Abstract
Coronavirus disease 2019 (COVID-19) is an emerging disease caused by the coronavirus, SARS-CoV-2, which leads to severe respiratory infections in humans. COVID-19 was first reported in December 2019 in Wuhan city, a populated area of the Hubei province in China. As of now, Wuhan and other cities nearby have become safe places for locals. The rapid control of the spread of COVID-19 infection was made possible due to several interventions and measures that were undertaken in Wuhan. This narrative review study was designed to evaluate the emerging literature on the combined measures taken to control the COVID-19 pandemic in Wuhan city. Science Direct, Springer, Web of Science, and the PubMed data repositories were searched for studies published between December 1, 2019, and June 07, 2020. The referred ”preferred reporting items for systematic reviews and meta-analyses” (PRISMA) protocol was used to conduct this narrative review. A total of 330 research studies were found as a result of the initial search based on exclusion and inclusion criteria, and 30 articles were chosen on final evaluation. It was discovered that the combined measures to control the spread of COVID-19 in Wuhan included cordon sanitaire, social distancing, universal symptom surveys, quarantine strategies, and transport restrictions. Based on the recommendations presented in this review study, existing policies with regard to combined measures and public health policies can be enforced by other countries to implement a rapid control procedure to control the spread of the COVID-19 pandemic.
Keywords: COVID-19, Combined measures, Lockdown, Public health, Review, Implications
1. Introduction
The outbreak of coronavirus disease 2019 (COVID-19) infection started in Wuhan in China in December 2019. Due to the severity of the COVID-19 infection, it was declared a class B infectious disease. However, prevention and control standards for class A diseases have been used to prevent the spread of the COVID-19 infection.1 Several studies have presented observations on the health safety of frontline medical staff and others who reported cases of COVID-19 infection in China. Health workers are valuable assets and the aim of standard precautions is to cut off the transmission routes of the virus among workers and other people.31 Standard precautions include hand and respiration hygiene, injection safety measures, environmental cleaning, proper linens, and sterilization of safety and patient equipment.
Countless challenges have been faced by the emerging economies of the world with regard to the purchase of diagnostic kits and equipment, and the training of the medical staff on biosafety and biosecurity. To prevent or curtail the COVID-19 infection, many countries have adopted prevention strategies. China is one of these countries, where several measures have been undertaken to control the COVID-19 pandemic.2, 3 This paper presents an overview of the emerging literature on the COVID-19 pandemic, with regard to the combined measures taken to control the COVID-19 pandemic in Wuhan, Hubei, China. This narrative review also presents some research implications regarding public health for other countries and regions.
A lockdown strategy, or a combination of social distancing, home quarantine, and case isolation for individuals, have been observed in several parts of the world. Some interventions that were mentioned earlier, or public health strategies, are projected to combat the COVID-19 pandemic. Middle- and low-income countries do not have sufficient resources and face financial and economic challenges, which may hinder their ability to effectively implement the COVID-19 infection treatment policies.4 It is hoped that lockdown and other intervention strategies may help reduce morbidity and delay the need for healthcare resources.
Xue et al.5 and Hellewell et al.6 highlighted the stochastic transmission model and found that increased case isolation and contact tracing are important measures to control the new outbreak of the COVID-19 pandemic. Xiao et al.7 stated that nearly 11 million people were placed in lockdown in Wuhan city. Moreover, entry and exit restrictions were imposed in the region8 and the lockdown was extended to other cities in the Hubei province as well.8 A study model presented by Xue et al.5 confirmed that lockdown and other healthcare capacity measures are effective in controlling the spread of COVID-19 positive cases. Similarly, a study of the COVID-19 infection and infected cases in Toronto and Italy showed that measures, such as personal protection and reducing the node edges of the infected people, have had better results in controlling the pandemic. In addition to these measures, the quarantining of close contacts is also an effective tool for reducing the peak epidemic and final epidemic size.
Several review studies have already been carried out on the COVID-19 pandemic effects on the public, medical, and workers’ health. Wang et al.34 emphasized the psychological toll of the COVID-19 pandemic. This study reported that community health services, online services, telemedicine, and other services played a vital role during the epidemic in Wuhan. Ibrahim35 identified that hospital and laboratory-based surveillance are important COVID-19 surveillance types. Useful and accurate data of surveillance types have been regarded as necessary for COVID-19 interventions. However, none of the reviews focused on investigating strategic and combined measures to combat the COVID-19 pandemic.
The primary question, as answered in this review article is, “What measures were taken to control COVID-19 in Wuhan, Hubei, China?”
We provide the literature evidence on the combined measures taken to control the transmission of COVID-19 in Wuhan. We sought to answer this question by performing a literature search, exploring how enhanced protective measures and social distancing measures were crucial to stopping the pandemic and how many lives were saved.32
2. Methods
The current narrative review was performed following the “preferred reporting items for systematic review and meta-analysis” (PRISMA) guidelines, also used in other studies.9 PRISMA consists of 27 items aimed to facilitate the preparation and reporting of a protocol for a systematic review. PRISMA guidelines are usually considered by funders and for commissioned reviews.10 We considered most of the guidelines (checklist items) to conduct a rapid review of studies that assessed the advantages of combined measures to control the COVID-19 pandemic in Wuhan. The checklist of the PRISMA protocol has been clearly documented in previous review studies.11 From this checklist, we adopted item 8 (search), item 9 (study selection), item 20 (result of individual studies), item 24 (summary of evidence), item 26 (conclusions), and item 27 (funding) from the listed items.
2.1. Search process
The search process was used to find relevant studies from target data repositories. For this, we applied the relevant search terms to Science Direct, Springer, Web of Science, and PubMed data repositories. The search terms were as follows:
-
•
“Combined measures” OR “lockdown in Wuhan”
-
•
“Coronavirus 2019” OR “COVID-19”
-
•
“Public health” AND “Controlling COVID-19 in Wuhan”
2.2. Study inclusion and exclusion criteria
2.2.1. Inclusion criteria
-
•
Studies that discussed COVID-19 along with combined measures for public health were included.
-
•
Studies written in the English language were included.
2.2.2. Exclusion criteria
-
•
Studies with only an abstract were excluded.
-
•
Studies that involved discussions on topics other than COVID-19 discussions on public health were excluded.
-
•
Studies that involved discussions on COVID-19 controlling measures in places other than Wuhan city were excluded.
-
•
Duplicate studies were excluded.
2.3. Quality assessment
The quality of each study was evaluated by the colleagues (IG and MFP) of this paper. Due to the limited number of emerging studies and also a short time, only research papers, including review articles, opinion papers, and short communication papers, were included in this study.
2.4. Statistical analysis
It was impossible to perform a meta-analysis because an appropriate and sufficient number of papers could not be found.
2.5. Data extraction
The data extraction strategy is shown in Fig. 1 .
Fig. 1.
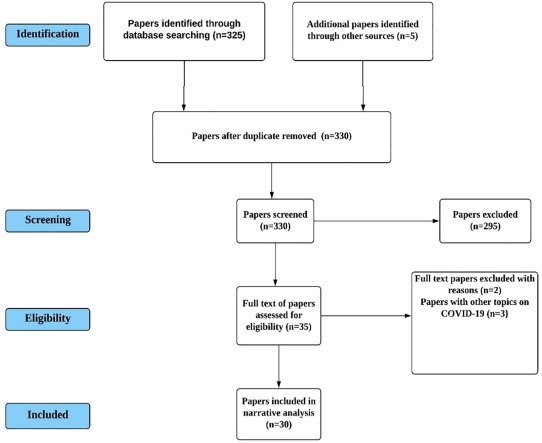
PRISMA process flow.
3. Results
As of 7th June 2020, 330 articles were identified. The exclusion and inclusion criteria for the identified studies were used following the PRISMA guidelines (Fig. 1). Of these 330 studies, 35 were included for full-text review, following a review and exclusion of titles, abstracts, and duplicate studies. Furthermore, five other studies were excluded because they were either not focused on COVID-19 topics with combined measures, or the full text was not available. In the end, as a result of the reviews, 30 studies met the inclusion criteria and were thus included in this narrative review (Fig. 1).
Table 1 illustrates the summaries of the chosen studies, which are close to our research topic. Among the 30 articles, we identified 27 papers that were focused on the COVID-19 pandemic, as shown in Table 1. Among these articles, 17 studies were conducted on data taken from Wuhan. A study6 compared isolation and contact tracing measures adopted during the COVID-19 pandemic in Wuhan, Toronto, and Italy. These measures are regarded as essential measures to control the outbreak of a new epidemic within three months. Studies7, 16, 34, 40 presented the psychological impacts of the COVID-19 pandemic during this pandemic. Mental illness, anxiety, depression, fear, and agony were severe, and affected medical workers, patients, and the public. Social distancing,8 corticosteroid treatment,9 and technology-and human-driven22 approaches have been discussed in the literature. A study24 revealed that quarantine alone is not the right approach to control the COVID-19 pandemic around the globe. We include studies36, 37, 38, 39 that highlight the COVID-19 pandemic effects on air quality. Several compounds that reflect air quality have been investigated in these studies. The levels of NO, SO2, O3, and CO2 are reported with the exposure and effects of benzene during the lockdown period in Italy. Nine pollutants have been assessed in these studies. In addition to these studies, many other studies have used comparable data concerning the COVID-19 pandemic from countries such as Saudi Arabia,2 Chile,4 Canada,5, 40 Italy,5, 36, 37 Malaysia,23 Spain, and Portugal.28 Additionally, studies10, 11 have been assessed the appropriate use of PRISMA guidelines, as discussed in the Methods section.
Table 1.
Summaries of the chosen studies.
| No | Summary of paper | Country | Province (City) | Reference |
|---|---|---|---|---|
| Medical management strategies | China | Heilongjiang | 1 | |
| Prevention and therapeutic strategies | Saudi Arabia | --- | 2 | |
| Control strategies to reduce social mixing | China | Wuhan- Hubei | 3 | |
| Healthcare demand estimation | Chile | --- | 4 | |
| A data driven network model to measure the emerging COVID-19 pandemic |
|
Wuhan- Hubei | 5 | |
| Wuhan, Toronto, and Italy use of isolation measures | China | Wuhan- Hubei | 6 | |
| Psychological impact in medical workers | China | Wuhan- Hubei | 7 | |
| Challenges of GIS and Big Data due to COVID-19 pandemic | China | Wuhan- Hubei | 12 | |
| Emergency surgery patients infected with COVID-19 | China | Wuhan- Hubei | 13 | |
| Recommendations for otolaryngology and head and neck surgery practices based on COVID-19 pandemic | China | Wuhan- Hubei | 14 | |
| Diffusion of COVID-19 infection and its controlling measures | China | Wuhan- Hubei | 15 | |
| Public health interventions during COVID-19 pandemic | China | Wuhan- Hubei | 17 | |
| Data on COVID-19 pandemic in Wuhan | China | Wuhan- Hubei | 18 | |
| Protection procedures in Hubei Cancer center | China | Wuhan- Hubei | 19 | |
| Modeling the trajectory of COVID-19 pandemic in Wuhan | China | Wuhan- Hubei | 20 | |
| Implementing the universal symptom survey in Wuhan | China | Wuhan- Hubei | 21 | |
| COVID-19 infection transmission in urban settings | China | Wuhan- Hubei | 23 | |
| COVID-19 outbreak in Malaysia and its control actions | Malaysia | --- | 25 | |
| Cordons sanitaire measures in Wuhan | China | Wuhan- Hubei | 27 | |
| Lesson from the crisis for small countries |
|
--- | 28 | |
| Biosafety and biosecurity challenges for USA and China |
|
--- | 29 | |
| Research on COVID-19 regarding engineering | China | --- | 30 | |
| Lockdown effects on air quality | Italy | Milan | 36 | |
| Chronic air pollution levels and their role in the Covid-19 pandemic outbreak risk | Italy | Northern Areas | 37 | |
| Socio-economic and environmental impacts of COVID-19 pandemic | China | Wuhan- Hubei | 38 | |
| Lockdown and its impacts on air pollution and health during lockdown in Wuhan | China | Wuhan- Hubei | 39 | |
| COVID-19 pandemic outbreak and its stress and mental illness effects | UK, USA, and Canada | --- | 40 |
4. Discussion
4.1. Epidemic model to control COVID-19 infection
The paper ‘COVID-19: challenges to GIS with Big Data’ is by Zhao and Chen, and it proposes an epidemic model to overcome the widespread infection in Hubei, China.12 The proposed model, 'Susceptible, Un-quarantined infected, quarantined infected, confirmed infected' (SUQC), best fits to predict the end of COVID-19 in the province, as mentioned earlier. In addition, the model can be successfully applied to track and predict the COVID-19 situation in various regions of China. This model is attractive due to its possible applications in multiple areas of other countries. This study suggests following the proposed model based on the predicted information concerning quarantine and prevention measures, which are necessary for all countries. Geographic Information Systems (GIS) technology is presented here with a greater potential for virus-free transportation and supply of materials during the COVID-19 epidemic. Themes discussed in the study are fascinating because of their broad level applications for public health safety during a time of crisis. However, this study has certain limitations regarding the prediction of the high death rates occurring in the USA and European countries. Why has the COVID-19 situation in the USA and European countries not been predicted by using the proposed prediction model? One possibility for this might be the fact that the focus of researchers in this study was on the collected data on COVID-19 infection in the Hubei province of China. Another limitation is that social barriers, which prevent data collection from commercial enterprises, still require the attention of researchers in future works. For instance, cultural, consent, and health safety concerns are the informed consent challenges for clinical trials.33 Therefore, these challenges need to be addressed in future studies.
Li et al.13 performed a retrospective cohort study on 164 patients who underwent emergency surgery (ESP) with or without COVID-19 pneumonia. The data were collected from Zhongnan Hospital of Wuhan University. The results of this study show that 54 ESPs were infected with COVID-19 in the hospital. Among the people infected with COVID-19, 43 were healthcare workers who were in direct contact with the ESP in the hospital. However, more importantly, the number of healthcare workers infected with COVID-19 decreased after January 2020. Healthcare workers used stringent control procedures to control intra-hospital transmission. Therefore, a significant decrease in COVID-19 transmission was reported in the operating rooms of the hospital.
However, inadequate protection of normal people is a major public health issue for clinicians and health workers while they test or treat people. Kowalski et al.14 in a study on the topic “COVID‐19 pandemic: Effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice” emphasized the effective biosafety measures in clinics and hospitals. Most people who visit clinics and hospitals are not symptomatic, as they require only their checkups for COVID-19 infection. Moreover, every subsequent patient without COVID-19 infection in the same suite or room may be at elevated risk of contamination, as are physicians and nurses. For this purpose, the USA Centers for Disease Control and Prevention (CDC) has given its recommendations to cease elective care and provide only urgent and emergency services.
4.2. Dentist services
In Wuhan, dental staff in the emergency ward treated more than 700 patients and also provided online consultations to more than 1,600 patients. Despite these measures, public health risks still exist, which threaten the safety of humans and the ecological environment. However, the ‘biological weapon convention’ is effective since 1975, and it enforces the implementation of international laws and regulations to ensure the safety and security of people at large.15 In the aforementioned study, the authors stated that COVID-19 was mainly aimed at accelerating the preparation of vaccines and protecting public health. Contrary to these benefits, COVID-19 is a harmful infection, as it can be easily transmitted with a high susceptibility and biosecurity risk. Moreover, bioterrorists can exploit it to harm the health of the target population.
4.3. Combined measures to control the COVID-19 pandemic
This section discusses the combined measures taken against the COVID-19 pandemic in the Wuhan city of China.
4.3.1. Cordons sanitaire
A survey study was conducted on adults (>18 years) from Wuhan city. The sample was taken from community-based adults and health professionals. The survey was undertaken during the first month of the cordon sanitaire.16 This study concluded that social support was a significant tool, with less anxiety and depression among the participants. Since social distancing avoids the mixing of people and, consequently, leads to adverse emotional effects, social support becomes a key emotional support mechanism for people. Ali Health, WeChat, and Ping An Good Doctor are known as significant social media tools used to search for COVID-19 news. To further explain the impacts of cordon sanitaire on the public health of people from Wuhan city, Pan et al.17 performed a cohort study to examine public health interventions during the COVID-19 pandemic. The time period between January 23, 2020 and February 1, 2020 was declared as the Cordon Sanitaire period. The findings of the above-mentioned study indicated that the cordon sanitaire intervention was temporarily associated with the reduced effective reproduction of COVID-19. Overall, this intervention proved to be a remarkable tool in blocking COVID-19 infection transmission routes.
A recent study revealed that the peak of the COVID-19 positive cases started to gradually fall since 2 February, 2020. This is because the travel ban, which was enforced two weeks earlier, remained efficient in combating the spread of the infection. However, the time lag between the onset of symptoms and diagnosis was 20 days.18
4.3.2. Social distancing
The social distancing measure was enforced in the radiation oncology department at the Hubei Cancer Hospital. A policy to allow a single patient in the LINAC waiting area was enforced. This treatment pattern was different from the other regular means prior to the outbreak of the COVID-19 pandemic. Additionally, in the general waiting area, patients were instructed to keep at least 2 meters of distance between each other.19 Schools and workplaces were closed to minimize the social mixing of people of different ages. The social distancing patterns were drastically focused on the epidemic setting in Wuhan city. Enforcing the social distancing rule in crowded cities is challenging for governments. This problem can be addressed by quantifying the social contact patterns at workplaces and homes based on the available information from local populations and their demographic structures, and household-level data across countries.3
Liu et al.20 shared the experience of controlling the COVID-19 pandemic in China, particularly in Wuhan. The impact of intervention strategies was measured by the data collected from the National Health Commission of China (NHCC). A model had been used that considered several factors, including the spring festival (chunyun), construction of Fangcang Hospital, and sealing of Wuhan. This study also concluded that the combined measures mentioned earlier were the primary intervention strategies used to control the spread of the COVID-19 infection. In contrast to Wuhan, England has been identified as an epicenter where an incorrect response was observed during the initial phases of the pandemic.
4.3.3. Universal symptom surveys
Another major measure, the universal symptom survey, was enforced between 6–10 and 17–19 February 2020 in Wuhan. This measure was accompanied by the isolation of cases, which altered the virus transmission. This evidence was stated by Wei et al.21 who found that after 14 February 2020, the virus transmission differed from previous results due to the implementation of universal symptom surveys. Pan et al.17 also stated that universal symptom surveys conducted between February 16 and 18, 2020 were effective in reducing the spread of COVID-19 infection in Wuhan. Both of the above-mentioned studies showed that the universal symptom surveys strategy was associated with the reduced reproduction number of COVID-19 and may inform public health policies across the world.
4.3.4. Quarantine strategy
A draconian approach, with the recommendations of the WHO, to place cities under a complete quarantine, was successfully implemented in various cities of China. China used its well-established surveillance systems. This indicates that across the country, with the help of combined measures and technology, China controlled the spread of the virus.22 Most of the strategies to control the virus were based on the identification of infected people in China. Major cities in China have effective surveillance systems. Security cameras and CCTV help detect the activities of people to ensure that quarantined people stay in their homes. CCTV cameras operate with the help of artificial intelligence technology (AI) and facial recognition for the identification of people.
4.3.5. Transport restriction
Wuhan is a major transportation hub in China and is connected to different areas in the country. A number of difficulties have been reported in controlling the COVID-19 outbreak.13 Tremendous and large movement of people made it difficult to control the spread of the infection in Wuhan city, China. Various measures were taken to contain the infection and control the spread of COVID-19 in other areas, which surround the city.23 In a recently published study, Sohrabi et al.24 stated that all public transportation such as metro, long route buses, express railways, and aviation, were sealed off. The process of sealing off all these services was facilitated by Wuhan’s infrastructure. An unprecedented lock down was observed amid the Chinese new year holiday period. These measures helped to control the spread of the COVID-19 infection in Wuhan city, China. In response to the measures taken by the Chinese government, a number of countries have followed similar control measures. For example, the Malaysian government enforced the movement control order (MCO) on March 18, 2020 and it remained effective in controlling public health. They also enforced interstate travel restrictions.25
Overall, the application of these interventions is valuable for global efforts to prevent or reduce the COVID-19 impact because these interventions can underscore the earlier interventions for public health.26 The enforcement of unprecedented efforts, including surveillance, isolation of COVID-19 patients, quarantine of close contacts, and community quarantine in Wuhan and other parts of China, helped in delaying the epidemic peak. Another model revealed that the larger travel restrictions (>90%) resulted in transmission delays, and daily cases in Wuhan did not exceed 1 in every 1000.27 These details highlight the importance of the synergistic efforts of public health measures. Therefore, other countries should learn and follow these measures to control the COVID-19 pandemic. The decline as well as the end of the cordon sanitaire in Wuhan also shows that public health strategies have worked. The authors, therefore, urge other nations to follow the preventive measures in the same way as China has done, as they can help in combating the COVID-19 pandemic.
4.4. Complications of COVID-19 pandemic and combined measures
Instead of the major benefits of combined measures, emerging literature sheds light on the adverse impacts of the COVID-19 pandemic on air quality. Ultimately, it creates more complications for the health systems of countries. In this regard, Collivignarelli et al.36 reported the COVID-19 pandemic impact on the health system in northern areas of Italy. Both partial and total lockdowns have been assessed regarding their air quality impacts in Milan. Pollution concentration decreased due to both types of lockdowns. Sulfur dioxide (SO2), which is an important air pollutant, dropped to an appreciable level, but remained unchanged in the adjacent areas. Conversely, the concentration of O3 increased in Milan, which is likely due to the higher consumption of benzene than that in the adjacent areas. A study37 established a correlation between the periodic emergence of COVID-19 with socioeconomic and environmental factors. The aforementioned study suggests that the air quality must be evaluated for the long term to prevent epidemic spread because the adoption of mitigation measures could be of limited utility. Contrary to the findings in,36 Bashir et al.38 stated that restricted economic activities resulted in a cleaner environment. The researchers forecasted that environmental changes are not permanent and showed their concerns regarding the rise in environmental pollution in the future.
Cole et al.39 presented a contradictory findings compared to those presented in.36 The former study showed that the lockdown strategy showed a decrease in SO2 amount, while the latter study shows that lockdowns do not have discernible impacts on the SO2 concentration. Thus, there is a need to carry out replicated studies to confirm the contradicting findings from the two earlier studies. We should investigate the contributing factors that cause fluctuations in the different constituents of air pollution.
Moreover, healthcare regulators' lockdowns and emergencies during the COVID-19 pandemic resulted in anxiety, depression, and related mental issues among health professionals, healthcare staff, and the public population. A recent study40 presented a solution to overcome the previously mentioned complications produced by the COVID-19 pandemic and its controlling measures. People should acknowledge that anxiety does not last for a long time, and social distance is like physical distancing. People can use authenticated resources to meet their family members, friends, and others through social media. Thus, psychological stress can be reduced by following the instructions on different websites.
This study identifies a few open challenges to public health that might be investigated in the future. For instance, we found varied insights from the emerging literature on air quality during and after the COVID-19 pandemic. Therefore, future research can be undertaken to investigate and verify the varying insights regarding combined measures’ impacts on the environment and people living in different regions of the world.
5. Conclusion and implications
This section concludes the research study and presents some updates on the public health and combined measures implications in the current COVID-19 pandemic situation.
Most of the reviewed studies presented the observations and novel approaches for controlling the COVID-19 infection and intervention measures undertaken in Wuhan, Hubei, China. The findings of this short review suggested that combined measures are the primary reasons behind controlling the spread of the COVID-19 infection in Wuhan. Therefore, lockdown along with the combined measures may have to be an international priority.
-
1.
High surveillance and proper biosafety and biosecurity procedures need to be used in public and private institutes conducting virus research. To avoid the accidental leakage of a virus that can damage the surrounding population, including human beings, animals, and vegetation, policymakers must revise the biosafety and biosecurity regulations. This is of vital importance to prevent a future pandemic, which can also create huge socioeconomic issues.28
-
2.
Collaboration between internal and external health stakeholders can be enhanced by providing them with more resources to sustain high-quality research according to public health standards on the COVID-19 pandemic. This will pave the way for underdeveloped countries to develop competitive advantages with regard to their human and natural resources.29
-
3.
Both China and the USA agreed to enhance collaboration in the area of synthetic biology during a workshop held on 16 July 2019, on “Biosafety and Biosecurity in the Era of Synthetic Biology”.30 The main purpose of the workshop was to enhance the responsibility of the two countries in promoting biosafety and biosecurity in biological research and its applications. The current COVID-19 pandemic situation is appealing to frontline countries, which are promoting the research on biosafety and biosecurity with regard to public health. Countries, including China and the USA, must take measures to avoid any future fatal human losses from a similar type of pandemic.
-
4.
Diagnostic methods (COVID-19 tests) used for the COVID-19 infection must be performed according to quality standards as well as a regulatory framework.
In addition to these implications, this review provided reference and support for other nations to incorporate the combined measures comprehensively to save human lives in the COVID-19 pandemic. There are still some restrictions on the combined measures, which can be improved in the future.
Authors’ contributions
This narrative review was presented by the collective effort of the above-listed authors. MH prepared the initial draft of the article; MFP and IG proofread it and fixed typos and grammatical errors, and also formatted the paper according to the style of the journal.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Wang H., Wang S., Yu K. COVID-19 infection epidemic: the medical management strategies in Heilongjiang Province, China. Crit Care. 2020:2–4. doi: 10.1186/s13054-020-2832-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Tawfiq J.A., Memish Z.A. COVID-19 in the Eastern Mediterranean Region and Saudi Arabia: prevention and therapeutic strategies. Int J Antimicrob Agents. 2020;105968 doi: 10.1016/j.ijantimicag.2020.105968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prem K., Liu Y., Russell T.W. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rainisch G., Undurraga E.A., Chowell G. A dynamic modeling tool for estimating healthcare demand from the COVID19 epidemic and evaluating population-wide interventions. Int J Infect Diseases. 2020 doi: 10.1016/j.ijid.2020.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xue L., Jing S., Miller J.C., Sun W., Li H., Estrada-Franco J.G., Zhu H. A data-driven network model for the emerging COVID-19 epidemics in Wuhan, Toronto and Italy. Math Biosci. 2020:108391. doi: 10.1016/j.mbs.2020.108391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hellewell J., Abbott S., Gimma A. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Global Health. 2020 doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. 2020 doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singhal T. A review of coronavirus disease-2019 (COVID-19) Ind J Pediatr. 2020:1–6. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tobaiqy M., Qashqary M., Al-Dahery S., Mujallad A., Hershan A.A., Kamal M.A., Helmi N. Therapeutic Management of COVID-19 Patients: a systematic review. Infect Prev Pract. 2020:100061. doi: 10.1016/j.infpip.2020.100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1136/bmj.b2700. [DOI] [PubMed] [Google Scholar]
- 12.Zhou C., Su F., Pei T. COVID-19: challenges to GIS with big data. Geogr Sustain. 2020 doi: 10.1016/j.geosus.2020.03.005. [DOI] [Google Scholar]
- 13.Li J., Gao R., Wu G. Clinical characteristics of emergency surgery patients-infected COVID-19 pneumonia in Wuhan, China. Surgery. 2020 doi: 10.1016/j.surg.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kowalski L.P., Sanabria A., Ridge J.A. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020 doi: 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci Total Environ. 2018 doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ni M.Y., Yang L., Leung C.M. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Mental Health. 2020;7(5):e19009. doi: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pan A., Liu L., Wang C. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. Jama. 2020 doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walach H., Hockertz S. Wuhan Covid19 data–more questions than answers. Toxicology. 2020 doi: 10.1016/j.tox.2020.152486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei W., Zheng D., Lei Y. (COVID-19) outbreak: experience of the Hubei Cancer Hospital in Wuhan, China. Radiother Oncol. 2019;2020 doi: 10.1016/j.radonc.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu M., Ning J., Du Y. Modelling the evolution trajectory of COVID-19 in Wuhan, China: experience and suggestions. Public Health. 2020 doi: 10.1016/j.puhe.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wei Y., Wei L., Jiang Y. Implementation of clinical diagnostic criteria and universal symptom survey contributed to lower magnitude and faster resolution of the COVID-19 epidemic in Wuhan. Engineering. 2020 doi: 10.1016/j.eng.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kummitha R.K.R. Smart technologies for fighting pandemics: the techno-and human-driven approaches in controlling the virus transmission. Government Inform Quarter. 2020 doi: 10.1016/j.giq.2020.101481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu L. Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: evidence from China. Cities. 2020 doi: 10.1016/j.cities.2020.102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Agha R. World Health Organization declares global emergency: a review of the novel coronavirus (COVID-19) Int J Surg. 2019;2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah A.U.M., Safri S.N.A., Thevadas R. COVID-19 outbreak in Malaysia: actions taken by the Malaysian Government. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.AlJaroudi W.A., Hage F.G. Cardiovascular disease in the literature: a selection of recent original research papers. J Nucl Cardiol. 2020;27(1):7–10. doi: 10.1007/s12350-016-0747-1. [DOI] [PubMed] [Google Scholar]
- 27.Wan K.H., Huang S.S., Ko C.N., Lam D.S. The end of cordon sanitaire in Wuhan: the role of non-pharmaceutical interventions. Public Health. 2020 doi: 10.1016/j.puhe.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chrousos G.P., Mentis A.F.A., Dardiotis E. Biomedical research: lessons from the last decade’s crisis and austerity-stricken small countries for the current COVID-19-related crisis. Nat Med. 2020:1–3. doi: 10.1038/s41591-020-0859-7. [DOI] [PubMed] [Google Scholar]
- 29.Inglesby T., Cicero A., Rivers C., Zhang W. Biosafety and biosecurity in the era of synthetic biology: meeting the challenges in China and the US. J Biosafety Biosecurity. 2019;1(2):73–74. doi: 10.1016/j.jobb.2019.09.003. [DOI] [Google Scholar]
- 30.S. Ma, P. Gao, D. Lu, G. Wang, Prudently conduct the engineering and synthesis of the SARS-CoV-2 virus. Synth Syst Biotechnol. https://doi.org/10.1016/j.synbio.2020.03.002. [DOI] [PMC free article] [PubMed]
- 31.Tang L.H., Tang S., Chen X.L. Avoiding health worker infection and containing the coronavirus disease 2019 pandemic: perspectives from the frontline in Wuhan. Int J Surg. 2019;2020 doi: 10.1016/j.ijsu.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang Q., Yi C., Vajdi A. Short-term forecasts and long-term mitigation evaluations for the COVID-19 epidemic in Hubei Province, China. Infect Dis Model. 2020;5:563e574. doi: 10.1016/j.idm.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ibrahim H., Kamour A.M., Harhara T., Gaba W.H., Nair S.C. Covid-19 pandemic research opportunity: is the Middle East & North Africa (MENA) missing out? Contemporary Clin Trials. 2020:106106. doi: 10.1016/j.cct.2020.106106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang S., Wen X., Liu B., Dong Y., hu Cui M. Psychological influence of Coronavirus disease 2019 (COVID-19) pandemic on the general public, medical workers and patients with mental disorders and its countermeasures. Psychosomatics. 2019;2020 doi: 10.1016/j.psym.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ibrahim N.K. Epidemiologic surveillance for controlling Covid-19 pandemic: challenges and implications. J Infect Public Health. 2020;2020 doi: 10.1016/j.jiph.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collivignarelli M.C., Abbà A., Bertanza G., Pedrazzani R., Ricciardi P., Miino M.C. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci Total Environ. 2020;732:139280. doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ Pollut. 2020 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bashir M.F., Benjiang M.A., Shahzad L. A brief review of socio-economic and environmental impact of Covid-19. Air Qual Atmosphere Health. 2020:1–7. doi: 10.1007/s11869-020-00894-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cole M.A., Elliott R.J., Liu B. The impact of the Wuhan Covid-19 lockdown on air pollution and health: a machine learning and augmented synthetic control approach. Environ Resour Econ. 2020:1–28. doi: 10.1007/s10640-020-00483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fofana N.K., Latif F., Sarfraz S., Bashir M.F., Komal B. Fear and agony of the pandemic leading to stress and mental illness: an emerging crisis in the novel coronavirus (COVID-19) outbreak. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113230. [DOI] [PMC free article] [PubMed] [Google Scholar]


