Abstract
Background
In order to contain the coronavirus disease 2019 (COVID-19) pandemic, Germany has implemented drastic restrictions on public or social life, while health institutions are invoked to postpone elective procedures. Although urologists are less involved in the direct treatment of COVID-19 patients, the current situation strongly affects the urological work routine.
Objective
To analyze the impact of the COVID-19 pandemic on various aspects of work and personal life among urologists in Germany.
Design, setting, and participants
A total of 589 urologists in Germany participated in an online survey between March 27 and April 11, 2020.
Outcome measurements and statistical analysis
Participants were stratified into subgroups according to professional characteristics.
Results and limitations
Most urologists rated Germany as “well prepared” and the increasing restrictions of social life as “very positive.” Routine operation was more restricted in hospitals than in the outpatient sector (p = 0.046). Moreover, urologists from the outpatient sector felt significantly less prepared for the COVID-19 pandemic (p = 0.001), reported a higher shortage of protective medical equipment (p < 0.001), and described a tendency toward a higher level of threat (p = 0.054). Although restrictions regarding telemedicine approaches were reported by 60% of participants, the outpatient sector used telehealth more frequently than hospitals (25.5% vs 17.0%, p < 0.001). Limitations include the national design and the restricted survey period.
Conclusions
This survey systematically evaluates the impact of the COVID-19 pandemic on personal and professional aspects of German urologists. We identified several issues, such as a higher shortage of medical protective equipment in the outpatient sector that could trigger specific measures to further improve the quality of urological care in Germany.
Patient summary
We evaluated a potential impact of the coronavirus disease 2019 (COVID-19) pandemic on professional and personal aspects of the urologists in Germany. Our results suggest that the outpatient sector should receive specific attention as, for example, shortage of protective equipment was more common.
Keywords: COVID-19 pandemic, Severe acute respiratory syndrome coronavirus 2, Urology, Telemedicine
Take Home Message
Our online survey analyzing the impact of the coronavirus disease 2019 (COVID-19) pandemic on German urologists revealed decisive differences between work sites. It will help identify weak spots within the health care system in order to improve the quality of urological care.
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has spread rapidly across the globe [1]. Owing to this unprecedented global health care crisis, drastic measures were taken within the German health care system and public life to contain the rapid dissemination of the virus and provide optimal patient care during this pandemic. As such, health care providers in Germany increased intensive care capacities significantly by postponing several “elective” surgical procedures, to be prepared for the growing number of coronavirus disease 2019 (COVID-19) patients [2]. While these measures eventually showed declining incidence and mortality rates in Germany, which in total were lower than those in many other European countries such as Italy, France, and Spain [1], they exert a strong impact on medical professionals’ private and work life. Although urologists do not represent a medical specialty leadingly involved in the treatment of COVID-19 patients, their regular working patterns have been altered radically. In order to support decision making during this unpredictable situation, the European Association of Urology (EAU) as well as the Germany Society of Urology (DGU) implemented guidelines regarding the diagnosis, surgical treatment, and follow-up for patients dealing with urological issues, including the use of personal protective equipment [3], [4], [5]. However, only very little real-world data on the actual implication of the COVID-19 pandemic among urologists exist to date. With this nationwide online survey compiled between March 27 and April 11, 2020, we intended to analyze the impact of the COVID-19 pandemic on daily work routine, communication, and telehealth approaches as well as on various aspects of private life among urologists in Germany.
2. Materials and methods
2.1. Data collection
Data collection was performed between March 27 and April 11, 2020. Participant acquisition was achieved via various communication channels. Detailed information of the participants is displayed in Table 1 . We acquired the survey data via a publicly accessible, web-based survey system (LimeSurvey, version 3.22.10). All participants agreed on the conditions of the survey before taking part. Please refer to the Supplementary material for detailed information on data collection.
Table 1.
Study population.
| Study population | |
|---|---|
| Total number of participating urologists | n = 589 |
| Gender (%) Female Male No answer |
28.4 69.9 1.7 |
| Age (yr), median (range) | 47 (25–78) |
| Work site (%) University Hospital/maximum-care hospital Regional hospital Ambulatory health care center/medical practice |
23.1 32.3 44.7 |
| Work environment (%) Operating room Standard care ward Outpatient clinic Not applicable |
27.5 23.6 8.5 40.4 |
2.2. Statistical analysis
All statistical analyses were performed using SPSS 23.0 (IBM Corporation, Armonk, NY, USA). Detailed information is given in the Supplementary material.
3. Results
3.1. Impact of the COVID-19 pandemic on professional aspects of German urologists
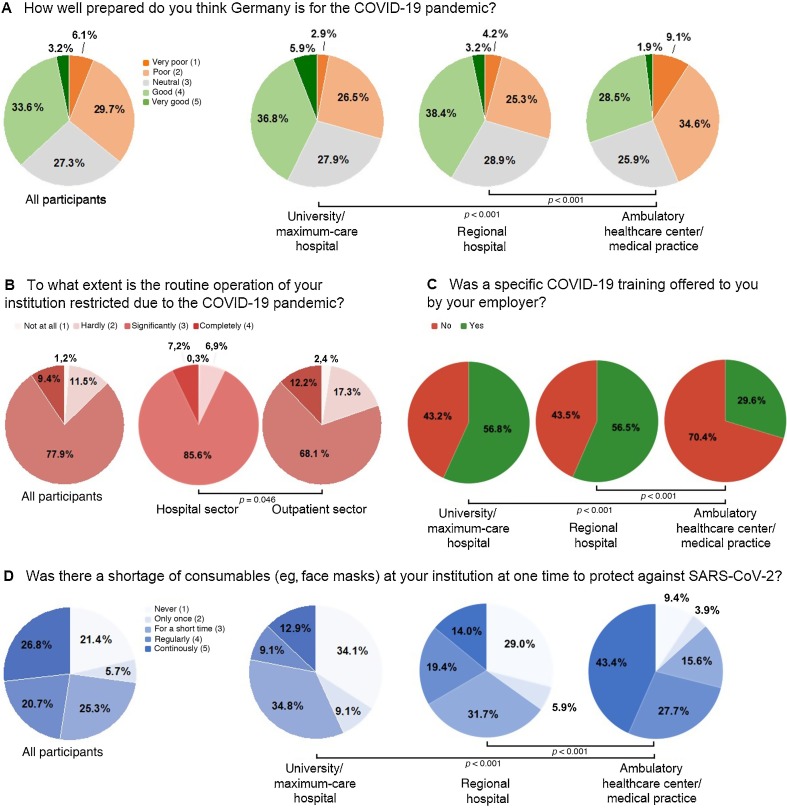
When asked to evaluate how well Germany is prepared for the COVID-19 pandemic, the most prominent answer (33.6%) was “good” (Table 2 ). Importantly, urologists from the outpatient sector rated the preparations significantly worse compared with both university hospitals and maximum-care hospitals (p = 0.001), as well as regional hospitals (p = 0.001; Table 2 and Fig. 1 A). In addition, most urologists (41.2%) feared a strong negative impact of past health policy decisions on the COVID-19 pandemic in Germany (Table 2). This assessment was consistent among urologists from different work sites (p = 0.342; Table 2).
Table 2.
Impact of the COVID-19 pandemic on professional aspects among German urologists.
| Not at all (1) | Hardly (2) | Moderate (3) | Strong (4) | Very strong (5) | p Value | |
|---|---|---|---|---|---|---|
| Has your daily work routine changed because of the COVID-19 outbreak? | 0.3 (2) | 2.6 (15) | 15.2 (87) | 42.4 (243) | 39.4 (226) | |
| Hospital Ambulatory health care center/medical practice |
0 (0) 0.8 (2) |
2.5 (8) 2.7 (7) |
14.5 (46) 16.1 (41) |
42.5 (135) 42.4 (108) |
40.6 (129) 38.0 (97) |
0.400 |
| Operating room Standard care ward Outpatient clinic |
0 (0) 0 (0) 0 (0) |
1.9 (3) 2.2 (3) 2.1 (1) |
9.5 (15) 13.3 (18) 27.1 (13) |
50.0 (79) 43.0 (58) 16.7 (8) |
38.6 (61) 41.5 (56) 54.2 (26) |
0.931 |
| Do you fear that past health policy decisions will have a negative impact on the COVID-19 pandemic in Germany? | 1.0 (6) | 7.9 (45) | 23.0 (132) | 41.2 (236) | 26.9 (154) | |
| Hospital Ambulatory health care center/medical practice |
0.9 (3) 1.2 (3) |
7.2 (23) 8.6 (22) |
23.3 (74) 22.7 (58) |
39.6 (126) 43.1 (110) |
28.9 (92) 24.3 (62) |
0.342 |
| Not at all (1) | Hardly (2) | Significantly (3) | Completely (4) | p Value | ||
| To what extent is the routine operation of your institution restricted due to the COVID-19 pandemic? | 1.2 (7) | 11.5 (66) | 77.9 (446) | 9.4 (54) | ||
| Hospital Ambulatory health care center/medical practice |
0.3 (1) 2.4 (6) |
6.9 (22) 17.3 (44) |
85.6 (272) 68.1 (174) |
7.2 (23) 12.2 (31) |
0.046 | |
| Very poor (1) | Poor (2) | Neutral (3) | Good (4) | Very good (5) | p Value | |
| How well prepared do you think Germany is for the COVID-19 pandemic? | 6.1 (36) | 29.7 (175) | 27.3 (161) | 33.6 (198) | 3.2 (19) | |
| University hospital/maximum-care hospital Regional Hospital Ambulatory health care center/medical practice |
2.9 (4) 4.2 (48) '9.1 (24) |
26.5 (36) 25.3 (48) 34.6 (91) |
27.9 (38) 28.9 (55) 25.9 (68) |
36.8 (50) 38.4 (73) 28.5 (75) |
5.9 (8) 3.2 (6) 1.9 (5) |
0.001 0.001 |
| How do you rate the measures taken by your employer against COVID-19? | 3.5 (20) | 13.5 (77) | 28.5 (163) | 39.9 (228) | 14.7 (84) | |
| Never (1) | Only once (2) | Only for a short time (3) | Regularly (4) | Continuously (5) | p Value | |
| Was there a shortage of consumables (eg, face masks or protective gowns) in your institution at one time to protect against SARS-CoV-2? | 21.4 (123) | 5.7 (33) | 25.3 (145) | 20.7 (119) | 26.8 (154) | |
| University hospital/maximum-care hospital Regional hospital Ambulatory health care center/medical practice |
34.1 (45) 29.0 (54) 9.4 (24) |
9.1 (12) 5.9 (11) 3.9 (10) |
34.8 (46) 31.7 (59) 15.6 (40) |
9.1 (12) 19.4 (36) 27.7 (71) |
12.9 (17) 14.0 (36) 43.4 (111) |
<0.001 <0.001 |
| No (1) | Yes (2) | p Value | ||||
| Was a specific COVID-19 training offered to you by your employer? | 55.3 (316) | 44.7 (225) | ||||
| University hospital/maximum-care hospital Regional hospital Ambulatory health care center/medical practice |
43.2 (57) 43.5 (81) 70.4 (178) |
56.8 (75) 56.5 (105) 29.6 (75) |
<0.001 <0.001 |
|||
In case of multiple pairwise comparisons, the level of significance was adjusted by Bonferroni correction. For three groups (three pairwise comparisons), a p-value of p=0.017 was considered statistically significant.
Fig. 1.
Impact of the COVID-19 pandemic on professional aspects of urologists during the COVID-19 pandemic. (A) Of all urologists, 33.6% rated Germany’s preparations for the COVID-19 pandemic as “good,” but urologists from the outpatient sector regarded the preparations as significantly worse compared with those from both university or maximum-care hospitals and regional hospitals (both p = 0.001). (B) Of all participants, 77.8% stated that operating procedures were “significantly” changed; however, these were significantly less affected in the outpatient sector (p = 0.046). (C) A specific COVID-19 training was offered to 44.7% of urologists and was significantly more frequently offered at university and maximum-care hospitals than at the outpatient sector (both p < 0.001). (D) Of all urologists, 26.8% reported a “permanent” shortage of consumable medical equipment. It was more common in the outpatient sector than in university or maximum-care hospitals and regional hospitals (both p < 0.001).
COVID-19 = coronavirus disease 2019; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
With respect to a potential change of daily work routine due to the SARS-CoV-2 outbreak, most urologists (42.4%) reported a “strong” alteration of daily work (Table 2). This assessment was consistent between work sites (p = 0.400) and different work environments (p = 0.931; Table 2). We next survey alterations in urological operating procedures during the COVID-19 outbreak. Here, most participants (77.8%) stated that operating procedures were “significantly” changed, meaning that, for example, almost no elective procedures were performed except for uro-oncological treatment (Table 3 ). Interestingly, routine operating procedures were significantly less affected in the outpatient sector (p = 0.046; Table 2 and Fig. 1B). In terms of measures against COVID-19 taken by their employer, most urologists (39.9%) rated the preparations as “good” and we observed no difference between work sites (p = 0.297; Table 2). We subsequently assessed the frequency of specific COVID-19 training that was offered to 44.7% of participants (Table 2 and Fig. 1C). Interestingly, COVID-19 training was significantly more frequently offered at university and maximum-care hospitals (56.8%) as well as regional hospitals (56.5%) than at ambulatory health care centers/medical practices (29.6%, both p < 0.001; Table 2 and Fig. 1C).
Table 3.
Significance of communication and telemedicine in urology during the COVID-19 pandemic.
| Very negative (1) | Negative (2) | Neutral (3) | Positive (4) | Very positive (5) | p Value | |
|---|---|---|---|---|---|---|
| How do you rate the quality of information in Germany regarding COVID-19? | 6.6 (39) | 14.1 (83) | 20.4 (120) | 49.4 (291) | 9.5 (56) | |
| Far too little (1) | Too little (2) | Just right (3) | Too much (4) | Far too much (5) | ||
| How do you rate the quantity of information in Germany regarding COVID-19? | 1.0 (6) | 10.9 (64) | 36.2 (213) | 43.6 (257) | 8.3 (49) | |
| Very low (1) | Low (2) | Moderate (3) | High (4) | Very high (5) | ||
| How do you rate the relevance of telemedical care/consultation during the COVID-19 pandemic? | 3.3 (19) | 19.0 (109) | 30.2 (173) | 32.6 (187) | 14.8 (85) | |
| Hospital Ambulatory health care center/medical practice |
0.6 (2) 6.7 (17) |
11.3 (36) 28.6 (73) |
26.7 (85) 34.5 (88) |
40.6 (129) 22.7 (58) |
20.8 (66) 7.5 (19) |
<0.001 |
| Not at all (1) | Only for individual cases (2) | Daily routine (3) | ||||
| Is there a possibility to reduce patient contact through telemedical approaches (eg, telephone consultation, videotelephony) at your institution? | 29.1 (167) | 50.1 (287) | 20.8 (119) | |||
| Hospital Ambulatory health care center/medical practice |
38.0 (121) 18.0 (46) |
45.0 (143) 56.5 (144) |
17.0 (54) 25.5 (65) |
<0.001 | ||
| No (1) | Partly (2) | Yes (3) | ||||
| Are there any technical or regulatory restrictions regarding the use of telemedicine during the COVID-19 pandemic at your institution? | 35.1 (201) | 40.1 (230) | 24.8 (142) | |||
| Hospital Ambulatory health care center/medical practice |
30.8 (98) 40.4 (103) |
45.0 (143) 34.1 (87) |
24.2 (77) 25.5 (65) |
0.161 | ||
In case of multiple pairwise comparisons, the level of significance was adjusted by Bonferroni correction. For three groups (three pairwise comparisons), a p-value of p=0.017 was considered statistically significant.
We concluded the section on work-related aspects by surveying a potential shortage of medical consumable materials among urologists in Germany. While most urologists (26.8%) reported a “permanent” shortage of consumable medical equipment, it was more common in the outpatient sector than in university or maximum-care hospitals (p < 0.001) and regional hospitals (p < 0.001; Table 2 and Fig. 1D).
3.2. Significance of communication and telemedicine in urology during the COVID-19 pandemic
We first asked participants to rate the overall quality and quantity of information on the COVID-19 outbreak in Germany. Here, most urologists (49.4%) gave “positive” feedback regarding the quality of COVID-19 information in Germany (Table 3). However, over 50% of urologists rate the quantity of information as either “too much” (43.6%) or even “far too much” (8.3%; Table 3).
We then evaluated the most important information channels that urologists in Germany use to gather information on the COVID-19 pandemic. The most prominent answer was “Internet” (85.4%) followed by “TV news” (63.5%), while “newspaper” (35.5%), “colleagues” (31.7%), “e-mail distribution list” (26%), as well as “friends and personal environment” (11.9%) were less common. Modern information channels such as “podcasts,” “social media,” and “apps” were used by 21.7%, 10.0%, and 8.0% of urologists, respectively. Interestingly, we observed significant differences in the preferred information channels between urologists of different ages. The use of social media (r: –0.153; 95% confidence interval [CI]: –0.222 to –0.077) and podcasts (r: –0.104; 95% CI: –0.180 to –0.024) correlated negatively and the use of newspapers (r: 0.145; 95% CI: 0.065–0.224) correlated positively with participants’ age.
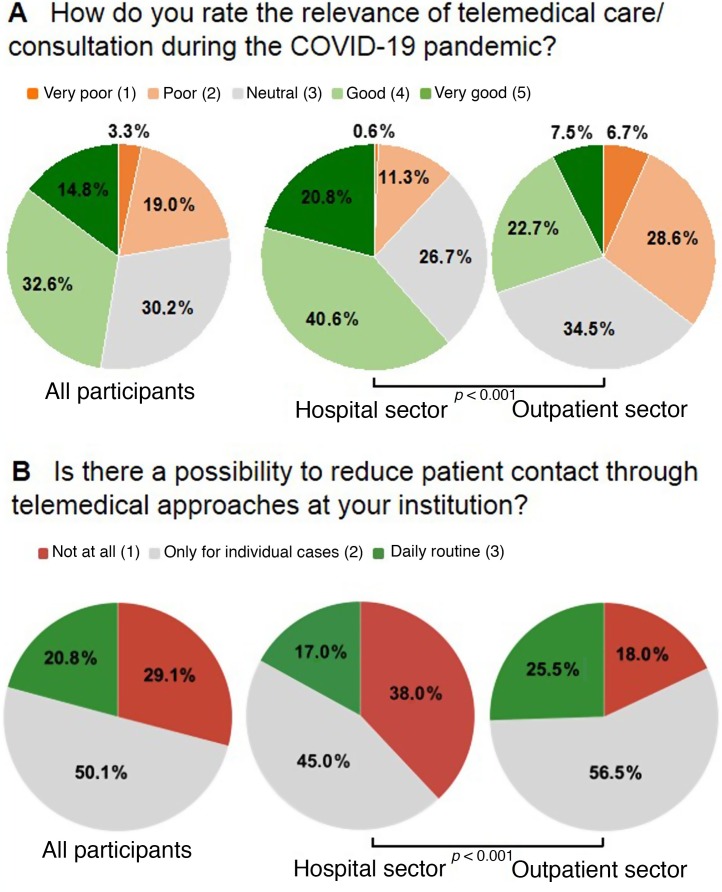
With respect to the significance of telemedicine during this pandemic, most participants (32.6%) stated that they see a “high” relevance of this approach (Table 3 and Fig. 2 A). Importantly, the relevance of telehealth was rated to be significantly higher in the hospital sector than in the outpatient sector (p < 0.001; Table 3 and Fig. 2A). When looking at the actual possibility to reduce patient contact through telemedical approaches (eg, telephone consultation and videotelephony), most urologists (50.1%) reported that this approach was feasible only for individual cases, but 20.8% said that this approach is already implemented in daily routine (Table 3 and Fig. 2B). Interestingly, the use of telemedicine was significantly higher in the outpatient sector than in hospitals (p < 0.001; Table 3 and Fig. 2B). Finally, we addressed potential technical or regulatory restrictions that might hamper the use of telemedicine during the COVID-19 pandemic. Here, >60% of participants reported some sort of restriction (“yes”: 24.8% and “partly”: 40.1%; Table 3). However, the prevalence of restrictions did not differ significantly between work sites (p = 0.161; Table 3).
Fig. 2.
Significance of communication and telemedicine of urologists during the COVID-19 pandemic. (A) Telemedicine was of high significance for most participants during the COVID-19 pandemic. Its relevance was rated as significantly higher in the hospital sector than in the outpatient sector (p < 0.001). (B) Of all urologists, 50.1% reported that telemedicine was feasible only for individual cases, but 20.8% said that this approach is already implemented in daily routine. The use of telemedicine was significantly higher in the outpatient sector than in hospitals (p < 0.001).
COVID-19 = coronavirus disease 2019.
3.3. Personal implications of the COVID-19 pandemic on urologists in Germany
We finally assessed personal implications of the COVID-19 pandemic. Most urologists (53.4%) felt a moderate level of threat caused by the COVID-19 pandemic (Table 4 ). The level of threat showed a strong trend toward higher levels among urologists from the outpatient sector compared with those from the hospital sector (p = 0.054; Table 4). Moreover, most urologists (46.5%) stated that their private life has strongly been affected by the pandemic and that COVID-19 had a “negative” (49.8%) influence on their personal mood (Table 4). In terms of official restrictions of public life set by the federal government, these measures were predominantly rated as “very positive” (56.1%; Table 4). However, urologists from the hospital sector tend to rate the restrictions significantly better than the urologists from the outpatient sector (p = 0.049; Table 4). Finally, we surveyed the level of concern that urologists have both about their own health and about the health of others during the COVID-19 pandemic. Interestingly, most participants stated a moderate level of concern with respect to their own health (43.1%) but a high level of concern with respect to the health of others (45.3%; Table 4). Of note, the level of concern regarding own health correlated significantly with participants’ age, meaning that older urologists tend to have a higher level of concern than younger urologists (r S: 0.139, p = 0.001).
Table 4.
Personal implications of the COVID-19 pandemic on urologists in Germany*.
| Not at all (1) | Hardly (2) | Moderate (3) | Strong (4) | Very strong (5) | p Value* | |
|---|---|---|---|---|---|---|
| How threatened do you feel by the COVID-19 pandemic? | 2.4 (14) | 19.4 (114) | 51.3 (302) | 21.7 (128) | 5.3 (31) | |
| Hospital Ambulatory health care center/medical practice |
2.8 (9) 1.9 (5) |
20.2 (66) 18.3 (48) |
53.4 (174) 48.7 (128) |
19.6 (64) 24.3 (64) |
4.0 (13) 6.8 (18) |
0.054 |
| How much is your private life restricted by the COVID-19 pandemic? | 0.2 (1) | 4.6 (26) | 19.6 (111) | 46.6 (264) | 29.0 (164) | |
| How concerned are you about your own health in the context of the COVID-19 pandemic? | 4.9 (28) | 34.5 (195) | 43.1 (244) | 12.5 (71) | 4.9 (28) | |
| How concerned are you about the health of others in the context of the COVID-19 pandemic? | 0.2 (1) | 5.7 (32) | 32.7 (185) | 45.3 (256) | 16.1 (91) | |
| Very negative (1) | Negative (2) | Neutral (3) | Positive (4) | Very positive (5) | p Value | |
| How does the COVID-19 pandemic influence your personal mood? | 4.6 (26) | 49.8 (281) | 43.4 (245) | 2.1 (12) | 0 (0) | |
| How do you rate the increasing restrictions of public life? | 1.2 (7) | 3.7 (21) | 6.3 (36) | 32.6 (185) | 56.1 (318) | |
| Hospital Ambulatory health care center/medical practice |
0.9 (3) 1.6 (4) |
3.2 (10) 4.4 (11) |
4.7 (15) 8.4 (21) |
32.0 (101) 33.5 (84) |
59.2 (187) 52.2 (131) |
0.049 |
In case of multiple pairwise comparisons, the level of significance was adjusted by Bonferroni correction.
A p-value of p=0.017 for three groups and p=0.003 for six groups was considered statistically significant.
4. Discussion
The outbreak of SARS-CoV-2 has been accompanied by remarkable changes in health care services and social life. Although urologists are less involved in direct treatment of COVID-19 patients, the SARS-CoV-2 pandemic decisively affects this subgroup of medical professionals. Our study is the first to analyze the impact of the COVID-19 pandemic on work-related and personal aspects of urologists in Germany.
According to the recommendations of the German federal government, hospitals are invoked to prepare for a growing number of COVID-19 patients, for example, by providing additional intensive care capacities, thus radically altering working patterns [2]. Our survey clearly illustrates the effects of these measurements, as the daily work routine of a German urologist has “strongly” (42.4%) or even “very strongly” (39.4%) changed. On March 13, 2020, the Federal Ministry of Health recommended to postpone “elective” surgical procedures in order to increase health care resources further. Our study corroborated these findings, as most urologists stated that routine operation was “significantly” restricted at their institution, which is in good agreement with other uro-oncological surveys from Europe [6]. This finding underlines the conflict of sufficiently preparing the health care system for an increasing number of COVID-19 patients on the one hand and maintaining adequate care for non–COVID-19 patients regarding emergency as well as routine services on the other. In order to support decision making in this unpredictable situation, the EAU as well as the DGU and different other national urological societies implemented guidelines for the diagnosis, surgical treatment, and follow-up of urological patients [3], [4], [5], [7], [8]. Considering the uncertainty of the ongoing COVID-19 pandemic in the near future, decisions for or against a surgical procedure or treatment should include aspects such as medical urgency, patients’ age, availability of alternative treatment options, and capacities of the health care provider [4], [5], [9], [10]. In this line of thinking, it is important to note that the drastic measures within the German health care system might have retrospectively been considered too excessive, as, for example, many of the additional intensive care capacities have not been used up to date. Importantly, reimbursement for “empty beds” of €560/d represents an incentive for hospitals to keep beds free instead of treating patients. Together, these points highlight the fine line between a too excessive shutdown and a potential overload of the health care system, which should be monitored continuously during this ongoing pandemic. Our data also indicate that hospitals more often postponed elective urological treatment compared with the outpatient sector, which can be explained by the fact that the outpatient sector is not obliged to free up resources such as intensive care capacities. Urologists working in the outpatient sector might thus consider extending their capacities and office hours to take care of urological patients who would have been treated in a hospital under normal conditions [4]. Of note, German authorities guarantee a financial compensation of 90% of their regulatory income for physicians in the outpatient sector who suffer significant losses due to the COVID-19 pandemic.
Although most urologists rated the measures offered by their employer as “good” and stated that Germany is “well” prepared for the COVID-19 pandemic, the outpatient sector rated the preparations as significantly worse compared with the hospital sector. Furthermore, most urologists feared a strong negative impact of past health policy decisions on the COVID-19 pandemic in Germany. In line with the global shortage of medical protective equipment such as protective gowns and face masks [11], most urologists reported a “permanent” shortage of consumable medical equipment, which was even more common in the outpatient sector. In addition, the outpatient sector obtained less COVID-19 training than hospitals. The lack of specific COVID-19 training as well as critical supply of personal protective equipment, especially in the outpatient sector, might result from prioritization of hospitals as they—at first glance—seem to be of higher systemic relevance [12]. However, as only a limited number of COVID-19 patients are hospitalized [13], the outpatient sector embodies a major pillar of patient care during this pandemic. Consequently, a need-based distribution of available resources is of utmost importance during the COVID-19 pandemic. In terms of medical training, the outpatient sector should also gain more attention as it is easier to provide specific COVID-19 training at larger health care institutions such as university hospitals. Although some specific training and online webinars for outpatient physicians on general information on COVID-19, treatment options, as well as measures to reduce the virus transmission have already been offered [14], these training programs should be expanded and further supported in the future.
During a global health care threat, such as the current COVID-19 pandemic, a reliable flow of information is essential. In our study, most urologists evaluated the quality of COVID-19 information in Germany as positive, but the quantity of information on COVID-19 is too much. A reason for that might be that urologists do not represent the medical specialty leadingly involved in the treatment of COVID-19 patients, thus also seeking for other information, for example, regarding urological treatment options. The study furthermore revealed that social media and podcasts were preferred by younger urologists, while older urologists more often favored newspapers. This is in line with a prior study evaluating the use of social media for knowledge acquisition among urologists [15].
Telemedicine could be of great value to reduce direct contact between patients and medical staff during this pandemic. In our study, most urologists stated a high relevance of telehealth and 20.8% of all urologists already included telemedical approaches (eg, telephone consultation and videotelephony) in their daily routine. This trend is also present in other European countries [16], [17]. Interestingly, the relevance of telehealth was rated to be higher by the hospital sector, while urologists from the outpatient sector had already included telemedical approaches in their daily routine and used it more frequently. This shows that telehealth currently seems to be more feasible in the outpatient sector as these urologists mainly hold a monitoring function for their patients and perform surgery less frequently. Of note, telemedical appointments are accepted by 84.7% of urological patients [18]. Despite a growing acceptance of telehealth among German urologists, 60% of all participants reported some sort of technical or regulatory restrictions. Data protection and security issues, inadequate reimbursement of many telemedical services in Germany, as well as a slow Internet connection, especially in rural areas, represent major issues in this line of thinking [18]. Thus, legislative changes regarding data protection and the consequent integration of telehealth services into reimbursement catalogs are of utmost importance to overcome these existing restrictions.
We finally evaluated the potential burden on various aspects of private life among German urologists. Most urologists described a “moderate” level of threat, a “strong” affection of private life, as well as a “negative” influence on their personal mood by the COVID-19 pandemic. This is in line with recent studies from China, displaying a high psychological burden on health care workers [19], [20]. Furthermore, most participants stated a “moderate” level of concern with respect to their own health, especially among older urologists, but a “high” level of concern with respect to the health of others, which can be explained by the fact that age has been reported as a major risk factor for more severe clinical courses of COVID-19 [21]. Although most German urologists rated the official restrictions of public life by the federal government as “very positive,” urologists working in the outpatient sector tend to rate the restrictions significantly worse compared with the urologists from the hospital sector. In addition, the level of threat was higher among urologists from the outpatient sector. A possible explanation for this finding might be the strong financial involvement of mostly self-employed urologists from the outpatient sector, who might fear financial damage due to the reduction of nonurgent patient consultations.
Of note, our study has some limitations. First, the survey included urologists only from the German health care system, which does not allow a transfer of results to other countries as well as other specialties. Second, we could not monitor response rates to our online survey, which might imply that the results are not fully representative of the population surveyed. Moreover, the online survey was performed within a timeframe of about 3 wk. Thus, long-term information on the perception and impact of the COVID-19 pandemic cannot be generated. Finally, the survey design and questions lack validation, and results were drawn from descriptive statistics and thus do not include analyses of potential confounding variables.
5. Conclusions
In summary, this study is the first to evaluate the early perception of the COVID-19 pandemic among urologists in Germany. Although routine work patterns during the COVID-19 pandemic has more decisively changed in the hospital sector due to official regulations, urologists from the outpatient sector felt less prepared for the COVID-19 outbreak and claim a higher shortage of consumables as well as a tendency toward a higher level of threat. Finally, telehealth was rated to represent a valuable tool in the treatment of urological patients during this ongoing pandemic and should be implemented further in the outpatient and hospital urological sector.
Author contributions: Pia Paffenholz had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Paffenholz, Loosen, Peine.
Acquisition of data: Paffenholz, Loosen, Peine.
Analysis and interpretation of data: Paffenholz, Loosen, Hellmich.
Drafting of the manuscript: Paffenholz, Loosen.
Critical revision of the manuscript for important intellectual content: Peine, Fischer, Pfister, Heidenreich.
Statistical analysis: Paffenholz, Loosen, Hellmich.
Obtaining funding: None.
Administrative, technical, or material support: Peine.
Supervision: Heidenreich.
Other: None.
Financial disclosures: Pia Paffenholz certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Acknowledgments: The authors would like to express their gratitude to all individual participants of the survey. Moreover, we would like to thank the DGU, Federation of German Urologists (BDU), German Society of Residents in Urology (GeSRU), and Bündnis Junge Ärzte (BJÄ), as well as several hospitals and individuals for distributing the online survey.
Conflict of interests: AH is chief executive officer and partner of Clinomic GmbH. No other conflict of interest declared.
Associate Editor: Malte Rieken
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.euf.2020.06.001.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Johns Hopkins Coronavirus Resource Center . 2020. COVID-19 map.https://coronavirus.jhu.edu/map.html [Google Scholar]
- 2.Combs S.E., Belka C., Niyazi M. First statement on preparation for the COVID-19 pandemic in large German speaking university-based radiation oncology departments. Radiat Oncol. 2020;15:74. doi: 10.1186/s13014-020-01527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.EAU Guidelines Panel . 2020. COVID-19 recommendations.https://uroweb.org/covid-19-recommendations-by-eau-guidelines-panels/ [Google Scholar]
- 4.Kriegmair M.C., Kowalewski K.F., Lange B. Urologie in der Corona-Virus-Pandemie – Leitfaden 4/20. Urologe. 2020;59:442–449. doi: 10.1007/s00120-020-01200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DGU (Deutsche Gesellschaft für Urologie e.V.). Priorisierungsliste Urologie in Zeiten den Corona-Pandemie mit reduzierten Kapazitäten (Version 2.0, April 2020). https://www.urologenportal.de/fileadmin/MDB/PDF/Presse/ab_Oktober_2019/DGU_Priorisierungsliste_2.0.pdf.
- 6.Oderda M, Roupret M, Marra G, et al. The impact of COVID-19 outbreak on uro-oncological practice across Europe: which burden of activity are we facing ahead? Eur Urol 2020. In press. 10.1016/j.eururo.2020.04.036. [DOI] [PMC free article] [PubMed]
- 7.American College of Surgeons. Clinical issues and guidance. https://www.facs.org/covid-19/clinical-guidance.
- 8.Ficarra V, Novara G, Abrate A, et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol 2020. In press. 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed]
- 9.Campi R, Amparore D, Capitanio U. Assessing the burden of urgent major uro-oncologic surgery to guide prioritisation strategies during the COVID-19 pandemic: insights from three Italian high-volume referral centres. Eur Urol 2020. In press. 10.1016/j.eururo.2020.03.054. [DOI] [PMC free article] [PubMed]
- 10.Stensland K.D., Morgan T.M., Moinzadeh A. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur Urol. 2020;77:663–666. doi: 10.1016/j.eururo.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Livingston E, Desai A, Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA 2020. In press. 10.1001/jama.2020.5317. [DOI] [PubMed]
- 13.Garg S., Kim L., Whitaker M. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.https://www.aekwl.de/fileadmin/user_upload/aekwl/Für_Ärzte/Fortbildung/Dokumente/Hochkantformat_Versand_COVID19-ohne_virtuelles_KH.pdfÄrztekammer Westfalen-Lippe. Covid-19—Online-Schulung für Ärztinnen und Ärzte. .
- 15.Rivas J.G., Socarras M.R., Patruno G. Perceived role of social media in urologic knowledge acquisition among young urologists: a European survey. Eur Urol Focus. 2018;4:768–773. doi: 10.1016/j.euf.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Marandino L, Di Maio M, Procopio G, Cinieri S, Domenico Beretta G, Necchi A. The shifting landscape of genitourinary oncology during the COVID-19 pandemic and how Italian oncologists reacted: results from a national survey. Eur Urol 2020. In press. 10.1001/jama.2020.4031. [DOI] [PMC free article] [PubMed]
- 17.Luciani L.G., Mattevi D., Cai T., Giusti G., Proietti S., Malossini G. Teleurology in the time of COVID-19 pandemic: here to stay? Urology. 2020;140:4–6. doi: 10.1016/j.urology.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boehm K, Ziewers S, Brandt MP, et al. Telemedicine online visits in urology during COVID-19 pandemic—potential, risk factors, and patients’ perspective. Eur Urol 2020. In press. 10.1016/j.eururo.2020.04.055. [DOI] [PMC free article] [PubMed]
- 19.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.