Abstract
Background
Management of ST-elevated myocardial infarction (STEMI) necessitates rapid reperfusion. Delays prolong myocardial ischemia and increase the risk of complications, including death. The COVID-19 pandemic may have affected management of STEMI. We evaluated the relative volume of hospitalizations and clinical time intervals within a regional STEMI system.
Methods
Four hundred ninety-four patients with STEMI were grouped into prelockdown, lockdown, and reopening cohorts. Clinical, temporal, and outcome data were collected and compared among groups for both urban and rural patients, receiving primary percutaneous coronary intervention (PCI) and pharmacoinvasive revascularization, respectively. Data were compared with a 10-year historical comparator.
Results
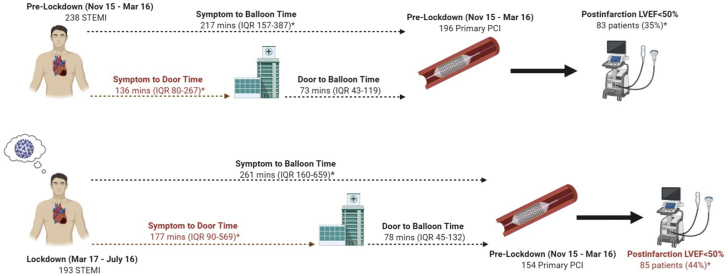
During prelockdown, there were 238 cases vs 193 in lockdown: a 19.0% reduction in volume. When lockdown was compared with the median caseload from a 10-year historical cohort, a 19.8% reduction was observed. For patients treated with primary PCI during lockdown, median symptom-to-balloon time increased by 44 minutes (217 interquartile range [IQR: 157-387] vs 261 [IQR: 160-659] minutes; P = 0.03); driven by an increase in median symptom-to-door time of 41 minutes (136 [IQR: 80-267] vs 177 [IQR: 90-569] minutes; P < 0.01). Only patients transferred from non-PCI facilities demonstrated an increase in door-to-reperfusion time (116 [IQR: 93-150] vs 139 [IQR: 100-199] minutes; P < 0.01). More patients had left-ventricular dysfunction during the lockdown (35% vs 44%; P = 0.04), but there was no difference in mortality.
Conclusions
During the COVID-19 lockdown, fewer patients presented with STEMI. Time-to-reperfusion was significantly prolonged and appeared driven predominantly by patient level and transfer delays. Public education and systems-level changes will be integral to STEMI care during the second wave of COVID-19.
Résumé
Contexte
La prise en charge de l’infarctus du myocarde avec élévation du segment ST (STEMI) nécessite une reperfusion rapide. Tout retard de reperfusion prolonge l’ischémie myocardique et augmente le risque de complications, y compris le risque de décès. Il est possible que la pandémie de COVID-19 ait nui à la prise en charge du STEMI. Nous avons donc évalué le nombre relatif d’hospitalisations et le temps écoulé avant la reperfusion au sein d’un système régional de traitement des STEMI.
Méthodologie
Au total, 494 patients ayant présenté un STEMI ont été divisés en trois cohortes : préconfinement, confinement et déconfinement. Les données cliniques et temporelles et les données relatives aux résultats ont été recueillies et comparées entre les groupes pour les patients vivant en milieu urbain et en milieu rural, les patients ayant subi une intervention coronarienne percutanée (ICP) en soins primaires et les patients ayant subi une revascularisation pharmaco-effractive, respectivement. Les résultats ont été comparés aux données historiques des dix dernières années.
Résultats
On a dénombré 238 cas durant la période précédant le confinement comparativement à 193 durant le confinement, ce qui représente une diminution de 19,0 %. Si on compare les données de la période de confinement à celles de la cohorte historique des 10 dernières années, on observe une réduction de 19,8 % du nombre médian de cas survenus. Dans le cas des patients traités par ICP en soins primaires durant le confinement, le temps médian écoulé entre l’apparition des symptômes et l’insertion du ballonnet a augmenté de 44 minutes (217 [intervalle interquartile {IIQ} : 157 à 387], par rapport à 261 [IIQ : 160 à 659] minutes; p = 0,03), en raison d’une augmentation de 41 minutes (136 [IIQ : 80 à 267] vs 177 [IIQ : 90 à 569] minutes; p < 0,01) du temps médian écoulé entre l’apparition des symptômes et l’arrivée à l’hôpital. Seuls les patients transférés depuis un établissement n’ayant pas les moyens d’effectuer une ICP ont affiché une augmentation du temps écoulé entre l’arrivée à l’hôpital et la reperfusion (116 [IIQ : 93 à 150] vs 139 [IIQ : 100 à 199] minutes; p < 0,01). Un plus grand nombre de patients ont présenté une dysfonction ventriculaire gauche durant le confinement (35 % vs 44 %; p = 0,04), mais il n’y avait pas de différence quant à la mortalité.
Conclusions
Pendant le confinement dû à la COVID-19, le nombre de patients hospitalisés pour un STEMI a diminué. Le temps écoulé avant la reperfusion était significativement plus long; cette augmentation semble principalement attribuable au temps écoulé entre l’apparition des symptômes et l’arrivée à l’hôpital et à la nécessité de transférer les patients vers un établissement en mesure d’effectuer une ICP. La sensibilisation du public et des modifications à l’échelle des systèmes devront faire partie de la stratégie de traitement du STEMI pendant la deuxième vague de la pandémie de COVID-19.
During the COVID-19 pandemic, a reduction in patients presenting with ST-elevated myocardial infarction (STEMI) has been reported.1,2 These studies lacked data on important areas including impact of the COVID-19 lockdown on STEMI care in regions with low incidence of disease, granular details regarding reperfusion management during lockdown, effect of the pandemic on STEMI care in rural regions, and patterns of STEMI volume post–COVID-19 lockdown. It is imperative to study the effects of COVID-19 comprehensively, so that lessons can be learned for a potential second wave or future pandemics.
From March 11, 2020, to August 16, 2020, the Ottawa regions recorded 2761 cases of COVID-19 and 267 COVID-19–related deaths.3 In response to the initial outbreak, the Ontario Ministry of Health declared a state of emergency and instituted lockdown measures on March 17, 2020.4 Various restrictions were imposed including closure of nonessential businesses, limits on social gatherings, and cancellation of elective medical procedures.4 These interventions were successful in limiting the spread of COVID-19; however, concerns regarding an unintended impact on STEMI care were raised.3,5
The University of Ottawa Heart Institute (UOHI) is the hub of STEMI care for the city of Ottawa and the surrounding Champlain region, a largely rural population. UOHI provides access to primary percutaneous coronary intervention (pPCI) and pharmacoinvasive (PI) revascularization for patients presenting with STEMI in urban and rural settings, respectively. In anticipation of the COVID-19 lockdown, the UOHI STEMI and PCI protocols were extensively modified owing to potential changes in cardiac patient care. Accordingly, we set a comprehensive evaluation of STEMI volume and changes in critical time intervals to determine the effects of the COVID-19 lockdown on management of STEMI.
Methods
Study setting
The UOHI STEMI program is a quaternary care dedicated cardiac facility that is the regional hub for a high-volume STEMI program. It services more than 1.3 million people, from both rural and urban communities, and treats more than 700 patients with STEMIs yearly. Because of its broad catchment area, the UOHI STEMI program includes patients managed with both primary percutaneous coronary intervention (pPCI) and pharmacoinvasive (PI) revascularization strategies. Patients presenting within approximately 100 kilometers may be transferred to the UOHI directly from the field or from a local emergency department for pPCI. Patients presenting from beyond 100 km are managed with a PI approach and transferred immediately to the UOHI after receiving fibrinolytic therapy in the local emergency department. Once assessed and preloaded with antithrombotic medications, patients are taken to the cardiac catheterization laboratory for PCI. The UOHI STEMI program is subject to constant quality assurance investigation that tracks key timing metrics and in-hospital outcomes, permitting data collection for the current study.
During the COVID-19 pandemic, several changes were implemented at the STEMI program to maintain timely and safe care. First, en route to UOHI, a screening assessment patient pretest for COVID-19 infection risk was performed. Second, 1 of the 4 cardiac catheterization laboratories was reorganized, suspended for use in elective cases, and reserved only for suspected cases of COVID-19. Third, the STEMI bay was relocated to an isolation room where staff, predonned in personal protective equipment (PPE), would await patient arrival and further assess COVID-19 risk. Patients at risk for COVID-19 infections were triaged to the dedicated catherization laboratory, where staff were predonned with PPE. Finally, a dedicated extra nurse was assigned to the COVID-19 catheterization laboratory to expedite flow.
Data source and search strategy
Retrospective chart review of electronic medical records (EMR) was performed on consecutive patients presenting from November 15, 2019, to August 16, 2020. All patients with discharge diagnoses of STEMI were analyzed. Patients were divided into 3 cohorts: prelockdown (November 15, 2019, to March 16, 2020), lockdown (March 17, 2020, to July 16, 2020), and reopening (July 17, 2020, to August 16, 2020). The chosen time periods were based on the province’s state of emergency and the regional phase 3 reopening, when most public health restrictions were lifted. The timelines provide an equal 121-day period between the prelockdown and lockdown cohorts, as well as a 30-day sample of STEMI admissions after reopening. The UOHI STEMI database was queried for a historical cohort of patients admitted during the lockdown months between 2009 and 2019, to generate a comparator.
Key variables
Key variables extracted and compared between cohorts include demographic and clinical characteristics, volume of STEMI admissions, presentation characteristics, time metrics for patients by reperfusion strategies, in-hospital mortality and presence of left-ventricular dysfunction (LVD) (defined by postinfarction transthoracic echocardiographic measurement of an ejection fraction of < 50%). The historical cohort was used as a comparator for differences observed in the number of STEMI admissions and time metrics in pPCI-treated patients. For timeline comparison between the lockdown and historical cohorts, only patients who presented within 24 hours of symptom onset were included, as late presenters (> 24 hours) were excluded in the UOHI pPCI STEMI database. Furthermore, the “door” times were readjusted based on ambulance off-loading of patients rather than EMR arrival times, to offer consistency with the historical data.
Statistical analysis
Normally distributed continuous variables are presented as mean +/– standard deviation. Variables with a skewed distribution are presented as median and interquartile range (IQR). Discrete variables are presented as frequencies. Normally distributed continuous variables were compared using the Student’s t-test. Variables with a skewed distribution were compared using the Mann-Whitney U test. Discrete variables were compared using the χ2 test or Fisher’s exact test. A P value of < 0.05 was considered statistically significant. Analysis was conducted using GraphPad Prism Version 8.4.3 (SYSTAT, San Jose, CA).
Results
Volume and patient characteristics by COVID-19 lockdown status
The results are summarized graphically in (Fig. 1).There were 238 and 193 STEMI admissions in the prelockdown and lockdown cohorts, respectively (Table 1). This accounts for a 19.0% reduction in STEMI admissions during the lockdown. Baseline characteristics were similar, except fewer smokers and patients with histories of previous myocardial infarction presented during the lockdown. No differences were observed in the mode of transport to hospital or the initial facility of presentation (Table 2). During the lockdown, 3 patients (2%) initially presented to a community-based COVID-19 testing centre and were transferred to UOHI. In the lockdown cohort, 36 patients with STEMI were classified as “suspected” for COVID-19 infection. Of these, only 1 was diagnosed with laboratory-confirmed COVID-19 infection. There were no differences in the strategies of revascularization between cohorts.
Figure 1.
Graphical summary of the differences in STEMI care during the COVID-19 lockdown. F/U, follow-up; IQR, interquartile range; LVEF, left-ventricular ejection fraction; PCI, percutaneous coronary intervention; STEMI, ST-elevated myocardial infarction. ∗Statistical significance with P < 0.05.
Adapted from BioRender.com (2021).
Table 1.
Baseline characteristics of patients presenting for management of STEMI before lockdown, during lockdown, and with reopening
| Prelockdown (November 15, 2019-March 16, 2020) | Lockdown (March 17, 2020-July 16, 2020) | Reopening (July 17, 2020-August 16, 2020) | |
|---|---|---|---|
| STEMI admissions | 238 | 193 | 63 |
| Demographics | |||
| Age | 64 ± 13 | 65 ± 12 | 62 ± 12 |
| Male (%) | 169 (71%) | 135 (70%) | 49 (78%) |
| BMI | 28 ± 6.0 | 28 ± 5.6 | 37 ± 6.1 |
| Medical history | |||
| Hypertension | 123 (52%) | 98 (51%) | 28 (44%) |
| Dyslipidemia | 99 (42%) | 86 (45%) | 22 (35%) |
| Diabetes | 54 (23%) | 55 (28%) | 15 (24%) |
| Current smoker | 93 (39%) | 53 (27%)∗† | 26 (41%) |
| Ex-smoker | 22 (9%) | 26 (13%) | 4 (6%) |
| Cardiac family history | 51 (21%) | 41 (21%) | 13 (20%) |
| Previous CAD | 38 (16%) | 42 (22%) | 15 (24%) |
| Previous MI | 22 (9%) | 24 (12%)† | 15 (24%) |
| Previous PCI | 22 (9%) | 26 (13%) | 11 (17%) |
| Previous CABG | 8 (3%) | 7 (4%) | 2 (3%) |
| Stroke or TIA | 11 (5%) | 13 (7%) | 2 (3%) |
| Pulmonary disease | 16 (7%) | 13 (7%) | 3 (5%) |
| Home medications | |||
| Aspirin | 45 (19%) | 30 (16%) | 12 (19%) |
| P2Y12 Inhibitors | 12 (5%) | 9 (5%) | 3 (5%) |
| β-Blocker | 27 (11%) | 31 (16%) | 9 (14%) |
| ACEi/ARB | 66 (28%) | 55 (28%) | 12 (19%) |
| Oral antihyperglycemic | 37 (16%) | 34 (18%) | 11 (17%) |
| Statin | 72 (30%) | 60 (31%) | 16 (25%) |
| Anticoagulant | 9 (4%) | 12 (6%) | 0 (0%) |
| Preprocedure medications | |||
| Aspirin | 229 (96%) | 178 (92%) | 59 (94%) |
| P2Y12 Inhibitors | 228 (96%) | 188 (97%) | 60 (95%) |
| Heparin | 227 (95%) | 184 (95%) | 60 (95%) |
ACEi, angiotensinogen converting enzyme inhibitor; ARB, angiotensin receptor blocker; BMI, body mass index; CABG, coronary artery bypass grafting; CAD, coronary artery disease; MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-elevated myocardial infarction; TIA, transient ischemic attack.
Statistical difference (P < 0.05) between the lockdown and prelockdown cohorts.
Statistical difference (P < 0.05) between the lockdown and reopening.
Table 2.
Summary of presentation and revascularization strategies in patients with STEMI presenting before, during, and after the COVID-19 lockdown
| Prelockdown (N = 238) (November 15, 2019-March 16, 2020) |
Lockdown (N = 193) (March 17, 2020-July 16, 2020) |
Reopening (N = 63) (July 17, 2020-August 16, 2020) |
|
|---|---|---|---|
| Mode of transport | |||
| Self-present | 46 (19%) | 40 (21%) | 11 (18%) |
| EMS | 193 (81%) | 153 (79%) | 51 (82%) |
| Facility of presentation | |||
| COVID center | N/A | 3 (2%) | 0 (0%) |
| Peripheral hospital | 148 (62%) | 112 (58%) | 31 (50%) |
| Field transfer | 91 (38%) | 78 (40%) | 31 (50%) |
| Revascularization strategy | |||
| Primary PCI | 196 (82%) | 154 (80%) | 49 (79%) |
| Pharmacoinvasive | 26 (11%) | 22 (11%) | 6 (10%) |
| Emergent CABG | 8 (3%) | 6 (4%) | 5 (8%) |
| Medical therapy | 8 (3%) | 11 (5%) | 3 (3%) |
CABG, coronary artery bypass grafting; EMS, emergency medical services; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
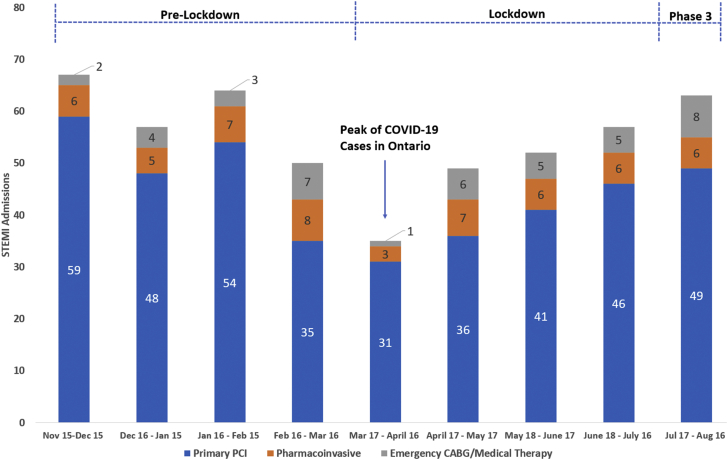
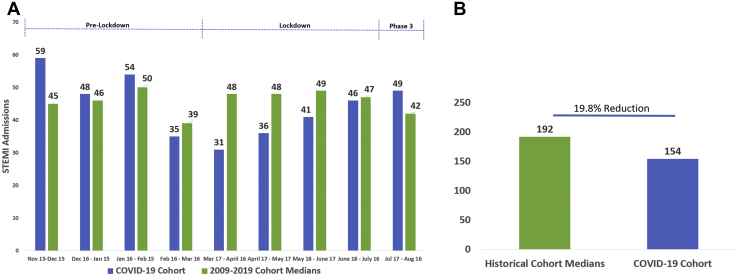
The distribution of cases over the entire study was U-shaped, with the nadir occurring March 17 to April 16, and a rebound in volume with reopening (Fig. 2). There was no difference in the decrease in volume between urban and rural patients. The distribution of cases in the historical cohort was steady, with little variation between months of presentation (Fig. 3A). There were decreases in STEMI volumes during the lockdown months compared with the historical cohort (Fig. 3A) and a numerical trend for increasing STEMIs toward reopening. Overall, there was a 19.8% reduction in total STEMI admissions between the lockdown cohort and historical cohorts (Fig. 3B).
Figure 2.
Number of admissions for ST-elevated myocardial infarction before, during, and after the COVID-19 lockdown. Blue bars denote patients managed with primary percutaneous coronary intervention; orange bars denote patients managed with pharmacoinvasive revascularization; gray bars denote patients managed with emergency coronary artery bypass grafting or medical therapy.
Figure 3.
(A) Number of patients treated with primary percutaneous coronary intervention for ST-elevated myocardial infarction (STEMI) before, during, and after the COVID-19 lockdown. Data are grouped into month periods and compared with a 10-year historical cohort (median volume per month, 2009 to 2019). Blue shaded bars represent patients with STEMI from the COVID-19 lockdown cohort. Green shaded bars represent patients with STEMI from a 10-year historical dataset. (B) Comparison of total admissions for STEMI during the COVID-19 months with a historical cohort from 2009 to 2019, during the same period.
Time intervals for primary PCI compared by COVID-19 lockdown status
Time intervals for reperfusion are shown in Table 3. Among patients receiving pPCI, there was a 41-minute increase in median symptom-to-door (S2D) time between the prelockdown and lockdown cohorts (136 [IQR: 80-267] vs 177 [IQR: 90-569] minutes; P < 0.01). The median S2D time decreased numerically by 54 minutes between the lockdown and reopening cohorts (177 [IQR: 90-569] vs 123 [IQR: 75-375] minutes; P = 0.13). No statistical difference in door-to-balloon (D2B) time was identified between cohorts. There was a significant increase of 44 minutes in the median symptom-to-balloon (S2B) time between the prelockdown and lockdown cohorts (217 [IQR: 157-387] vs 261 [IQR: 160-659] minutes; P = 0.03). A numerical decrease of 38 minutes in median S2B time was observed between the lockdown and reopening cohorts (261 [IQR: 160-659] vs 223 [IQR: 165-525] minutes; P = 0.38). A significant increase in patients presenting > 12 hours (7.7 vs 21.4%; P < 0.01) and > 24 hours (3.0 vs 9.7%; P < 0.01) after symptom onset was present between the prelockdown and lockdown cohorts.
Table 3.
Summary of time intervals for patients presenting for primary percutaneous coronary intervention before, during and after the COVID-19 lockdown
| Prelockdown (November 15, 2019-March 16, 2020) | Lockdown (March 17, 2020-July 16, 2020) | Reopening (July 17, 2020-August 16, 2020) | |
|---|---|---|---|
| Primary PCI | N = 196 | N = 154 | N = 49 |
| Symptom-door | 136 (80-267) | 177 (90-569)∗ | 123 (75-375) |
| Presentation > 12 hrs | 15 (7.7%) | 28 (21.4%)∗ | 4 (8%) |
| Presentation > 24 hrs | 6 (3.0%) | 15 (9.7%)∗ | 2 (4%) |
| Door-balloon (all) | 73 (49-119) | 78 (45-132) | 71 (56-100) |
| Door-balloon (field) | 51 (30-65) | 46 (30-62) | 59 (40-73) |
| Door-balloon (transfer) | 120 (92-159) | 128 (96-186) | 114 (82-199) |
| Symptom-balloon | 217 (157-387) | 261 (160-659)∗ | 223 (165-525) |
| Pharmacoinvasive | N = 26 | N = 22 | N = 7 |
| Symptom-door | 111 (73-174) | 148 (82-317) | 90 (49-164) |
| Door-needle | 28 (14-55) | 36 (24-93) | 26 (13-34) |
| Symptom-needle | 138 (108-225) | 191 (96-445) | 120 (83-177) |
| Door-balloon | 221 (191-355) | 287 (206-390) | 204 (168-296) |
| Symptom-balloon | 416 (274-510) | 436 (362-744) | 306 (265-371) |
Symptom-to-door time is defined as time from onset of chest pain to presentation at first medical facility. Door-to-balloon time is defined as time from presentation to medical facility and reperfusion across culprit lesion. Symptom-to-balloon time is defined as the time from chest pain onset to reperfusion across culprit lesion. All times are quantified in minutes.
Significant difference (P < 0.05) between Lockdown and Prelockdown groups.
When comparing time intervals with the historic control (Table 4), there was a significant 48-minute increase in S2D time between the lockdown and historical cohorts (96 [IQR: 57-207] vs 144 [IQR: 74-350] minutes; P < 0.01). A significant 23-minute increase was observed in D2B time for patients transferred from rural-based emergency departments (116 [IQR: 93-150] vs 139 [100-199] minutes; P < 0.01], but there was no difference in field patients or all comers. There was a significant increase in S2B time of 41 minutes between the historical and lockdown cohorts (207 [IQR: 140-352] vs 248 [IQR: 151-430] minutes; P < 0.01].
Table 4.
Summary of time intervals for patients treated with primary percutaneous coronary intervention for STEMI during COVID-19 lockdown compared with a historical cohort
| Lockdown (N = 139) (March 17, 2020-July 16, 2020) |
Historical (N = 1848) (2009-2019) |
|
|---|---|---|
| Symptom-door | 144 (74-350)∗ | 96 (57-207) |
| Door-balloon (all) | 85 (54-140) | 92 (62-125) |
| Door-balloon (field) | 54 (36-72) | 54 (38-72) |
| Door-balloon (transfer) | 139 (100-199)∗ | 116 (93-150) |
| Symptom-balloon time | 248 (151-430)∗ | 207 (140-352) |
For the contemporary group, patients with > 24 hours of chest pain were excluded and “door time” for lockdown period was adjusted to ambulance unloading time vs electronic medical record registration time, allowing direct comparison with historical data. The historical cohort represents patients with STEMI presenting from 2009 to 2019 over the same time periods of the lockdown cohort. Symptom-to-door time is defined as time from onset of chest pain to presentation at first medical facility. Door-to-balloon time is defined as time from presentation to medical facility and reperfusion across culprit lesion. Symptom-to-balloon time is defined as the time from chest pain onset to reperfusion across culprit lesion. All times are quantified in minutes.
STEMI, ST-elevation myocardial infarction.
Significant difference (P < 0.05) between lockdown and historical control cohort.
Time intervals for pharmacoinvasive revascularization strategy compared by COVID-19 lockdown status
For patients receiving PI revascularization, the S2D time was numerically increased between the lockdown and prelockdown cohorts (111 [IQR: 73-174] vs 148 [IQR: 82-317] minutes; P = 0.18). There was a nonsignificant increase in door to needle (D2N) time between the prelockdown and lockdown cohorts (28 [IQR: 14-55] vs 36 [IQR: 24-93] minutes; P = 0.23). Symptom-to-needle (S2N) time increased numerically, when comparing the prelockdown and lockdown cohorts (138 [IQR]: 108-225) vs 191 [IQR: 96-445] minutes; P = 0.32). D2B times numerically increased between the prelockdown and lockdown cohorts (221 [IQR: 191-355] vs 287 [IQR: 206-390] minutes; P = 0.41). Overall, S2B times for this cohort were nonsignificantly but numerically longer (416 [IQR: 274-510] vs 436 [IQR: 362-744] minutes; P = 0.28).
In-hospital and echocardiographic outcomes
No difference was observed in the rates of in-hospital death (15 [6.3%] vs 11 [5.7%] ; P = 0.79) or median length of stay (4 [IQR: 2-7] vs 4 [IQR: 2-6]; P = 0.42) between prelockdown and lockdown cohorts. There was an increase in patients with postinfarction LVD between the prelockdown and lockdown cohorts (83 [35%] vs 85 [44%]; P = 0.04).
Discussion
Our study evaluated STEMI care in a large region, with a relatively low incidence of COVID-19, consisting of both urban and rural patients. The major findings included: a 19.0% and 19.8% reduction in STEMI admissions when comparing the lockdown cohort with the prelockdown and historical cohorts, respectively; a reduction in volume was equal irrespective of urban or rural settings; S2B time was increased during the lockdown, with a delay incurred predominantly by a prolonged S2D time, a trend consistent for urban and rural patients; D2B times for transfer patients—but not patients triaged from the field—were increased during the COVID-19 lockdown; more patients presented with late infarctions, corresponding to an increase in postinfarction LVD during the lockdown; and a return to prelockdown volume was observed with reopening of the region.
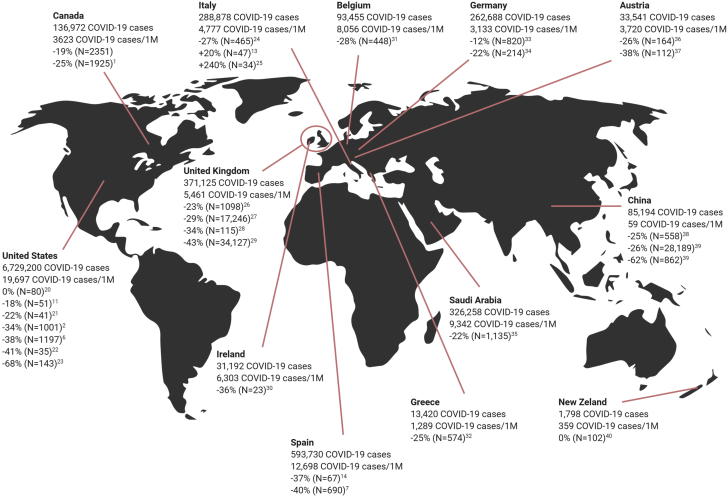
Our study demonstrated a near 20% reduction in STEMI admissions during COVID-19. Our reduction in STEMI volume is substantially smaller than the 40% drop seen in the United States and Spain.6,7 There was a vast discrepancy in incidence of COVID-19 between Canada and the United States or Spain, yet there was still a marked decline in STEMI in our jurisdiction. This suggests that patient perception may be a main driver for decreased STEMI volume, a trend that is further supported by documentation worldwide (Fig. 4). The reduction of STEMI admissions observed in Ottawa is similar to data from the province of Ontario, which demonstrated between a 18% and 25% reduction in cases of STEMI.1 The nadir of our STEMI admissions occurred between March 17 and April 16: the period of peak incidence of COVID-19 during the Ontario lockdown. Subsequently, the mean cases per month gradually rose into the reopening period, when incident COVID-19 cases began to fall and public health restrictions were lifted. In context with other literature, our data imply that both the incidence of COVID-19 and resulting public health restrictions are important determinants of the reduction in cases of STEMI observed. The decrease in volume is likely multifactorial. A main driver may be hesitancy of patients to seek medical attention for fear of contracting COVID-19.8 The exact cause will not be elucidated; however, patients suffering STEMIs at home to avoid contracting COVID-19 is a major concern for a second wave of COVID-19.
Figure 4.
Summary of reports in literature demonstrating the drop in STEMI volume and relative prevalence of COVID-19.1,2,6,7,9,10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 For each country, the total number of COVID-19 cases, the cases per million, the drop in STEMI volume by percentages, and the size of the study are shown.
Adapted from BioRender.com (2021).
Public health messaging regarding social distancing has been effective, as patients generally support limiting in-person contact and staying at home.33 However, concern arises if these attitudes are carried over to health care-seeking behaviour for acute illnesses such as STEMI. A significant finding in our study is the incurred delay to reperfusion during the lockdown period. The basis of the delay to treatment appeared attributable to patients presenting late after onset of symptoms, resulting in an increase in LVD during the lockdown. This is of particular concern, as patients presenting with late STEMIs have larger infarcts and are known to have higher incidence of heart failure and worse long-term outcomes.9,34 Our observed increase in S2D time is in keeping with findings in other studies.10,11,35 Early analysis of admissions to emergency departments during COVID-19 suggest that patients fear contracting COVID-19 at hospitals and are unclear about when to present for medical care.8 Notably, several of our patients with STEMI presented directly to community COVID-19 swab centres during the lockdown, with the impression that their symptoms may be caused by COVID-19. All this supports the importance of public education on the dangers of avoiding seeking medical attention and the need to inform the public on symptoms of myocardial infarction.36 With the anticipated second wave of COVID-19, and possible repeat lockdowns, it is imperative that public service announcements and associated strategies be considered by health agencies now.
COVID-19 overwhelmed health care systems, leading some interventional cardiologists to propose a switch to fibrinolytics as a first-line approach to STEMI reperfusion.37,38 Current guidelines in the province of Ontario advocate maintaining a pPCI approach during COVID-19.39 A previous Ontario-wide study of pPCI during COVID-19 showed increases in D2B times for patients triaged from the field; however, our study did not.1 This is likely based on the pre-emptive modifications to our system to avoid delays. We did observe an increase in D2B time for patients transferred for pPCI and PI revascularization, suggesting potential delays in noncardiac facility triaging systems and transfer protocols during the COVID-19 lockdown. Adaptation of the approach to STEMI triage at our institution and further amendments to transfer systems may help reduce hospital-level delays in STEMI care, especially if emergency medical services resources are strained during a second wave of COVID-19.
Study limitations
We report data from a single cardiac centre, so our study is reflective of the local STEMI program. However, our results are consistent to Ontario-wide data, which suggest that our findings are generalizable. Furthermore, our STEMI program services a large geographic area, consisting of both urban and rural surrounding communities, thus providing data not reported in previous studies. In addition, owing to the retrospective nature of our study, not all patients had complete clinical information. This resulted in 8 of 454 potential patients being excluded for the timeline analysis, as their complete clinical timelines could not be verified. This amounts to only a 2% exclusion rate and is therefore unlikely to affect findings. Finally, our study does not establish definitive causality for decrease in volumes or delays.
Conclusions
We demonstrated a 19.0% reduction in STEMI cases during COVID-19 lockdown. Time-to-reperfusion was significantly prolonged, with a predominant driver being patient-related factors and transfer delays. Public education and systems-level change will be integral to STEMI care during a second wave of COVID-19.
Funding Sources
There was no funding relevant to the present study.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: This study was approved by the Ottawa Health Science Network Research Ethics Board (OHSN-REB) and adheres to all relevant regulations.
See page 572 for disclosure information.
References
- 1.Natarajan M.K., Wijeysundera H.C., Oakes G. Early observations during COVID-19 pandemic in cardiac catheterization procedures for ST elevation myocardial infarctions (STEMI) across Ontario. CJC Open. 2020;2:678–683. doi: 10.1016/j.cjco.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gluckman T.J., Wilson M.A., Chiu S.-T. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020;5:1–6. doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daily COVID-19 Dashboard–Ottawa Public Health. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx Available at:
- 4.COVID-19 Guidance for the Health Sector–Ministry Programs–Health Care Professionals –MOH. http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/2019_guidance.aspx Available at:
- 5.Tanner R., MacDaragh Ryan P., Caplice N.M. COVID-19: where have all the STEMIs gone? Can J Cardiol. 2020;36:1161.e9–1161.e10. doi: 10.1016/j.cjca.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the united states during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodríguez-Leor O., Cid-Álvarez B., Ojeda S. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 8.Wong L.E., Hawkins J.E., Langness S. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020:1–12. [Google Scholar]
- 9.Afilalo J., Piazza N., Tremblay S., Soucy N., Huynch T. Symptom-to-door time in ST segment elevation myocardial infarction: overemphasized or overlooked? Results from the AMI-McGill study. Can J Cardiol. 2008;24:213–216. doi: 10.1016/s0828-282x(08)70587-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gramegna M., Baldetti L., Beneduce A. ST-segment-elevation myocardial infarction during COVID-19 pandemic: insights from a regional public service healthcare hub. Circ Cardiovasc Interv. 2020;13 doi: 10.1161/CIRCINTERVENTIONS.120.009413. [DOI] [PubMed] [Google Scholar]
- 11.Rebollal-Leal F., Aldama-López G., Flores-Ríos X. Impact of COVID-19 outbreak and public lockdown on ST-elevation myocardial infarction care in Spain. Cardiol J. 2020;27:425–426. doi: 10.5603/CJ.a2020.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lotfi A.S., Capatina A., Kugelmass A.D. Assessment of ST-segment elevation myocardial infarction volume trends during the COVID-19 pandemic. Am J Cardiol. 2020;131:132–133. doi: 10.1016/j.amjcard.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan W., Parikh R.V., Chester R. Single center trends in acute coronary syndrome volume and outcomes during the COVID-19 pandemic. Cardiol Res. 2020;11:256–259. doi: 10.14740/cr1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia S., Stanberry L., Schmidt C. Impact of COVID-19 pandemic on STEMI care: an expanded analysis from the United States. Catheter Cardiovasc Interv. 2020;11:1–6. doi: 10.1002/ccd.29154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammad T.A., Parikh M., Tashtish N. Impact of COVID-19 pandemic on ST-elevation myocardial infarction in a non-COVID-19 epicenter. Catheter Cardiovasc Interv. 2020;97:1–7. doi: 10.1002/ccd.28997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Rosa S., Spaccarotella C., Basso C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trabattoni D., Montorsi P., Merlino L. Late STEMI and NSTEMI patients’ emergency calling in COVID-19 outbreak. Can J Cardiol. 2020;36:1161.e7–1161.e8. doi: 10.1016/j.cjca.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mafham M.M., Spata E., Goldacre R. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu J., Mamas M., Rashid M. Patients response, treatments and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur Hear J Qual Care Clin Outcomes. 2020;4:39–44. doi: 10.1093/ehjqcco/qcaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdelaziz H.K., Abdelrahman A., Nabi A. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: insights from a British cardiac center. Am Heart J. 2020;226:45–48. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwok C.S., Gale C.P., Kinnaird T. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart. 2020;106:1805–1811. doi: 10.1136/heartjnl-2020-317650. [DOI] [PubMed] [Google Scholar]
- 22.Coughlan J.J., Chongprasertpon N., Arockiam S., Arnous S., Kiernan T.J. COVID-19 and STEMI: a snapshot analysis of presentation patterns during a pandemic. Int J Cardiol Heart Vasc. 2020;30:100546. doi: 10.1016/j.ijcha.2020.100546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Claeys M.J., Argacha J.F., Collart P. Impact of COVID-19-related public containment measures on the ST elevation myocardial infarction epidemic in Belgium: a nationwide, serial, cross-sectional study. Acta Cardiol. 2020;75:1–7. doi: 10.1080/00015385.2020.1796035. [DOI] [PubMed] [Google Scholar]
- 24.Papafaklis M.I., Katsouras C.S., Tsigkas G. “Missing” acute coronary syndrome hospitalizations during the COVID-19 era in Greece: medical care avoidance combined with a true reduction in incidence? Clin Cardiol. 2020;43:1–8. doi: 10.1002/clc.23424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scholz K.H., Lengenfelder B., Thilo C. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin Res Cardiol. 2020;109:1511–1521. doi: 10.1007/s00392-020-01703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rattka M., Baumhardt M., Dreyhaupt J. 31 days of COVID-19–cardiac events during restriction of public life: a comparative study. Clin Res Cardiol. 2020;109:1476–1482. doi: 10.1007/s00392-020-01681-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daoulah A., Hersi A.S. STEMI and COVID-19 pandemic in Saudi Arabia. 2021;46:100656. doi: 10.1016/j.cpcardiol.2020.100656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reinstadler S.J., Reindl M., Lechner I. Effect of the COVID-19 pandemic on treatment delays in patients with ST-segment elevation myocardial infarction. J Clin Med. 2020;9:1–10. doi: 10.3390/jcm9072183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tam C.C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xiang D., Xiang X., Zhang W. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elliott J.M., Crozier I.G. Decreases in cardiac catheter laboratory workload during the COVID-19 level 4 lockdown in New Zealand. Intern Med J. 2020;50:1000–1003. doi: 10.1111/imj.14922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Czeisler M.É., Tynan M.A., Howard M.E. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance: United States, New York City, and Los Angeles, May 5–12, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:751–758. doi: 10.15585/mmwr.mm6924e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McNair P.W., Bilchick K.C., Keeley E.C. Very late presentation in ST elevation myocardial infarction: predictors and long-term mortality. Int J Cardiol Heart Vasc. 2019;22:156–159. doi: 10.1016/j.ijcha.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braiteh N., Rehman W., Alom M. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J. 2020;226:147–151. doi: 10.1016/j.ahj.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahajan S., Valero-Elizondo J., Khera R. Variation and disparities in awareness of myocardial infarction symptoms among adults in the United States. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.17885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bainey K.R., Bates E.R., Armstrong P.W. ST-segment-elevation myocardial infarction care and COVID-19: the value proposition of fibrinolytic therapy and the pharmacoinvasive strategy. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006834. [DOI] [PubMed] [Google Scholar]
- 38.Daniels M.J., Cohen M.G., Bavry A.A., Kumbhani D.J. Reperfusion of ST-segment-elevation myocardial infarction in the COVID-19 era: business as usual? Circulation. 2020;141:1948–1950. doi: 10.1161/CIRCULATIONAHA.120.047122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Principles G. 2020. Recommendations for an Ontario approach to managing STEMI during COVID-19; pp. 5–7. Available at: https://www.corhealthontario.ca/CorHealth-COVID-19-Cardiac-Memo3-Recommendations-for-an-Ontario-Approach-to-Managing-STEMI-During-COVID-19.pdf. Accessed March 25, 2021. [Google Scholar]