Abstract
Objectives
The implementation of social confinement measures to reduce the spread of coronavirus disease 2019 (COVID-19) has limited the clinical and laboratory diagnosis of sexually transmitted diseases (STDs) and their transmission. This study aims to explore the epidemiological behaviour of two notifiable STDs during the first 6 months of the COVID-19 pandemic in Cuba.
Study design
This is an exploratory study of the incidence rates of syphilis and gonorrhoea during the COVID-19 pandemic in Cuba.
Methods
This study compares national weekly surveillance data on syphilis and gonorrhoea incidence rates in Cuba with the timeline of implemented social confinement measures.
Results
Incidence rates for both STDs were declining before the first case of COVID-19 was identified in Cuba. Following the confirmation of COVID-19 in Cuba and the implementation of social confinement measures, the decreasing incidence rates of syphilis and gonorrhoea continued. When social measures were subsequently relaxed, there was an increase in the incidence of syphilis, but incidence levels of gonorrhoea remained at a plateau.
Conclusions
The results of this study suggest that the social measures introduced to curb the spread of COVID-19 influenced the sexual risk behaviours of individuals and subsequently modified the incidence of syphilis and gonorrhoea. It is necessary to continue epidemiological surveillance for longer periods of time and to explore it at the local, regional and national levels to better understand STDs in times of COVID-19.
Keywords: COVID-19, SARS-CoV-2, STD, Syphilis, Gonorrhoea
In Cuba, the first cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, causing the coronavirus disease 2019 (COVID-19), were reported on 11 March 2020 (epidemiological week 11) [1]; coinciding with the day when the World Health Organisation declared COVID-19 a pandemic. Community transmission of COVID-19 was recorded 4 weeks later in Cuba [2].
Since the beginning of the pandemic in Cuba, and according to the epidemiological situation, the government and the Ministry of Public Health have taken measures to reduce COVID-19 transmission. The main actions, at first, were social distancing and hygienic-sanitary measures. However, when community transmission was declared, it was necessary to reduce population mobility by stopping transportation and increasing social and physical distancing. In addition to social and sanitary measures, in localities with high transmission rates, quarantine/lockdown measures were established, and ambulatory and external consultation services were limited in some health institutions [2].
In June, after an improvement in the COVID-19 epidemiological situation in Cuba, restrictions were relaxed and activities resumed (phase 1 of post-COVID-19 recovery); including the reopening of national tourism, transportation, nightclubs, swimming pools, beaches, as well as other socialisation and recreational facilities [3]. However, as of 1 September, due to an increase in the number of people infected by SARS-CoV-2, stricter social confinement measures was reinstated in the capital for 1 month (including the limitation of movements of people and vehicles from 7pm to 5am) and quarantine/lockdown was declared in other affected regions [4].
Some studies have investigated the effect of COVID-19 on the incidence of sexually transmitted diseases (STDs); the lockdown that was implemented as a result of the pandemic has limited the clinical and laboratory diagnosis of STDs and presumably also their transmission [5,6]. This study compares syphilis and gonorrhoea incidence rates in Cuba with the timeline of social confinement measures implemented to reduce the spread of SARS-CoV-2 infection.
Syphilis and gonorrhoea are notifiable diseases in Cuba, treated mainly in primary care health centres and their diagnoses are aetiological (case confirmation by specific laboratory tests) [7].
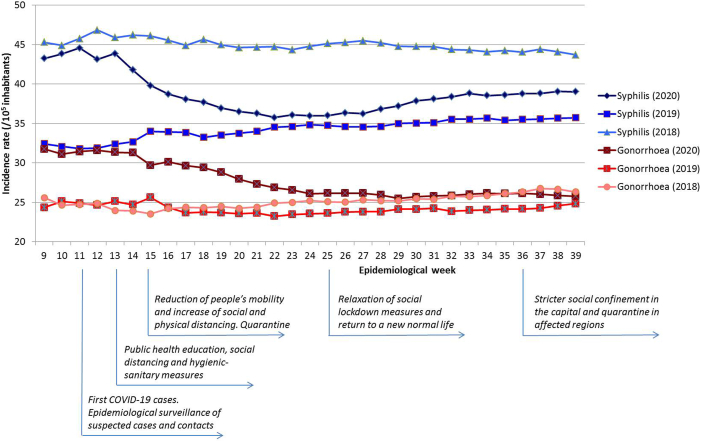
The nationwide weekly surveillance data from the Weekly Epidemiological Bulletins of the Tropical Medicine Institute “Pedro Kourí” [8] and the Statistical Yearbook of Health [9] show that the incidence of syphilis and gonorrhoea declined in the first half of 2020 (see Fig. 1). Both syphilis and gonorrhoea have reported this trend annually since 2018 and 2013, respectively.
Fig. 1.
Syphilis and gonorrhea incidence rates per week during 2018–2020 and the timeline of social measures to reduce the spreading of COVID-19 during 2020 in Cuba.
Comparing incidence rates for syphilis and gonorrhoea between June and September 2020, an increase of syphilis incidence is seen (from 36.34 to 39 cases/100,000 inhabitants per week) and a plateau (similar to the historical behaviour in 2018 and 2019) for gonorrhoea (around 26 cases/100,000 inhabitants per week) [see Fig. 1. During this time, an increase in the number of individuals and regions affected by SARS-CoV-2 infection was also reported. Young and middle-aged groups had the highest number of cases, but were also the least vulnerable population to develop severe clinical forms of COVID-19 [1]. However, these age groups also have the highest sexual activity and at the highest risk of acquiring STDs; consequently, these individuals could be an important link in the transmission of STDs and COVID-19. It is important to mention that 60.8% of the Cuban population with SARS-CoV-2 infection were asymptomatic at the time of diagnosis [1], which presumably decreases the risk perception to this and other infectious diseases.
These results suggest that the relaxation of social lockdown measures and the return to a new normal life, including resuming sexual risk behaviours, led to the increased incidence of syphilis and maintained the usual pre-COVID 19 incidence rates of gonorrhoea.
The differences between the syphilis and gonorrhoea incidence rates could be a result of various different factors, including the following reasons. The consistent and correct use of latex condoms reduces the risk for STDs when the infected area or site of potential exposure is covered. However, during the early stages of syphilis, extragenital ulcers or skin lesions can be present that transmit the infection when a person is in direct contact. Condom use is often based on the perceived risk of infection and it can be difficult to recognise the signs and symptoms of STDs - a partner may only be perceived to be infected when clinical manifestations are evident (e.g. the presence of genital discharge or genital lesions), thus this may also increase the likelihood of transmission of some pathogens.
The decrease in the syphilis and gonorrhoea rates during the first weeks of the pandemic could be as a continuity of the historical epidemiological behaviour of these diseases or as a consequence of the measures that were introduced to deal with the COVID-19 pandemic. It is important to determine whether the reduced incidence rates of syphilis and gonorrhoea are due to a reduction in sexual risk behaviours of individuals or to a decrease in visits to medical services (attributable to the social confinement or to concerns about being exposed to COVID-19-infected people in health institutions, as it has been reported in other studies) [10]. [11] and thus reporting.
This exploratory approach investigating the influence of COVID-19 social measures on the incidence of syphilis and gonorrhoea during the first 6 months of pandemic in Cuba is based on statistical data for the country, but the incidences of these two STDs change according to the provinces and municipalities. Thus, it is recommended that further studies are carried out at the provincial and municipal levels, considering sex, gender, age, social and sexual contacts, risk perceptions and behaviours, as well as social determinants related to these STDs. This applies not only to Cuba, but also to countries that have been facing COVID-19 for longer periods of time, in order to have robust information for decision-makers in public health systems.
It is important to adapt the prevention measures for STDs to COVID-19 times, mainly in key populations that practice casual or transactional sex, such as young people, men who have sex with men and trans-gender persons. In addition, it is critical to monitor STD surveillance data and determine any epidemiological patterns that correlate with the timeline of implemented pandemic-response measures.
Figure. Syphilis and gonorrhea incidence rates per week during 2018–2020 and the timeline of social measures to reduce the spreading of COVID-19 during 2020 in Cuba.
Ethical approval
Not required. Ethical approval was not taken because the article was written on secondary data.
Funding
The authors did not receive any funding for this study.
Declaration of competing interestCOI
All authors declare no conflicts of interest.
Authors’ contributions
I.R. conceived the study and collected the data. I.R. and Y.H. analysed the data, wrote and revised the draft. Both authors read and approved the submitted manuscript.
Acknowledgements
The authors would like to thank Yosiel Molina for his critical revision of the language.
References
- 1.MINSAP. COVID-19 Cuba Data. 2020. https://covid19cubadata.github.io/#cuba [Google Scholar]
- 2.Martínez L. 2020. COVID-19: Cuba entró en fase de transmisión autóctona limitada.http://www.cubadebate.cu/noticias/2020/04/07/cuba-en-fase-de-transmision-autoctona-limitada/ [Google Scholar]
- 3.Editora política. Etapa de recuperación pos COVID-19: medidas a implementar en sus tres fases. 2020. http://media.cubadebate.cu/wp-content/uploads/2020/06/Etapa-de-recuperación-pos-COVID-19-medidas-a-implementar-en-sus-tres-fases.pdf [Google Scholar]
- 4.Alonso R., Figueredo O., Doimeadios D., García D., Terrero A. 2020. COVID-19: Nuevas medidas restrictivas para reforzar el aislamiento físico en La Habana.http://www.cubadebate.cu/noticias/2020/08/27/covid-19-nuevas-medidas-restrictivas-para-reforzar-el-aislamiento-fisico-en-la-habana/ [Google Scholar]
- 5.Latini A., Magri F., Donà M.G., Giuliani M., Cristaudo A., Zaccarelli M. Is COVID-19 affecting the epidemiology of STIs? The experience of syphilis in Rome. Sex. Transm. Infect. 2020:1. doi: 10.1136/sextrans-2020-054543. [DOI] [PubMed] [Google Scholar]
- 6.Białynicki-Birula R., Siemasz I., Otlewska A., Ł Matusiak, Szepietowski J.C. Influence of COVID-19 pandemic on hospitalizations at the tertiary dermatology department in south-west Poland. Dermatol. Ther. 2020;33(4) doi: 10.1111/dth.13738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MINSAP. Plan . 2019. Estratégico Nacional para la prevención y control de las ITS, VIH y las hepatitis (2019-2023)http://www.bvs.sld.cu/libros/plan_estrategico/plan_estrategico_its_vih_hepatitis.pdf [Google Scholar]
- 8.Boletín Epidemiológico del IPK https://instituciones.sld.cu/ipk/bolipk/ Available from URL:
- 9.Anuario Estadistico de Salud 2019. https://files.sld.cu/bvscuba/files/2020/05/Anuario-Electrónico-Español-2019-ed-2020.pdf Available from URL:
- 10.Li W., Li G., Xin C., Wang Y., Yang S. Changes in sexual behaviors of young women and men during the coronavirus disease 2019 outbreak: a convenience sample from the epidemic area. J. Sex. Med. 2020;17(7):1225–1228. doi: 10.1016/j.jsxm.2020.04.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shilo G., Mor Z. COVID-19 and the changes in the sexual behavior of men who have sex with men: results of an online survey. J. Sex. Med. 2020;17(10):1827–1834. doi: 10.1016/j.jsxm.2020.07.085. [DOI] [PMC free article] [PubMed] [Google Scholar]