2020 has been an unprecedented year because a modified coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), spread rapidly from China to all continents, leading to the COVID-19 pandemic. The first studies of COVID-19-associated sleep disorders were reported in China. Huang and Zhao1 collected information from a survey of 7236 volunteers (mean age 35·3 years [SD 5·6]). About a third of them were health-care workers. About 35% of these participants reported symptoms of general anxiety, 20% of depression, and 18% of poor sleep quality.1 The participants who were most worried about the pandemic also reported the most symptoms. Health-care workers were clearly under great pressure, which was reflected in the high prevalence of mental-health symptoms that they reported.1
The increased prevalence of sleep disorders in 2020 has also been highlighted in several other publications from different countries. These studies examined the effect on sleep of SARS-CoV-2 infection and confounders related to isolation, quarantine, anxiety, stress, or financial losses. According to a European task force, symptoms of insomnia could be related to psychosocial factors and to the confinements.2 In Italy, anxiety related to COVID-19 was highly associated with disturbed sleep. In a survey of 2291 Italians, 57·1% reported poor sleep quality, 32·1% high anxiety, 41·8% high distress, and 7·6% reported post-traumatic symptoms of stress.3 In the International COVID-19 Sleep Study,4 different factors are being investigated using a harmonised set of questions. Insomnia, nightmares, sleep apnoea, fatigue, exhaustion, and REM sleep behaviour disorder are being investigated by this collaboration.4 The hypothesis is that fatigue, sleepiness, and REM sleep behaviour disorder might be related to SARS-CoV-2 infection per se, whereas insomnia might be related mainly to confinement, anxiety, and other psychosocial factors.2
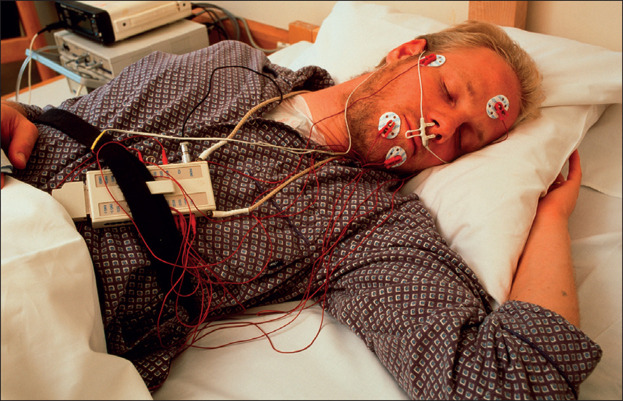
Although studies related to COVID-19 have dominated the field in 2020, other important investigations have also been published. Untreated severe sleep apnoea is associated with poor health and cardiovascular morbidity and mortality. However, the cost-effectiveness of treating mild severe sleep apnoea with continuous positive airway pressure (CPAP) is still unclear. Two important randomised studies on the treatment of patients with severe sleep apnoea have been reported. The MERGE trial in the UK, which included 233 participants with mild untreated severe sleep apnoea (defined as having scores of 5–14 on the Apnoea–Hypopnoea Index [AHI]), showed that CPAP significantly improved quality of life (as measured by the Short Form Health Survey).5 Although this study is methodologically robust, it does not provide final answers, and its follow-up time was short (only 3 months). Although 81% of the treated participants were willing to continue CPAP after completion of the trial, the improved quality of life might have been due to other factors. Effects of body-mass index, physical exercise, and sleepiness on quality of life were not analysed. All patients with untreated severe sleep apnoea should lose weight if they are obese, avoid excessive stress, and have a healthy lifestyle. CPAP can therefore not be routinely recommended for all cases of mild untreated severe sleep apnoea. In addition to their subjective quality of life, assessing daytime functioning in these patients is crucial.
© 2021 CC Studio/Science Photo Library
Another large randomised study was done in Spain. The ISAAC study recruited 2551 individuals.6 Of the 1264 patients without excessive daytime sleepiness (Epworth Sleepiness Scale score [ESS] ≤10) and moderate-to-severe untreated sleep apnoea (AHI scores ≥15), 633 were randomly assigned to receive CPAP and 631 to receive usual care. The median follow-up time was 3·35 years. No significant differences in the occurrence of cardiovascular events were found. 98 (16%) of the events were observed in the CPAP group and 108 (17%) in the usual care group. The hazard ratio was 0·89 (95% CI 0·68–1·17; p=0·40).6 Unfortunately, the investigators did not stratify patients with untreated severe sleep apnoea according to moderate (AHI scores 15–19) or severe (AHI scores ≥30) disease. Furthermore, they did not include patients with mild (ESS 11–14), moderate (ESS 15–17), or severe (ESS ≥18) daytime sleepiness and untreated severe sleep apnoea. Therefore, the results cannot be generalised to all patients with obstructive sleep apnoea, and certainly not to patients with moderate or severe (ESS >14) daytime sleepiness. The results indicate that CPAP might not be necessary in patients without excessive daytime sleepiness (ESS ≤10) and AHI scores of 15 or lower. The findings from the ISAAC and MERGE trials thus point to different directions. What is more important: preventing cardiovascular morbidity for a 3-year period or improving quality of life for a 3-month period? This question remains open. Meta-analyses and studies addressing potential confounders are needed.
Further important findings in sleep medicine came from Hablitz and colleagues,7 who showed that CSF distribution is under circadian control. Researchers in Copenhagen (Denmark) and Rochester (New York, USA) have proposed that interstitial ion signalling is crucial in controlling sleep and wakefulness.8 These investigators have also proposed that ion homoeostasis failure might contribute to neurological diseases and cognitive-behavioural disorders.8 New studies done by Erlend Nagelhus and colleagues also show that Ca2+ signalling is essential in the regulation of slow wave sleep.9 All of these new studies support that astrocytes are key elements in the regulation of brain function. Emerging evidence indicates that disturbed sleep might be among the strongest risk factors for development of neurodegenerative diseases. Therefore, all physicians should incorporate questions about sleep hygiene and quality into their routine clinical practice.
Acknowledgments
I declare personal fees and other from Bioprojet, other from Jazz Pharmaceuticals, personal fees from UCB-Pharma, personal fees from GlaxoSmithKline, personal fees from Takeda, personal fees and other from MSD, personal fees from Orion, and personal fees and other from Umecrine, outside the submitted work.
References
- 1.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altena E, Baglioni C, Espie CA. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 3.Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Partinen M, Bjorvatn B, Holzinger B. Sleep and circadian problems during the coronavirus disease 2019 (COVID-19) pandemic: the International COVID-19 Sleep Study (ICOSS) J Sleep Res. 2020 doi: 10.1111/jsr.13206. published online Nov 12. [DOI] [PubMed] [Google Scholar]
- 5.Wimms AJ, Kelly JL, Turnbull CD. Continuous positive airway pressure versus standard care for the treatment of people with mild obstructive sleep apnoea (MERGE): a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8:349–358. doi: 10.1016/S2213-2600(19)30402-3. [DOI] [PubMed] [Google Scholar]
- 6.Sánchez-de-la-Torre M, Sánchez-de-la-Torre A, Bertran S. Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (ISAACC study): a randomised controlled trial. Lancet Respir Med. 2020;8:359–367. doi: 10.1016/S2213-2600(19)30271-1. [DOI] [PubMed] [Google Scholar]
- 7.Hablitz LM, Plá V, Giannetto M. Circadian control of brain glymphatic and lymphatic fluid flow. Nat Commun. 2020;11 doi: 10.1038/s41467-020-18115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rasmussen R, O'Donnell J, Ding F, Nedergaard M. Interstitial ions: a key regulator of state-dependent neural activity? Prog Neurobiol. 2020;193 doi: 10.1016/j.pneurobio.2020.101802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bojarskaite L, Bjørnstad DM, Pettersen KH. Astrocytic Ca2+ signaling is reduced during sleep and is involved in the regulation of slow wave sleep. Nat Commun. 2020;11 doi: 10.1038/s41467-020-17062-2. [DOI] [PMC free article] [PubMed] [Google Scholar]