Background and Purpose:
Since the beginning of the coronavirus disease 2019 (COVID-19) pandemic, many countries have introduced strict hygiene measures of social distancing to prevent further spreading of the disease. This may have led to a decreased presentation to hospital of patients with acute medical conditions and time-dependent management, such as stroke.
Methods:
We conducted a nationwide cohort study using administrative database of all hospitalized patients with main diagnosis of acute ischemic stroke (AIS), transient ischemic attack, or intracerebral hemorrhage. Data from a total of 1463 hospitals in Germany were included. We compared case numbers and treatment characteristics of pandemic (March 16 to May 15, 2020) and prepandemic (January 16 to March 15, 2020) cases and also with corresponding time period in 2019.
Results:
We identified a strong decline for hospitalization of AIS (−17.4%), transient ischemic attack (−22.9%), and intracerebral hemorrhage (−15.8%) patients during the pandemic compared with prepandemic period. IVT rate in patients with AIS was comparable (prepandemic versus pandemic: 16.4% versus 16.6%, P=0.448), whereas mechanical thrombectomy rate was significantly higher during the pandemic (8.1% versus 7.7%, P=0.044). In-hospital mortality was significantly increased in patients with AIS during the pandemic period (8.1% versus 7.6%, P=0.006).
Conclusions:
Besides a massive decrease in absolute case numbers, our data suggest that patients with AIS who did seek acute care during the pandemic, continued to receive acute recanalization treatment in Germany.
Keywords: coronavirus, diagnosis, Germany, hygiene, thrombectomy
At the beginning of coronavirus disease 2019 (COVID-19) pandemic, Germany was one of the countries with the highest numbers of infections. The German Ministry of Health recommended on March 16 that all elective treatments should be postponed to increase hospital capacities for the expected rising numbers of patients with COVID-19. Shortly afterwards, the German government introduced strict hygiene and lockdown measures for strong social distancing to control the spread of COVID-19.
While social distancing and lockdown appear to have successfully flattened the curve of COVID-19 spread in many countries, it has been argued that these measures result in fear of acquiring a severe acute respiratory syndrome coronavirus 2 infection in case of hospitalization. Several previous reports from single-center and regional studies all over the world have shown that patients with acute medical conditions like acute ischemic stroke (AIS) did not present to hospitals1,2 and did not receive time-dependent treatment procedures such as intravenous thrombolysis (IVT) and mechanical thrombectomy (MT)3,4 which is attributed to delays in stroke onset to hospital arrival time5,6 and probably fear to acquire a severe acute respiratory syndrome coronavirus 2 infection. Some of these studies reported different results which may have its reason in regional variations.
We sought to investigate and compare the number of patients hospitalized for AIS, transient ischemic attack (TIA), and intracerebral hemorrhage (ICH), as well as treatment rates of IVT, MT, and in-hospital mortality rate during the COVID-19 pandemic in Germany. This study represents the first nationwide analysis of acute stroke care during the COVID-19 pandemic with full coverage of all hospitalized patients in a country.
Methods
For this study, no informed consent or ethical approval was required because we used completely anonymized data provided by the German Federal Statistical Office in compliance with the German data protection regulations. The latest Good Practice in Secondary Data Analysis recommendations (version 2; 2008) of the German Working Group for the Survey and Utilization of Secondary Data (with representatives from the German Society for Social Medicine and Prevention and the German Society for Epidemiology) and the Working Group for Epidemiological Methods (with representatives from the German Society for Epidemiology, the German Society for Medical Informatics, Biometry and Epidemiology and the German Society for Social Medicine and Prevention) state in their respective Guideline 1 that “…recommendation to consult with an ethics committee need not apply to secondary data analyses, if all the data protection provisions on pseudo-anonymization of all personal data are fulfilled… and no link to primary data is intended.”
The data that support the findings of this study are available from the corresponding author upon reasonable request.
We analyzed case numbers and treatment characteristic of all hospital admissions of patients with AIS, TIA, and ICH during and previous to the COVID-19 pandemic on a nationwide level using high-quality and validated administrative diagnosis-related group database (Data transmission according to §21 KHEntgG and §24 para. 2 KHG; official data on file, source: Institut für das Entgeltsystem im Krankenhaus, InEK, www.g-drg.de). In Germany, all in-patient stroke cases are encoded according to the International Classification of Diseases, Tenth Revision (ICD-10)-GM and relevant operating and procedure keys (OPS-301 codes) issued by the German Institute of Medical Documentation and Information (DIMDI) covering almost 100% of all in-patient cases. We considered the following ICD main diagnosis codes: G45.0-G45.99 (TIA), I63.0-I63.9 (AIS), and I61.0-I61.9 (ICH). All case numbers were aggregated at the level of the 3-digit ICD codes. In addition, the following OPS codes in combination with each considered main diagnosis were analyzed: 8-020.8 (IVT); 8-836.80 (MT). In-hospital mortality was assessed using discharge key 07 (death during hospital stay).
We compared the prepandemic period (January 16 to March 15, 2020) and the pandemic period (March 16 to May 15, 2020). We also compared the data with the corresponding time period in 2019 (March 16 to May 15, 2019; historical controls).
Statistical differences in categorical variables between patients were calculated using χ2 test and for continuous variables using t test. P<0.05 was defined as level of statistical significance.
Results
Acute Ischemic Stroke
Hospital admissions for AIS sharply dropped during the pandemic period (n=31 165) compared with the prepandemic period (n=37 748, −17.4%) and the corresponding time period in 2019 (n=38 247; −18.5%). Commencing in the second half of March 2020, there was a rapidly declining number of hospitalized patients with AIS (Figure). Mean age and gender distribution of patients with AIS, TIA, and ICH are given in the Table.
Table.
Numbers, Demographics, and Clinical Characteristics of Hospitalized AIS, TIA, and ICH Patients in Germany During the Different Time Periods
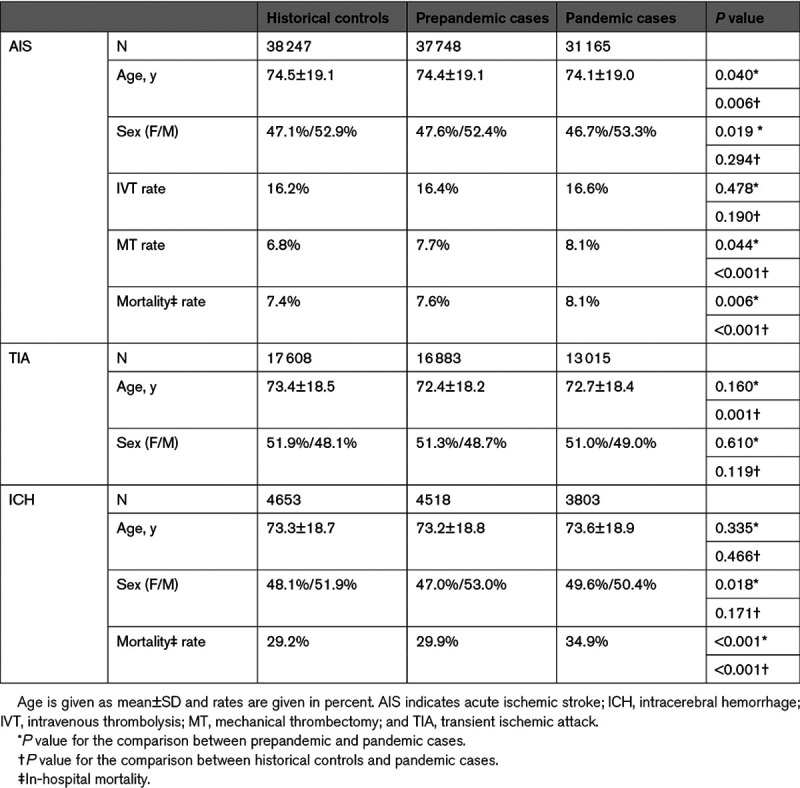
Figure.
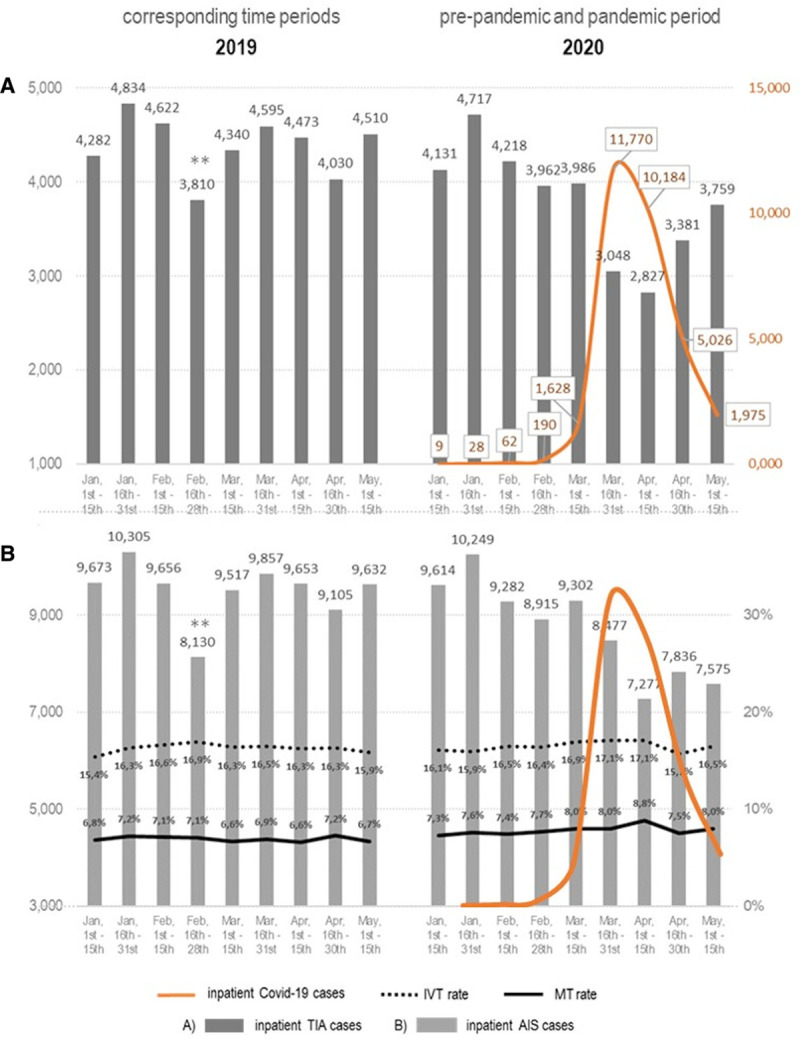
Course of hospital admissions of patients with acute cerebrovascular events. Hospitalized patients with transient ischemic attack (TIA; A) and acute ischemic stroke (AIS; B) are demonstrated as bar graphs representing a 2-wk period. Treatments rates are given in percent. Schematic course of the number of hospitalized coronavirus disease 2019 (COVID-19) cases in Germany is given as curve diagram (orange). Apr indicates April; Feb, February; IVT, intravenous thrombolysis; Jan, January; Mar, March; and MT, mechanical thrombectomy. **The 1–3 days shorter period in second half of February 2019 needs to be considered in this comparison.
Concerning treatment rates in patients with AIS, the absolute numbers of patients receiving IVT markedly decreased (pandemic period: n=5170; prepandemic period: n=6186), paralleling the decline in hospital admissions, while the relative IVT treatment rate (16.6% versus 16.4%, P=0.478; 16.2% in 2019; P=0.190) remained unchanged. The absolute number of MT procedures also decreased during the pandemic, but to a lesser degree (pandemic period: n=2514; prepandemic period: n=2888), resulting in a slight but significant overall increase in the MT treatment rate (8.1% versus 7.7%, P=0.044; 6.8% in 2019, P<0.001; Figure). We found a significantly higher in-hospital mortality in patients with AIS during the pandemic period (8.1%) compared with the prepandemic period (7.6%; P=0.006) and in comparison with the historical controls (7.4%; P<0.001; Table).
Transient Ischemic Attack
There was a massive decrease of 22.9% in hospitalization of patients with TIA during the COVID-19 pandemic (n=13 015) compared to the prepandemic period (n=16 883) and in comparison with the same time period in 2019 (n=17 608; −26.1%). The decrease in TIA patients´ admissions also commenced in the second half of March 2020 (Figure).
Intracerebral Hemorrhage
A relevant decrease of 15.8% was also found for hospital admissions of patients with ICH during the pandemic period (n=3803) compared to the prepandemic period (n=4518; Table). Similar to patients with AIS, we found a significant increase of the in-hospital mortality in patients with ICH during the pandemic (34.9%) compared with the prepandemic period (29.9%, P<0.001).
Discussion
This study represents the first nationwide stroke patient care analysis with almost 100% coverage of all hospitalized patients in a country. We found a profound decline in hospitalizations for all stroke subtypes during the peak phase of the COVID-19 pandemic from March 16 to May 15, 2020, when massive social distancing and lockdown measures were present. The strongest decline in hospitalization was observed in patients with TIA.
A similar trend has been observed in other regions of the world who were affected by the COVID-19 pandemic.7–9 Uchino et al8 found a decline in acute stroke presentations in Ohio, United States, of about 30% from March 9 to April 2, 2020. Hoyer et al9 reported a massive decline particularly for patients with TIA (up to −82%) in four German academic stroke centers. The stronger decline compared with our nationwide data and to other regions of the world is probably attributed to regional variations. However, it is likely that patients were primarily less frequently seeking medical attention during the pandemic due to fear of acquiring COVID-19 during hospitalization. This assumption is supported by the dynamic of the observed decline seen from mid-March 2020 on, when Germany had the first deaths due to COVID-19 and the German government imposed strong measures for social distancing and postponement of elective treatments. A national survey done by the American College of Emergency Physician reported that 74% of the surveyed adults were first and foremost concerned to contract another illness while being at a medical facility during the COVID-19 outbreak.10 Furthermore, it is unlikely that numbers of admissions were influenced by measures to avoid hospitalization since ICU capacities were still underutilized in Germany despite the pandemic situation.11
Concerning acute recanalization treatment rates in patients with AIS, we did not observe a change in the relative rate of IVT treatments during the COVID-19 pandemic, while the relative MT rate did actually slightly increase during the pandemic.9 The IVT rate was comparable to nationwide IVT rates of previous years.12 In a recent regional analysis of the telestroke network in Bavarian, Germany, the colleagues also described an increase for MT recommendations but a decrease for IVT recommendations during the COVID-19 pandemic.3 Our data indicate that provision of acute recanalization treatments in eligible patients with AIS was not affected by the COVID-19 pandemic in Germany as compared to other European countries.13
The relative increase in the MT treatment rate might correspond to the similarly observed higher overall mortality rate in German hospitalized patients with AIS during the pandemic period. We assume that patients with stroke who were hospitalized during the peak phase of COVID-19 pandemic could have had more severe strokes, while primarily patients with TIA and minor stroke did not seek medical help in hospitals. Consistently, other studies have also shown that especially stroke patients with more severe symptoms at admission presented to hospitals during the COVID-19 pandemic.7 Unfortunately, there are no consistent nationwide data available for stroke severity at admission. Alternatively, the somewhat higher MT rate could be part of the steadily rising MT rate in Germany over the last years.3,12 Interestingly, a recently published analysis from 93 Italian Stroke Units also demonstrated a slight increase of endovascular treatment rates during pandemic, while absolute numbers of admissions and treatments were reduced.14
Our nationwide study, including data from a total of 1463 hospitals in Germany, has several strength and limitations. Our data refer to the overall number of hospitalized patients with a main diagnosis of AIS, TIA, and ICH, irrespective of, for example, time of symptom onset, clinical details, or basis of indication for recanalization procedures, such as premorbid functional status, site of vascular occlusion, symptom severity, and comorbidities. Thus, possible confounding is the main limitation of our study. Furthermore, we do not have data on long-term outcome. However, our administrative data have high quality and accuracy because registration of all stroke cases and acute treatment procedures is a prerequisite to get financial compensation and the coding of operating and procedure keys for MT and IVT are closely controlled by medical services of the medical health insurances. The system itself assures that one IVT or MT procedure refers only to one patient with AIS, even if the patient has been transferred to a second hospital for MT. Regarding the data from 2020, the hospitals were forced by law to submit accurate data until July 15, 2020, to enable the government to evaluate the adopted measures for hospitals in times of COVID-19 pandemic. Thus, in contrast to observational registries, our data are very robust as they provide almost 100% coverage of all hospitalized patients in Germany with a very low risk of missing patients or double coding of procedures, resulting in high validity and consistency.15
Conclusions
We found a marked decline in absolute numbers of patients with AIS, TIA, and ICH during the COVID-19 pandemic. Our data suggest that those patients with AIS who did seek acute hospital care during the pandemic were treated with the same high quality as before the pandemic. The decline in case numbers of AIS, TIA, and ICH is most likely attributed to the fear of patients to acquire a severe acute respiratory syndrome coronavirus 2 infection during hospitalization. These data might be helpful to policymakers and health care providers taking decisions on the still ongoing or a future pandemic situation.
Acknowledgments
All authors participated in the study design. Drs Richter and Krogias drafted the article and performed the statistical analysis. Dr Bartig conducted the data abstraction. Drs Eyding, Weber, Grau, and Hacke participated in article revision.
Sources of Funding
None.
Disclosures
Dr Eyding has received travel grants from Boehringer Ingelheim and Bayer Vital and grants for the realization of scientific meetings by Bayer Health Care, Boehringer Ingelheim, Sanofi Aventis, and Pfizer. Dr Weber has received speaker honoraria from Medtronic/Covidien and Bristol-Myers Squibb and from serving on a scientific advisory board of Medtronic. Dr Bartig has received orders for analysis of the German Diagnosis-Related Groups system from Boehringer Ingelheim and Sanofi Aventis. Dr Grau has received public funding by the Innovationsfonds des Gemeinsamen Bundesausschusses. Dr Hacke has received speaker and consultancy honoraria from Boehringer Ingelheim, Medtronic, and Cerenovus and a research grant from Boehringer Ingelheim. Dr Krogias has received speaker honoraria or travel grants for scientific meetings from Bayer Vital and Daiichi Sankyo. The other author reports no conflicts.
Nonstandard Abbreviations and Acronyms
- AIS
- acute ischemic stroke
- COVID-19
- coronavirus disease 2019
- ICD-10
- International Classification of Diseases, Tenth Revision
- ICH
- intracerebral hemorrhage
- MT
- mechanical thrombectomy
- TIA
- transient ischemic attack
This manuscript was sent to Emmanuel Touzé, Consulting Editor, for review by expert referees, editorial decision, and final disposition.
Presented in part at the European Stroke Organisation-World Stroke Organization 2020 Virtual Conference, November 7–9, 2020.
For Sources of Funding and Disclosures, see page 720.
Contributor Information
Daniel Richter, Email: daniel.richter-c34@rub.de.
Jens Eyding, Email: eyding@web.de.
Ralph Weber, Email: ralph.weber@krupp-krankenhaus.de.
Dirk Bartig, Email: dirk.bartig@drg-market.de.
Armin Grau, Email: graua@klilu.de.
Werner Hacke, Email: werner.hacke@med.uni-heidelberg.de.
References
- 1.Deutsche Gesellschaft für Neurologie. Das Phaenomen der leeren Stroke-units waehrend der Corona-Krise. https://dgn.org/neuronews/journal_club/phaenomen-der-leeren-stroke-units-waehrend-der-corona-krise-profchristian-gerloff-sprach-dazu-in-ndr-visite/. Accessed October 10, 2020
- 2.Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, Zaino D, Michieletti E, Guidetti D. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020;83:213–215. doi: 10.1159/000507666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlachetzki F, Theek C, Hubert ND, Kilic M, Haberl RL, Linker RA, Hubert GJ. Low stroke incidence in the TEMPiS telestroke network during COVID-19 pandemic-effect of lockdown on thrombolysis and thrombectomy. J Telemed Telecare. 2020;0:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pop R, Quenardelle V, Hasiu A, Mihoc D, Sellal F, Dugay MH, Lebedinsky PA, Schluck E, LA Porta A, Courtois S, et al. Impact of the COVID-19 outbreak on acute stroke pathways - insights from the Alsace region in France. Eur J Neurol. 2020;27:1783–1787. doi: 10.1111/ene.14316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teo KC, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY, Kwok WM, Leung KK, Tse MY, Cheung RTF, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen-Huynh MN, Tang XN, Vinson DR, Flint AC, Alexander JG, Meighan M, Burnett M, Sidney S, Klingman JG. Acute stroke presentation, care, and outcomes in Community Hospitals in Northern California during the COVID-19 pandemic. Stroke. 2020;51:2918–2924. doi: 10.1161/STROKEAHA.120.031099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uchino K, Kolikonda MK, Brown D, Kovi S, Collins D, Khawaja Z, Buletko AB, Russman AN, Hussain AS. Decline in stroke presentations during COVID-19 surge. Stroke. 2020;51:2544–2547. doi: 10.1161/STROKEAHA.120.030331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoyer C, Ebert A, Huttner HB, Puetz V, Kallmünzer B, Barlinn K, Haverkamp C, Harloff A, Brich J, Platten M, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. 2020;51:2224–2227. doi: 10.1161/STROKEAHA.120.030395 [DOI] [PubMed] [Google Scholar]
- 10.American College of Emergency Physicians. American College of Emergency Physicians COVID-19. https://www.emergencyphysicians.org/globalassets/emphysicians/all-pdfs/acep-mc-Covid19-april-poll-analysis.pdf. Accessed August 19, 2020
- 11.Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin. DIVI Intensivregister. https://www.intensivregister.de/#/intensivregister?tab=laendertabelle. Accessed October 13, 2020. [PubMed]
- 12.Weber R, Eyding J, Kitzrow M, Bartig D, Weimar C, Hacke W, Krogias C. Distribution and evolution of acute interventional ischemic stroke treatment in Germany from 2010 to 2016. Neurol Res Pract. 2019;1:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bersano A, Kraemer M, Touzé E, Weber R, Alamowitch S, Sibon I, Pantoni L. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol. 2020;27:1794–1800. doi: 10.1111/ene.14375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sacco S, Ricci S, Ornello R, Eusebi P, Petraglia L, Toni D; Italian Stroke Organization. Reduced admissions for cerebrovascular events during COVID-19 outbreak in Italy. Stroke. 2020;51:3746–3750. doi: 10.1161/STROKEAHA.120.031293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eyding J, Misselwitz B, Weber R, Neumann-Haefelin T, Bartig D, Krogias C. [Comparability of different data sources on stroke care in Germany]. Nervenarzt. 2020;91:877–890. doi: 10.1007/s00115-020-00989-8 [DOI] [PubMed] [Google Scholar]


