150 min | 530 (32.77%) |
| 150 min or more | 732 (45.26%) |
| Diagnosed with mental health condition prior to COVID-19 | 300 (18%) |
| At risk of COVID-19 | 300 (18%) |
| Adjusting to lockdown | |
| Extremely easy – Slightly easy | 639 (38.65%) |
| Neither easy nor difficult | 246 (14.88%) |
| Slightly difficult – extremely difficult | 732 (44.28%) |
| Loneliness (UCLA-LS > 6) | 782 (47.2%)b |
| Poor sleep quality (PSQI > 5) | 1207 (73%)b |
| Perceived stress (PSS > 14) | 1273 (77)%b |
| State anxiety (STAI > 40) | 976 (59%)b |
| Depression (PHQ-9 > 10) | 578 (34.9%)b |
Note: Percentages reflect valid proportion of respondents for each item. Responses to ‘distress due to finances’ and ‘adjusting to lockdown’ is displayed as combined categories for brevity.
Represents range.
Represents percentage of participants scoring above the cut-off for loneliness, poor sleep quality, moderate stress, anxiety and depression.
3.2. Rates of stress, depression, anxiety and poor sleep
High rates of perceived stress were observed in the sample, with 77% of the respondents reporting at least moderate levels of stress (Table 1). Moderate or higher levels of depression was noted for 35% of respondents. Clinically probable levels of anxiety were noted for state anxiety in 59% of the participants. Poor sleep quality was also common, reported by 73% of the participants.
Higher levels of perceived stress were strongly associated with both depression (r = 0.72, p < .001) and anxiety (r = 0.72, p < .001) symptoms (See Supp Table 1). In addition, poor sleep quality, higher levels of loneliness shared positive relationships with anxiety and depression. Higher resilient coping was associated with lower symptoms of anxiety (r = −0.11, p < .001) and depression (r = −0.33, p < .001). Previous diagnosis of a mental health condition had a low, but significant, correlation with depression (r = 0.26, p < .001) and anxiety (r = 0.15, p < .001) symptoms.
3.3. Differences in mental health outcomes based on number of cases and country
Participants were divided into three groups based on number of COVID-19 cases in their country (based on the data available on May 25th 2020). Following categories were used – 0–50,000 cases (n = 795), 50,000–1,00,000 (n = 84) cases and > 1,00,000 cases (n = 752). No significant group differences were observed for anxiety and depression across the groups. However, small effect size was noted for stress, as respondents from countries with higher number of cases reported more stress (p > .01, Partial η 2 = 0.008).
The severity of stress, depression, anxiety and sleep symptoms based on recommended cut-offs across respondents from top five countries (n = 1360) were also explored (Table 1; Supp Table 2 ). There was a significant difference between the groups for anxiety, depression and stress (all p < .001). Subsequent post-hoc testing revealed that participants from South Africa reported a significantly higher proportion of at least moderate levels of depression compared to the other countries.
Table 2.
Results from Analysis of Covariance in resilience, anxiety, depression, stress and sleep quality based on following age-groups – 18–34 years (n = 492), 35–54 years (n = 665), and 55 years or above (n = 270).
| Scales | Sum of Squares | Df | Mean Squares | f | Partial η2 | R2 |
|---|---|---|---|---|---|---|
| BRCS⁎⁎ | 10.552 | 2 | 52.76 | 6.87 | 0.10 | 0.20 |
| STAI⁎⁎⁎ | 7077.09 | 2 | 3538.54 | 18.16 | 0.25 | 0.59 |
| PHQ⁎⁎⁎ | 551.53 | 2 | 275.76 | 9.18 | 0.01 | 0.22 |
| PSS⁎⁎⁎ | 2169.14 | 2 | 1084.57 | 27.29 | 0.03 | 0.28 |
| PSQI⁎ | 93.76 | 2 | 46.84 | 3.84 | 0.00 | 0.07 |
| UCLA-LS⁎⁎⁎ | 138.57 | 2 | 69.28 | 20.42 | 0.03 | 0.03 |
Abbreviations used: BRCS – Brief Resilient Coping Scale, STAI – State-Trait Anxiety Scale, PHQ – Patient Health Questionnaire, PSS – Perceived Stress Scale, PSQI – Pittsburgh Sleep Quality Index, UCLA-LS – Loneliness Scale.
p < .05.
p < .01.
p < .001.
3.4. Factors mediating the relationship between stress, and depression and anxiety during the pandemic
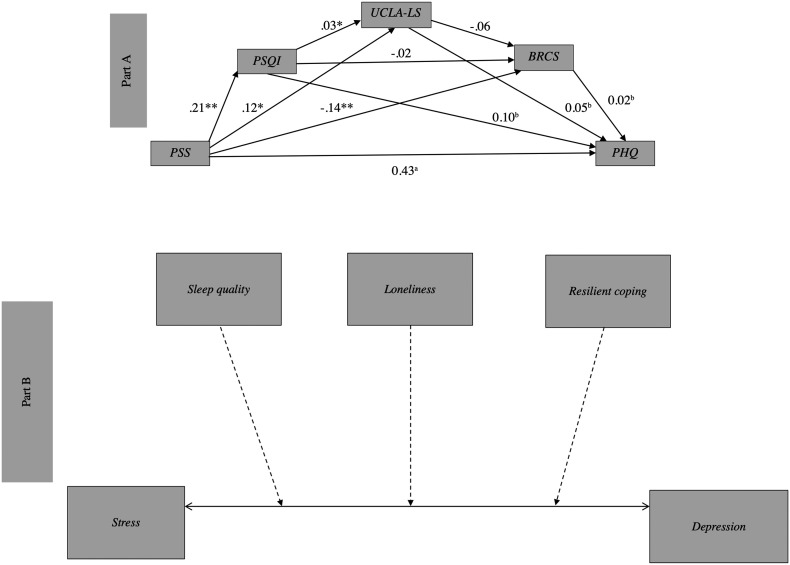
A mediation analysis was conducted to see which factors mediated the relationship between stress and depression. Three variables that shared the highest correlation with depression (apart from stress) were considered as potential mediators (Supp Table 1). Hence, sleep quality, loneliness and resilient coping were added as possible mediating variables to the mediation model. Significant mediation effects were observed (Fig. 1 ), where poor sleep quality accounted for 10% of the variance in the relationship between stress and depression, followed by loneliness (by 5%) and resilient coping (by 2%). After controlling for the mediators, the relationship between stress and depression still remained significant (β = 0.61, t (1493) = 39.86, p < .001), indicating partial mediation.
Fig. 1.
Mediation effects (N = 1495) of sleep quality, loneliness and resilient coping on the relationship between stress and depression (Part – A).
All three mediators had significant, direct effects on the associations between stress and depression (Part B). **p < .001, *p < .01.
aIndicates significant direct association.
bIndicates significant mediation effect.
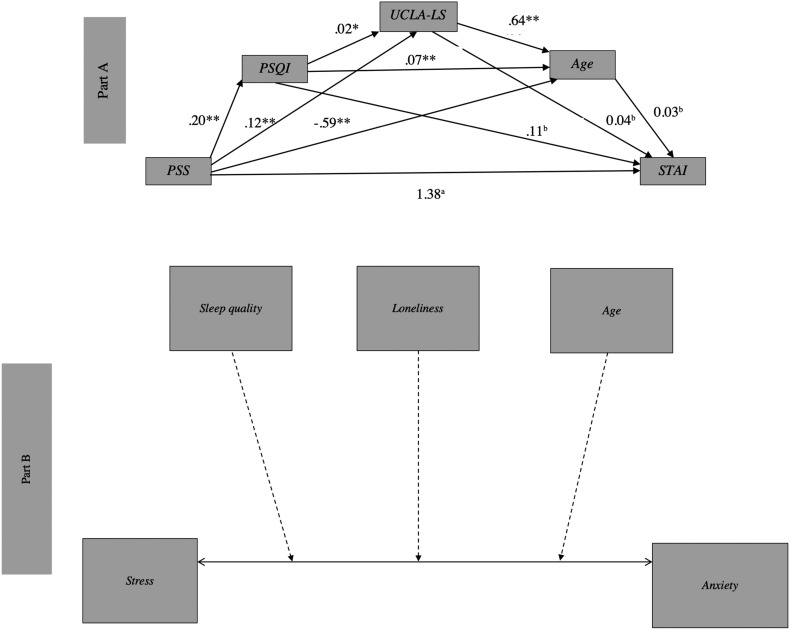
A second mediation analysis was performed to examine if any factors mediated the relationship between stress and anxiety. Sleep quality, loneliness and age were three factors that shared the strongest correlation with anxiety (excluding stress) and were entered into the mediation model. Significant mediation effects were observed (Fig. 2 ), where poor sleep quality, increased loneliness and younger age mediated the relationship between stress and anxiety, accounting for a combined 18% change in the relationship. Poor sleep quality was the largest mediator, predicting 11% change in the relationship between stress and anxiety, followed by isolation (by 4%) and age (by 3%). The relationship between stress and anxiety remained significant even after accounting for all mediators (β = 1.57, t (1493) = 43.16, p < .001), indicating partial mediation.
Fig. 2.
Mediation effects (N = 1495) of sleep quality, loneliness and resilient coping on the relationship between stress and anxiety (Part – A).
All three mediators had significant, direct effects on the associations between stress and anxiety (Part B). **p < .001, *p < .01.
aIndicates significant direct association.
bIndicates significant mediation effect.
Note: p-values between groups based on Bonferroni post-hoc testing.
3.5. Factors predicting depression and anxiety across different age groups
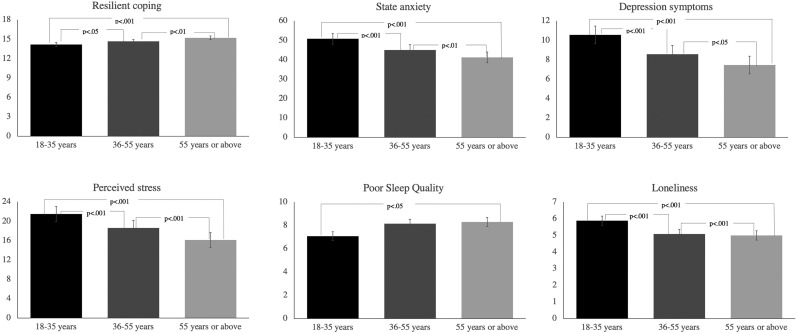
With regards to difference in psychological distress across different age-groups, results revealed significant group differences for all measures (Table 2). In particular, moderate to large effect sizes were noted for both anxiety (p < .001) and stress (p < .001), with younger people reporting significantly higher scores on both measures compared to the other age groups (Fig. 3 ). Older individuals reported higher resilient coping (p < .05) compared to the other age groups but slightly poorer sleep quality (p < .05) compared to the youngest age group.
Fig. 3.
Group differences in anxiety symptoms, resilient coping, depression symptoms, perceived stress, sleep quality and loneliness. People in the youngest age group reported higher levels of anxiety, depression and stress, whereas older individuals reported higher resilient coping but poorer sleep quality.
Multiple regression was conducted to analyze what factors predicted largest variance in scores for depression across different groups (Table 3 ). The following variables were entered as independent variables – stress, sleep quality, distress due to finances, previous mental health diagnosis, loneliness, resilient coping, weekly exercise minutes, adjustment to lockdown and number of dependents.
Table 3.
Multiple regression predicting change in depression scores across following age-groups – 18–34 years (n = 492), 35–54 years (n = 665), and 55 years or above (n = 270).
| Age group | Variables | β | T | R2 | |
|---|---|---|---|---|---|
| 18–34 years | Depression | PSS | 0.56 | 6.52 | 0.49⁎⁎⁎ |
| Weekly exercise minutes | -0.25 | -3.14 | 0.05⁎⁎ | ||
| PSQI | 0.28 | 3.09 | 0.03⁎ | ||
| Distress due to finances | 0.23 | 2.78 | 0.04⁎⁎ | ||
| Anxiety | PSS | 0.58 | 8.75 | 0.48⁎⁎⁎ | |
| PSQI | 0.14 | 2.38 | 0.02⁎ | ||
| UCLA-LS | 0.13 | 2.16 | 0.01⁎ | ||
| 35–54 years | Depression | PSS | 0.54 | 7.36 | 0.43⁎⁎⁎ |
| PSQI | - 0.21 | - 2.94 | 0.05⁎⁎ | ||
| Weekly exercise minutes | 0.27 | 3.72 | 0.04⁎⁎ | ||
| Anxiety | PSS | 0.63 | 13.21 | 0.54⁎⁎⁎ | |
| BRCS | - 0.17 | - 3.81 | 0.02⁎⁎⁎ | ||
| PSQI | 0.12 | 2.65 | 0.01⁎⁎ | ||
| 55 years or above | Depression | PSS | 0.46 | 3.46 | 0.28⁎⁎ |
| PSQI | 0.41 | 3.07 | 0.16⁎ | ||
| Number of dependents | 0.30 | 2.28 | 0.10⁎ | ||
| Adjusting to lockdown | - 0.30 | - 2.25 | 0.09⁎ | ||
| Anxiety | PSS | 0.61 | 8.04 | 0.50⁎⁎⁎ | |
| PSQI | 0.26 | 3.38 | 0.05⁎⁎ |
Abbreviations used: PSS – Perceived Stress Scale, PSQI – Pittsburgh Sleep Quality Index.
p < .05.
p < .01.
p < .001.
In all age-groups, perceived stress emerged as the largest predictor of changes in depression symptoms. In the 18–34 age group, more exercise minutes (per week) were related to lower depression symptoms. Poor sleep quality and increased distress due to financial circumstances also predicted changes in depression symptoms. Similar to the younger age-group, in individuals aged 35–54 years, greater exercise minutes and good sleep quality was associated with lower scores on depression measure. Poor sleep quality contributed to changes in depression symptoms in individuals aged 55 years and above. In particular, having dependents was related to higher depression symptoms. In contrast, better adjustment to lockdown regulations was related to lower depression symptoms.
A second multiple regression was performed to examine factors that predicted anxiety scores across different age groups using the same independent variables (Table 3). Similar to depression outcomes, perceived stress was the strongest predictor of anxiety symptoms in each age group. However, in younger adults, both poor sleep quality and loneliness were related to anxiety symptoms. Higher resilience was inversely related to anxiety in individuals aged 35–54 years. Poor sleep quality was a significant predictor of anxiety in individuals aged 55 years or above. Notably, factors like weekly exercise minutes, adjusting to lockdown and distress due to financial changes were not significant predictors of anxiety in any age group.
4. Discussion
The findings from this global survey indicate that there was significant psychological distress during the early stages of the pandemic. High rates of stress, state anxiety, depression and poor sleep were endorsed by the respondents in this study, highlighting the psychological impact of the current pandemic across the globe. Prior mental health diagnosis was related to poorer mental health. Further, 20% of respondents reported significant distress related to their financial situation, which was associated with both psychological distress and poorer sleep. Factors such as poor sleep quality, loneliness, resilience and age emerged as mediators of the relationship between stress and mental health, highlighting these as potential areas for targeted interventions. Younger age-groups were more vulnerable, reporting greater stress, anxiety and depression compared to middle and older age groups.
There was a considerable degree of psychological distress in our sample, with 77% of respondents reporting moderate to severe levels of stress. State anxiety was reported by 60% of the participants, which may reflect the state of apprehension that is prevalent globally during the pandemic. About 35% of the respondents reported significant depressive symptoms, however the severity of depressive symptoms overall was mostly in the mild to moderate range. This is comparable to only 18% of the sample who reported having a mental health diagnosis. It is possible that selection bias may have had an effect on these figures, since participants were responding to a survey regarding mental health and sleep. However, these figures are comparable to other national surveys during this period,(Fisher et al., 2020; Gao et al., 2020; Wang et al., 2020) and are well above pre-pandemic prevalence figures.(McGinty et al., 2020)
4.1. Country level differences in mental health
Some differences were observed for mental health outcomes across the top five countries, based on recommended clinical cut-offs for each measure. However, post-hoc testing did not reveal any significant differences across the countries. Regardless, the differences in results may be attributed to proportion of participants from each country, or may also reflect differences in how the pandemic was being dealt with at the time of the survey, which differ across countries. For instance, during the time of data collection (www.thinkglobalhealth.org/article/updated-timeline-coronavirus), South Africa was in Phase I of reopening its economy (then scheduled for May 1), which may have led to increased apprehension. It must be noted that soon after the opening, South Africa witnessed rapid increased in COVID-19 cases. The death rate in the United States' surpassed that of Italy during the time of data collection, which could have contributed to increased stress among US respondents. In comparison, Australia had lower number of cases and were in lockdown throughout the data collection period. Despite the differences in case numbers and government-imposed stay-at-home orders, no major differences were reported for mental health outcomes between countries. Taken together, these results suggest that high levels of stress and poorer mental health may be consistent across the globe, possibly stemming from overall apprehension and rapidly changing nature of the pandemic, rather than direct threat of the virus.
4.2. Mediators of stress and mental health: age effects
While cause-effect cannot be determined, the mediation models indicated that several mediators effect the associations between stress and anxiety, and stress and depression. For depression, poor sleep quality, loneliness and resilient coping mediated the relationship between stress and depression. In particular, sleep quality was the strongest predictor for both models, accounting for over 10% of the variance. This is not surprising, given the well-established association between sleep and psychopathology during the pandemic previously reported.(Hetkamp et al., 2020; Huang et al., 2020; Stanton et al., 2020) Previous studies have shown that sleep and affective brain functioning are linked.(Palmer and Alfano, 2017) Sleep disturbances also increase the risk of depression and anxiety.(Harvey, 2011) In particular, reports from China suggest that depression and anxiety are associated with higher levels of insomnia in adolescents and young adult during the pandemic.(Zhou et al., 2020) Loneliness, particularly social isolation, is associated with a larger cortisol awakening response,(Grant et al., 2009) potentially explaining the mediating role of loneliness in the links between stress and depression. This suggests that targeted interventions for improving sleep and enhancing social connectedness may help to reduce the burden of stress, depression and anxiety post-pandemic.
For the stress-anxiety mediation model, younger age was a significant mediator, suggesting that younger adults may be vulnerable to stress and anxiety during this pandemic. This was also supported by the age-specific analysis. Younger adults fared the worst with regards to depression, stress and anxiety symptoms. In comparison, older adults had the lowest ratings on these measures. This finding is similar to an Australian survey conducted in April 2020, in which respondents under 45 years of age were most vulnerable to psychological distress.(Rossell et al., 2020) While poor sleep and perceived stress were common contributing factors for both depression and anxiety across all age groups, there were some factors that were specifically related to these outcomes within each age category. Within younger adults, loneliness and financial distress were associated with poorer depression and anxiety outcomes, respectively. A number of protective factors were also identified. For example, in individuals under 55 years, increased levels of weekly exercise were associated with lower endorsement of depressive symptoms. Older adults demonstrated more resilience than other age-groups, which may be a key factor in protection against psychological distress. Additionally, resilience was an inverse contributor to the relationship between stress and depression. However, in line with previous studies, these findings highlight the importance of carefully tailoring mental health intervention strategies for each age group. It must also be noted that while factors like financial distress or loneliness may not be immediately modifiable, other factors associated with poor mental health outcomes should be a target for intervention. For instance, improving sleep can result in positive outcomes for both depression and anxiety even when the conditions are not directly treated.(Cunningham and Shapiro, 2018) Similarly, employing stress reduction strategies, such as mindfulness, can have positive outcomes for mental health.(Gu et al., 2015) Furthermore, there is a need to start public health programs aimed at promoting better sleep at a broader level. Governments and industries should consider adopting strategies that can reduce stress and improve sleep and well-being among citizens and employees during the time of the pandemic.
Apart from sleep, developing and implementing programs aimed at enhancing resilience deserve the same urgent priority that is assigned to the development and testing of vaccines and antivirals. Large scale proactive measures are a key part of successfully preparing millions of people as they resume their day-to-day lives and livelihoods and is an essential step in re-starting stalled economies on a global scale. In the absence of such proactive measures, COVID-19's long-term global impact on mental health could easily be as devastating and costly as the financial impact of the virus. Multifaceted approaches may need to be employed for this purpose. Firstly, broader public health initiatives should be employed, targeting factors that mediate the links between stress and mental health. Such initiatives should be aimed at enhancing psychological resilience and treating mental health problems, and may include evidence-based complementary and alternative medicine interventions. As suggested by Moreno and colleagues, mental health systems need to be adapted to the pandemic as well.(Moreno et al., 2020) Results from this study support the need for telehealth for reducing stress, and improving mental health and sleep disorders. To improve accessibility and affordability, digital therapeutics, including evidence-based self-help tools need adoption. These tools are showing promising effectiveness at improving sleep and mental health outcomes.(Low et al., 2020) Secondly, specific measures should be employed to address age-based concerns regarding mental health. The current study supports previous reports that young adults are at an increased risk of poor mental health as a result of the pandemic, and that factors such as loneliness and financial distress are impacting younger individuals more than others. Financial inequalities and associated distress can increase the risk of psychological distress and also prevent people from seeking adequate care. To tackle this, government action may be required to address financial or occupational uncertainty of the pandemic, and provide adequate mental health resources to address the emerging youth mental health crisis.
Lastly, vulnerable groups may need greater support to mitigate the risks of poor mental health. For instance, people with pre-existing psychiatric conditions require better access to economical treatments.(Moreno et al., 2020) Individuals who have experienced childhood trauma, who are at increased risk of depression and suicide,(Pompili et al., 2014) and those impacted by domestic violence or at risk of abuse during the pandemic,(Bradbury-Jones and Isham, 2020) may need additional support. Ultimately, affordable, high-quality, and readily-disseminatable mental health services are required at a global level to prevent worsening of mental health.
4.3. Strengths and limitations
The strength of this study is that it included respondents from more than 60 countries. It has been noted that several countries and communities have been underrepresented in recent research,(Holmes et al., 2020) and the current study was able to overcome this issue by surveying participants from a range of different countries. The current findings highlight and support previous reports that the number of COVID-19 cases in a particular country do not necessarily predict major differences in mental health outcomes.
Some limitations of this study need to be noted. The levels of depression detected in this study were at most mild-moderate across all groups, therefore the findings need to be interpreted cautiously and not overstated. It is also possible that there was a selection bias in that individuals suffering and feeling frustrated with mild anxiety and stress may be more likely to notice an online survey mentioning salient symptoms and opt-in to participate.(Keusch, 2015) It is also important to note that half of people aged 75 and over, and many with mental illness (who represent a key COVID-19 risk group), are not regular internet users,(Hargittai et al., 2019) so this study might not be a representative sample in terms of tapping into a wider group of non-social media users. The sample was also highly educated, and the majority of respondents were employed, thus it may not be representative of a broader demographic. It is important to note that while selection bias may have occurred, this study did not specifically try to recruit people with mental health issues. The advertisements were simply framed as questions on ‘sleep, mental health and changes in routine’ during the pandemic. Due to the cross-sectional nature of this study, we cannot determine the direction of the relationship between stress and mental health. Future longitudinal studies will help to determine whether mental health issues improve over time, or if additional stressors emerge as countries face ongoing challenges due to the virus.
5. Conclusion
The findings from the current study add to the emerging evidence demonstrating a decline in mental health during the pandemic which is consistent across the globe, regardless of the number of regional COVID-19 cases. Younger age groups may be more vulnerable to the mental health impact of the pandemic. Certain modifiable factors may mediate the associations between stress and mental health, including sleep, loneliness and resilience. Hence, nuanced mental health strategies, rather than a ‘one size fits all’ approach, are required to reduce pandemic uncertainties and address specific vulnerabilities. Findings from this study highlight the need for low-cost public health interventions that can be widely disseminated to improve sleep and increase resilience. As all countries battle different waves of the pandemic, and try to establish a “new normal” with approval of vaccines and changes to restrictions, it is yet to be seen whether the levels of psychological distress reported in this study are maintained. Ongoing longitudinal studies are urgently required to examine the trajectory of the mental health burden over time.
Ethical statement
The study was approved by the Monash University Human Research Ethics Committee and conducted in accordance with the Declaration of Helsinki.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We wish to thank the participants who have generously given their time to complete the survey, particularly during these difficult times. We thank Shelley Webb and Stephen Ghosh for their assistance with data entry. We also thank Prof Luke Downey for his comments on an earlier draft of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pnpbp.2020.110236.
Appendix A. Supplementary data
Supplementary material
References
- Bartlett D., Jackson M.L. The bidirectional nature of sleep problems and psychopathology. Medicine Today. 2016;17(3):23–28. [Google Scholar]
- Blume C., Schmidt M.H., Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020;30:R783–R801. doi: 10.1016/j.cub.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury-Jones C., Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J. Clin. Nurs. 2020;29(13):2047–2049. doi: 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cunningham J.E.A., Shapiro C.M. Cognitive behavioural therapy for insomnia (CBT-I) to treat depression: a systematic review. J. Psychosom. Res. 2018;106:1–12. doi: 10.1016/j.jpsychores.2017.12.012. [DOI] [PubMed] [Google Scholar]
- Ernstsen L., Havnen A. Mental health and sleep disturbances in physically active adults during the COVID-19 lockdown in Norway: does change in physical activity level matter? Sleep Med. 2020 doi: 10.1016/j.sleep.2020.08.030. In press. [DOI] [PubMed] [Google Scholar]
- Fisher J.R., Tran T.D., Hammargerg K., et al. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med. J. Aust. 2020;1 doi: 10.5694/mja2.50831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant N., Hamer M., Steptoe A. Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Ann. Behav. Med. 2009;37(1):29–37. doi: 10.1007/s12160-009-9081-z. [DOI] [PubMed] [Google Scholar]
- Gu J., Strauss C., Bond R., Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Hargittai E., Piper A.M., Morris M.R. From internet access to internet skills: digital inequality among older adults. Univ. Access Inf. Soc. 2019;18(4):881–890. [Google Scholar]
- Harvey A.G. Sleep and circadian functioning: critical mechanisms in the mood disorders? Annu. Rev. Clin. Psychol. 2011;7:297–319. doi: 10.1146/annurev-clinpsy-032210-104550. [DOI] [PubMed] [Google Scholar]
- Hetkamp M., Schweda A., Bäuerle A., et al. Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: relation to infection rates, deaths, and German stock index DAX. Sleep Med. 2020;75:350–353. doi: 10.1016/j.sleep.2020.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Wang Y., Zeng L., et al. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a Chinese population during the COVID-19 epidemic. Frontiers in Psychiatry. 2020;11:894. doi: 10.3389/fpsyt.2020.568329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N.C., Lekkas D., Price G., et al. Flattening the mental health curve: COVID-19 stay-at-home orders are associated with alterations in mental health search behavior in the United States. JMIR Ment Health. 2020;7(6):e19347. doi: 10.2196/19347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janati Idrissi A., Lamkaddem A., Benouajjit A., et al. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Med. 2020;74:248–253. doi: 10.1016/j.sleep.2020.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung S.J., Yang J.S., Jeon Y.J., et al. Lancet; 2020. The Impact of COVID-19 on Psychological Health in Korea: A Mental Health Survey in Community Prospective Cohort Data.https://ssrn.com/abstract=3618193 Available at SSRN 3618193. [Google Scholar]
- Keusch F. Why do people participate in Web surveys? Applying survey participation theory to Internet survey data collection. Management Rev. Q. 2015;65(3):183–216. [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Taylor E.C., Cloonan S.A., Dailey N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konjarski M., Murray G., Lee V.V., Jackson M.L. Reciprocal relationships between daily sleep and mood: a systematic review of naturalistic prospective studies. Sleep Med. Rev. 2018;42:47–58. doi: 10.1016/j.smrv.2018.05.005. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Qin Q., Sun Q., Sanford L.D., Vgontzas A.N., Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J. Clin. Sleep Med. 2020;16(8):1417–1418. doi: 10.5664/jcsm.8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low T., Conduit R., Varma P., Meaklim H., Jackson M.L. Treating subclinical and clinical symptoms of insomnia with a mindfulness-based smartphone application: a pilot study. Internet Interv. 2020;21 doi: 10.1016/j.invent.2020.100335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S.S., Cicchetti D. The construct of resilience: implications for interventions and social policies. Dev. Psychopathol. 2000;12(4):857–885. doi: 10.1017/s0954579400004156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI) Br. J. Clin. Psychol. 1992;31(3):301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C., Wykes T., Galderisi S., et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer C.A., Alfano C.A. Sleep and emotion regulation: an organizing, integrative review. Sleep Med. Rev. 2017;31:6–16. doi: 10.1016/j.smrv.2015.12.006. [DOI] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili M., Innamorati M., Lamis D.A., et al. The associations among childhood maltreatment,“male depression” and suicide risk in psychiatric patients. Psychiatry Res. 2014;220(1–2):571–578. doi: 10.1016/j.psychres.2014.07.056. [DOI] [PubMed] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019—a perfect storm? JAMA Psychiatry. 2020;77(11):1093–1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Rossell, S., Neill, E., Phillipou, A., et al., 2020. An overview of current mental health in the general population of Australia during the COVID-19 pandemic: Results from the COLLATE project. medRxiv 2020.07.16.20155887. [DOI] [PMC free article] [PubMed]
- Russell D.W. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini G., Pompili M., Innamorati M., Gentile G., Borro M. Gene variants with suicidal risk in a sample of subjects with chronic migraine and affective temperamental dysregulation. Eur. Rev. Med. Pharmacol. Sci. 2012;6(10):1389–1398. [PubMed] [Google Scholar]
- Sinclair V.G., Wallston K.A. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment. 2004;11(1):94–101. doi: 10.1177/1073191103258144. [DOI] [PubMed] [Google Scholar]
- Stanton R., To QG, Khalesi S., et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Staples L., Kayrouz R., et al. Rapid report: early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic. Internet Interv. 2020;21 doi: 10.1016/j.invent.2020.100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2020. Mental Health and Psychosocial Considerations During COVID-19 Outbreak.https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf [Google Scholar]
- Wright K.P., Linton S.K., Withrow D., et al. Sleep in university students prior to and during COVID-19 stay-at-home orders. Curr. Biol. 2020;30:R797–R798. doi: 10.1016/j.cub.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin M., Luo S., She R., et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am Psychol. 2020;75(5):607–617. doi: 10.1037/amp0000692. [DOI] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.-J., Wang L.-L., Yang R., et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;75:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material