Abstract
Background
Containment measures for COVID-19 have affected surgical training globally. We sought to assess how neurosurgical training has been affected across Africa in April 2020.
Methods
A cross-sectional survey was distributed to African Neurosurgical trainees seeking to review demographics and effects of COVID on training.
Results
A total of 123 neurosurgery trainees responded from 23 African countries and a further 6 were abroad. A total of 91.80% were men, and 96.70% were training in public institutions. Only 41% had received training in COVID-19 with 61.79% worried that they would contract COVID-19 while performing their clinical duties. There was a marked reduction in clinical activities including a median reduction of elective surgery (−80%), clinics (−83%), and emergency surgery (−38.50%). A total of 23.58% of residents did not receive a formal salary, with 50% on less than $1000 USD gross per month.
Conclusions
This is the first continental survey of neurosurgery trainees in Africa. COVID-19 has significantly affected clinical and learning opportunities. There are concerns of the long-term effects on their training activities for an uncertain period of time during this pandemic. Although there has been a global increase in e-learning, there is need to evaluate if this is accessible to all trainees.
Key words: Africa, COVID-19, Education, Neurosurgery, Pandemic, Trainees
Abbreviations and Acronyms: CAANS, Continental Association of African Neurosurgical Societies; COSECSA, College of Surgeons of East, Central, and Southern Africa; COVID-19, Coronavirus disease 2019; HCWs, Health care workers; PPE, Personal protective equipment; WFNS, World Federation of Neurosurgical Societies
Introduction
The first case of coronavirus disease 2019 (COVID-19) was reported in Africa on February 14, 2020 in Egypt. As of July 16, 2020 there were 645,591 cases and 14,067 deaths on the African continent.1 As with all other areas affected by COVID-19, educational establishments were closed as part of the public health measures to reduce spread of the disease. In addition, many institutes rearranged their clinical workflows to limit elective work in anticipation of an influx of patients requiring admission and critical care facilities. One of the most comprehensive continental articles to detail this is the College of Surgeons of East, Central, and Southern Africa (COSECSA),2 which sets to limit elective activity and protect health care staff with provision of appropriate personal protective equipment (PPE).
There is a general worldwide shortage of doctors. Park et al.3 noted that there is a deficit of 23,500 neurosurgeons to provide at least 5 million essential neurosurgery procedures. In the last 20 years, there has been a huge drive to expand training numbers to cater for this unmet need.
The long-term effects of COVID-19 on neurosurgical training at present remains unclear.4 We sought to take a snapshot of the effect on neurosurgical training in April 2020.
Methods
A 52-question survey was formulated covering several key areas: demographics, presence of a neurosurgical society, the availability of COVID national speciality guidelines, the effects of COVID on clinical work, personal finances, and family dynamics. The effect on residents' training was also assessed and is the principal focus of this article. A separate article covers the effect of COVID-19 on neurosurgery services and the psychosocial impact on African neurosurgeons.5 The survey was discussed by the Continental Association of African Neurosurgical Societies (CAANS) Administrative Council.
The CAANS COVID-19 survey was undertaken between April 16 and May 21, 2020. The survey was disseminated through the secretary of CAANS Administrative Council, emails to African surgeons, and through social media (Twitter, WhatsApp, and Telegram).
Results
Demographics
A total of 123 trainees responded to the survey. They were in 23 countries (Figure 1 ) with a further 6 undergoing training out of Africa at the time of the survey. Nigeria (27) and South Africa (19) had the highest response rates (Figure 2 ). Ninety-five (77.24%) respondents were men with 113 (91.80%) being <40 years old. One hundred eighteen (96.70%) were training in public institutions, which were mainly in urban settings (112, 91.80%). Median duration of training was 5 (p25 = 5 p75 = 6) (min. = 2.5 max. = 8) years. Senior trainees comprised the laregst group of respondents (Figure 3). Twenty-seven (21.95%) reported they were currently training in a different country to their families.
Figure 1.
Countries that responded.
Figure 2.
Trainees by country.
Figure 3.
Training level of trainees as reported by respondents.
Academic Program
Departmental teaching had been cancelled for 54 (43.90%) respondents, although it is encouraging to note that 54 (43.90%) had received online teaching and 15 (12.20%) received online national teaching. Seventy (56.90%) were logging on to webinars provided by other international bodies or departments. Unsurprisingly, the disruption of the regular academic program resulted in 71 (57.72%) having their examinations postponed and 24 (19.51%) having their examinations cancelled. Most respondents were still working in their respective departments with only 14 (11.38%) re-deployed, although 31 (25.20%) had their training rotations suspended, 9 (7.32%) having their training suspended at present, and 4 (3.25%) had been sent home.
Clinical Activity
There was an overall reduction in clinical activities with clinics being most affected (Figure 4 ). Fifty-six (45.50%) respondents reported clinics were cancelled, and 61.00% (75) had a reduction in clinic volumes. One hundred thirteen (91.87%) reported that elective surgery volumes had reduced, and only 2 (1.63%) respondents reported an increase in elective cases. There was a reported 83% reduction in median clinic volume from 30 (p25 = 15 p75 = 50) (min. = 0 max. = 150) to 5 (p25 = 0 p75 = 10) (min. = 0 max. = 300) patients per week. One hundred thirteen (91.90%) reported a reduction in elective surgery. There was an 80% reduction in median weekly elective surgical cases from 5 (p25 = 3 p75 = 10) (min. = 0 max. = 40) to 1 (p25 = 0 p75 = 4) (min. = 0 max. = 40). Weekly emergency surgery per resident also dropped by −53.85% from a median of 6 (p25 = 4 p75 = 14) (min. = 0 max. = 90) to 3 (p25 = 1 p75 = 7) (min. = 0 max. = 40) and this was reported by 92 (74.80%) resident respondents (Figure 5 ).
Figure 4.
Percentage of respondents reporting changes in clinical activities.
Figure 5.
Changes in clinical activity.
Up to the month of April 2020, 112 (93.40%) reported there were COVID-19 cases in their resident country, although only 19 (14.4%) knew of a member of the neurosurgical community who had tested positive for COVID-19. As of April, there were no known deaths from COVID reported within the neurosurgical community by our respondents. Only 50 (41.0%) reported receiving any training in managing COVID-19 patients, and only 52 (41.6%) had received training on how to wear PPE. Fifty-five (28%) reported that they lacked PPE, and 76 (61.79%) were fearful that they would contract COVID-19 during their clinical duties. As of April 2020, 28 (22.75%) of respondents had been exposed to a COVID-19 patient in their clinical activities, a further 34 (27.64%) suspected that they may have been exposed to COVID-19-positive patients, whereas 56 (45.52%) were confident that they had not been exposed to COVID-19-positive patients. The emergency room (35, 28.46%) followed by the critical care (14, 11.38%) were reported to be the clinical areas where respondents were most likely to have been exposed to COVID-19-positive patients (Figure 6 ). Seventy (56.91%) respondents stated they lacked training in managing neurosurgical patients who are COVID-19-positive.
Figure 6.
Clinical areas and risk of exposure to COVID-19.
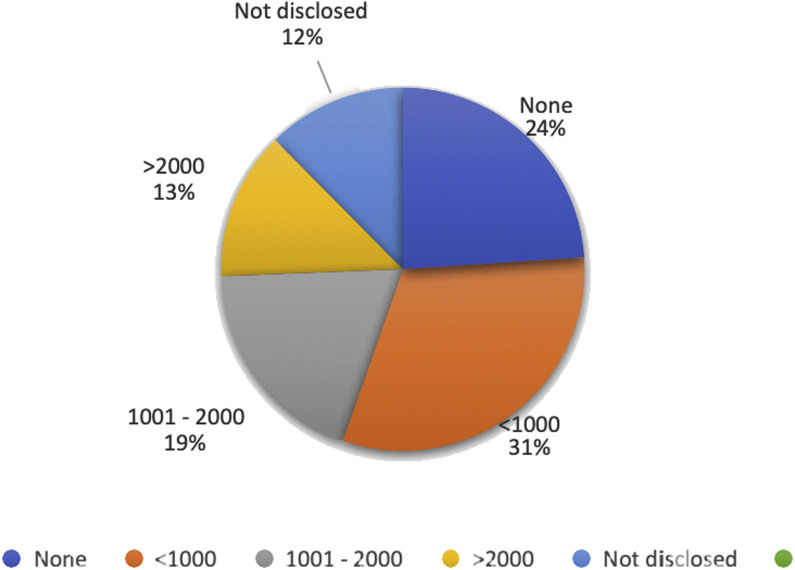
Income
As pertains to income, 29 (23.58%) do not receive a formal salary during their residency, with 50% receiving a gross monthly income of less than $1000 USD per month. Fifteen (12.20%) of the respondents supplement their income with locum-based income of whom 8 (53.30%) receive a private practice income less than $500 USD gross per month (Figure 7 ). Fortunately, as of April 2020, COVID-19 had no effect on income for 104 (84.55%) respondents, although 12 (9.76%) did report a drop in income, whereas 5 (4.07%) reported an increase in income. Fifteen (12.20%) stated they had financial concerns owing to the effect of COVID on their finances.
Figure 7.
Respondents monthly income (USD).
Discussion
Neurosurgery training is principally an apprenticeship with years of continuous clinical exposure augmented by didactic, simulated, or personal study. COVID-19 is a highly contagious disease, which in a fairly short space of time has changed how we interact professionally and personally. Because it was declared a pandemic by the World Health Organization March 11, 2020,6 many countries have taken different steps to reorganize its clinical services in anticipation of the surge of patients. Guidelines have been issued by various neurosurgical organizations in Africa, France, America, and India.2 , 7, 8, 9 Most guidelines recommend a reduction or postponement of elective activities.
The reorganization of clinical and academic activities is bound to affect neurosurgical training. Scullen et al.10 reports New Orleans experience in the reduction of the number of residents on duty, utilization of teleconferencing to maintain academic activities, and redeployment to support the critical care services. Similar adaptations have been reported by Bambakidis and Tomei11 in Canada and Lee et al.12 in Singapore. Although our survey reports a reduction of clinical activity, the level of redeployment was low (11.35%). This low level of redeployment may reflect that as a continent there were relatively fewer cases per population at the time of the survey, and neurosurgery services are relatively small compared with the population. It is also a reflection of COVID-19-positive cases being reported later in the continent, as the number of cases rises, staff (especially trainees) may find themselves redeployed.
For those trainees who have had examinations cancelled or postponed, institutions worldwide are exploring alternatives that utilize video conferencing. Telemedicine has had a dramatic uptake during this pandemic,13, 14, 15, 16, 17, 18 and it will be interesting to see if components of assessing teleconsultations will be incorporated in future examinations. By the same token, increased utilization of online resources and webinars by residents calls for an assessment to see if there are any socioeconomic barriers, such as access to laptops, internet access, et cetera, that may cause a disadvantage to some of the trainees. Another challenge is also the sudden proliferation of educational webinars, which on their own merit could have been meaningful to trainees, but because there is no structure or coordination, it may lead to a chaotic and confusing educational space. There is an opportunity to set up a continental e-learning platform that can help standardize training, encourage collaboration, and widen participation for surgeons who may work relatively remotely or in countries with very small neurosurgical communities.19
The adoption of technology in training will enhance training in the continent both at a training unit level and in increasing regional collaboration. This includes creating centralized e-learning hubs that curate teaching opportunities much like other international neurosurgical organizations have done.20 Key areas would be in creating a platform where research and audit projects in the region can be recorded and appropriately indexed. In terms of skills training, utilizing augmented reality platforms,21 portable microscopes and endoscopes, and simple exoscopes would be very useful. We can innovate and adapt saw-bone cranial and spinal models to use across hospital facilities and develop a stronger culture of dry labs in World Federation of Neurosurgical Societies (WFNS)-accredited training sites, and to lobby corporates through the WFNS Foundation to provide such material to trainees in low- and middle-income countries. This would ensure that hands-on training becomes an integral part of resident training, given that cadaver labs are more unlikely to be available. The increasing utility of augmented reality in training22 should also be explored as this may allow remote supervision of operating surgeons by more experienced colleagues or allow for relay of cadaver or intraoperative surgery for training.
Residents expressed concerns on the lack or training in managing COVID-19-positive patients and in wearing PPE. There are emerging publications of neurologic conditions as a result of COVID-19,23 therefore it is important for clinicians to recognize when COVID-19 should be considered as a differential. There have been concerns internationally on training health care workers (HCWs).24, 25, 26, 27 Understandably, there is a worry of contracting COVID-19 on the job.28 These fears have been realized in other countries where clinicians contracted COVID-19 and some sadly paid the ultimate price. As of April 5, 2020, some 12,252 health workers in Italy have tested positive for COVID-19, making up 10% of Italy's COVID-19 cases; furthermore, 80 medical doctors and 25 nurses have died.27 African countries know only too well the impact of HCWs illness and death as have been witnessed with the HIV epidemic,29 tuberculosis,30 and in localized epidemics from Ebola.31 It was evident from previous epidemics that most African countries lacked the logistical and financial abilities to rapidly expand inpatient facilities, especially critical care capacity. This has resulted in a strong public health response to COVID-19 and efforts are now coordinated in part by the Africa Center for Disease Control32; although funding of health initiatives remains a challenge.
There does remain a need to ensure that HCWs on the continent receive the right training and PPE to be able to undertake their clinical duties.24 We need to learn from what other countries have done to limit infection of HCWs including provision of PPE, training, temperature checks, et cetera, as demonstrated in countries such as Singapore.33 In our survey, trainees reported to have most likely been exposed to COVID-19-positive patients in the emergency room, which reflects the clinical reality where junior team members are most likely to be onsite triaging patients prior to a formal diagnosis of COVID-19 being made. Senior team members are also more likely to give a clinic opinion on the telephone, and therefore will have an overall reduced volume of contact with emergency patients. This calls for collaboration with emergency departments to ensure that all patients are reviewed with the assumption that they may be COVID-19-positive, and therefore at risk of infecting the doctors taking care of them.
There are already reports of increased anxiety and depression among HCWs.34, 35, 36, 37 This is due to caring for acutely unwell patients for a health condition not fully understood and with a risk of infection and mortality with no known cure. Studies36 indicate being junior, having a young family, and having infected family members are particular risk factors for anxiety. The changes in clinical roles and rotas, need to self-isolate, or separation from family may result in loss of social support structures. It would be prudent for supervising consultants to bear this in mind and appreciate that some trainees may require more social support owing to the disruption to their personal lives and extended separation from their social support network. This may be in the form of rotas that ensure adequate rest breaks, access to meals while on duty, rest spaces, and maintain contact via various communication platforms.
Many African countries do not have formal neurosurgery training schemes or fellowship opportunities.3 , 38, 39, 40 Not surprisingly, given the paucity of training centers, 21.95% of trainees were in a different country to their families. At the time of the survey, with the exception of Burundi and Tanzania, all other countries had closed their borders, and passenger international air travel had effectively ceased. This meant that these trainees have been separated from their families and it is unclear when cross-border travel will be feasible. Even when the air space or border restrictions are eased, a likely increase in travel costs may further delay trainees reconnecting with their families.
As pertains to income, 23.58% of trainees did not receive a salary, and 50% received less than $1000 USD gross salary per month. Residency positions are few, and some institutions do not have funding allocated for residents' remuneration. These residents often supplement their income with working as locum staff in local hospitals or clinics. This locum work is often to cover elective work and, as noted in our data, there is a significant reduction in elective work, which will significantly reduce the potential for these residents to earn enough to cover their living expenses. If the disruption of surgical training is prolonged, the financial strain on this group of trainees may affect their ability to complete their training. As noted by Prause et al.,41 income volatility is linked to depression. It is also worthwhile for neurosurgical organizations to factor this in when organizing academic activities, as this may account for the historically low turnout of African residents at international meetings, which are often held in high-income countries. There is an expected global economic downturn, which may further exacerbate this situation. With this in mind, there is a need to explore how academic training and collaborations can be strengthened using teleconferencing and consideration of grants or scholarships to support trainees.
Strengths and Limitations of the Study
This survey is the first continental survey of neurosurgical trainees. The neurosurgical community on the African continent is certainly growing exponentially and there is a need to curate their experiences. In addition, these findings can help identify common challenges and explore avenues to collectively address them. The survey utilized social media and online platforms, and the wide geographic coverage denotes improved telecommunications on the continent. As responses were individualized and anonymized, we believe this gave trainees the opportunity to be more open as opposed to institutional survey opportunities to express themselves freely may have been curtailed.
The study utilized social media and an online survey. The cost and availability of Wi-Fi access is variable within countries and this expense may have been a barrier to some trainees.
This survey was collected when many African countries were in the early phase of the pandemic and may not reflect the evolving practice and experience in the coming months.
Conclusions
This survey highlights the training challenges of African neurosurgery trainees during the COVID-19 pandemic. Although the continent is viewed as being in the early stages of the disease spread, there is a need to mitigate these training challenges around clinical exposure, academic activities, and the support of training with PPE and training on managing COVID-19-positive patients. The financial situation of trainees needs to be borne in mind if any adjustments are made to their training duration and also to be factored in academic activities by regional and international societies. We recommend other surveys to evaluate the long-term impact of COVID-19.
CRediT authorship contribution statement
Jebet Beverly Cheserem: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing - original draft, Visualization, Project administration. Ignatius N. Esene: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing - original draft, Project administration. Muhammad Raji Mahmud: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing - original draft, Visualization, Project administration, Supervision. Kazadi Kalangu: Writing - review & editing, Project administration, Supervision. Samuila Sanoussi: Writing - review & editing, Supervision. Aaron Musara: Writing - review & editing, Supervision. Nasser M.F. El-Ghandour: Writing - review & editing. Graham Fieggen: Methodology, Investigation, Data curation, Writing - review & editing, Project administration, Supervision. Mahmood Qureshi: Methodology, Investigation, Data curation, Writing - review & editing, Project administration, Supervision.
Acknowledgments
The authors thank the Young African Neurosurgeons Forum (Young CAANS). African.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Coronavirus Disease 2019 (COVID-19)–Africa CDC [Internet] https://africacdc.org/covid-19/ Available at:
- 2.Ademuyiwa A.O., Bekele A., Berhea A.B., et al. COVID-19 preparedness within the surgical, obstetric and anesthetic ecosystem in sub Saharan Africa. Ann Surg. 2020;272:e9–e13. doi: 10.1097/SLA.0000000000003964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park K.B., Johnson W.D., Dempsey R.J. Global neurosurgery: the unmet need. World Neurosurg. 2016;88:32–35. doi: 10.1016/j.wneu.2015.12.048. [DOI] [PubMed] [Google Scholar]
- 4.Park K.B., Kanmounye U.S., Lartigue J.W. Global neurosurgery in the time of COVID-19. Neurospine. 2020;17:348–350. doi: 10.14245/ns.2040246.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahmud M.R., Cheserem B., Esene I.N. The impact of COVID-19 on neurosurgical services in Africa. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.11.004. accessed November 25, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coronavirus (COVID-19) events as they happen [Internet] https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen Available at:
- 7.Germanò A., Raffa G., Angileri F.F., Cardali S.M., Tomasello F. Coronavirus disease 2019 (COVID-19) and neurosurgery: literature and neurosurgical societies recommendations update. World Neurosurg. 2020;139:e812–e817. doi: 10.1016/j.wneu.2020.04.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grelat M., Pommier B., Portet S., et al. COVID-19 patients and surgery: guidelines and checklist proposal. World Neurosurg. 2020;139:e769–e773. doi: 10.1016/j.wneu.2020.04.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta P., Muthukumar N., Rajshekhar V., et al. Neurosurgery and neurology practices during the novel COVID-19 pandemic: a consensus statement from India. Neurol India. 2020;68(2):246–254. doi: 10.4103/0028-3886.283130. [DOI] [PubMed] [Google Scholar]
- 10.Scullen T., Mathkour M., Maulucci C.M., Dumont A.S., Bui C.J., Keen J.R. Impact of the COVID-19 pandemic on neurosurgical residency training in New Orleans. World Neurosurg. 2020;139:718–719. doi: 10.1016/j.wneu.2020.04.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bambakidis N.C., Tomei K.L. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020:1–2. doi: 10.3171/2020.3.JNS20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee Z.D., Chyi Yeu D.L., Ang B.T., Ng W.H., Seow W.T. Editorial. COVID-19 and its impact on neurosurgery: our early experience in Singapore. J Neurosurg. 2020:1–2. doi: 10.3171/2020.4.JNS201026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.José Antonio S.S., Tito P., Marcelo Z., et al. Early report on the impact of COVID-19 outbreak in neurosurgical practice among members of the Latin American federation of neurosurgical societies. World Neurosurg. 2020;140:e195–e202. doi: 10.1016/j.wneu.2020.04.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ozoner B., Gungor A., Hasanov T., Toktas Z.O., Kilic T. Neurosurgery practice during coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;140:198–207. doi: 10.1016/j.wneu.2020.05.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 16.Daggubati L.C., Eichberg D.G., Ivan M.E., et al. Telemedicine for outpatient neurosurgical oncology care: lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859–e863. doi: 10.1016/j.wneu.2020.05.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blue R., Yang A., Zhou C., et al. Telemedicine in the era of COVID-19: a neurosurgical perspective. World Neurosurg. 2020;139:549–557. doi: 10.1016/j.wneu.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Szmuda T., Ali S., Słoniewski P., NSurg4WL group Telemedicine in neurosurgery during the novel coronavirus (COVID-19) pandemic. Neurol Neurochir Pol. 2020;54:207–208. doi: 10.5603/PJNNS.a2020.0038. [DOI] [PubMed] [Google Scholar]
- 19.Kanmounye U.S., Esene I.N. Letter to the Editor “COVID-19 and neurosurgical education in Africa: making lemonade from lemons”. World Neurosurg. 2020;139:732–733. doi: 10.1016/j.wneu.2020.05.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stienen M.N., Schaller K., Cock H., Lisnic V., Regli L., Thomson S. eLearning resources to supplement postgraduate neurosurgery training. Acta Neurochir (Wien) 2017;159:325–337. doi: 10.1007/s00701-016-3042-7. [DOI] [PubMed] [Google Scholar]
- 21.Tagaytayan R., Kelemen A., Sik-Lanyi C. Augmented reality in neurosurgery. Arch Med Sci. 2018;14:572–578. doi: 10.5114/aoms.2016.58690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis M.C., Can D.D., Pindrik J., Rocque B.G., Johnston J.M. Virtual interactive presence in global surgical education: international collaboration through augmented reality. World Neurosurg. 2016;86:103–111. doi: 10.1016/j.wneu.2015.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niazkar H.R., Zibaee B., Nasimi A., Bahri N. The neurological manifestations of COVID-19: a review article. Neurol Sci. 2020;1:1–5. doi: 10.1007/s10072-020-04486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chersich M.F., Gray G., Fairlie L., et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Global Health. 2020;16 doi: 10.1186/s12992-020-00574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang M., Zhou M., Tang F., et al. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect. 2020;105:183–187. doi: 10.1016/j.jhin.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen W., Huang Y. To protect healthcare workers better, to save more lives. Anesth Analg. 2020;131:97–101. doi: 10.1213/ANE.0000000000004834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chirico F., Nucera G., Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020;1 doi: 10.1017/ice.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferioli M., Cisternino C., Leo V., Pisani L., Palange P., Nava S. Protecting healthcare workers from sars-cov-2 infection: practical indications. Eur Respir Rev. 2020;29 doi: 10.1183/16000617.0068-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bell D.M. Occupational risk of human immunodeficiency virus infection in healthcare workers: an overview. Am J Med. 1997;102:9–15. doi: 10.1016/s0002-9343(97)89441-7. [DOI] [PubMed] [Google Scholar]
- 30.von Delft A., Dramowski A., Khosa C., et al. Why healthcare workers are sick of TB. Int J Infect Dis. 2015;32:147–151. doi: 10.1016/j.ijid.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 31.Kilmarx P.H., Clarke K.R., Dietz P.M., et al. Ebola virus disease in health care workers—Sierra Leone, 2014. Morb Mortal Wkly Rep. 2014;63:1168–1171. [PMC free article] [PubMed] [Google Scholar]
- 32.Kapata N., Ihekweazu C., Ntoumi F., et al. Is Africa prepared for tackling the COVID-19 (SARS-CoV-2) epidemic. Lessons from past outbreaks, ongoing pan-African public health efforts, and implications for the future. Int J Infect Dis. 2020;93:233–236. doi: 10.1016/j.ijid.2020.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Htun H.L., Lim D.W., Kyaw W.M., et al. Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis. 2020;71:1947–1952. doi: 10.1093/cid/ciaa468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blake H., Bermingham F., Johnson G., Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int J Environ Res Public Health. 2020;17:2997. doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elbay R.Y., Kurtulmuş A., Arpacıoğlu S., Karadere E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhagavathula A., Aldhaleei W.A., Rahmani J.R., Mahabadi M.A., Bandari D.K. Novel coronavirus (COVID-19) knowledge and perceptions: a survey of healthcare workers. JMIR Public Heal Surveill. 2020;60:e19160. doi: 10.2196/19160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Punchak M., Mukhopadhyay S., Sachdev S., et al. Neurosurgical care: availability and access in low-income and middle-income countries. World Neurosurg. 2018;112:e240–e254. doi: 10.1016/j.wneu.2018.01.029. [DOI] [PubMed] [Google Scholar]
- 39.Fuller A., Tran T., Muhumuza M., Haglund M.M. Building neurosurgical capacity in low and middle income countries. eNeurologicalSci. 2016;3:1–6. doi: 10.1016/j.ensci.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sader E., Yee P., Hodaie M. Barriers to neurosurgical training in sub-Saharan Africa: the need for a phased approach to global surgery efforts to improve neurosurgical care. World Neurosurg. 2017;98:397–402. doi: 10.1016/j.wneu.2016.07.098. [DOI] [PubMed] [Google Scholar]
- 41.Prause J., Dooley D., Huh J. Income volatility and psychological depression. Am J Community Psychol. 2009;43:57–70. doi: 10.1007/s10464-008-9219-3. [DOI] [PubMed] [Google Scholar]