Abstract
Introduction
To investigate student clinical placement concerns and opinions, during the initial COVID-19 pandemic outbreak and to inform educational institution support planning.
Methods
Between mid-June to mid-July 2020, educational institutions from 12 countries were invited to participate in an online survey designed to gain student radiographer opinion from a wide geographical spread and countries with varying levels of COVID-19 cases.
Results
1277 respondents participated, of these 592 had completed clinical placements during January to June 2020. Accommodation and cohabiting risks were identified as challenging, as was isolation from family, travel to clinical placements, and to a lesser extent childcare. Students stated they had been affected by the feeling of isolation and concerns about the virus whilst on placement. Overall 35.4% of all respondents were ‘Not at all worried’ about being a radiographer, however, 64.6% expressed varying levels of concern and individual domestic or health situations significantly impacted responses (p ≤ 0.05). Year 4 students and recent graduates were significantly more likely to be ‘Not worried at all’ compared to Year 2 and 3 students (p ≤ 0.05). The need for improved communication regarding clinical placements scheduling was identified as almost 50% of students on clinical placements between January to June 2020 identified the completion of assessments as challenging. Furthermore, only 66% of respondents with COVID-19 imaging experience stated being confident with personal protective equipment (PPE) use.
Conclusion
Student radiographers identified key challenges which require consideration to ensure appropriate measures are in place to support their ongoing needs. Importantly PPE training is required before placement regardless of prior COVID-19 imaging experience.
Implications for practice
As the next academic year commences, the study findings identify important matters to be considered by education institutions with responsibility for Radiography training and as students commence clinical placements during the on-going global COVID-19 pandemic.
Keywords: COVID-19, Clinical placement, Radiographers, Radiography education, Students, Surveys and questionnaires
Introduction
The COVID-19 pandemic has introduced challenges for educational training institutions and healthcare professions globally since the initial outbreak in China and as COVID-19 impacted globally and declared a pandemic in March 2020.1 Several publications have reported the concerns and experiences of several professions including dentistry and several medical disciplines, to include radiology, surgery and urology.2, 3, 4, 5, 6 A recent paper by Robbins et al.2 investigated the impact of the pandemic on radiology resident training and their wellbeing in the United States. The “Well-Being Subcommittee” of the Association of Program Directors in Radiology (APDR) surveyed its members (n = 312) and 108 responded. Respondents felt that the COVID-19 pandemic has negatively impacted their residency programs concerning educational (70%), clinical (83%), and well-being matters. Residency involvement in clinical activities had been negatively impacted due to the re-organisation of the radiology departments during the pandemic which in turn had resulted in reduced clinical training hours within the clinical environment for trainees.2 During the first wave of the pandemic, many radiology departments internationally were forced to change operations and focus principally on dealing with COVID-19 and as a consequence, many routine procedures were cancelled or postponed. Several papers have documented these changes in practice and currently, the focus is on how to best address radiology waiting lists at a time when a second COVID-19 wave is anticipated and as some countries are still dealing with the initial wave.7, 8, 9, 10, 11, 12
Patients awaiting medical imaging procedures have been significantly affected and there is substantial concern that many pathologies are not being diagnosed in an optimal period due to imaging delays and the publics’ reticence to attend general practitioner appointments or hospital appointments during the lockdown phases applied to reduce the impact of the COVID-19 pandemic.7, 8, 9, 10, 11, 12 Also, there is evidence that the morbidity arising from the virus is significant and will require ongoing monitoring of chronic illness.13 , 14 A further impact of the disruption to radiology services is to radiography training as well as radiology residency training. This includes the rapid switch from the foundation of in-person teaching to online education and also the impact on clinical placements. With a lack of radiography examinations being referred, aside from chest examinations, and substantially reduced patient numbers attending emergency and outpatient departments during lockdown, many radiography training institutions internationally have had to cancel or postpone student clinical schedules. Also, some radiographic practise has had to adapt to account for the infectious characteristics of COVID-19.2 , 15, 16, 17, 18 The additional risk of COVID-19 has also placed doubt on whether early-stage radiography students should be in the clinical environment as they posed a possible increased infection prevention and control risk. Additionally, radiographers, as frontline healthcare staff, have been primarily focussed on dealing with the extreme pressures of COVID-19 imaging since the commencement of the pandemic.19 , 20 Verbal communication with multiple Radiography training centres has indicated that many countries withdrew the majority of students from clinical placements with the exception possibly of final year/graduating cohorts as identified by Yi Xiang Tay et al., (2020).21
The impact upon student radiographers to date has not been investigated and this paper aimed to gain insight into how student radiographers, in clinical placements during the initial wave of COVID-19, dealt with issues and to ask student radiographers in general about their perceptions regarding clinical training. The findings of the study are to be disseminated to training institutions internationally to support activity going into the next academic year.
Methods
Survey design
A survey containing 20 questions was designed to investigate the impact of COVID-19 upon student radiographers, including final year students who graduated during the investigated time frame, and their clinical placements. Institutional ethical approval was gained in the form of an exemption from full ethical review. The survey was intended to be completed in less than 10 min. No incentive was offered for survey participation. The survey requested demographic information, to include: country of training, academic stage of training, student age, and living accommodation details. Students indicated if they had been in on clinical placement between January to June 2020. The students/new graduates were asked about their involvement with COVID-19 imaging, their main challenges and concerns related to clinical placements and continuing students responded in relation to their concerns going forwards into the next academic year. All participants were asked if the COVID-19 pandemic had impacted how they felt about being a radiographer and if they had spoken about their concerns and their communication supports. A mix of closed, rating, and open response options were employed. The Survey Monkey online platform (http://www.surveymonkey.com/) was employed as the survey tool and the anonymous responses were collated in excel spreadsheets for analysis. The independent samples t-test was used to explore for statistically significant differences between certain response categories with p-values ≤0.05 indicating statistical significance.
Participating institutions
Selected Radiography training institutions (n = 14) were invited to participate from twelve countries. The study involved a convenience sampling methodology to facilitate responses from a spread of international geographical locations and from jurisdictions which had encountered varying levels of COVID-19 infection. The research partners confirmed local ethical approval as appropriate before the commencement of the study. Participating countries had one educational participant except for Ireland and the United Kingdom where two training institutions participated. In Italy, The European country most impacted in the initial wave, all training institutions were invited to participate through the Italian Federation of Scientific Radiographers Societies (FASTeR) and the Italian Board of Didactic Coordinators. Respondents from Italy were asked to identify their geographical location as either Lombardy (the Italian epicentre of the COVID-19 outbreak) or outside Lombardy.
The link to the survey was distributed to the participating centres who forwarded the survey details to their student radiographers (n = 4712; Table 1 ) with a request for their participation. During a four-week period, from mid-June to mid-July 2020, the survey was open for responses with two reminders sent to students, to request their participation.
Table 1.
Demographic data of student respondents and response rates.
| Country | Participating Institution | Students Invited (n) |
Responses (n) | Response Rate (%) | Year | Ages | n (%) |
|---|---|---|---|---|---|---|---|
| Australia | University of Sydney | 535 | 45 | 8.4 | Year 2: 27 Year 3: 8 Year 4: 6 Graduate: 4 |
18–23 24–29 30–35 36–40 41+ |
40 (88.9) 2 (4.4) 1 (2.2) 0 (0.0) 2 (4.4) |
| Austria | FH Campus Vienna | 263 | 44 | 16.7 | Year 2: 15 Year 3: 15 Year 4: 1 Graduate: 13 |
18–23 24–29 30–35 36–40 41+ |
30 (68.2) 13 (29.6) 1 (2.3) 0 (0.0) 0 (0.0) |
| Belgium | Odisee University of Applied Sciences | 63 | 30 | 47.6 | Year 2: 1 Year 3: 17 Graduate: 12 |
18–23 24–29 30–35 36–40 41+ |
24 (80.0) 6 (20.0) 0 (0.0) 0 (0.0) 0 (0.0) |
| Denmark | University College Lillebaelt | 215 | 42 | 19.5 | Year 2: 16 Year 3: 18 Year 4: 3 Graduate: 5 |
18–23 24–29 30–35 36–40 41+ |
22 (52.4) 14 (33.3) 3 (7.1) 1 (2.4) 2 (4.8) |
| Ireland | University College Dublin | 365 | 328 | 82.6 | Year 2: 127 Year 3:80 Year 4: 68 Graduate: 53 |
18–23 24–29 30–35 36–40 41+ |
284 (86.6) 31 (9.5) 4 (1.2) 6 (1.8) 3 (0.9) |
| University College Cork | 32 | ||||||
| Italy | Italian Radiography & Diagnostic Imaging course didactic coordinators | 2100 | 483 | 23.0 | Year 2: 206 Year 3: 199 Year 4: 10 Graduate: 68 |
18–23 24–29 30–35 36–40 41+ |
395 (81.8) 60 (12.4) 20 (4.1) 4 (0.8) 4 (0.8) |
| Netherlands | Hanze University of Applied Sciences | 200 | 33 | 16.5 | Year 2: 0 Year 3: 8 Year 4: 20 Graduate: 5 |
18–23 24–29 30–35 36–40 41+ |
29 (87.9) 4 (12.1) 0 (0.0) 0 (0.0) 0 (0.0) |
| Singapore | Singapore Institute of Technology | 237 | 52 | 21.9 | Year 2: 20 Year 3: 23 Year 4: 9 Graduate: 0 |
18–23 24–29 30–35 36–40 41+ |
33 (63.5) 11 (21.2) 1 (1.9) 3 (5.8) 4 (7.7) |
| Slovenia | University of Ljubljana | 130 | 57 | 43.8 | Year 2: 29 Year 3: 18 Year 4: 2 Graduate: 8 |
18–23 24–29 30–35 36–40 41+ |
49 (86.0) 5 (8.8) 1 (1.8) 1 (1.8) 1 (1.8) |
| South Africa | University of Johannesburg | 400 | 101 | 25.3 | Year 2: 57 Year 3: 24 Year 4: 20 Graduate: 0 |
18–23 24–29 30–35 36–40 41+ |
73 (72.3) 24 (23.8) 3 (3.0) 1 (1.0) 0 (0.0) |
| United Kingdom | Keele University | 70 | 41 | 33.1 | Year 2: 19 Year 3: 21 Graduate: 1 |
18–23 24–29 30–35 36–40 41+ |
29 (70.7) 7 (17.1) 4 (9.8) 1 (2.4) 0 (0.0) |
| University of Exeter | 54 | ||||||
| United States of America | Quinnipiac University | 48 | 21 | 43.8 | Year 2: 1 Year 3: 4 Year 4: 1 Graduate: 15 |
18–23 24–29 30–35 36–40 41+ |
19 (90.5) 1 (4.8) 1 (4.8) 0 (0.0) 0 (0.0) |
Results
Demographics
Overall 1277 responses were received from student radiographers training in 12 countries (representing an overall response rate of 27.1%). Table 1, Table 2 outline the demographics of responses. The length of Radiography programmes were identified as 4 years (n = 508; 39.8%), 3.5 years (n = 53; 4.2%), 3 years (n = 651; 51.0%), and other (n = 65; 5.1%) were accelerated graduate entry programmes of 2–2.5 years duration. The participants were from varying stages of training: Year 2 (n = 518; 40.6%), Year 3 (n = 435; 34.1%), Year 4 (n = 140; 11.0%), and new graduates (n = 184; 14.4%). Ages ranged in years from 18 to 23 (80.4%), 24–29 (13.9%), 30–35 (3.1%), 36–40 (1.3%) and over 40 years (1.3%).
Table 2.
Demographic data of student respondents and response rates for Italy: Lombardy Region and Outside Lombardy.
| Italy | Italian Radiography & Diagnostic Imaging course didactic coordinators | 2100 | 129 (Lombardy) | 23.0 | Year 2: 57 Year 3: 54 Graduate: 18 |
18–23 24–29 30–35 36–40 41+ |
106 (82.2) 17 (13.2) 4 (3.1) 1 (0.8) 1 (0.8) |
| 354 (Outside Lombardy) | Year 2: 149 Year 3: 145 Year 4: 10 Graduate: 50 |
18–23 24–29 30–35 36–40 41+ |
289 (81.6) 43 (12.2) 16 (4.5) 3 (0.9) 3 (0.9) |
Living situation
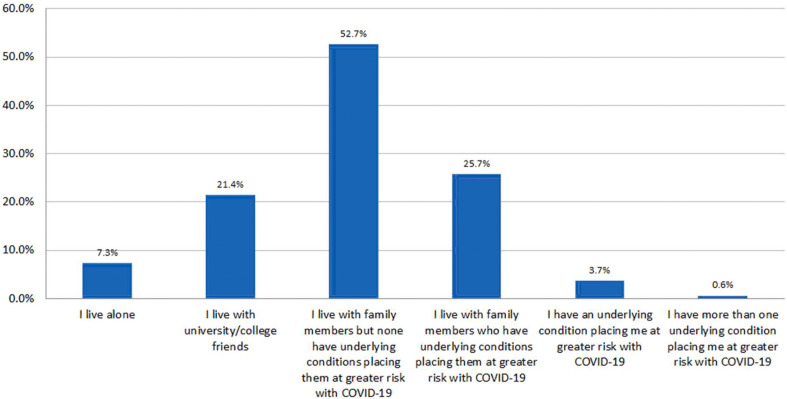
Responses related to living conditions are outlined in Fig. 1 . Cohabiting increases the risk of COVID-19 spread and Fig. 1 also identifies students and new graduates who are either at heightened risk themselves due to known underlying conditions or living with friends or relatives who are compromised concerning COVID-1922. Overall 329 (25.8%) respondents live with a compromised family member and 4.4% (n = 56) of respondents have at least one underlying risk factor.
Figure 1.
Summary of responses on living situation and underlying conditions.
Clinical placements
Just under half of the 1277 respondents (n = 592; 46.4%) had been in clinical placement between January to June 2020. Of this cohort, 184 (33.3%) had been involved in COVID-19 imaging for the duration of their placements. Overall, 223 (40.3%) had some experience of COVID-19 patients, while 146 (26.4%) had no exposure to COVID-19 patients while on clinical placements.
Of the 592 respondents who had been in clinical between January to June 2020, 553 responded to further questions relating to these clinical placements. The duration of their clinical placements during this period were identified as: 1–4 weeks (n = 300; 54.3%), 5–8 weeks (n = 118; 21.3%), 9–12 weeks (n = 77; 13.9%) and over 12 weeks (n = 58; 10.5%).
Responses were mixed regarding communication about clinical placement schedules since the start of the COVID-19 pandemic; while over 50% (n = 279) were ‘Very satisfied’ (n = 69; 12.5%) or ‘Satisfied’ (n = 210; 38.0%), 26% (n = 144) were ‘Neither satisfied nor dissatisfied’, and 23.5% (n = 130) were either ‘Dissatisfied’ (n = 99; 17.9%) or ‘Very Dissatisfied’ (n = 31; 5.6%).
While 407 (73.6%) of those who had undertaken clinical placements had either been exposed to COVID-19 Imaging for either all or part of their placements, only 217 respondents (39.2%) said they were either ‘Extremely confident’ (n = 68; 12.3%) or ‘Very confident’ (n = 149; 26.9%) in the use of personal protective equipment (PPE). Of the remaining respondents who had completed clinical placements during the pandemic, 226 (40.9%) were ‘Somewhat confident’ in PPE use, while the remainder were ‘Not so confident’ (n = 91; 16.5%) or ‘Not at all confident’ (n = 19; 3.4%).
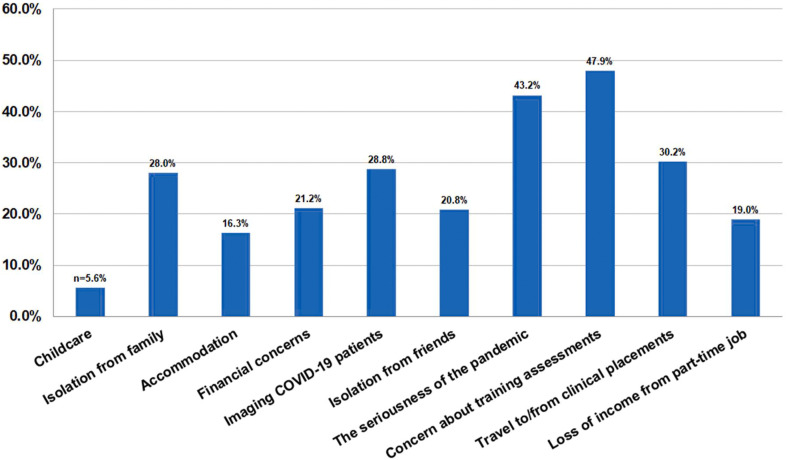
Fig. 2 outlines the identified challenges experienced during clinical placements. Respondents identified the lack of available patients for practice and assessment purposes; unavailability of staff who were unwell or self-isolating; anxiety about spreading the infection to family and others; and anxiety among my family for my safety, were all specified as challenges/concerns.
Figure 2.
A summary of the challenges identified by respondents who undertook clinical placements during the pandemic (respondents were asked to identify their top three challenges).
When asked if they had concerns before commencing clinical placements during the pandemic only 16.3% (n = 90) indicated that they were ‘Not worried at all’. Those who expressed concerns were ‘Extremely worried’ (n = 58; 10.5%), ‘Very worried’ (n = 88; 16.0%), ‘Somewhat worried’ (n = 194; 35.2%), or ‘Slightly worried’ (n = 121; 22.0%).
All survey respondents were then asked if they may not be able to complete clinical placements due to a personal medical condition and how worried they are about this. Of the 1110 who responded to this question, 445 (40.1%) indicated that this was ‘Not applicable’ to them due to an absence of underlying medical concerns, 68 (6.1%) indicated that they were ‘Not at all worried’, however, 305 (27.5%) respondents were either ‘Extremely worried’ (n = 135; 12.2%) or ‘Very worried’ (n = 170; 15.3%).
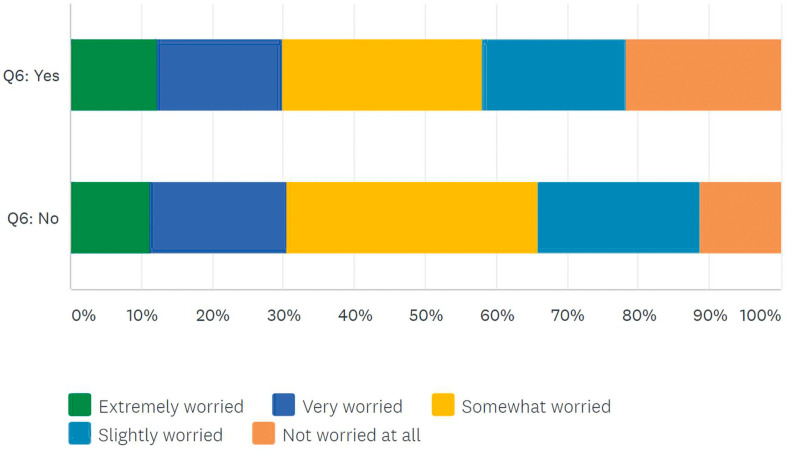
When asked about future clinical placements, similar response patterns (Fig. 3 ) were seen for those who had undertaken clinical placement since January 2020 and those who had not undertaken placements during the pandemic. Significant differences were seen in the ‘Not worried at all’ category with 21.6% of those who had undertaken clinical placements versus 11.2% of those who had not undertaken clinical placements (p ≤ 0.05) and in the ‘Somewhat worried’ category where 28.2% of those who had undertaken clinical placements versus 35.3% of those who had not undertaken clinical placements (p ≤ 0.05).
Figure 3.
Worried about future clinical placements due to COVID-19 (‘Yes’ = those who have undertaken clinical placement during the pandemic and ‘No’ = those who have not).
Other COVID-19 affects
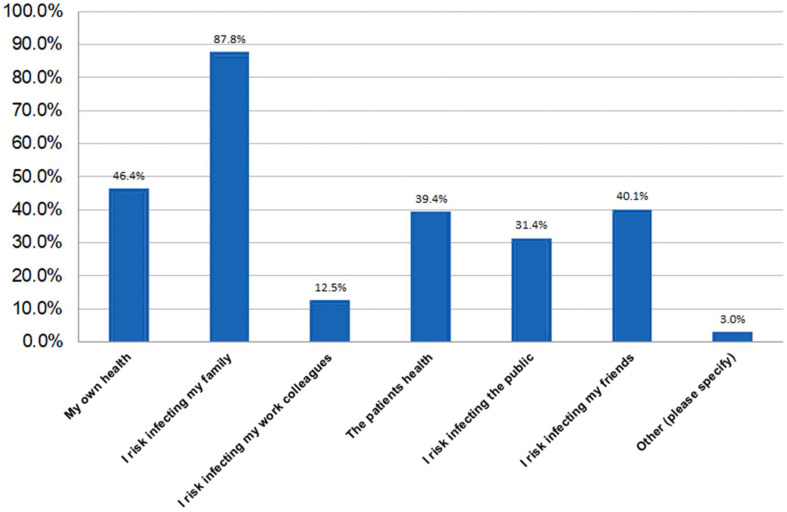
Fig. 4 summarises the main infection prevention and control concerns among respondents. Comments to this question were provided by 33 respondents and included: concerns over infecting patients/clients in other clinical or care facilities where respondents work part-time; fear of being infected by other students or staff; not being able to self-isolate due to shared accommodation arrangements; and several stated that they have no concerns as they assume all appropriate measures will be in place to avoid risk.
Figure 4.
A summary of responses concerning infection prevention and control during the COVID-19 pandemic (respondents were asked to identify their top three concerns).
When asked ‘Has Covid-19 made you worry about being a radiographer?’, reassuringly, 393 (35.4%) of respondents indicated that they were ‘Not at all worried’ about being a radiographer’ however, 47 (4.2%) were ‘Extremely worried’, 79 (7.1%) were ‘Very worried’, 307 (27.7%) were ‘Somewhat worried’, and 284 (25.6%) were ‘Slightly worried’.
When asked ‘How worried are you about the impact of Covid-19 on you personally?’, only 110 (9.9%) of respondents indicated that they were ‘Not at all worried’ and 317 (28.6%) were ‘Not so worried’. However, 78 (7.0%) were ‘Extremely worried’, 154 (13.9%) were ‘Very worried’, and 451 (40.6%) were ‘Somewhat worried’.
When asked if they had spoken to anybody about their COVID-19 related concerns, the majority indicated that they had spoken to family or friends. This was followed by considerably fewer discussions with clinical tutors/clinical practice educators, radiographers, lecturers, and student advisers. 199 (17.9%) of respondents indicated that they had not discussed their concerns with anybody.
Finally, students and graduates were asked how confident they were that they had an appropriate support network outside the university/radiography training environment. Reassuringly, 530 (47.8%) were either ‘Extremely confident’ (n = 155; 14.0%) or ‘Very confident’ (n = 375; 33.8%) that they had an appropriate support network in place whereas 188 (16.9%) were either ‘Not so confident’ (n = 142; 12.8%) or ‘Not confident at all’ (n = 46; 4.1%) that they had access to a support network.
Comparison of the domestic situation and health concerns with other responses
As shown in Table 3 , some statistically significant differences were identified. Those living with university/college friends or living with a family member with an underlying condition were more likely to be ‘Extremely worried’ than those living with family members without any underlying conditions.
Table 3.
Comparison of domestic and health situations with worry in advance of commencing clinical placements undertaken between January to June 2020 (during the COVID-19 pandemic).
| My Situation | Extremely worried | Very worried | Somewhat worried | Slightly worried | Not worried at all | Total respondents |
|---|---|---|---|---|---|---|
| A. I live alone | 13.9% (5) | 13.9% (5) | 30.6% (11) | 19.4% (7) | 22.2% (8) | 6.5% (36) |
| B. I live with university/college friends | 18.4% (25)a | 13.2% (18) | 33.1% (45) | 19.9% (27) | 15.4% (21) | 24.6% (136) |
| C. I live with family members, but none have underlying conditions placing them at greater risk with Covid-19 | 5.8% (16)b | 16.1% (44) | 35.8% (98) | 26.3% (72)c | 16.1% (44) | 49.6% (274) |
| D. I live with family members who have underlying conditions placing them at greater risk with Covid-19 | 13.1% (20)a | 17.7% (27) | 39.2% (60) | 15.7% (24)a | 14.4% (22) | 27.7% (153) |
| E. I have an underlying condition placing me at greater risk with Covid-19 | 9.1% (2) | 27.3% (6) | 36.4% (8) | 4.6% (1) | 22.7% (5) | 4.0% (22) |
| F. I have more than one underlying condition placing me at greater risk with Covid-19 | 0.0% (0) | 50.0% (1) | 0.0% (0) | 50.0% (1) | 0.0% (0) | 0.4% (2) |
| Total respondents | 10.5% (58) | 15.9% (88) | 35.4% (196) | 21.9% (121) | 16.3% (90) | 100.0% (553) |
aSignificantly higher than those in ‘Situation’ category C (p ≤ 0.05).
bSignificantly lower than those in ‘Situation’ categories B and D (p ≤ 0.05).
cSignificantly higher than those in ‘Situation’ category D (p ≤ 0.05).
Table 4 also highlights some significant differences in terms of future clinical placements, those living with university/college friends (18.5%) or living with family members without any underlying conditions (17.0%) were significantly more likely to be ‘Not worried at all’ versus those living with a family member with an underlying condition (10.5%). Those living with a family member with an underlying condition (16.5%) or having an underlying condition themselves (18.2%) were significantly more likely to report being ‘Extremely worried’ than those living with family members without any underlying conditions (8.9%).
Table 4.
Comparison of domestic and health situations with worry in advance of future clinical placements.
| My Situation | Extremely worried | Very worried | Somewhat worried | Slightly worried | Not worried at all | Total respondents |
|---|---|---|---|---|---|---|
| A. I live alone | 14.6% (12) | 20.7% (17) | 29.3% (24) | 18.3% (15) | 17.1% (14) | 7.4% (82) |
| B. I live with university/college friends | 12.2% (29) | 19.3% (46) | 28.6% (68) | 21.4% (51) | 18.5% (44)a | 21.4% (238) |
| C. I live with family members, but none have underlying conditions placing them at greater risk with Covid-19 | 8.9% (52)b | 17.3% (101) | 34.4% (201) | 22.4% (131) | 17.0% (99)a | 52.6% (584) |
| D. I live with family members who have underlying conditions placing them at greater risk with Covid-19 | 16.5% (47)c | 20.0% (57) | 31.9% (91) | 21.1% (60) | 10.5% (30)d | 25.7% (285) |
| E. I have an underlying condition placing me at greater risk with Covid-19 | 18.2% (8)c | 22.7% (10) | 25.0% (11) | 13.6% (6) | 20.5% (9) | 4.0% (44) |
| F. I have more than one underlying condition placing me at greater risk with Covid-19 | 28.6% (2) | 0.0% (0) | 42.9% (3) | 0.0% (0) | 28.6% (2) | 0.6% (7) |
| Total respondents | 11.7% (130) | 18.6% (206) | 32.0% (355) | 21.7% (241) | 16.0% (178) | 100% (1110) |
aSignificantly higher than those in ‘Situation’ category D (p ≤ 0.05).
bSignificantly lower than those in ‘Situation’ categories D and E (p ≤ 0.05).
cSignificantly higher than those in ‘Situation’ category C (p ≤ 0.05).
dSignificantly lower than those in ‘Situation’ categories B and C (p ≤ 0.05).
Individual domestic or health situation was found to significantly impact on views about worries about being a radiographer in some cases (Table 5 ); those living alone (9.8%), living with university/college friends (5.9%), or those living with a family member with an underlying condition (4.9%) were significantly more likely to be ‘Extremely worried’ about being a radiographer than those living with family members without any underlying conditions (2.2%). Those living alone (41.5%) were significantly more likely to be ‘Not worried at all’ than those having an underlying condition themselves (22.7%).
Table 5.
Comparison of domestic and health situations with worry about being a radiographer.
| My Situation | Extremely worried | Very worried | Somewhat worried | Slightly worried | Not worried at all | Total respondents |
|---|---|---|---|---|---|---|
| A. I live alone | 9.8% (8)a | 8.5% (7) | 15.9% (13) | 24.4% (20) | 41.5% (34)b | 7.4% (82) |
| B. I live with university/college friends | 5.9% (14)a | 7.6% (18) | 29.0% (69)c | 23.1% (55) | 34.5% (82) | 21.4% (238) |
| C. I live with family members, but none have underlying conditions placing them at greater risk with Covid-19 | 2.2% (13)d | 6.0% (35) | 27.9% (163)c | 27.6% (161) | 36.3% (212) | 52.6% (584) |
| D. I live with family members who have underlying conditions placing them at greater risk with Covid-19 | 4.9% (14)a | 7.7% (22) | 29.5% (84)c | 26.3% (75) | 31.6% (90) | 25.7% (285) |
| E. I have an underlying condition placing me at greater risk with Covid-19 | 6.8% (3) | 9.1% (4) | 34.1% (15)c | 27.3% (12) | 22.7% (10)c | 4.0% (44) |
| F. I have more than one underlying condition placing me at greater risk with Covid-19 | 28.6% (2) | 0.0% (0) | 42.9% (3) | 14.3% (1) | 14.3% (1) | 0.6% (7) |
| Total respondents | 4.2% (47) | 7.1% (79) | 27.7% (307) | 25.6% (284) | 35.4% (393) | 100.0% (1110) |
aSignificantly higher than those in ‘Situation’ category C (p ≤ 0.05).
bSignificantly higher than those in ‘Situation’ category E (p ≤ 0.05).
cSignificantly higher than those in ‘Situation’ category A (p ≤ 0.05).
dSignificantly lower than those in ‘Situation’ categories A, B and D (p ≤ 0.05).
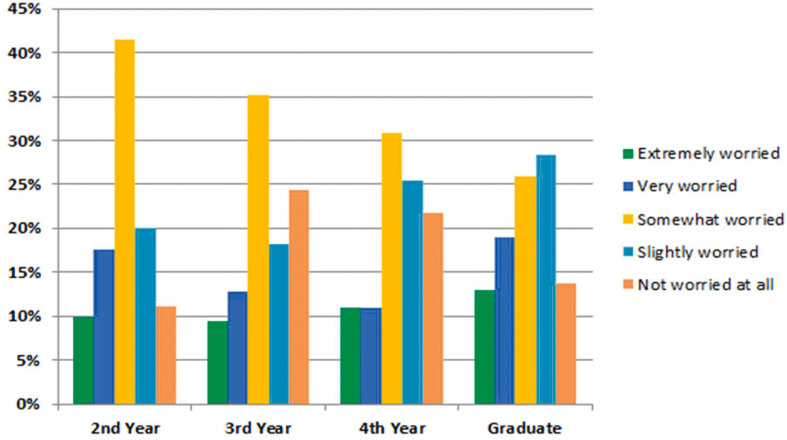
Comparisons of respondent year groups with other responses
Year 4 students and recent graduates were significantly more likely to report being ‘Not worried at all’ when compared to Year 2 and Year 3 students (p ≤ 0.05). Responses in the ‘Extremely worried’ category demonstrated minimal variation between all four respondent groups (Fig. 5 ). 19.0% of Graduates and 17.5% of Year 2 students indicated that they were ‘Very worried’ compared to 12.8% of Year 3 students and 10.9% of Year 4 students, however, these differences were not statistically significant.
Figure 5.
Year group versus concerns in advance of clinical placement between January to June 2020 (during the COVID-19 pandemic).
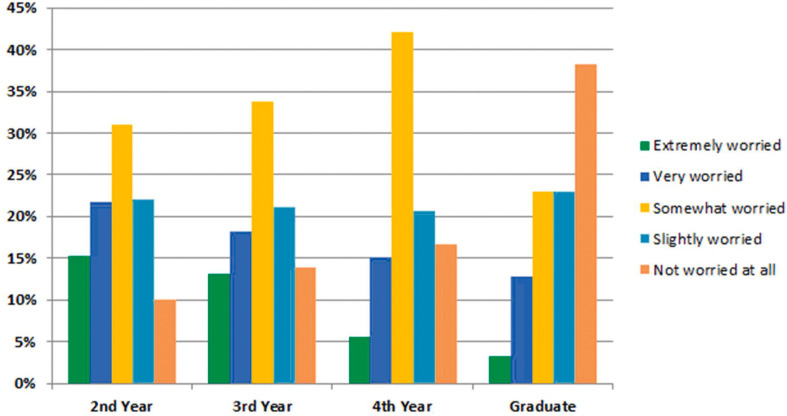
As shown in Fig. 6 , a significantly higher proportion of Year 2 (15.3%) and Year 3 (13.0%) students reported being ‘Extremely worried’ about their future clinical placements compared to Year 4 students (5.6%) and Graduates (3.2%) (p ≤ 0.05). Similarly, Year 2 students were significantly more likely to be ‘Very worried’ versus Graduates (21.8% v 12.7%; p ≤ 0.05). The Graduates were significantly more likely to state that they were ‘Not worried at all’ (38.2%) versus Year 2 (10.0%), Year 3 (13.9%), and Year 4 (16.7%) students.
Figure 6.
Year group versus concerns in advance of future clinical placements.
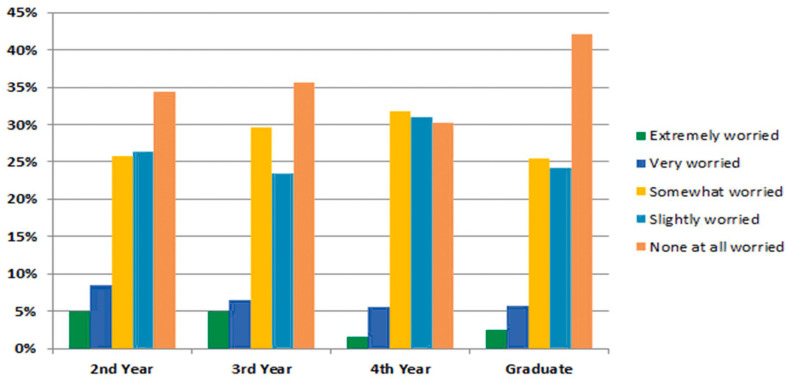
In terms of their worries about becoming a radiographer based on their experiences during the COVID-19 pandemic (Fig. 7 ), responses between all four respondent cohorts demonstrated minimal variability for each category except for the ‘Not at all worried’ category where significantly more Graduates (42.0%) than Year 4 students (30.2%) gave this response.
Figure 7.
Year group versus worries about being a radiographer.
Discussion
A snapshot of student radiographer concerns was gained from 1277 respondents from selected countries and institutions around the world. Radiographers are frontline healthcare professionals who have a critical role in healthcare provision during the COVID-19 pandemic.18, 19, 20 The entry of new graduates to the profession is critical to maintaining workforce numbers, particularly as health services recover from the initial impact of COVID-19 and prepare for further waves of the pandemic.23, 24, 25, 26, 27 Radiography training was impacted in many countries due to COVID-19s’ significant impact on medical imaging services during the first half of 2020 and Radiography education institutions, and clinical partners, need to be aware of student radiographer issues to help best inform on-going planning in the current pandemic crisis.21
The research identified several issues that require consideration, firstly cohabiting, which is widely evidenced to increases the risk of COVID-19 spread which, presents additional risk in those with underlying conditions, or living with friends or relatives who are compromised concerning COVID-19.1 , 22 The survey identified that 92.7% of respondents co-habited, a quarter of whom stated they lived with family members with underlying conditions and 4.4% of student radiographers declared at least one underlying condition (Fig. 1). A recent Italian study, which surveyed 14,374 students and staff from the University of Milan during the peak of the initial COVID-19 wave, discussed the risks associated with cohabiting were discussed and an approximation of 10% of the academic community was identified as being affected by COVID-19.22 Whilst education institutions often have limited flexibility in the scheduling of student clinical placements, there is now an increased need to consider specific student concerns about the risk of transmitting COVID-19 due to cohabiting and those with underlying conditions need to be identified, using appropriate protocols, to ensure appropriate measures are in place to support their needs.
Travel to clinical sites was raised as a concern by 30% of respondents which is as expected as the initial pandemic spread caused significant disruption to public transport internationally during lockdown periods.28 , 29 Those who relied on public transport would have dealt with reduced travel timetables and the concern of COVID-19 risk. This may continue to impact students however public transport safety is being managed in many countries with the use of social distancing and face mask use as mandatory and transport guideline examples are available from the WHO.30 Childcare facilities and schools also closed during the initial wave of the pandemic and uncertainty remains on how these facilities will be provided in many countries. Whilst only a small percentage of respondents (n = 31) stated childcare concerns during clinical placements, this matter requires consideration by education institutions and flexibility is recommended and should be part of discussions with students in the planning of timetables and clinical placements from the outset.
Financial concerns were noted, with students identifying their loss of gaining part-time work income which could potentially impact on a students’ ability to pay for travel and accommodation costs related to clinical training, education fees, or other costs. Financial stress is one of many factors which may impact student worries and wellbeing.
Despite the challenges raised 393 (35.4%) of all respondents indicated that they were ‘Not at all worried’ about being a radiographer, however, education institutions should take note that the remaining 64.6% expressed varying levels of concern and individual domestic or health situation was found to significantly impact on responses (Table 5), particularly for those living alone, living with university/college friends, or those living with a family member with an underlying condition. Year 4 students and recent graduates were significantly more likely to report being ‘Not worried at all’ when compared to Year 2 and Year 3 students (p ≤ 0.05) whilst no significant differences were noted across other response categories. Of concern though was that 199 (17.9%) of respondents indicated that they had not discussed their concerns with anybody and 188 (16.9%) were either ‘Not so confident’ (n = 142; 12.8%) or ‘Not confident at all’ (n = 46; 4.1%) that they had access to a support network.
Additionally, students stated being affected by the feeling of isolation or concerns about the virus. These emotions are not specific to Radiography as the psychological impact of COVID-19 and subsequently extended lockdown situations is well documented.26 The findings suggest clinical timetabling needs to contain mechanisms by which student concerns, specifically due to COVID-19, require early recognition at a time when direct contact between academic institutions and students is limited. The relationships that academic teams forge with clinical departments may never have been so important, particularly as many academic institutions internationally plan either full or partial delivery of their academic programmes via distance learning. It, therefore, appears reasonable to state a potentially greater dependency on clinical staff to identify and liaise with the educational institutions about concerns over student wellbeing, if observed whilst on clinical placement, is of paramount importance. Room for improvement concerning communication about clinical placements was noted, as over one-fifth of students (n = 130; 23.5%) who had been on clinical placement between January to June 2020 had been dissatisfied with communication about schedules.
This study also demonstrates the importance of students being able to complete clinical assessments promptly, with almost 50% (n = 265) of those completing clinical placements between January to June 2020 identifying this as one of their main challenges (Fig. 2). When asked about future clinical placements, those who had been in clinical during the first half of 2020 were significantly less concerned compared to those who had not undertaken clinical placements (p ≤ 0.05) highlighting the need for clinical staff to be aware of the students’ previous experience and prior exposure to COVID-19 imaging.
One further important matter requiring both educational institutional and clinical placement site attention relates to the use of PPE. Of the 592 students who had been in clinical between January to June 2020, 73.6% had an experience of COVID-19 imaging, however, only 217 respondents (39.2%) were either ‘Extremely confident’ (n = 68; 12.3%) or ‘Very confident’ (n = 149; 26.9%) in the use of PPE. These responses highlight the need for educational institutions to possibly provide training support for students before future clinical placements and to highlight this matter to clinical supervisors in the clinical training centres. As the remaining 685 students had no experience of PPE in the COVID-19 clinical environment, the need for bespoke training is further evidenced. As clinical staff are now accustomed to the use of PPE, they potentially need to be alerted to the fact students will continue to require supportive guidance and surveillance in the use of PPE.
Limitations
Convenience sampling was applied and education institutions across a number of countries were invited to participate, the findings are relevant in the context of the institutions sampled and potential bias due to the methodology chosen is noted. The study aim was to disseminate its findings in time for the start of the 2020/2021 academic year, time was therefore limited, and the sampling method provided rapid access to student cohorts in an internal context, whilst recognising the findings may vary from other institutions. It is also noted the survey was distributed across a disproportionate number of Italian educational institutions and findings were collated to identify Lombardy, the epicentre of the European pandemic. The overall response rate was 27.1% with rates varying between 8.4% (Australia) and 82.6% (Ireland). The Italian response numbers are comparable to Irish, national, data collected (483 versus 328) where the survey was also distributed to 96% of Irish student radiographers.
Summary
This research aimed to identify matters of concern related to clinical placements for student radiographers so these can be planned for in the forthcoming academic year. Several challenges for students were identified to include accommodation and travel concerns, childcare and financial worries. Whist education institutions may be limited in their ability to respond to all the student needs in the current planning period and for the next academic year, the research identifies the need for flexibility to support students. The nature of the COVID-19 pandemic means rapid responses to virus surges and therefore planning stability is impacted however the importance of effective communication with students about clinical placements and their assessments is important to the student radiographers.
Conclusions
With the prospect of reduced direct student contact time within education institutions, the need for clear communication with students and with clinical partners is essential. The need to manage individual students in terms of personal health, family health and other concerns, is crucial. Clinical staff also need to be made aware of key information relating to the students they will host. Education institutions and clinical departments need to be cognisant that even students who have experienced COVID-19 imaging are not fully confident in the use of PPE and practical training sessions are strongly recommended before or at the start of clinical placements in the coming year. A mentoring process, in clinical departments, is advisable, particularly if COVID-19 activity is intensive, so students can express and be supported with any concerns. Further research into how best to manage communication between academic and clinical departments during crisis situations, such as the COVID-19 pandemic is warranted.
Conflict of interest statement
None.
Acknowledgements
We would like to thank all of the radiography students who took the time to participate in this survey. We also acknowledge the significant contribution of the Italian Federation of Scientific Radiographers Societies (FASTeR), and their Vice-President, Patrizia Cornacchione, for their support with this work. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.World Health Organisation Coronavirus disease (COVID-19) dashboard. https://covid19.who.int
- 2.Robbins J.B., England E., Patel M.D., DeBenedictis C.M., Sarkany D.S., Heitkamp D.E. COVID-19 impact on well-being and education in radiology residencies: a survey of the association of program Directors in radiology. Acad Radiol. 2020;27(8):1162–1172. doi: 10.1016/j.acra.2020.06.002. https://doi:10.1016/j.acra.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dedeilia A., Sotiropoulos M.G., Hanrahan J.G., Janga D., Dedeilias P., Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34(3 Suppl):1603–1611. doi: 10.21873/invivo.11950. https://doi:10.21873/invivo.11950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garg T., Shrigiriwar A., Patel K. Trainee education during COVID-19. Neuroradiology. 2020;62:1057–1058. doi: 10.1007/s00234-020-02478-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deery C. The COVID-19 pandemic: implications for dental education. Evid Base Dent. 2020;21(2):46–47. doi: 10.1038/s41432-020-0089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amparore D., Claps F., Cacciamani G.E., Esperto F., Fiori C., Liguori G. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. 2020;72(4):505–509. doi: 10.23736/S0393-2249.20.03868-0. https://doi:10.23736/S0393-2249.20.03868-0 [DOI] [PubMed] [Google Scholar]
- 7.Sim W.Y., Ooi C.C., Chen R.C., Aw L.P., Abu Baker R., Tan C.C. How to safely and sustainably reorganise a large general radiography service facing the COVID-19 pandemic. Radiography. 2020 Nov;26(4):e303–e311. doi: 10.1016/j.radi.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freudenberg L.S., Dittmer U., Herrmann K. Impact of COVID-19 on nuclear medicine in Germany, Austria and Switzerland: an international survey in April 2020. Nuklearmedizin. 2020;59(4):294–299. doi: 10.1055/a-1163-3096. https://doi:10.1055/a-1163-3096 [DOI] [PubMed] [Google Scholar]
- 9.Albano D., Bruno A., Bruno F., Calandri M., Caruso D., Clemente A. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. European Radiology. 2020 doi: 10.1007/s00330-020-07046-7. [published online ahead of print, July 14] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegal D.S., Wessman B., Zadorozny J., Palazzola J., Montana A., Rawson J.V. Operational radiology recovery in academic radiology departments after the COVID-19 pandemic: moving toward normalcy. J Am Coll Radiol. 2020 doi: 10.1016/j.jacr.2020.07.004. [published online ahead of print, July 11] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herpe G., Naudin M., Léderlin M., Enikeeva F., Boumendil O., Cassagnes L. COVID-19 impact assessment on the French radiological centers: a nationwide survey. European Radiology. 2020 doi: 10.1007/s00330-020-07035-w. [published online ahead of print, July 3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Implementing best practices for restarting radiology. 2020. https://www.auntminnie.com/index.aspx?sec=nws&sub=rad&pag=dis&ItemID=129286 Dhruv Chopra. [Google Scholar]
- 13.Kang S.J., Jung S.I. Age-related morbidity and mortality among patients with COVID-19. Infect Chemother. 2020;52(2):154–164. doi: 10.3947/ic.2020.52.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Y., Wang Y., Chen Y. Qin Q Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020 Jun;92(6):568–576. doi: 10.1002/jmv.25748. https://doi-org.ucd.idm.oclc.org/10.1002/jmv.25748 Epub 2020 Mar 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stogiannos N., Fotopoulos D., Woznitza N., Malamateniou C. COVID-19 in the radiology department: what radiographers need to know. Radiography. 2020;26(3):254–263. doi: 10.1016/j.radi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zanardo M., Martini C., Monti C.B., Cattaneo F., Ciaralli C., Cornacchione P. Management of patients with suspected or confirmed COVID-19, in the radiology department. Radiography. 2020;26(3):264–268. doi: 10.1016/j.radi.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.England A., Littler E., Romani S., Crosson P. Modifications to mobile chest radiography technique during the COVID-19 pandemic – implications of X-raying through side room windows. Radiography. 2021 Feb;27(1):193–199. doi: 10.1016/j.radi.2020.07.015. [published online ahead of print, August 3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohakud S., Ranjan A., Naik S., Deep N. COVID-19 preparedness for portable x-rays in an Indian hospital – safety of the radiographers, the frontline warriors. Letter to Editor. Radiography. 2020;26(3):270–271. doi: 10.1016/j.radi.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McNulty J. Radiographers on the frontline. J Health Manag. 2020;20(5) https://healthmanagement.org/c/healthmanagement/issue/volume-20-issue-5-2020 [Google Scholar]
- 20.McNulty J., Newman D. EFRS e-learning platform on COVID-19 training for radiographers. www.efrs.eu
- 21.Xiang Tay Yi, Hoon Sng Li, Chow Hwei Chuin, Zainulin Muhammad Rahizan. Clinical placements for undergraduate diagnostic radiography students amidst the COVID-19 pandemic in Singapore: preparation, challenges and strategies for safe resumption. J Med Imag Radiat Sci. 2020 Aug 18 doi: 10.1016/j.jmir.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Negri E., La Vecchia C. A survey on the frequency of COVID-19-like symptoms on students and staff of the University of Milan. Eur J Canc Prev. 2020 doi: 10.1097/CEJ.0000000000000609. [published online ahead of print, July 22] [DOI] [PubMed] [Google Scholar]
- 23.Wu Y., Wang J., Luo C., Hu S., Lin X., Anderson A.E. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manag. 2020;60(1):e60–e65. doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albott C.S., Wozniak J.R., McGlinch B.P., Wall M.H., Gold B.S., Vinogradov S. Battle buddies: rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesth Analg. 2020;131(1):43–54. doi: 10.1213/ANE.0000000000004912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El-Hage W., Hingray C., Lemogne C., Yrondi A., Brunault P., Bienvenu T. Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19): quels risques pour leur santé mentale ? [Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks?] Encephale. 2020;46(3S):S73–S80. doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martínez-Lorca M., Martínez-Lorca A., Criado-Álvarez J.J., Armesilla M.D.C., Latorre J.M. The fear of COVID-19 scale: validation in Spanish university students. Psychiatr Res. 2020;293:113350. doi: 10.1016/j.psychres.2020.113350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morgantini L.A., Naha U., Wang H., Francavilla S., Acar O., Fores J.M. medRxiv; 2020. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. Preprint. [online May 22] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Güner R., Hasanoğlu I., Aktaş F. COVID-19: prevention and control measures in community. Turk J Med Sci. 2020;50(SI-1):571–577. doi: 10.3906/sag-2004-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Government of Ireland . Government publications; 2020. Ireland's response to COVID-19: transport and travel measures.https://www.gov.ie/ga/foilsiuchan/ed29dc-irelands-response-to-covid-19-transport-measures/ [Google Scholar]
- 30.World Health Organization Country and technical guidance - coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance