The Merriam-Webster dictionary defines a pandemic as “an outbreak of a disease that occurs over a wide geographic area and affects an exceptionally high proportion of the population”.1 The world has again become acutely aware of this term because of a disease (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that has dramatically changed our daily behaviors and habits. As of May 30th, 2020, there have been 5,775,043 confirmed cases and 361,220 confirmed deaths in 216 countries.2 There will undoubtedly be lasting effects as a result of the COVID-19 pandemic, although how these lasting effects will impact daily life for the foreseeable future, as we begin to control viral spread and recover, remains uncertain at this time. One hope is that some of the lasting effects resulting from COVID-19 will be positive; we must learn from challenging times and try to make the world a better, healthier, and safer place for all inhabitants.
While certainly different from the current health crisis induced by COVID-19, we have been living with several other significant health conditions that continue to have catastrophic effects on a global scale. In fact, obesity,3 physical inactivity,4 diabetes5 and other noncommunicable diseases (NCDs)6 (e.g., cardiovascular disease, certain forms of cancer, and respiratory disease) have all been characterized as pandemics. Table 1 lists key metrics for each of these conditions according to the World Health Organization (WHO).7., 8., 9., 10., 11., 12., 13. Clearly, the data listed in Table 1 make a strong case for each condition being characterized as a pandemic. These health conditions are also interrelated; for example, physical inactivity increases obesity risk which then increases risk for diabetes and other NCDs.14 , 15 What is worse is that, while we have long recognized aggressively addressing the conditions in Table 1 is of paramount importance, we are making little impact in reversing trends; excess body weight, for example (i.e., obesity), continues to increase on a global scale.16
Table 1.
Major health conditions described as pandemics.
| Condition | Key Global Statistics From the World Health Organization |
|---|---|
| Overweight and obesity |
|
| Physical inactivity |
|
| Diabetes |
|
| Noncommunicable diseases |
|
We have come to the point, based on overwhelming scientific evidence spanning several decades, that the importance and value of healthy living (HL) (i.e., physical activity, good nutrition, appropriate body weight and not smoking) in preventing (primary prevention) and treating (secondary prevention) the conditions listed in Table 1 is beyond dispute.17., 18., 19., 20., 21., 22. In fact, HL is the primary medicine to treat the obesity, physical inactivity/sedentarism, diabetes and NCD pandemics.17 , 23 Moreover, and critically important to the current perspective, any movement away from unhealthy behaviors towards HL has significant health benefits. Moving from no physical activity to two 30-minute walks per week or replacing processed foods with two servings of fruits and vegetables per day, while not meeting ideal goals, significantly improves health outcomes.17., 18., 19. , 22 For too long we have created a false and, for a large proportion of the population, unattainable all or nothing view of HL behaviors. If approached from the perspective that some HL behaviors are better than none and more is even better, we have a renewed opportunity to make significant progress in improving global trends in unhealthy lifestyles patterns and the resultant poor health trajectory.
As data from COVID-19 continues to evolve rapidly, one pattern is becoming clear - the presence of preexisting medical conditions, such as obesity, diabetes, hypertension and cardiovascular and respiratory diseases, significantly increase the risk of poor outcomes due to the viral infection.24., 25., 26., 27. Again, many of these preexisting medical conditions have also been described as pandemics and are listed in Table 1. Publications regarding the troubling interrelationships between COVID-19 and pre-existing medical conditions are already emerging. For instance, Dietz and Santos25 discussed the increased hospitalization and mortality risk with H1N1 influenza infection in patients who are obese or severely obese, citing the impact significant excess body mass has on pulmonary function as one of the reasons for this association. Given the impact of COVID-19 on the pulmonary system as a primary manifestation and reason for hospitalization, concerns over the increased health risks for individuals who are obese is certainly justified. Moreover, individuals who are obese Fig. 1 present with other detrimental alterations relevant to the COVID-19 pandemic including: 1) A baseline increase in systemic inflammation that, when a viral infection is present, blunts macrophage activation and pro-inflammatory cytokine production with macrophage stimulation, contributing to compromised immune function; 2) increased viral shedding time (i.e., contagious for a longer period than normal weight individuals); 3) the potential for more virulent viral strains induced by the obese microenvironment; and 4) a positive correlation between body mass index and viral spread through exhaled breath.24 These concerns are exponentially magnified given the global prevalence of excess body mass and obesity (Table 1). From the perspective of multimorbidity, Muniyappa and Gubbi28 discussed COVID-19 in the context of patients with diabetes, drawing attention to the hypertension-obesity-diabetes triad that is common and the severe health risks (i.e., hospital admission, acute respiratory distress syndrome, mechanical ventilation, or death) with SARS-CoV-2 infection when an individual expresses this phenotype. Moreover, while the independent contribution of increased plasma glucose on increased risk following SARS-CoV-2 infection is unclear at this point, it has been shown to be a predictor of morbidity and mortality in those infected with SARS.29 In recently reported findings from Wuhan China, Chen et al27 found that older patients hospitalized with SARS-CoV-2 infection had a higher prevalence of comorbidities, greater symptom severity, and a higher likelihood of multi-organ involvement and mortality compared to younger patients. It has recently been estimated that ≈33% of the global population are affected by multimorbidity, particularly in those individuals who are 65 years or older.30 In a recent CDC Monthly and Mortality Weekly Report,26 the percentage of patients with SARS-CoV-2 infection and at least one pre-existing medical condition that required intensive care unit (ICU) admission (358 of 457, 78%) or hospitalization without ICU admission (732 of 1037, 71%) was significantly higher compared to those who were not hospitalized (1388 of 5143, 27%). Diabetes, as well as cardiovascular and chronic respiratory diseases, was the most reported pre-existing medical conditions. In >5000 patients admitted with SARS-CoV-2 infection to 12 New York (New York City, Long Island, and Westchester County) hospitals, Richardson et al31 reported >90% had a pre-existing medical condition while 88% had two or more; the most common pre-existing conditions were hypertension (≈57%), obesity (≈42%), and diabetes (≈34%). These trends are disturbing in the context of the COVID-19 pandemic given the prevalence of the pre-existing health conditions listed in Table 1, indicating a large percentage of the global population present with a baseline health status that substantially increases the risk of hospitalization and poor health outcomes with SARS-CoV-2 infection.
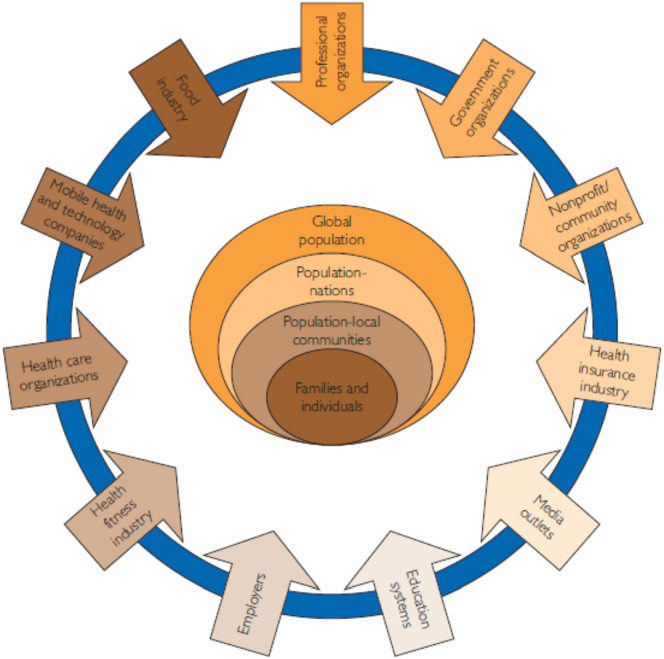
Fig 1.
Conceptual model for a comprehensive approach to healthy lifestyle promotion, education and interventions.
With permission: Arena, R., et al. Healthy lifestyle interventions to combat noncommunicable disease-a novel nonhierarchical connectivity model for key stakeholders: a policy statement from the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine. Mayo Clin Proc, 2015. 90(8): p. 1082–103.
Conversely, there is strong evidence base that indicates high cardiorespiratory fitness (CRF) as well as regular physical activity and a healthy diet improve immune function, affording protection against viral infections.32., 33., 34., 35. The COVID-19 pandemic, which has precipitated widespread shelter in place and social distancing policies, has also caused great concern regarding physical activity and exercise patterns.36., 37., 38., 39. The world was already largely physically inactive and sedentary pre COVID-19 and trends were not improving.36 A reasonable question post-COVID-19 becomes will these trends in physical inactivity and sedentarism further accelerate, leading to a greater prevalence of the obesity, diabetes and NCD pandemics in the years to come? Initial evidence is emerging that indicates the answer to the first part of this question is yes. Zhang et al40 recently reported a significant reduction in physical activity and a significant increase in screen time during the COVID-19 pandemic in >2400 children and adolescents in Shanghai, China. In >3000 adults in the United States, Meyer et al41 found that, in people who were previously active, physical activity was reduced by ≈33% during the COVID-19 pandemic as well as a substantial increase in sedentary time regardless of pre-COVID-19 activity patterns. Decreased physical activity and increased sedentary time were both associated with worsening mental health. Interestingly, Irfan Ahmed42 recently hypothesized that: 1) a measure of CRF, when available, may be valuable in risk stratifying individuals in the context of future viral pandemics; and 2) exercise training may serve a role in “preconditioning” individuals prior to viral infection. Both hypotheses should be investigated thoroughly and, if supported, would further bolster the importance of HL.
Like COVID-19, if we view the conditions listed in Table 1 as pandemics and we simultaneously recognize HL has profound benefits in preventing, mitigating and treating these pandemics, there becomes an opportunity to view a new global path forward for HL medicine. In this context, we would like to introduce the H ealthy L iving for P andem i c E v ent Pr ot ection (HL-PIVOT) network. The Merriam-Webster noun and verb definitions for pivot are “a person, thing, or factor having a major or central role, function, or effect” and “to turn on or as if on a pivot”, respectively.27 We feel these definitions support our choosing of the PIVOT acronym for the proposed new initiative: 1) the COVID-19 pandemic is playing the major role in impacting daily life patterns and how we perceive population health and; 2) this impact warrants turning or pivoting in a different direction with the goal of meaningfully increasing HL behaviors on a global level. The overarching goal of this network is to promote human resilience and quality of life by increasing healthy living behaviors. Table 2 lists areas of focus in knowledge discovery, education, policy, and implementation. We acknowledge that such a broad focus will require the network to consist of members from differing areas of expertise and interests. In this context, the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine jointly published a policy statement in 2015 entitled “Healthy Lifestyle Interventions to Combat Noncommunicable Disease: A Novel Nonhierarchical Connectivity Model for Key Stakeholders”.20 This policy statement took an all hands on deck approach to increase HL initiatives and behaviors. Fig 1 illustrates the central figure from this publication, identifying key stakeholders from multiple sectors who can work collaboratively to promote HL from a population to family/individual level. This policy statement, encouraging collaboration across multiple sectors in innovative ways, serves as a foundational framework for the HL-PIVOT network; any activity that promotes HL falls within the scope of the network. Admittedly, the novelty of HL-PIVOT is not to establish the importance that HL behaviors have on health trajectory; this premise is already beyond dispute. Rather, our hope is that HL-PIVOT becomes one of the important and lasting positive initiatives to emerge from the COVID-19 pandemic. Future goals regarding increasing HL behaviors and reducing the prevalence of unfavorable health conditions listed in Table 1 have been previously established; on our current trajectory we will not meet these goals.28 A change in optics and a new approach for collaboration are primary driving forces for inception of the HL-PIVOT network. Healthy living has previously been described as a polypill that can come in many “shapes and sizes”18 and still have tremendous benefits. Moreover, the HL polypill is an essential medicine for all the pandemics described in this commentary; no other medicine in the world can claim to have the same impact in treating multiple health conditions at the same time. Given the universal nature of HL medicine, working collaboratively, across professions in an unprecedented way, is warranted and perhaps the only way a meaningful impact on global health can be made at this point. Initially, founding HL-PIVOT network members will be encouraged to bring ongoing HL projects/initiatives under the HL-PIVOT umbrella. Subsequently, we intend to expand the HL-PIVOT network and continue to promote/facilitate collaboration and develop projects/initiatives in all areas listed in Table 2. It is our hope that a unified voice, promoting HL on a global scale, will greatly move the field forward and translate to meaningful improvements in HL behaviors and health outcomes.
Table 2.
Major areas of focus for the HL-PIVOT Network.
| Knowledge discovery |
|
| Education |
|
| Policy |
|
| Implementation |
|
Abbreviations: HL-PIVOT, Healthy Living for Pandemic Event Protection.
In conclusion, the COVID-19 pandemic has caused a dramatic shift in how individuals live on a global scale. This change has dramatic implications for lifestyle behaviors (e.g., physical activity and nutrition), of which we will not understand the true lasting impact for some time. The COVID-19 pandemic also has the potential for valuable, long lasting lessons to be learned. Perhaps there is an opportunity to realize that we have been living in a world of invisible pandemics for some time now, specifically the obesity, physical inactivity, diabetes and NCD pandemics. Simultaneously, we are beginning to appreciate the relationship between the COVID-19 pandemic and pandemics that have been existing for years; those with obesity, diabetes or one or more NCD diagnoses who contract SARS-CoV-2 have a significantly higher risk for adverse health events. In this context, increasing HL behaviors across the lifespan, thereby building human resilience, can protect individuals from NCDs as well as a worsening health trajectory because of a viral infection. Now more than ever, HL is of paramount importance. Our hope is that the HL-PIVOT initiative brings this fact to the forefront and facilitates a new global path forward.
Footnotes
There is no conflict of interest of any of the listed authors.
Appendix 1. Founding members of the HL-PIVOT Network
Antonio Abbate, MD, PhD, Virginia Commonwealth University, Richmond, Virginia, USA
Gopala Krishna Alaparthi, PhD, PT, University of Sharjah, United Arab Emirates
Leslie D. Austford, MN, MBA, CMPE, TotalCardiology Research Network, and TotalCardiology™, Calgary, Alberta, Canada
Robert S. Axtell, PhD, Southern Connecticut State University, New Haven, Connecticut, USA
Abraham Samuel Babu, PhD, PT, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, India Dr. Simon L. Bacon, PhD, FTOS, FCCS, FABMR, Concordia University and CIUSSS-NIM, Montreal, Quebec, Canada.
James R. Bagley, PhD, San Francisco State University, San Francisco, California, USA.
Kathy Berra, MSN, NP-BC, FAANP, FPCNA, FAHA, FAAN, The LifeCare Company, Redwood City, California and Stanford University, Menlo Park, California, USA
Jarett D. Berry, MD, UT Southwestern Medical Center, Dallas, TX, USA
Samantha Bond, MS, University of Illinois at Chicago, Chicago, Illinois, USA
Sandra A Billinger, PhD, University of Kansas Medical Center, Kansas City, Kansas, USA
Audrey Borghi-Silva, PhD, PT, Federal University of Sao Carlos, Sao Paulo, Brazil
Harry Brar, POWERbreathe International Ltd, Warwickshire, UK
Patrice Brassard, PhD, Université Laval, Québec, Canada
Peter H. Brubaker PhD, Wake Forest University, Winston Salem, North Carolina, USA
Paolo Brugnoli, CosMed, Inc., Rome, Italy
Marco Brugnoli, CosMed, Inc., Rome, Italy
Tavis S. Campbell, PhD, University of Calgary, Calgary, Alberta, Canada
Salvatore Carbone, PhD, MS, Virginia Commonwealth University, Richmond, Virginia, USA
Kalyana Chakravarthy B, PhD, PT, University of Sharjah, United Arab Emirates Dr. Cabrera-Lazarini, MBA, Monterrey Institute of Technology, Monterrey, Mexico
Paul J. Chase, PhD, Ohio University, Athens, Ohio, USA
Sundeep Chaudhry, MD, MET-TEST, Roswell, Georgia, USA
Jeffrey W Christle, PhD, CEP, Stanford University, Stanford, CA, USA
Andrew J Stewart Coats, Monash University, Melbourne, Australia and University of Warwick, Coventry, United Kingdom
Naama W. Constantini, MD, DFM, FACSM, Heidi Rothberg Sport Medicine Center, Shaare Zedek Medical Center, Jerusalem, Israel
Jeff S. Coombes, PhD, University of Queensland, Brisbane, Queensland, Australia
Andréa Lúcia Gonçalves da Silva, PhD, PT, University of Santa Cruz do Sul, Santa Cruz do Sul, Brazil
Luiz Carlos Soares de Carvalho Junior, PhD, PT, Federal University of Recôncavo of Bahia, Cruz das Almas, Bahia, Brazil
Mildred Vanessa López Cabrera, PhD, Monterrey Institute of Technology, Monterrey, Mexico
Victor Zuniga Dourado, PhD, PT, Federal University of São Paulo, Santos, São Paulo, Brazil
Daniela Bassi Dibai, PhD, PT, Ceuma University, São Luís, Brazil
Snehil Dixit, PhD, PT, King Khalid University, Abha, Saudi Arabia
Victor Zuniga Dourado, PhD, PT, Federal University of São Paulo, Santos, SP, Brazil
Brandon Dykstra, PhD, Taylor University, Upland, Indiana, USA
Patrick Dunn, PhD, American Heart Association and Walden University, Dallas, Texas, USA
Diane Eastabrook, Freelance Journalist, Chicago, Illinois, USA
Barry A. Franklin, PhD, Beaumont Health, Royal Oak, Michigan, USA
Sherry L. Grace, PhD, York University & University Health Network, Toronto, Canada and International Council of Cardiovascular Prevention and Rehabilitation, Markham, Ontario, Canada
Gregory J. Grosicki, PhD, Georgia Southern University (Armstrong Campus), Savannah, Georgia, USA
Solange Guizilini, PhD, PT, Federal University of Sao Paulo, Sao Paulo, Brazil.
Grenita Hall, PhD, University of Illinois at Chicago, Chicago, Illinois, USA
Matthew P. Harber, PhD, Ball State University, Muncie, Indiana, USA
Erik Hayes, PhD, Taylor University, Upland, Indiana, USA
Samuel. A. E. Headley, PhD, FACSM, Springfield College, Springfield, Massachusetts, USA
John P. Heybach, PhD, Altus Academy, Chicago, Illinois, USA
Andrew P. Hills, PhD, University of Tasmania, Tasmania, Australia
Anne E Holland PhD, PT, Monash University and Alfred Health, Melbourne, Australia
Panniyammakal Jeemon, Ph.D, MPH, FESC, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala, India
Richard A Josephson, MS, MD, Case Western Reserve University and University Hospitals of Cleveland, Cleveland, Ohio, USA
Leonard A. Kaminsky, PhD, Ball State University, Muncie, Indiana, USA
Bradley Kendall, PhD, CSCS, Taylor University, Upland, Indiana, USA
Aditya Khetan, MD, McMaster University, Hamilton, Ontario, Canada
Peter Kokkinos, PhD, Rutgers University, New Brunswick, NJ, and Veterans Affairs Medical Center Washington, DC, USA
Deepika R. Laddu, PhD, University of Illinois at Chicago, Chicago, Illinois, USA
Jari Laukkanen, MD, PhD, Institute of Clinical Medicine, University of Eastern Finland, Kuopio, Finland, Dr. Lavoie, Ph.D., FCPA, FABMR, University of Quebec at Montreal, Montreal, Quebec, Canada
Gregory D. Lewis, MD, Massachusetts General Hospital, Boston, Massachusetts, USA
Andrew T. Lovering, PhD, University of Oregon, Eugene, Oregon, USA
Sara Maldonado-Martín, PhD, Department of Physical Education and Sports, University of the Basque Country (UPV/EHU), Basque Country, Spain
Susan Marzolini, RKin, PhD, KITE Research Institute, Toronto Rehabilitation and University Health Network, Cardiovascular Prevention and Rehabilitation Program, Toronto, Canada
Norman Morris, PhD, PT, Griffith University and Metro North Hospital and Health Service, The Prince Charles Hospital, Queensland, Australia
Jonathan Myers, PhD, VA Palo Alto Health Care System and Stanford University, Palo Alto, California, USA
Jagat Narula, MD, PhD, Mount Sinai Heart, New York, New York, USA
Javaid Nauman, PhD, United Arab Emirates University, Al-Ain, UAE. Norwegian University of Science and Technology, Trondheim, Norway
Josef Niebauer, MD, PhD, MBA, Institute of Sports Medicine, Prevention and Rehabilitation, Paracelsus Medical University, Salzburg, Austria
James H. O'Keefe, MD, University of Missouri, Kansas City, Kansas, USA
Silvia Lizett Olivares Olivars, PhD, Monterrey Institute of Technology, Monterrey, Mexico
Francisco B. Ortega, PhD, University of Granada, Granada, Spain and Karolinska Institute, Stockholm, Sweden
Cemal Ozemek, PhD, University of Illinois at Chicago, Chicago, Illinois, USA
Ambarish Pandey, MD, MSCS, University of Texas Southwestern Medical Center
Dallas, Texas, USA
James E. Peterman, PhD, Ball State University, Muncie, Indiana, USA
Shane A. Phillips, PhD, PT, University of Illinois at Chicago, Chicago, Illinois, USA
Dejana Popovic, MD, PhD, Clinic for Cardiology, Clinical Center of Serbia, University of Belgrade, Belgrade, Serbia
Axel Pressler, MD, PhD, FESC, Private Center of Sports Cardiology & Prevention, Munich, Germany
Nicolaas P. Pronk, PhD, MA, HealthPartners Institute, Bloomington, Minnesota, and Harvard TH Chan School of Public Health, Boston, Massachusetts, USA
Chathuranga Ranasinghe MBBS, D.Sp.Med, PhD, Faculty of Medicine, University of Colombo, Colombo, Sri LankaMollie Rose, BS, University of Illinois at Chicago, Chicago, Illinois, USA
Robert Ross, PhD, RKin, Queen's University, Kingston, Ontario, Canada
Michel Silva Reis, PhD, PT, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
Fabrizio Ricci, MD, PhD, FEACVI, G.d'Annunzio University, Chieti, Italy
Daniel S. Rubin, M.D., M.S., University of Chicago, Chicago, Illinois, USA
Ahmad Sabbahi, PT, PhD, University of Illinois at Chicago, Chicago, Illinois, USA and Cairo University, Giza, Egypt
Patrick Savage, MS, University of Vermont Medical Center, Cardiac Rehabilitation Program, South Burlington, Vermont, USA
Richard Severin, PT, DPT, CCS, University of Illinois at Chicago, Chicago, Illinois and Baylor University, Waco, Texas, USA
Dorthe Stensvold, PhD, Norwegian University of Science and Technology, Trondheim, Norway
Lindsey Strieter, MS, University of Illinois at Chicago, Chicago, Illinois, USA
Xing Guo Sun, MD, Beijing Fuwai Hospital National Center for Cardiovascular Diseases, Beijing, China
Renata Trimer, PhD, PT, University of Santa Cruz do Sul, Santa Cruz do Sul, Brazil
Jean-Luc Vachiery, MD, Cliniques Universitaires de Bruxelles-Hôpital, Brussels, Belgium
Laurie P. Whitsel, PhD, Ligonier, Pennsylvania, USA
Mark A. Williams, PhD, Creighton University, Omaha, Nebraska, USA
Ulrik Wisløff, PhD, Norwegian University of Science and Technology, Trondheim, Norway, and School of Human Movement and Nutrition Science, University of Queensland, Queensland, Australia.
References
- 1.Merriam-Webster Definition of pandemic. 2020. https://www.merriam-webster.com/dictionary/pandemic
- 2.World Health Organization Coronavirus disease (COVID-19) pandemic. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [2020]
- 3.Meldrum D.R., Morris M.A., Gambone J.C. Obesity pandemic: causes, consequences, and solutions-but do we have the will? Fertil Steril. 2017;107(4):833–839. doi: 10.1016/j.fertnstert.2017.02.104. [DOI] [PubMed] [Google Scholar]
- 4.Kohl H.W., 3rd, Craig C.L., Lambert E.V., et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380(9838):294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 5.The Lancet The diabetes pandemic. Lancet. 2011;378(9786):99. doi: 10.1016/S0140-6736(11)61068-4. [DOI] [PubMed] [Google Scholar]
- 6.Allen L. Are we facing a noncommunicable disease pandemic? J Epidemiol Glob Health. 2017;7(1):5–9. doi: 10.1016/j.jegh.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Physical inactivity: a global public health problem. 2020. https://www.who.int/dietphysicalactivity/factsheet_inactivity/en/ [2020]
- 8.World Health Organization Noncommunicable diseases. 2020. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 9.World Health Organization Insufficient physical activity. 2020. https://www.who.int/gho/ncd/risk_factors/physical_activity_text/en/
- 10.World Health Organization Global health observatory data: overweight and obesity. 2020. https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en/ [4/17/2020]
- 11.World Health Organization Diabetes. 2020. https://www.who.int/news-room/fact-sheets/detail/diabetes
- 12.World Health Organization Cardiovascular diseases. 2020. https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1
- 13.World Health Organization Overweight and obesity. 2020. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight
- 14.Vidal-Puig A., Enerback S. “Obesity-associated metabolic complications, the second wave of the tsunami” 14th Key Symposium. J Intern Med. 2018;284(5):447–449. doi: 10.1111/joim.12828. [DOI] [PubMed] [Google Scholar]
- 15.Karakurt M., Acar B., Ozeke O., et al. From the obesity tsunami to the diabetes avalanche: primordial prevention of the diabesity-related cardiovascular epidemic by diabeto-cardiologists. Angiology. 2019;70(4):371–373. doi: 10.1177/0003319718808921. [DOI] [PubMed] [Google Scholar]
- 16.The Lancet Public Health Tackling obesity seriously: the time has come. Lancet Public Health. 2018;3(4) doi: 10.1016/S2468-2667(18)30053-7. [DOI] [PubMed] [Google Scholar]
- 17.Sagner M., McNeil A., Puska P., et al. The P4 Health Spectrum - a predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis. 2017;59(5):506–521. doi: 10.1016/j.pcad.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Arena R., Lavie C.J., Guazzi M. Prescribing a healthy lifestyle polypill with high therapeutic efficacy in many shapes and sizes. Am J Lifestyle Med. 2017;11(6):476–478. doi: 10.1177/1559827615619341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arena R., Lavie C.J. Preventing bad and expensive things from happening by taking the healthy living polypill: everyone needs this medicine. Mayo Clin Proc. 2017 doi: 10.1016/j.mayocp.2017.02.005. [S0025-6196(17)30121-0] [DOI] [PubMed] [Google Scholar]
- 20.Arena R., Guazzi M., Lianov L., et al. Healthy lifestyle interventions to combat noncommunicable disease-a novel nonhierarchical connectivity model for key stakeholders: a policy statement from the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine. Mayo Clin Proc. 2015;90(8):1082–1103. doi: 10.1016/j.mayocp.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Gaye B., Canonico M., Perier M.C., et al. Ideal cardiovascular health, mortality, and vascular events in elderly subjects: the three-city study. J Am Coll Cardiol. 2017;69(25):3015–3026. doi: 10.1016/j.jacc.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Aneni E.C., Crippa A., Osondu C.U., et al. Estimates of mortality benefit from ideal cardiovascular health metrics: a dose response meta-analysis. Journal of the American Heart Association. 2017;6(12) doi: 10.1161/JAHA.117.006904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fani Marvasti F., Stafford R.S. From sick care to health care—reengineering prevention into the U.S. system. N Engl J Med. 2012;367(10):889–891. doi: 10.1056/NEJMp1206230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luzi L., Radaelli M.G. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020;57(6):759–764. doi: 10.1007/s00592-020-01522-8. Epub 2020 Apr 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dietz W., Santos-Burgoa C. Obesity and its implications for COVID-19 mortality. Obesity (Silver Spring, Md) 2020;28(6):1005. doi: 10.1002/oby.22818. Epub 2020 Apr 18. [DOI] [PubMed] [Google Scholar]
- 26.Chow N., Fleming-Dutra K., Gierke R., et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 — United States, February 12–March 28, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(13) doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen T., Dai Z., Mo P., et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2020 doi: 10.1093/gerona/glaa089. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muniyappa R., Gubbi S. COVID-19 pandemic, corona viruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318(5):E736–E741. doi: 10.1152/ajpendo.00124.2020. Published online 2020 Mar 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang J.K., Feng Y., Yuan M.Y., et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006;23(6):623–628. doi: 10.1111/j.1464-5491.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen H., Manolova G., Daskalopoulou C., Vitoratou S., Prince M., Prina A.M. Prevalence of multimorbidity in community settings: a systematic review and meta-analysis of observational studies. J Comorb. 2019;9 doi: 10.1177/2235042X19870934. [2235042X19870934-12235042X19870934] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Jama. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laddu D.R., Lavie C.J., Phillips S.A., Arena R. Physical activity for immunity protection: inoculating populations with healthy living medicine in preparation for the next pandemic. Progress in Cardiovascular Diseases. Apr 9 2020 doi: 10.1016/j.pcad.2020.04.006. [S0033-0620(20)30078-5, online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Rosa V., Galgani M., Santopaolo M., Colamatteo A., Laccetti R., Matarese G. Nutritional control of immunity: balancing the metabolic requirements with an appropriate immune function. Semin Immunol. 2015;27(5):300–309. doi: 10.1016/j.smim.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 34.Butler M.J., Barrientos R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.040. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zbinden-Foncea H, Francaux M, Deldicque L, Hawley JA. Does high cardiorespiratory fitness confer some protection against pro-inflammatory responses after infection by SARS-CoV-2? Obesity. [n/a(n/a)]. doi: 10.1002/oby.22849. Online ahead of print. [DOI] [PMC free article] [PubMed]
- 36.Hall G., Laddu D.R., Phillips S.A., Lavie C.J., Arena R. A tale of two pandemics: how will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Progress in Cardiovascular Diseases. Apr 8 2020 doi: 10.1016/j.pcad.2020.04.005. [S0033-0620(20)30077-3, online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sim Y.J., Yu S., Yoon K.J., Loiacono C.M., Kohut M.L. Chronic exercise reduces illness severity, decreases viral load, and results in greater anti-inflammatory effects than acute exercise during influenza infection. J Infect Dis. 2009;200(9):1434–1442. doi: 10.1086/606014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong C.M., Lai H.K., Ou C.Q., et al. Is exercise protective against influenza-associated mortality? PloS One. 2008;3(5) doi: 10.1371/journal.pone.0002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nieman D.C., Wentz L.M. The compelling link between physical activity and the body’s defense system. J Sport Health Sci. 2019;8(3):201–217. doi: 10.1016/j.jshs.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xiang M., Zhang Z., Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Progress in Cardiovascular Diseases. 2020 doi: 10.1016/j.pcad.2020.04.013. [S0033-0620(0020)30096-30097] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meyer J., McDowell C., Lansing J., et al. Changes in physical activity and sedentary behaviour due to the COVID-19 outbreak and associations with mental health in 3,052 US adults. Cambridge Open Engage. 2020 doi: 10.33774/coe-2020-h0b8g. [DOI] [Google Scholar]
- 42.Ahmed I. COVID-19 - does exercise prescription and maximal oxygen uptake (VO2 max) have a role in risk-stratifying patients? Clinical Medicine (London, England) 2020 doi: 10.7861/clinmed.2020-0111. [DOI] [PMC free article] [PubMed] [Google Scholar]