Sir,
The COVID-19 pandemic has presented microbiology laboratories and infection prevention and control (IPC) teams with unprecedented challenges and questioned their integrated roles. As we reopen clinical services, rapid integrated COVID-19 laboratory results with IPC activities are essential to minimize cross-infection. The challenges associated with COVID-19 laboratory testing have been addressed [1], but pre- and post-analytical aspects are also crucial, including the timely dissemination of results for prompt IPC action. During the first wave of the pandemic, we developed an interactive COVID-19 dashboard by rapidly adapting over six days a pre-existing locally developed carbapenemase-producing Enterobacterales (CPE) dashboard. This was crucial because it enabled real-time oversight of SARS-CoV-2 results for patient placement and other decisions, when the hospital was experiencing unprecedented numbers of COVID-19 admissions.
Beaumont Hospital is an 820-bed adult tertiary referral hospital, providing acute care services to a catchment area of 290,000 people and with national services in renal transplantation, neurosurgery and cochlear implants. Only 16% of beds are in single rooms, of which 77% have en suite facilities, there are only 12 airborne isolation rooms, and normally the hospital functions at near 100% bed occupancy. The hospital has an onsite laboratory with an information management system (LIMS) and a patient administration system (PAS) with paper-based medical records. There is no national electronic patient record (EPR), and during outbreaks, the absence of an electronic solution to patient placement management to provide an overview of the location of infectious patients or those colonized with multi-drug resistant organisms (MDRO) is challenging [2]. Our microbiology laboratory commenced daily SARS-CoV-2 real-time reverse-transcription polymerase chain reaction (PCR) testing on 16th March 2020 on patients with suspected COVID-19. SARS-CoV-2 testing of all admissions regardless of symptoms or suspected COVID-19 status commenced on 19th April 2020.
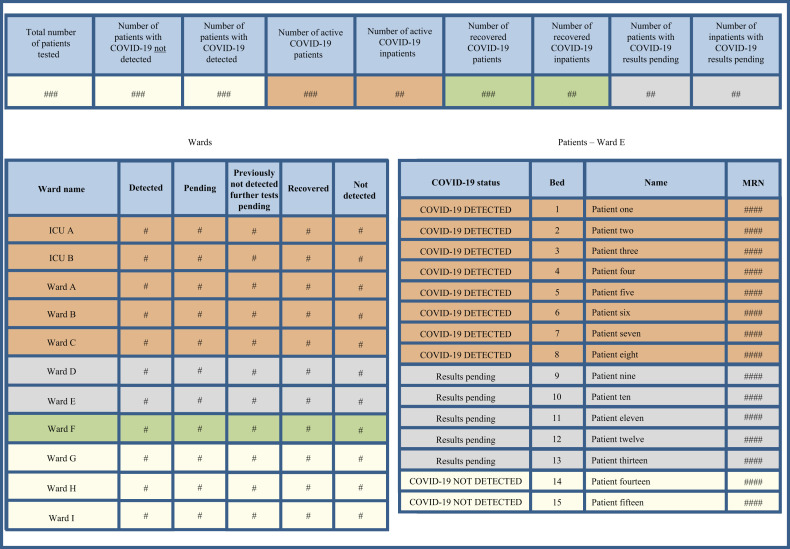
In early March 2020, we adapted the CPE dashboard using existing IT infrastructure that feeds from the LIMS database every 10 min, to create a COVID-19-specific Oracle™ database. SARS-CoV-2 tests (irrespective of the molecular diagnostic testing platforms that have changed with availability and access to validation results) identified via an order communication system are supplemented with patient location, using an embedded live feed from the PAS, i.e. pre-analytical phase. Each patient is assigned a COVID-19 status based on latest results, with manually entered clinical information. The available statues include COVID-19 detected or not, results pending, and at day 14 after symptom onset or positive test date (whichever first), each COVID-19 case is evaluated and may be assigned ‘COVID-recovered’ based on criteria in national guidance [3]. Data are accessible from any hospital computer for authorized users through an interactive dashboard, enabling live tracking of patients by location and test result, i.e. post-analytical action. The dashboard displays hospital- and ward-level data, each ward is ranked by caseload, including results pending, and is colour-coded presenting the overall inpatient caseload of confirmed COVID-19 patients, those with results pending and results where SARS-CoV-2 was not detected (Figure 1 ). Patient location data is automatically updated on transfer, discharge or death. In the ward-level view, each patient is ranked by their COVID-19 status, using the same colour coding with ward location and bed number in the information display.
Figure 1.
Front screen of patient flow COVID-19 dashboard. The available statues include COVID-19 detected or not, results pending, previously not detected further tests pending, and COVID-19 previously detected now recovered for patients who have clinically recovered from COVID-19. Wards with COVID-19 detected patients are displayed at the top of the ward list in orange, wards with no detected patients but with patients awaiting results are displayed in grey, and wards with COVID-19 recovered patients are displayed in green.
Since March 2020, the dashboard has been formally reviewed at daily multi-disciplinary COVID-19 team and other meetings, where latest results inform decisions on patient isolation/cohorting, identification, the management of potential cross-transmission and hospital strategy relating to clinical services. As the dashboard provides up to date laboratory results and patient transfers, it is used throughout the day by the IPC team to identify new cases and to monitor the placement of confirmed cases. It also facilitates the provision of numerous situation reports to external agencies, contributing to national surveillance. The development of this dashboard demonstrates the benefit of adapting existing IT infrastructure to meet quickly an acute healthcare facility's needs during an emergency. Previous studies have highlighted the need for in-house expertise to ensure prompt development and ongoing support of IT systems [4] and this pandemic has placed additional focus on commercial providers of EPRs to provide rapid modifications [5].
This pandemic has highlighted the importance of a holistic and integrated approach including a locally based responsive microbiology laboratory, real-time surveillance, proactive patient flow and responsive IPC services. The successful adaptation of a locally developed dashboard, with regular multi-disciplinary review has hugely supported our hospital's response during the COVID-19 pandemic, through the provision of reliable, timely laboratory information on infection status at patient, ward and hospital levels. This is especially valuable as we have limited single rooms and we lack an integrated IT system. The database is now especially crucial as we reopen hospital services and develop our IPC approach for a possible second wave, and it ensures synergy between different components of service delivery. Our dashboard could be readily adapted by other hospitals and for other pathogens such as during the upcoming influenza season.
Acknowledgements
The authors acknowledge the contribution of Anne Quirke, Gavin McEvoy and Fionnuala Duffy in the development of this project.
Author contributions
M.F. and F.F. conceptualized this letter and drafted it with contributions from I.O’N., B.O’N., H.H., K.B. and E.de B. All authors approved the final version of the letter.
Conflict of interest statement
H.H. has recently been in receipt of research funding from Astellas and Pfizer, and has received a consultancy fee from Pfizer in the last three years. All other authors have no conflicts of interest to declare.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Tang Y.-W., Schmitz J.E., Persing D.H., Stratton C.W. Laboratory diagnosis of COVID-19: current issues and challenges. J Clin Microbiol. 2020;58:e00512–e00520. doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cafferkey J., Skally M., Finn C., Donlon S., Fitzpatrick M., Burns K. Value of a hospital-wide point prevalence survey of carbapenemase-producing Enterobacterales – low-level prevalence confirmed. J Hosp Infect. 2019;1:191–194. doi: 10.1016/j.jhin.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Health Protection Surveillance Centre . 2020. Interim infection prevention and control precautions for possible or confirmed COVID-19 in a pandemic setting.https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/infectionpreventionandcontrolguidance/Interim%20Infection%20Prevention%20and%20Control%20Precautions%20for%20Possible%20or%20Confirmed%20COVID-19%20in%20a%20Pandemic%20Setting.pdf V 1.0. Available at: [last accessed May 2020] [Google Scholar]
- 4.Wong H.J., Caesar M., Bandali S., Agnew J., Abrams H. Electronic inpatient whiteboards: improving multidisciplinary communication and coordination of care. Int J Med Inform. 2009;78:239–247. doi: 10.1016/j.ijmedinf.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Mobi Health News . 2020. How the world of health and tech is looking at the coronavirus outbreak.https://www.mobihealthnews.com/news/europe/how-world-health-and-tech-looking-coronavirus-outbreak Available at: [last accessed May 2020] [Google Scholar]