Dear Sir,
The Corona Virus Disease 2019 (COVID) pandemic poses unique challenges in the provision of inpatient psychiatric care due to difficulty in adhering to respiratory etiquette, and physical distancing norms by patients. In order to reduce the risk and mitigate the COVID outbreak in the closed wards at our tertiary care psychiatry facility, preventive measures were put into place within two weeks of the first COVID case being reported in the city of Bengaluru. Despite following a universal screening protocol, male closed wards had a COVID outbreak. In this paper, we provide an experiential account of risk mitigation strategies after an outbreak, and continuing challenges during the COVID pandemic in the National Institute of Mental Health And Neuro Sciences (NIMHANS) which is a tertiary neuropsychiatric care Institute located in South India.
The psychiatric inpatient division of the hospital has 545 beds: 120 of which (about 20 %) are earmarked for difficult to manage patients as well as those with social/medico-legal issues (homeless persons with mental illness, those without adequate family/social support or with forensic issues). The 120 beds are distributed across two closed wards (male/female). Prior to COVID-19, 47 of the PMIs (25 males, 22 females) were long-stay patients who had been under the care of the institution for a mean period of 15.1 years (range 2–55 years), as no family member could be identified for a safe discharge. The mean age of these patients was 48.2 (24–79) years, all of them had severe mental illness (psychosis/mood disorders), with associated cardio-metabolic comorbidities (40.4 %) and neuroendocrine disorders (23.4 %). Given this context, it was deemed that the closed wards represented a high-risk area for COVID-19 incidence and spread. The higher risk stemmed from the possibility of a single infection rapidly turning into a cluster outbreak within the closed wards. Given the potential risk of poor outcomes in the event of an outbreak, the need for a proactive response was considered. The Department of Psychiatry, in liaison with the Hospital Infection Control Committee (HICC) of the Institute, developed a preparedness and contingency plans and adhered to the standard protocol provided by the Ministry of Health and Family Welfare (MoHFW), Government of India (GoI), and Government of Karnataka (“Health & Family Welfare, ” n.d., “Indian Council of Medical Research, New Delhi, ” n.d., “MoHFW | Home, ” n.d.).
Despite the all precautions, four health care workers (HCWs) developed COVID-19 symptoms and tested positive for COVID-19 infection at different time points in the three months from April 2020-June 2020. Subsequent to a HCW working in the male ward testing positive, a total of 10 male psychiatric in-patients developed COVID-19 following exposure to HCW. The specific steps taken during the month following the incident are described below.
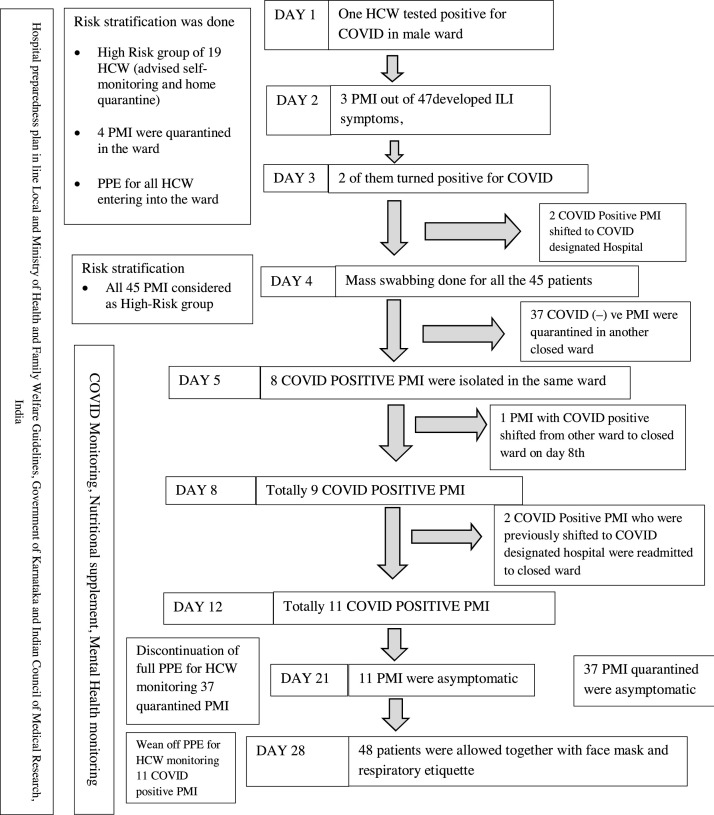
Fig. 1 shows details of the chain of events and continuity of care during the COVID-19 outbreak in the Male Ward. One HCW in the male closed ward tested positive for COVID-19. The ward was declared a containment zone. The risk stratification of all patients and staff was done and high-risk contacts were isolated. On the 2nd day of exposure, 3 of the inpatients developed Influenza-Like Illness (ILI) symptoms. They were immediately swabbed and 2 of them who tested positive were referred to the nearby COVID-19 designated care centre.As two patients had turned positive, a further reappraisal of risk stratification was done. In liaison with the HICC, it was deemed that all the other 45 patients had a high risk of exposure to the positive patients. The ward was then put into total lockdown. Patients swabbing was done on the 5th-day of exposure to the primary case (HCW). Out of the 45 inmates, 8 more tested positive and were isolated in the same ward rather than referral to the COVID designated Hospital. This was because of the rapidly changing COVID hospital policies for admission of COVID-19 positive patients. The remaining 37 patients who were tested negative were shifted and quarantined in an adjacent ward and monitored for COVID-19. Another patient admitted into one of the open inpatient psychiatry wards who had turned positive and did not have a family was also shifted to the male closed ward for isolation, with the remaining 8 patients. Two of the COVID- positive patients who had been previously sent to the general hospital for COVID care centre returned to the male closed ward after stabilisation and were readmitted. These two patients were separated from the other COVID positive patients in the same facility. In the other ward, 9 out of 37 high risk exposed inmates developed ILI symptoms and were housed in separate spaces. However, all of them tested negative.
Fig. 1.
Chain of events during COVID-19 outbreak in the male closed ward.
All the HCWs and treating team underwent a telemedicine-based training programme for the medical management of COVID-19. Our team was also guided by the specialist team from the COVID-19 designated hospital during the care of our patients in the ward. The HCWs in this ward had de-escalation from full PPE to face shields with N95 masks at the end of three weeks of the primary outbreak. At the end of the fourth week, the outbreak was declared contained and in-patient activities resumed with the usual COVID-precautions. Subsequent to the HCW working in the male and female ward testing positive, other HCWs working in the ward were either advised quarantine (in case of high-risk exposure) or continuation of the duty with self-monitoring (low-risk exposure) based on risk stratification. Among the HCWs exposed to the primary case, one tested positive for COVID-19 on the fifth day post-exposure. The 2 COVID-19 positive HCWs recovered with self-isolation and periodic monitoring.
Although HCWs were provided appropriate COVID preventive equipment at work, they developed ILI symptoms and tested positive for infection. It may be conceded that precautionary measures by HCWs at and near their residences lapsed, thus community transmission may have found its way into this hospital population.. Even though HCWs were asked to report for COVID symptoms at the workplace, the resentment may have been due to COVID stigma and related reasons. In order to mitigate the above issues, small-group online sessions with different cadres of HCWs by HICC and mental health education team was reinforced in addition to the regular orientation and training session which were organized during COVID preparedness of the institute. The sessions were focussed on self-monitoring, the importance of screening and early risk stratification. The Institute emphasised on existing policies on self-quarantining in case of the high risk of exposure and new-onset COVID /ILI symptoms and initiated COVID Rapid Antigen Testing services.
The focus of creating a mitigation plan for the scenario when clustering or outbreak of coronavirus disease (COVID-19) in a healthcare facility has to be contained, usually is to suit and manage according to the dynamic situations as and when they arise, by putting together a standard operating procedure (SOP) that focuses on upgradation and customization of the existing protocols, which means the measures are drafted and implemented to reduce the morbidity and spread. COVID-19 preparedness and mitigation plan are usually put in place in an extreme situation where redefining working patterns of HCWs, categorisation of hospital facilities into different zones, training hospital staff in risk mitigation and containment measures like isolation, quarantine, universal screening, source control and early risk stratification can help to prevent the spread of COVID-19 due to clustering and outbreaks within psychiatric institutions.These measures are practically feasible and can be implemented worldwide in such facilities.
Funding
This research has not received a specific grant from any funding agency in the public, commercial or not- for -profit sectors.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
We convey our sincere thanks to
All the Junior residents, senior residents, faculty members of the Department of Psychiatry and all the in-charge Single Point Of Contact of different psychiatric wards, National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru.
Nursing supervisors, nursing staff and other health care workers, who worked at pavilions 1, 2 and 3, National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru.
References
- Health & Family Welfare [WWW Document], n.d. URL https://karunadu.karnataka.gov.in/hfw/Pages/home.aspx (Accessed 9.5.20).
- Indian Council of Medical Research, New Delhi [WWW Document], n.d. URL https://www.icmr.gov.in/ (Accessed 9.5.20).
- MoHFW | Home [WWW Document], n.d. URL https://www.mohfw.gov.in/ (Accessed 9.5.20).