Abstract
Background
The Coronavirus disease 2019 pandemic caused the Japanese government to declare a State of Emergency on April 7, 2020. The aim of this study is to provide an overview of the effects of the pandemic on surgical cases at a university hospital trauma center.
Methods
An observational study was performed at a trauma center in a tertiary hospital in Tokyo, Japan. The number of surgeries was compared between two periods: a historical control period (Tuesday April 9 to Monday May 27, 2019) and the period of the Japan State of Emergency due to COVID-19 (Tuesday April 7–Monday May 25, 2020). Information on patient age, gender, and surgical diagnosis, site, and procedure was collected for cases operated on in each period. The number of trauma surgeries was compared between the two periods. Data from the two periods were compared statistically.
Results
The total number of surgical cases was 151 in the control period and 83 in the COVID-19 period (including no cases with COVID-19), a decrease of 45.0%. There were significantly more surgeries for patients with hip fractures in the COVID-19 period (9 vs. 19, P < 0.001 by Fisher exact test).
Conclusions
During the State of Emergency in Japan, the number of operations for trauma patients at the trauma center decreased, but surgeries for hip fracture increased.
1. Introduction
The outbreak of the new coronavirus disease 2019 (COVID-19), which started in Wuhan, Hubei Province, People's Republic of China, on December 12, 2019, resulted in 41 hospitalizations in Wuhan on January 2, 2020, and 2794 cases, including 80 deaths, by January 26 [1,2]. The pathogen of COVID-19 was initially named 2019-nCoV [3,4], and later renamed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses (ICTV) on February 11, 2020.
The COVID-19 epidemic quickly spread around the world, and the WHO declared a pandemic on March 11, 2020. The first case of COVID-19 in Japan was confirmed on January 15, 2020 in a Chinese man in his 30s with pneumonia who had been living in Wuhan. Subsequently, the number of positive SARS-CoV-2 cases increased rapidly in Tokyo after late March (Tokyo Metropolitan Government, COVID-19 information web site, https://stopcovid19.metro.tokyo.lg.jp/, cited Aug 5, 2020). The 7-day moving averages of the number of positive SARS-CoV-2 tests in the Tokyo metropolitan area were 1.0–4.1 in first half of March, but increased to 98.3 on April 7, 2020.
In response to the spread of the pandemic, the government declared a State of Emergency on April 6, 2020. The Japan State of Emergency is based on the law on countermeasures against the new coronavirus, which was enacted on March 13, 2020. The State of Emergency was declared by the Prime Minister and designated the period or area in which emergency measures were to be taken. Under this ruling, the prefectural governor of an affected area was able to request residents to refrain from going out of their homes and to cooperate in prevention of spread of the disease. In Tokyo, the State of Emergency was declared until May 25, 2020.
Our trauma center is attached to a university hospital and provides acute trauma care to an area with a population of approximately 1.9 million. The Tokyo Metropolitan Government requested the assistance of university hospitals to treat COVID-19 patients because this became impossible for designated infectious disease hospitals alone. As a result, our General Intensive Care Unit (GICU) beds were operated as dedicated COVID-19 patient beds and were managed by intensivists. Operating room use was restricted: elective operations were reduced by 20% from April 6, 2020, 50% from April 13, 2020 to May 10, 2020 and 30% from May 11, 2020 to May 16, 2020. Thus, the number of surgeries at our university hospital decreased significantly in April and May, 2020, with 533 and 421 surgeries, compared to 836 and 806 in the same months in 2019.
At our trauma center, we treat primary, secondary and tertiary emergency trauma cases, and we perform about one thousand trauma surgeries a year. Due to the declaration of the State of Emergency, it was no longer possible for the hospital to treat multiple tertiary emergency cases in the emergency room at the same time due to the requirement for prevention of nosocomial infection of COVID-19. Thus, the COVID-19 pandemic markedly changed the environment surrounding our trauma center by changing social activities and the healthcare system. The purpose of this study is to determine the impact of the pandemic on trauma surgery cases at our university hospital trauma center, and to help establish a medical system for future pandemics.
2. Materials and methods
An observational study was performed at a single trauma center at a university hospital in Tokyo. The number of surgeries was compared between two periods: a historical control period (Tuesday April 9 to Monday May 27, 2019) and the period of the Japan State of Emergency due to COVID-19 (COVID-19 period, Tuesday April 7 to Monday May 25, 2020). Information on patient age, gender, and surgical diagnosis, site, and procedure was collected for cases operated on in each period. The number of trauma surgeries (hip fracture, upper limb fracture, lower limb fracture, spinal cord injury, pelvic acetabular fracture, head and neck or thoracoabdominal trauma, and elective surgery for trauma such as fracture due to non-union) was compared between the two periods. Open fractures were studied in the same way. The location and mechanism of injury of hip fractures were compared between the two periods. The numbers of refusals of emergency calls for trauma cases and the numbers of hip fracture cases transferred from outside our medical area were examined in the two periods.
Data from the two periods were compared by t-test, Fisher exact test and Pearson chi-square analysis for significance, which was defined as p ≤ 0.05, using IBM SPSS ver.24.0 (IBM Corp., Armonk, NY, USA). This study was approved by the Institutional Review Board of our hospital. The authors have no conflict of interest to declare.
3. Results
The total number of surgical cases was 151 in the control period (101 males and 50 females) and 83 in the COVID-19 period (47 males and 36 females, including no cases with COVID-19), a decrease of 45.0%. There was no significant difference in the gender ratio between the two periods (Fisher exact test). The patients were significantly older in the COVID-19 period compared to the control period [mean age: 58.3 (SD 23.1) vs. 47.9 (SD 22.0) years, P < 0.001 by t-test, 95% confidence interval (CI) 4.41 to 16.46] (Table 1 ).
Table 1.
General characteristics of surgical cases in the periods of the study.
| Control (2019) | COVID-19 (2020) | |
|---|---|---|
| Total number of surgical cases | 151 | 83 |
| Gender (male), n (%) | 101 (67) | 47 (57) |
| Average age (years) | 47.9 | 58.3 |
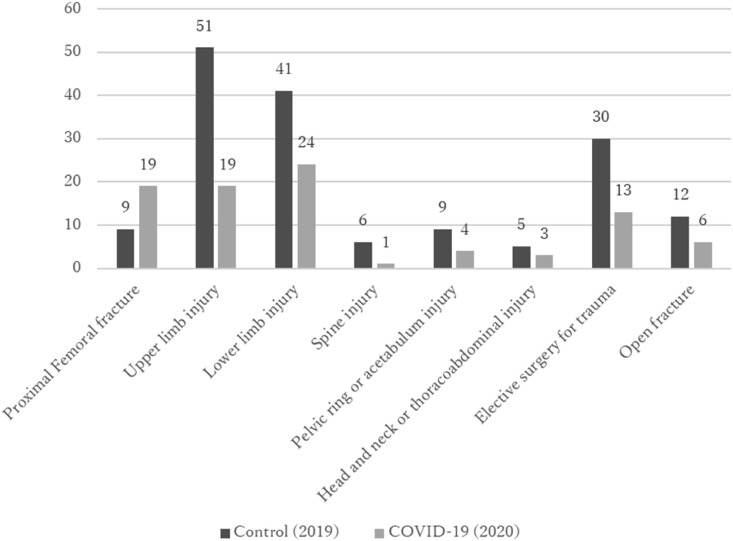
The numbers of surgeries in the two periods are shown in Fig. 1 . The number of cases of hip fractures almost doubled from 9 in the control period to 19 in the COVID-19 period. In a comparison of these surgeries with other surgeries in the two periods, there were significantly more hip fracture surgeries in the COVID-19 period (P < 0.001 by Fisher exact test, 95% CI 0.08 to 0.53). There were 6 surgeries for open fractures in the COVID-19 period compared to 12 in the control period, and the patients treated in these surgeries were significantly older in the COVID-19 period [mean age: 75.0 (SD 19.2) vs. 37.8 (SD 26.8) years, P < 0.05 by t-test, 95% CI -63.41 to −11.09]. The location of hip fracture in the control and COVID-19 periods was at home or in an institution in 5 (56%) and 16 (84%) cases, and the mechanism of injury was fall from a standing height in 6 (67%) and 18 (95%) cases, respectively (Table 2 ).
Fig. 1.
Distribution of injuries in cases that underwent surgery for trauma in the control (2019) and COVID-19 (2020) periods. Open fracture cases overlap with other injuries.
Table 2.
Number of hip fracture cases in the periods of the study.
| Control (2019) | COVID-19 (2020) | |
|---|---|---|
| Total number of hip fracture cases | 9 | 19 |
| Location (home or institute), n (%) | 5 (56) | 47 (84) |
| MOI (fall from standing height), n (%) | 6 (67) | 18 (95) |
MOI: mechanism of injury.
There were no refusals of emergency calls for tertiary trauma cases in the control period, but there were six such refusals in the COVID-19 period (Table 3 ). For secondary emergency cases, there were 30 refusals of emergency calls in the control period and 47 in the COVID-19 period (Table 3). None of the hip fracture cases were transported from outside our medical area in the control period, but there were three transfer cases in the COVID-19 period.
Table 3.
Number of refusals of tertiary/secondary emergency calls in the periods of the study.
| Control (2019) | COVID-19 (2020) | |
|---|---|---|
| Refusals of tertiary emergency | 0 | 6 |
| Refusals of secondary emergency | 47 | 30 |
4. Discussion
During the period of the Japan State of Emergency due to the COVID-19 pandemic, the number of surgeries at our trauma center decreased significantly compared to the equivalent time period in the previous year, while the number of hip fracture surgeries more than doubled. One reason for the decrease in the number of trauma surgeries may have been a change in the system at our center. We have three tertiary emergency rooms, one of which is a hybrid emergency room system (HERS) equipped with computed tomography (CT) and radiography equipment. In tertiary emergency cases, it is difficult to obtain a history and symptoms. Thus, to prevent loss of hospital function due to nosocomial infection, all tertiary emergency patients were screened for COVID-19 by chest CT scan in the HERS. No trauma patients with COVID-19 were identified during this period.
As a result of this change, only one line was used for tertiary emergency care, whereas it would normally have been possible for three lines to respond to such cases. This resulted in six refusals of emergency calls for tertiary trauma cases during the State of Emergency, whereas there were no such refusals in the same period of the previous year. However, the difference of 18 severe tertiary trauma surgery cases (spinal cord injuries, pelvic acetabular fractures, head and neck or thoracoabdominal injury, and limb open fractures) between the two periods is not fully accounted for by the 6 refusal cases in the COVID-19 period.
During the State of Emergency, all schools and universities, and many department stores and restaurants, were closed, and many workplaces promoted remote work. Thus, human movement declined markedly. For example, a report from the Japan Ministry of Land, Infrastructure and Transport showed that the average daily traffic volume per day on the Metropolitan highway decreased by 28% from 1,088,000 vehicles in April 2019 to 781,000 vehicles in April 2020 (Japan Ministry of Land, Infrastructure and Transport, in Japanese, https://www.mlit.go.jp/policy/shingikai/content/001351206.pdf, cited Aug 5, 2020). This reduction in human movement might be a reason for the lower number of trauma surgeries in the COVID-19 period than in the equivalent period in 2019.
According to the Japan Trauma Data Bank Report 2019 (in Japanese, https://www.jtcr-jatec.org/traumabank/dataroom/dataroom.htm, cited Aug 5, 2020), traffic accidents were the most common injury mechanism at 32.3%, and fall from a high place was the third most common at 20.9%. The number of traffic accidents and injuries in Tokyo in April and May 2020, which are generally in the State of Emergency period, decreased by about 40% compared to the previous year (Table 4 , based on Metropolitan Police Department, Report of Traffic Injury Accidents, in Japanese, https://www.keishicho.metro.tokyo.jp/smph/about_mpd/jokyo_tokei/tokei_jokyo/traffic_accident.html, cited Aug 5, 2020). In addition, an analysis of 932 trauma cases showed that 551 (59%) were suicide attempts [5] and the number of suicides is likely to be related to the number of attempts. The National Police Agency showed that the total number of suicides of 293 in Tokyo in April and May 2020 was down 23.3% from that of 382 in April and May 2019 (Table 4, based on Statistics on Ensuring Life Safety and other Statistics on Suicides, in Japanese, https://www.npa.go.jp/publications/statistics/safetylife/jisatsu.html, cited Aug 5, 2020). The number of suicide attempts decreased during the State of Emergency period, and thus the number of serious crash trauma cases also decreased. The significantly older age of patients with severe trauma due to open fractures (75.0 years in the COVID-19 period compared to 37.8 years in the control period in 2019) may also reflect a decrease in high-energy trauma in young people during the State of Emergency period.
Table 4.
Number of traffic accidents, injuries due to traffic accidents, and suicides in the Tokyo metropolitan area in April and May in 2019 and 2020.
| 2019 | 2020 | % Reduction | |
|---|---|---|---|
| Accidents | 5256 | 2945 | 43.9% |
| Injuries | 5941 | 3307 | 44.3% |
| Suicides | 382 | 293 | 23.3% |
Severe trauma surgery cases, such as open fractures, spine and pelvic injuries, or head and neck and thoracoabdominal injuries, which are the most common types of severe trauma treated in trauma centers, were markedly less common in the COVID-19 period than in the control period, while the number of cases of hip fractures in elderly people increased. The emergency transport system in Japan is divided into three levels according to the severity and urgency of the injury. Our facility is a trauma center attached to a university hospital in Tokyo, and we handle both tertiary emergencies, the most severe and urgent of the three levels, and primary/secondary emergencies.
Most cases of hip fractures in elderly patients are treated as secondary emergencies. The increase in the number of elderly patients with these fractures at our trauma center during the State of Emergency may be due to hospitals outside our medical area that normally treat secondary emergencies being unable to accommodate these patients, or it may be that a decrease in severe trauma cases created room for secondary emergencies in trauma centers. The former explanation is supported by our findings showing that three hip fracture cases were transported from outside our medical area in the COVID-19 period that were not in the control period. The latter is supported by the reduced non-responses to secondary emergency trauma cases of 30 in the COVID-19 period compared to 47 in the control period. As we showed above, while the number of high-energy trauma cases associated with leaving home decreased substantially due to behavioral changes under the State of Emergency, elderly people still fell from standing height at home or in an institute and sustained an injury, and the number of cases of hip fracture did not decrease.
If COVID-19 was suspected, the patient was screened for COVID-19 using questionnaires and a chest CT scan. Until the results of RT-PCR for COVID-19 were available, the patient was admitted to a special ward for suspected COVID-19 cases, but there were no SARS-CoV-2 positive cases among the trauma cases. Many reports indicate that the prognosis of hip fractures complicated by COVID-19 is poorer than that of patients without COVID-19 complications [[6], [7], [8], [9]]. Screening by interview and CT imaging of the chest or preoperative diagnosis by RT-PCR may be important to evaluate the surgical risk and to prevent nosocomial infection [10,11]. The number of hip fracture surgeries did not decrease, even when social activities were restricted by the infection epidemic, and elderly patients with COVID-19 may have injuries. Therefore, trauma centers need to establish a system to prevent nosocomial infections in treating severe trauma cases with COVID-19.
In the UK, “social distancing” due to the COVID-19 pandemic began on March 17, 2020, and the country was “locked down” on March 24. The number of surgeries at a Level 1 trauma center in London in one month beginning on March 17 fell by two-thirds compared to the same period in 2019; however, there was no significant change in the number of hip fracture cases [12]. The University Hospital Trauma Center in Barcelona, Spain also reported that the number of trauma cases decreased by about a quarter, but with no significant change in the number of osteoporotic hip fracture cases from March 14-April 2, 2020, when a State of Emergency was declared in Spain, compared to the same periods in 2018 and 2019 [13]. Our findings are similar to those in these two studies. The results indicate that trauma surgery cases decrease in a setting of extensively limited social activity, such as the State of Emergency, but that surgeries for hip fractures do not decrease. These fractures often occur in elderly people in a “stay at home” setting. In this study, the overall mean age and the age of cases with open fracture in the COVID-19 period were higher than those in the control period. Therefore, the impact of the State of Emergency on fractures in elderly people was smaller than that in younger people.
The limitations of the current study include its retrospective observational design and performance at a single center at a university hospital in Tokyo. Thus, the results may not be representative of the national profile. However, the strength of the study is that it is the first of its kind in a large tertiary referral trauma center in Japan during the COVID-19 pandemic. Within these limitations, we conclude that the COVID-19 pandemic led to a decrease in the number of trauma surgeries at our university hospital trauma center, but that the number of surgeries for hip fracture increased despite the emergency situation.
Ethical approval
This study was approved by the Institutional Review Board.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgement
We thank Dr. Tokuhide Doi for helpful supports in research progression.
References
- 1.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R.D., Liu M.Q., Chen Y., Shen X.R., Wang X., Zheng X.S., Zhao K., Chen Q.J., Deng F., Liu L.L., Yan B., Zhan F.X., Wang Y.Y., Xiao G.F., Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 Mar;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., Hu Y., Tao Z.W., Tian J.H., Pei Y.Y., Yuan M.L., Zhang Y.L., Dai F.H., Liu Y., Wang Q.M., Zheng J.J., Xu L., Holmes E.C., Zhang Y.Z. A new coronavirus associated with human respiratory disease in China. Nature. 2020 Mar;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 Feb 20;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yahata T., Ishii K., Fujiwara T., Kurimoto H. A comparative study of the injury patterns after accidental and intentional high falls. Kanto journal of orthopedics and traumatology. 2012;43(2):111–114. [in Japanese] [Google Scholar]
- 6.LeBrun D.G., Konnaris M.A., Ghahramani G.C., Premkumar A., DeFrancesco C.J., Gruskay J.A., Dvorzhinskiy A., Sandhu M.S., Goldwyn E.M., Mendias C.L., Ricci W.M. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma. 2020 Aug;34(8):403–410. doi: 10.1097/BOT.0000000000001849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kayani B., Onochie E., Patil V., Begum F., Cuthbert R., Ferguson D., Bhamra J.S., Sharma A., Bates P., Haddad F.S. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint Lett J. 2020 Sep;102-B(9):1136–1145. doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. [DOI] [PubMed] [Google Scholar]
- 8.Muñoz Vives J.M., Jornet-Gibert M., Cámara-Cabrera J., Esteban P.L., Brunet L., Delgado-Flores L., Camacho-Carrasco P., Torner P., Marcano-Fernández F., Spanish Hip-Covid Investigation Group Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study. J Bone Joint Surg Am. 2020 Jul 1;102(13):e69. doi: 10.2106/JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thakrar A., Chui K., Kapoor A., Hambidge J. Thirty-day mortality rate of patients with hip fractures during the COVID-19 pandemic: a single centre prospective study in the United Kingdom. J Orthop Trauma. 2020 Sep;34(9):e325–e329. doi: 10.1097/BOT.0000000000001889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Konda S.R., Ranson R.A., Solasz S.J., Dedhia N., Lott A., Bird M.L., Landes E.K., Aggarwal V.K., Bosco J.A., 3rd, Furgiuele D.L., Gould J., Lyon T.R., McLaurin T.M., Tejwani N.C., Zuckerman J.D., Leucht P., Ganta A., Egol K.A., Nyu Covid Hip Fracture Research Group Modification of a validated risk stratification tool to characterize geriatric hip fracture outcomes and optimize care in a post-COVID-19 world. J Orthop Trauma. 2020 Sep;34(9):e317–e324. doi: 10.1097/BOT.0000000000001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J., Mi B., Hu L., Xiong Y., Xue H., Zhou W., Cao F., Liu M., Chen L., Yan C., Li H., Liu G. Preventive strategy for the clinical treatment of hip fractures in the elderly during the COVID-19 outbreak: wuhan's experience. Aging (Albany NY) 2020 May 7;12(9):7619–7625. doi: 10.18632/aging.103201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park C., Sugand K., Nathwani D., Bhattacharya R., Sarraf K.M. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the “golden month”. Acta Orthop. 2020 Oct;91(5):556–561. doi: 10.1080/17453674.2020.1783621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nuñez J.H., Sallent A., Lakhani K., Guerra-Farfan E., Vidal N., Ekhtiari S., Minguell J. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020 Jul;51(7):1414–1418. doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]