Dear Editor,
A recent study by Kunutsor and Laukkanen, published in the Journal of Infection, described a possible link between high levels of liver injury markers at admission and the severity and death of Coronavirus disease 2019 (COVID-19)1. This study suggests that underlying liver disease may be a risk factor for COVID-19. Cirrhosis patients, especially those with clinically significant portal hypertension (CSPH), are in immunocompromised status and at higher risk of SARS-CoV-2 infection and mortality2. However, the information of clinical characteristics and outcomes in these patients with COVID-19 is scarce. Furthermore, there is not much experience in managing COVID-19 in cirrhosis patients. Here, we described the clinical, laboratory, and radiological characteristics, treatments and outcomes of 17 COVID-19 patients with cirrhosis.
We retrospectively analyzed 17 cirrhosis patients diagnosed with COVID-19 from February 1, 2020 to Match 15, 2020 in Wuhan Tongji hospital, Wuhan Jin Yin-tan hospital and Wuhan Puai hospital. We collect hospital admissions, laboratory tests, radiological tests, treatments and outcomes from clinical electronic medical records. All patients had a history of cirrhosis, confirmed by imaging and liver biopsy results. CSPH was confirmed by hepatic venous pressure gradient (HVPG) > 10 mmHg. COVID-19 was confirmed by detecting nucleic acids of SARS-CoV-2 in throatswab specimens. Severe COVID-19 was defined according to previous study3. Acute-on-chronic liver failure (ACLF) was defined according to guidelines4. Wilcoxon signed rank test was used for continuous variables, and the Chi-square or Fisher's exact test was used for categorical variables.
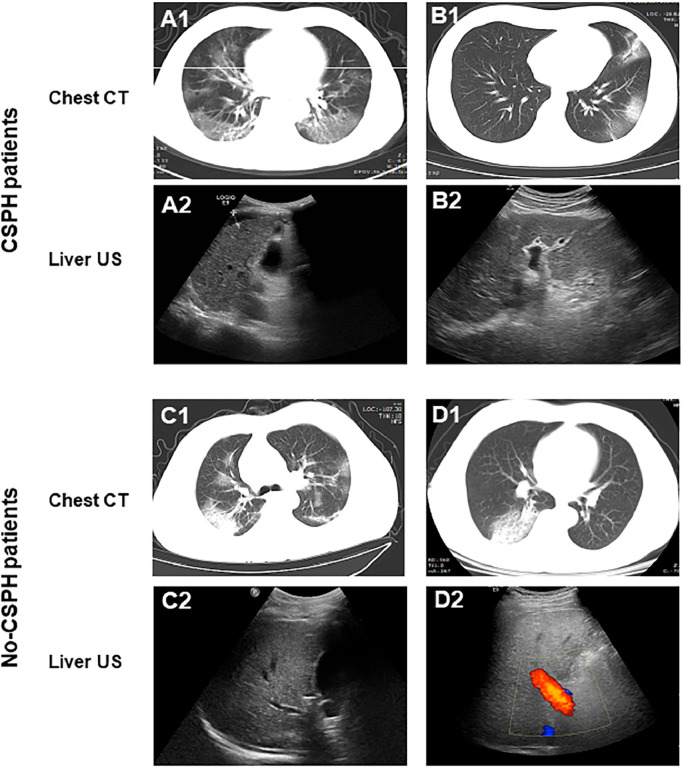
Our study cohort included 17 cirrhosis patients with COVID-19 (6 CSPH patients and 11 non-CSPH patients), with a median age of 56 years (interquartile range, 51 to 64). Most patients had a history of HBV/HCV infection (14/17, 82.4%), and were in the state of Child-Pugh classification A (15/17, 88.2%) (Table 1 ). Chest CT showed typical COVID-19 pneumonia features5 in 17 patients (Fig. 1 ) and the main symptoms of COVID-19 in these patients were fever and cough, with a mean incubation period of 5 days (interquartile range, 4–6 days). There were no significant differences in age, etiology and stage of cirrhosis, symptoms and incubation period of COVID-19 between CSPH and non-CSPH patients.
Table 1.
Clinical characteristics of cirrhosis patients with COVID-19.
| Variable, n (%) or median (IQR) | Normal range | Overall (n = 17) | CSPH (n = 6) | Non-CSPH (n = 11) | p value |
|---|---|---|---|---|---|
| Age | – | 56 (51–64) | 59 (50–61) | 57 (53–65) | 0.5820 |
| Male | – | 13 (76.5) | 5 (83.3) | 8 (72.7) | 0.4927 |
| Etiology of liver disease | |||||
| HBV | – | 12 (70.6) | 5 (83.3) | 7 (63.6) | 0.3607 |
| HCV | – | 2 (11.8) | 1 (16.7) | 1 (9.1) | |
| Others | – | 3 (17.6) | 0 (0) | 3 (27.3) | |
| Incubation period, days | 2–7 | 5 (4–6) | 5 (4–7) | 5 (3–6) | 0.4718 |
| Child-pugh classification | |||||
| A | – | 15 (88.2) | 4 (66.7) | 11 (100) | 0.1252 |
| B | – | 1 (5.9) | 1 (16.7) | 0 (0) | |
| C | – | 1 (5.9) | 1 (16.7) | 0 (0) | |
| Presenting symptoms | |||||
| Fever | – | 13 (76.5) | 5 (83.3) | 8 (72.7) | 0.6223 |
| Short of breath | – | 4 (23.5) | 2 (33.3) | 2 (18.2) | 0.4816 |
| Cough | – | 11 (64.7) | 4 (66.7) | 7 (63.6) | 0.9006 |
| Fatigue | – | 6 (35.3) | 2 (33.3) | 4 (36.4) | 0.1249 |
| Diarrhea | – | 4 (23.5) | 1 (16.7) | 3 (27.3) | 0.6223 |
| Headache | – | 2 (11.8) | 1 (16.7) | 1 (9.1) | 0.6431 |
| Complications | |||||
| EGVB | – | 1 (5.9) | 1 (16.7) | 0 (0) | 0.1626 |
| Cardiac injury | – | 2 (11.8) | 1 (16.7) | 1 (9.1) | 0.6431 |
| ARDS | – | 5 (29.4) | 3 (50.0) | 2 (18.2) | 0.1688 |
| ACLF | – | 2 (11.8) | 2 (33.3) | 0 (0) | 0.1103 |
| Acute kidney injury | – | 8 (47.1) | 4 (66.7) | 4 (36.4) | 0.2316 |
| Shock | – | 2 (11.8) | 1 (16.7) | 1 (9.1) | 0.6431 |
| Laboratory findings | |||||
| WBC (× 109/L) | 3.5–9.5 | 4.5 (3.69–5.76) | 5.0 (3.3–6.0) | 4.5 (3.7–5.5) | 0.3988 |
| Lymphocyte count, × 109/L | 1.10–3.20 | 0.72 (0.62–1.12) | 0.61 (0.47–0.9) | 0.86 (0.68–1.28) | 0.0487 |
| Neutrophil count, × 109/L | 1.80–6.30 | 3.29 (2.19–4.28) | 3.78 (1.88–4.54) | 3.14 (2.49–4.17) | 0.2834 |
| Platelet count, × 109/L | 125.0–350.0 | 98 (68–136) | 60.5 (51.2–67.5) | 133 (105–145) | <0.0001 |
| Hemoglobin, g/L | 130–175 | 121 (109–138) | 110 (101–119) | 129 (112–140) | 0.0154 |
| ALT, U/L | 7.0–40.0 | 47 (29–72) | 65.5 (50–78) | 37 (25–58) | 0.2158 |
| AST, U/L | 13.0–35.0 | 47 (41–91) | 76.5 (49–117) | 47 (38–75) | 0.1375 |
| T-BIL, μmol/L | 0–21.0 | 14.3 (10.4–32.2) | 37.2 (22.2–52.9) | 10.8 (10.1–16.7) | 0.0347 |
| Albumin, g/L | 40.0–55.0 | 37.5 (34.8–39.5) | 36.2 (34.0–39.1) | 37.6 (34.8–39.3) | 0.2158 |
| Creatinine, μmol/L | 41.0–73.0 | 77.0 (60.0–88.0) | 71.5 (61.3–85.5) | 77.0 (62.0–93.0) | 0.2640 |
| BUN, mmol/L | 2.6–7.5 | 7.2 (5.6–8.3) | 7.2 (5.9–8.0) | 7.8 (5.7–9.5) | 0.3061 |
| PT, s | 11.5–14.5 | 14.5 (13.7–15.9) | 15.9 (15.6–16.2) | 13.8 (12.8–14.6) | 0.0090 |
| APTT, s | 29.0–42.0 | 42.0 (34.7–44.9) | 45.9 (43.5–48.9) | 39.3 (34.2–42.6) | 0.0329 |
| INR | 0.8–1.2 | 1.1 (1.03–1.2) | 1.24 (1.19–1.27) | 1.03 (1.0–1.08) | 0.0831 |
| D-dimer, mg/L | 0–1.5 | 1.4 (0.6–2.6) | 2.7 (1.7–9.6) | 0.6 (0.3–1.3) | 0.5657 |
| PCT (ng/mL) | 0.02–0.05 | 0.06 (0.04–0.13) | 0.87 (0.09–1.87) | 0.06 (0.04–0.06) | 0.0791 |
| CRP (mg/L) | 0–5.0 | 29.3 (7.3–45.4) | 21.3 (5.3–24.2) | 39.1 (15.8–48.9) | 0.4183 |
| Ferritin, ng/mL | 4.63–204 | 915 (433–1353) | 915 (687–1144) | 567 (418–1316) | 0.2583 |
| Treatments | |||||
| Oxygen support | – | 6 (35.3) | 4 (66.7) | 2 (18.2) | 0.0456 |
| Mechanical ventilation | – | 2 (11.8) | 1 (16.7) | 1 (9.1) | 0.6431 |
| Antiviral treatment | – | 15 (88.2) | 6 (100.0) | 9 (81.8) | 0.2662 |
| Antimicrobial treatment | – | 13 (76.5) | 4 (66.7) | 9 (81.8) | 0.4816 |
| Hepatoprotective agents | – | 11 (64.7) | 6 (100.0) | 5 (45.4) | 0.0245 |
| Glucocorticoids | – | 1 (5.9) | 0 (0.0) | 1 (9.1) | 0.1628 |
| Endoscopic sclerotherapy | – | 1 (5.9) | 1 (16.7) | 0 (0) | 0.1626 |
| Severity | |||||
| Mild | – | 11 (64.7) | 2 (33.3) | 9 (81.8) | 0.0456 |
| Severe | – | 6 (35.3) | 4 (66.7) | 2 (18.2) | |
| Outcome | |||||
| ICU admission | – | 3 (17.6) | 2 (33.3) | 1 (9.1) | 0.2102 |
| Dead | – | 3 (17.6) | 2 (33.3) | 1 (9.1) | 0.2102 |
CSPH=Clinically significant portal hypertension, HBV=hepatitis B virus, HCV=Hepatitis C virus, EGVB=Esophageal gastric variceal bleeding, ARDS=Acute respiratory distress syndrome, ACLF=Acute-on-chronic liver failure, WBC=White blood cells, ALT=Alanine aminotransferase, AST=Aspartate aminotransferase, T-BIL=Total bilirubin, BUN=Blood urea nitrogen, PT=Prothrombin time, APTT=Activated partial thromboplastin time, INR=International standard ratio, PCT=Procalcitonin, CRP=C-reactive protein, ICU= Intensive care unit.
Fig. 1.
Typical pulmonary CT and hepatic ultrasound in patients with CSPH and non-CSPH patients. CSPH, Clinically significant portal hypertension.
In laboratory tests, abnormalities were observed in indicators related to cirrhosis and infection, such as platelet count, hemoglobin, coagulation function, procalcitonin, C-reactive protein, and ferritin. For example, 14 had hypoproteinemia, 12 patients had lymphopenia, and 9 patients had thrombocytopenia. Meanwhile, compared with non-CSPH patients, patients with CSPH showed lower lymphocyte, platelet and hemoglobin, higher total bilirubin, longer prothrombin time and activated partial thromboplastin time (Wilcoxon signed rank test, P < 0.05). During the course of COVID-19, the most frequent complications were abnormal liver function (64.7%), kidney injury (47.1%), and ARDS (29.4%), and all CSPH patients showed abnormal liver function. Notably, one CSPH patient developed esophageal gastric variceal bleeding (EGVB), which is one of the most serious complications. In addition, 66.7% (4/6) of CSPH patients were severe cases, compared with 18.2% (2/11) of non-CSPH patients (P = 0.025).
In the course of treatment, antiviral (88.2%), antimicrobial (76.5%), hepatoprotective (64.7%) and oxygen (35.3%) therapy were the most commonly used, and CSPH patients had a higher proportion of hepatoprotective therapy (6/6 vs 5/11, P = 0.025) and oxygen therapy (4/6 vs 2/11, P = 0.046) than non-CSPH patients. Also, the endoscopic sclerotherapy was applied to deal with EGVB. In addition, 3 patients (17.6%) were admitted to the intensive care unit (ICU), and died.
Many researches have shown that the liver is a target organ for SARS-CoV-2, and some patients with COVID-19 suffered from liver injury, although this may not lead to serious clinical consequences6. However, for patients with pre-existing liver disease, there may be a greater risk after SARS-CoV-2 infection. For example, Ji et al. reported that non-alcoholic fatty liver disease (NAFLD) patients with COVID-19 had a higher rate of disease progression7.
Cirrhosis patients tend to be at high risk of COVID-19 due to their specific characteristics8. On the blood test findings, many indicators were abnormal, which may be caused by the characteristics of cirrhosis, and these may be markers of the severity of COVID-19, such as decreased platelets and lymphocytes9 , 10, which were more obvious in CSPH patients. Consistent with these findings, 35.3% of COVID-19 patients with cirrhosis in our study were severe illness, and the proportion of CSPH patients was 64.7%, suggesting that cirrhosis, especially CSPH, may play an important role in the progression of COVID-19. However, it is encouraging to note that the mortality of in this study was not high, possibly because our center has rich experience in the treatment of cirrhosis and CSPH, as well as in the treatment of other organs in conjunction with the multidisciplinary team. When treating COVID 19 patients with cirrhosis, other complications such as EGVB, heart damage, and kidney damage should also be noted in the control of pulmonary symptoms.
However, only 17 cirrhosis patients with COVID-19 were included in this study, due to the low overall incidence of cirrhosis patients. More cases and comparative studies should be analyzed for more robust results. Nonetheless, our results suggest that cirrhosis, especially CSPH, may aggravate the severity of COVID-19.
Declaration of Competing Interest
The authors disclose no conflicts.
Acknowledgments
Author contributions
XC and ZZ conceived this study. XL, GJ, ZZ, BZ and WZ treated the patients. ZZ and FL made a statistical analysis and wrote the manuscript.
Acknowledgement
This retrospective study was authorized by the Ethic Committee of Wuhan Tongji Hospital.
Funding
This study was funded by the State Key Project on Infection Disease of China (No. 2018ZX10723204–003).
References
- 1.Kunutsor S.K., Laukkanen J.A. Markers of liver injury and clinical outcomes in COVID-19 patients: a systematic review and meta-analysis. J Infect. 2020 doi: 10.1016/j.jinf.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernardi M., Moreau R., Angeli P., Schnabl B., Arroyo V. Mechanisms of decompensation and organ failure in cirrhosis: from peripheral arterial vasodilation to systemic inflammation hypothesis. J Hepatol. 2015;63(5):1272–1284. doi: 10.1016/j.jhep.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Liu F., Long X., Zhang B., Zhang W., Chen X., Zhang Z. ACE2 expression in pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarin S.K., Choudhury A., Sharma M.K., Maiwall R., Al M.M., Rahman S. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int. 2019;13(4):353–390. doi: 10.1007/s12072-019-09946-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology2020200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed]
- 6.Zhang Y., Zheng L., Liu L., Zhao M., Xiao J., Zhao Q. Liver impairment in COVID-19 patients: a retrospective analysis of 115 cases from a single center in Wuhan city. China. Liver Int. 2020 doi: 10.1111/liv.14455. [DOI] [PubMed] [Google Scholar]
- 7.Ji D., Qin E., Xu J., Zhang D., Cheng G., Wang Y. Implication of non-alcoholic fatty liver diseases (NAFLD) in patients with COVID-19: a preliminary analysis. J Hepatol. 2020 doi: 10.1016/j.jhep.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riordan S.M., Williams R. The intestinal flora and bacterial infection in cirrhosis. J Hepatol. 2006;45(5):744–757. doi: 10.1016/j.jhep.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Lippi G., Plebani M., Henry B.M. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.Q. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5(1):33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]