Abstract
On 25 March 2020, the Chief Dental Officer issued national guidance restricting the provision of all routine, non-urgent dental services in response to the spread of COVID-19. We analysed odontogenic cervicofacial infections (CFI) presenting to oral and maxillofacial surgery (OMFS) departments during the first wave of COVID-19 in the United Kingdom.
From 1 April 2020 until 31 July 2020 a database was used to prospectively collect records for all patients with CFI who presented to oral and maxillofacial teams. Information gathered included clinical presentation, location/origin of infection, and how this was managed. The OMFS units were asked to compare the patient’s care with the treatment that would usually have been given prior to the crisis. A total of 32 OMFS units recorded 1381 cases of CFI in the UK. Most of the infections were referred via the emergency department (74%). Lower first or second molars were the most common origin, contributing 40% of CFI. Collaborators reported that patients' treatments were modified as a response to COVID in 20% of cases, the most frequently cited reason being the application of COVID-19 hospital policy (85%). The impact of the first wave of COVID modified the management of a significant number of patients presenting with CFI, and there was a proactive move to avoid general anaesthetics where possible. Some patients who presented to secondary care were given no treatment, suggesting they could have been managed in primary dental care if this had been available. We recommend that OMFS units and urgent dental care centres (UDCCs) build strong communication links not only to provide the best possible patient care, but to minimise COVID exposure and the strain on emergency departments during the pandemic.
Keywords: Odontogenic infections, COVID-19, Coronavirus, Urgent Dental Care, Emergency Dental Care
Introduction
The spread of coronavirus disease 2019 (COVID-19) in the United Kingdom has presented significant challenges to oral and maxillofacial surgical (OMFS) departments. On 25 March 2020, the chief dental officers (CDO) of the four nations (England, Northern Ireland, Scotland, and Wales) issued national guidance restricting the provision of all routine, non-urgent dental services in keeping with national lockdown measures.1, 2
The guidance suggested that general dental practitioners (GDPs) should move to a telephone triage service to offer advice, and analgesia and antibiotics (AAA) where appropriate. Only novel urgent dental care centres (UDCCs) were able to provide face-to-face assessment and treatment for emergency dental services, with patients requiring referral via their GDP or through the national telephone advice line NHS 111.
With significantly reduced access to primary care dentistry, both to prevent and provide early treatment of odontogenic infections, it was predicted that patients would present to local OMFS departments with increased frequency and disease severity.3 In the context of diverted hospital resources, redeployed trainees, and the increasing prevalence of COVID-19, this had the potential to overwhelm an already strained National Health Service (NHS).
Our national, multicentred service evaluation aimed to evaluate odontogenic cervicofacial infections (CFI) presenting to OMFS departments during the start of the COVID-19 pandemic in the UK. It focused on the impact of the pandemic on treatment pathways and patient outcomes. Our secondary aims were to assess any correlation with patient age, aetiology, and surgical management.
Material and methods
From 1 April 2020, the National Facial Oral and Oculoplastic Research Centre (NFORC) set up a database on the Research Electronic Data Capture (REDCap) database system hosted at the Barts Cancer Research UK Centre, Queen Mary University of London.4, 5, 6 REDCap is a secure, web-based software platform designed to support data capture for research studies.
The data on REDCap were anonymous, so to support the use of this database, a pro forma in a portable document format (pdf) and a spreadsheet in Excel© (Microsoft Corp), along with user guides were provided to researchers in each hospital. The lead in each OMFS unit was asked to obtain local approval from their hospital to collect the data. Each unit chose a start date that represented the start of formal changes in care provision caused by COVID-19 in their hospital. Data on all patients presenting to the OMF team with an odontogenic infection, regardless of treatment, were collected from that date until 31 July 2020. There were no exclusion criteria.
Information collected included age, gender, clinical presentation, source of referral, location and type of infection and, if patients were admitted, the length of hospital stay (LOS). Respondents were also asked if and how a patient’s management compared to what would usually have been given before the pandemic.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics for Windows version 26 (IBM Corp). The analytical method used for differences between the two groups (expected pre-lockdown versus during lockdown treatments) was dependent on the variable and skew of the data. Non-parametric data were analysed using Mann Whitney U tests, normally distributed non-categorical data using Student’s t tests, and binomial data using Chi squared (χ2) analysis, with a significance level at p < 0.05 and confidence intervals at 95%.
Results
A total of 32 OMFS units recorded 1381 presentations of CFI in the UK-wide study (Fig. 1 ). The mean (range) age of patients at presentation was 37.3 (1 – 97) years (SD 17.4 years). There were almost equal numbers of males and females.
Fig. 1.
Cervicofacial infection (CFI) presentations according to OMFS region (n = number of units that participated from each region).
The majority of patients presented on the day of the onset of symptoms (median (IQR) 0 (2), range 0 – 90 days) and those admitted had a median (IQR) length of stay 2 (2) days, range 1 – 48 days. Over half the patients had an American Society of Anesthesiologist’s (ASA) classification of 1 (n = 822, 60%), with a reducing number of presentations with increasing ASA scores (ASA 2: 32.4%; ASA 3: 7.6%, ASA 4: 0.4%).
The majority of patients who presented to the OMF service came from emergency departments (ED) (n = 1044, 74%) (Fig. 2 ). The second most common source of referral was via NHS 111 primary care triage (n = 135, 13%), followed by referrals from GDPs (n = 84, 6%), UDCCs (n = 61, 5%), inpatient referrals (n = 42, 3%) and general medical practitioners (GMP) (n = 28, 2%,).
Fig. 2.
Referral sources of cervicofacial infections (CFI).
The primary presenting symptom for all CFI patients was a space infection with collection (n = 422, 31%), followed by paradental swelling (n = 373, 27%); dental pain (n = 346, 25%), localised cellulitis (n = 223, 16%) and finally, purulent discharge from the dental socket (n = 14,1%). There was a single case of necrotising fasciitis.
The most common causes of infection were caries/periapical periodontitis (n = 1178, 85%), followed by pericoronitis of the third molar (n = 88, 6.4%) and post-extraction infection (n = 68, 4.9%).
Teeth were grouped according to their presentation (Fig. 3 ). Lower first or second molars were the most common source, contributing 40% (n = 552) of CFI. Lower third molars 13.0% (n = 179) and lower anterior/premolars 8.4% (n = 116) were the next most common sources, followed by upper premolar/molar (23.5%, n = 323) and upper anterior teeth/canines (13.5%, n = 186).
Fig. 3.
Odontogenic source and presenting symptom.
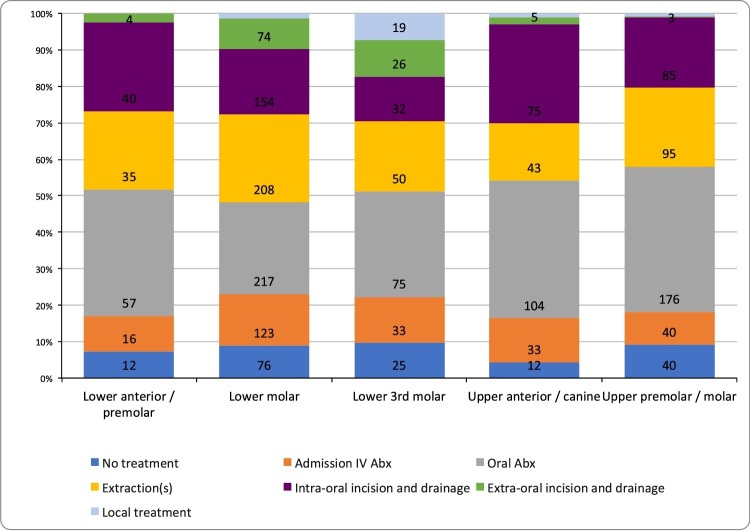
All treatment options applied to all CFI regardless of odontogenic source (Fig. 4 ). The majority of patients (n = 1076) were managed with antibiotics (n = 645 (60%) orally, and n = 431 (40%) admitted for intravenous antibiotics).
Fig. 4.
Odontogenic location and intervention.
Of the patients treated, local anaesthetic (LA) was used in 35% (n = 441), general anaesthetic (GA) in 20% (n = 290); the remaining patients did not receive anaesthetic (n = 628, 47%). Five patients were admitted to the intensive care unit (0.4%) and there were no reported deaths. The majority of GAs were provided to treat space infections with collection (n = 202, 74%) and paradental swellings (n = 42, 15%).
Of the 61 referrals from UDCCs, 23 (38%) presented with a space infection with collection and 12 (28%) with local cellulitis. Forty (66%) needed a surgical intervention, either under a GA (n = 22, 30%) or LA (n = 18, 30%). The remainder were either given antibiotics or had packing/debridement of their socket (n = 21, 34%).
Collaborators reported that treatment was modified by COVID in a fifth of patients (n = 283, 20%). The most frequently cited reason for the change in treatment was to apply the hospital’s COVID-19 policy to reduce the number of patients going to theatre (n = 240, 85%). Thirty-five patients (12%) had altered management to avoid an aerosol-generating procedure. Other reasons included limiting activity to reduce the need for personal protective equipment (PPE) (n = 4, 1%), having no access to the emergency theatre (n = 2, 1%), and patients suspected of having COVID-19 (n = 2, 1%).
For the interventions given in this study, the collaborators were asked if they would have provided an intervention for the same condition if the patient had presented before the COVID-19 crisis (Table 1 ). Of the 411 patients who had a tooth extracted, 308 (75%) would have had an intervention before COVID, whereas 103 (25%) would not. For patients receiving antibiotics, 459 (72%) would have had an intervention whereas 182 (29%) would not. For patients treated with intraoral incision and drainage 314 (80%) would have had an intervention whereas 78 (20%) would not. For those who had extraoral drainage 103 (87%) would have had an intervention whereas 15 (13%) would not. For those who were admitted for intravenous antibiotics, 202 (81%) would have had an intervention whereas 48 (19%) would have not been admitted. Even though all these changes in treatment were statistically significant (p < 0.005) compared with the pre-COVID treatment plan, the intervention that was given during this episode may not have been the same as the one they would have had pre-COVID. However, patients who had a GA (n = 247, 96.1%) or LA (n = 294, 73%) would have had the same treatment before the pandemic. Conversely, 175 patients did not receive any treatment and 68 (39%) of them would have received treatment pre-COVID-19. Overall, there were no significant correlations between treatment changes and the characteristics of the patients concerned.
Table 1.
Impact of Covid-19 pandemic on treatment. Data are number (%).
| Procedure | Intervention | Would have received intervention pre-COVID-19 | Would not have received intervention pre-COVID-19 | p value (χ² analysis) |
|---|---|---|---|---|
| Extraction | 411 | 308 (75) | 103 (25) | < 0.005 |
| Oral antibiotics | 641 | 459 (72) | 182 (29) | < 0.005 |
| Intraoral incision and drainage | 392 | 314 (80) | 78 (20) | < 0.005 |
| Extraoral incision and drainage | 118 | 103 (87) | 15 (13) | < 0.005 |
| Admission IV antibiotics | 250 | 202 (81) | 48 (19) | < 0.005 |
Discussion
The COVID-19 pandemic resulted in significant changes to the provision of dental care in the UK. Whilst other studies have assessed individual hospital experience with odontogenic infections, to our knowledge this is the first to include multicentre data across the UK, and to ask the treating team how the care provided would compare with that offered under normal conditions.6, 7
Using opinion rather than comparing the data is a weakness of this study, as is the lack of denominator data of the total number of patients presenting in relation to those included.
Almost three-quarters of all patients presented first to the emergency department (ED), with the remaining quarter directed according to national guidelines via referral from the national advice telephone line (NHS 111) or UDCCs. This may reflect the national variation in patient awareness and accessibility, as well as the inevitable growing demand for UDCCs throughout lockdown.8 Similarly, it is not clear whether UDCCs advised patients to attend the ED without contacting OMFS directly. Good communication between OMFS and UDCC services is essential to streamline patient pathways, especially in the context of reducing COVID-19 exposure in the future.
In keeping with the experiences of the UDCCs during COVID-19, the most common presentation was periapical periodontitis, often from molars and least often from anterior teeth.3 The majority of patients were treated with oral antibiotics as outpatients rather than with intravenous antibiotics as inpatients, illustrating the shift towards outpatient management to minimise the risk of in-hospital exposure to COVID-19 and infection.
As expected, space infections associated with lower molars, especially third molars, were managed with extraoral incision and drainage more than any other subset of teeth, reflecting the typical location of abscess formation in these teeth. Fortunately, only five patients required an admission to intensive care and no patient died.
Due to COVID-19, almost 300 patients had their treatment modified whilst under the care of OMFS teams. Clinicians reported approximately a quarter of patients undergoing extractions who would not have done so prior to COVID. The database did not record whether this variance was because the teeth were restorable or because extraction would not usually have been offered and the patient instead directed to their own dentist for further care. Another 28% of patients given antibiotics would not have received them prior to COVID. This may have been cautious prescribing to prevent representation, or OMFS providing treatment that would usually have been provided in primary care.
The reasons cited for a change in treatment were predominantly ‘to preserve hospital resources’, including theatre, operating personnel, and PPE. The impact of COVID-19 positive status appears to have had little conscious impact on patient management, perhaps as most patients were of unknown COVID-19 status at the time.
Few patients’ treatment under GA was at variance from pre-COVID care. This is to be expected, as patients with a sufficiently serious infection to warrant surgery under GA would need this treatment. A larger number of patients who received dental extraction/drainage under LA would not have received one before the pandemic and could have had either GA or antibiotics or no treatment. Reasons for down-staging from management under GA may have been to preserve already scarce resources, such as anaesthetists, emergency theatres, or bed capacity, as well as an increased acceptance by patients of LA procedures. Similarly, OMFS clinicians may have taken a more proactive approach in patients they would have otherwise managed conservatively, opting for LA incision and drainage and/or antibiotics to minimise the risk of re-collection and re-attendance. This may have been facilitated by the presence of more senior OMFS staff in the emergency department who were making more rapid decisions and treatment plans to minimise the exposure of patients to COVID-19.
A significant number of patients who presented to secondary care received no treatment. This suggests they were patients with pulpitis who normally would have been managed by GDPs via telephone triage or UDCCs. This was also found in a COVID paper from an individual OMFS unit.9 About a third of the patients referred from a UDCC were still treated without active surgery. UDCC services were formed as a reaction to the pressures of COVID-19, and their organisation was often led locally with variable provision of PPE in the early stages of lockdown. These centres may not have been able to cope with the demand, or patients were not aware of the facilities available.
In view of a second wave or alternative infectious disease, our recommendations are to build stronger communication links between OMFS and UDCCs. This would serve not only to provide the best possible care in a pandemic, but would also minimise the risks of exposure to COVID and reduce the strain on emergency departments.10
Our aim was to assess the impact of COVID on patients with odontogenic CFIs who presented to OMFS during national lockdown in the UK, based on the perception of the clinical team. Complementary studies can assess the presentation of odontogenic infection pre-COVID and peri-COVID in individual hospitals, as well as the impact that the local prevalence of COVID and local access to UDCCs have on the hospital management of these patients. This will prove useful in future infective outbreaks in terms of resource planning, both at a hospital level for local provision of UDCCs and to support GDPs.
List of collaborators who participated in the infection study
Aidan Adams, Ayesha Ahmed, Huma Aiman, Lucy Alderson, Maha Aljefri, Jack Allison, Nishma Ardeshna, Mariam Asaad, Katriana Bacik, Indran Balasundaram, Matthew Barker, Lydia Barker-Chapman, Sherif Bayoumi, Robert Bentley, Vyomesh Bhatt, Manuel Blanco-Guzman, Angela Boscarino, Raghu Boyapati, Deborah Boyd, Theo Boye, Dirk Stephanus Brandsma, Laura Brooks, Timothy Brown, Marta Cabral, Micheala Camilleri, Kris Carroll, Laura Chapman, Anna Chrystal, Sarah Clyde, Tom Cole, Zachary Cole-Healy, Benjamin Collard, Sarah Crummey, Roger Currie, Anna Dahill, Huw T. Davies, Rumandeep Dhillon, David Drake, Rebecca Exley, Kathleen Fan, Shona Feare David Fisher, Lynne Fryer, Andrew Fulton, Andrew Gardner, Shona Garland, Peter Glen, David Graham, Catherine Grant Elizabeth Gruber, Ben Gurney, Nick Hampton, Abeer Hasan, Kerry Herd, Stuart Hislop, Michael Ho, Ceri Hughes, Hannah Huguet, Huw Jones, Shyam Karia, Karim Kassam, Mairead Kelly, Steven Key, Farhan Khalid, Rhydian King, Raghav Kulkarni, Anand Kumar, Deepshikha Kumar, Paul Lang, Kirstie Lau, David Laugharne, Nicholas J. Lee, Leh Lim, Terrence Lowe, Patrick Magennis, Vasanthan Manoharan, Louisa McCaffrey, Nicola McCurley, Christopher McDonald, Ian McHenry, Edward McParland, Hussein Mohammedbhai, Heather Morgan, Colm Murphy, Dara Murphy, Ayesha Mustafa, Kowoon Noh, Kerry O'Brien, Kevin O'Grady, Lewis Olsson, Joan Onochie, Anika Patel, Ankit Patel, Jayna Patel, Sachit Patel, Rajat Paul, Samantha Plant, Ioanna Politti, Eoin Power, Dhulshan Preena, Fabien Puglia, Euan Rae, Eson Rasikh, Neelam Rathod, Dhurrika Raveendran, Zahrah Raza, Charlotte Richards, Martyn Ritchie, Hamed Safaei, Sunil Sah, Kiren Sall, Susan Sanders, Rupert Scott, Keval Shah, Kishore Shekar, Faheema Sidat, Branan Sivanantha, Claire Skimming, James Sloane, Rebecca Smith, Caroline Smith, Kohmal Solanki, Andrew Stirrup, Imran Suida, Jill Sweeney, Eleanor Swinnerton, Eilidh Thomas, Sundeep Thusu, Hannah Tompkins, Clare Tyers, Drazsen Vuity, Callum Wemyss, Lindsey Young.
Conflict of interest
We have no conflicts of interest.
Funding
Funding for the subscription to the REDCap database was part funded by the British Association of Oral and Maxillofacial Surgeons and the Saving Faces Charity (www.savingfaces.co.uk).
Ethics statement/Confirmation of patients’ permission
Neither ethics approval nor patients’ permission was required.
Acknowledgement
We would like to thank all the clinicians from each of the units who participated.
References
- 1.Hurley S, Rooney E, Reece C. Issue 2 preparedness letter for primary dental care 20 March 2020. Available from URL: https://www.gdc-uk.org/docs/default-source/covid-19/issue-2-prepardness-letter-for-primary-dental-care-20-march-2020.pdf?sfvrsn=69d46d90_2 (last accessed 2 April 2021).
- 2.Further advice from CDO for primary dental care 25 March 2020. External announcement. Available from URL: https://www.mddus.com/coronavirus/coronavirus-update/2020/march/preparedness-letter-for-primary-dental-care (last accessed 2 April 2021).
- 3.Long L., Corsar K. The COVID-19 effect: number of patients presenting to The Mid Yorkshire Hospitals OMFS team with dental infections before and during the COVID-19 outbreak. Br J Oral Maxillofac Surg. 2020;58:713–714. doi: 10.1016/j.bjoms.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris P.A., Taylor R., Thielke R. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris P.A., Taylor R., Minor B.L. The REDCap consortium: building an international community of software partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Politi I., McParland E., Smith R. The impact of COVID-19 on cervicofacial infection of dental aetiology. Br J Oral Maxillofac Surg. 2020;58:1029–1033. doi: 10.1016/j.bjoms.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Currie C.C., Stone S.J., Connolly J. Dental pain in the medical emergency department: a cross-sectional study. J Oral Rehabil. 2017;44:105–111. doi: 10.1111/joor.12462. [DOI] [PubMed] [Google Scholar]
- 8.Carter E., Currie C.C., Asuni A. The first six weeks - setting up a UK urgent dental care centre during the COVID-19 pandemic. Br Dent J. 2020;228:842–848. doi: 10.1038/s41415-020-1708-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blackhall K.K., Downie I.P., Ramchandani P. Provision of emergency maxillofacial service during the COVID-19 pandemic: a collaborative five centre UK study. Br J Oral Maxillofac Surg. 2020;58:698–703. doi: 10.1016/j.bjoms.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pajpani M., Patel K., Bendkowski A. Rapid response: activity from a hospital based Urgent Dental Care Centre during the COVID-19 pandemic. Br J Oral Maxillofac Surg. 2020;58:e98–e103. doi: 10.1016/j.bjoms.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]