Supplemental Digital Content is available in the text.
Keywords: COVID-19, mortality, pandemic, public health, stroke
Background and Purpose:
The magnitude and drivers of excess cerebrovascular-specific mortality during the coronavirus disease 2019 (COVID-19) pandemic are unknown. We aim to quantify excess stroke-related deaths and characterize its association with social distancing behavior and COVID-19–related vascular pathology.
Methods:
United States and state-level excess cerebrovascular deaths from January to May 2020 were quantified using National Center for Health Statistic data and Poisson regression models. Excess cerebrovascular deaths were analyzed as a function of time-varying stroke-related emergency medical service (EMS) calls and cumulative COVID-19 deaths using linear regression. A state-level regression analysis was performed to determine the association between excess cerebrovascular deaths and time spent in residences, measured by Google Community Mobility Reports, during the height of the pandemic after the first COVID-19 death (February 29).
Results:
Forty states and New York City were included. Excess cerebrovascular mortality occurred nationally from the weeks ending March 28 to May 2, 2020, up to a 7.8% increase above expected levels during the week of April 18. Decreased stroke-related EMS calls were associated with excess stroke deaths one (70 deaths per 1000 fewer EMS calls [95% CI, 20–118]) and 2 weeks (85 deaths per 1000 fewer EMS calls [95% CI, 37–133]) later. Twenty-three states and New York City experienced excess cerebrovascular mortality during the pandemic height. A 10% increase in time spent at home was associated with a 4.3% increase in stroke deaths (incidence rate ratio, 1.043 [95% CI, 1.001–1.085]) after adjusting for COVID-19 deaths.
Conclusions:
Excess US cerebrovascular deaths during the COVID-19 pandemic were observed and associated with decreases in stroke-related EMS calls nationally and mobility at the state level. Public health measures are needed to identify and counter the reticence to seeking medical care for acute stroke during the COVID-19 pandemic.
An excess of all-cause mortality has been observed in the United States during the coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2.1 However, the magnitude and driving factors of cerebrovascular-specific excess mortality have not been described. Excess stroke-related deaths during the pandemic, if any, may be attributable to biology as well as behavior. Biologic factors, such as COVID-associated hypercoagulability and endotheliopathy, may have contributed to higher stroke incidence, which resulted in excess cerebrovascular-related mortality.2–4 Additionally, studies have demonstrated a decrease in hospital presentation for acute stroke symptoms during the pandemic, which is concerning given the established benefits of stroke treatments for acute and long-term outcomes and lower 30-day mortality if treated in an integrated stroke care system.5–9 Government stay-at-home policies as well as the public’s widespread fear of contracting the contagion in a hospital and inundating scarce medical resources may have prompted avoidance of healthcare settings and consequently, more stroke-related deaths.10–12
We analyze cerebrovascular-specific, national, and state-wide mortality rates from the National Center for Health Statistic (NCHS). The goals of this study are to (1) determine the degree of excess cerebrovascular-related mortality in the United States from January 1 to May 16, 2020, compared to prior years, (2) quantify the time-varying relationship between excess cerebrovascular-related mortality and emergency medical service (EMS) calls for stroke-like symptoms as well as COVID-19 incident deaths per week, and (3) identify whether social distancing behavior quantified by increased time spent at home during the first height of the pandemic at the state-level was associated with excess cerebrovascular-related deaths adjusted for cumulative COVID-19–related deaths. We hypothesize that there was excess cerebrovascular-related mortality during the pandemic period. We postulate that excess cerebrovascular deaths during the pandemic were driven by social distancing behaviors leading to less emergency healthcare utilization and consequently greater mortality in addition to direct COVID-19 cerebrovascular pathology (Figure 1).
Figure 1.
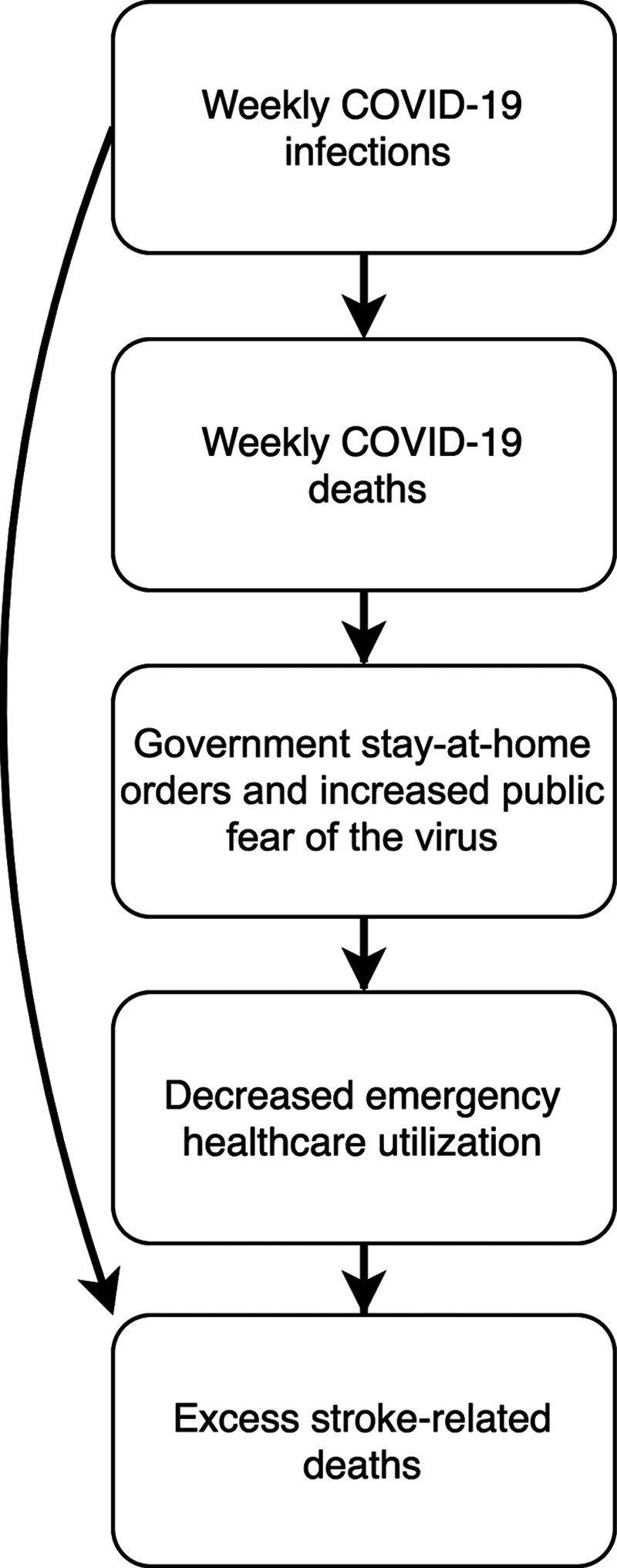
Visual summary of the hypothesized factors associated with excess stroke mortality during the pandemic. We predict that excess stroke-related deaths during the pandemic were secondary to (A) implementation of stay-at-home orders and growing public fear of contracting the virus led to decreased mobility and utilization of emergency healthcare services and (B) direct coronavirus disease 2019 (COVID-19) cerebrovascular pathology.
Methods
Study Design
This is a retrospective, population-based analysis of cerebrovascular-specific mortality in the United States during the COVID-19 pandemic. We studied trends in excess cerebrovascular mortality at a national level from January 1 to May 16, 2020. We analyzed factors associated with excess mortality at the state level from March 1 to May 16, 2020, which we define as the first height of the pandemic because of its association with case fatalities after the first US COVID-19–related death on February 29, 2020. This study was considered exempt from Institutional Board Review due to its utilization of only publicly available, aggregate data sources.
Outcomes
The outcome of interest was predicted excess cerebrovascular mortality, which was calculated using the ExcessILI package created by coauthor, Dr Weinberger.13 Predictions of excess cerebrovascular deaths were generated by fitting Poisson regression models to the weekly counts of state-level, cerebrovascular-specific deaths from 2014 to 2019. Predicted cerebrovascular death counts were then compared with the observed cerebrovascular death counts from January 1 to May 16, 2020, to estimate excess mortality. We used the sum of total excess cerebrovascular deaths in the included geographies for each week from January 1 to May 16, 2020, to estimate weekly, national excess cerebrovascular deaths, and calculated the ratio of observed/predicted cerebrovascular-related mortality for each 2020 calendar week.
Data Sources
Cerebrovascular-specific mortality data from 2014 to 2020 were gathered from the NCHS Mortality Surveillance Data, which are updated biweekly.14 Underlying cause of death is identified using death certificate data from all US deaths provided by state vital statistics offices and is coded using disease-specific International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes. Cerebrovascular disease–related deaths were coded with ICD-10-CM codes I60 to I69, encompassing nontraumatic subarachnoid hemorrhage, intracerebral hemorrhage, and cerebral infarction. Complete data from January 1, 2014 to May 16, 2020, were available in 41 geographies including 40 states and New York City (NYC). New York state and NYC data are mutually exclusive. Alaska, Connecticut, District of Columbia, New Hampshire, North Carolina, North Dakota, Montana, Rhode Island, South Dakota, Vermont, and Wyoming were missing ≈60% of weekly mortality counts and were not included. NCHS data was last updated on June 17 and downloaded on June 23, 2020, to allow for at least a 4-week reporting lag of cause-specific deaths. The weekly sum of the excess counts of stroke-related deaths among included geographies was the outcome of interest in the national analysis. Observed counts of stroke-related deaths offset by predicted stroke-related deaths in each geography were the outcomes analyzed at the state level.
We obtained national-level, EMS utilization data from the National Emergency Medical Services Information System Data Cube, which captures 90% of all EMS calls nationally.15 Weekly, count data were gathered by selecting for any EMS call with a primary provider impression (eSituation.11) of cerebrovascular disease (ICD-10-CM codes I60–I69). Data for each week from January 1 to May 16 in the years 2017 to 2020 were used. National Emergency Medical Services Information System data collection is 75% complete within 17.2 days, and we accessed this data on June 23 to allow for at least 5 weeks of reporting. The weekly counts of national emergency department visits for stroke were abstracted from the National Syndromic Surveillance Program via the Centers for Disease Control, which captures 73% of all emergency room visits nationally.10 Weekly, incident COVID-19 cases and deaths in the United States were obtained from the COVID-Tracking Project.16
The degree of time spent at home in each state was measured using the Google COVID-19 Community Mobility Reports, which reported the percent change in time spent in places of residence for each geography.17 We specifically abstracted this metric on the projected date of peak COVID-19 hospitalizations per geography, predicted by the Institute for Health Metrics and Evaluation,18 as this projection may affect medical care-seeking behavior. Mobility data was used to capture behavioral patterns that may be associated with decreased stroke-related hospital presentations since state-specific EMS data was not publicly available. Weekly counts of COVID-19 deaths were obtained for each state from the COVID-Tracking Project and aggregated from January 1 to May 16, 2020.16 COVID-19 mortality data for NYC was acquired from the NYC Health Department and subtracted from the New York state counts.19 Aggregate counts of COVID-19 deaths were utilized as these are commonly reported in the media, may impact behavior, and reflect the burden of severe COVID-19 within each geography. Finally, the proportion of excess deaths due to pneumonia, influenza, or COVID-19 that were recorded as caused by COVID-19 was included to adjust for differences in death recording practices as COVID-19 may take precedence over stroke.
Statistical Analysis
All analyses were performed using R version 4.0.0.
National Analysis
We assessed the relationships between excess cerebrovascular-specific mortality and the number of stroke-related EMS calls, the primary exposure of interest. Univariable linear regression models were used to test the associations between weekly excess stroke-related mortality and (1) weekly number of stroke-related EMS calls, (2) weekly incident COVID-19 related deaths, and (3) calendar week. We separately explored different time-lagged periods of the EMS calls to evaluate the time-varying effects of changes in EMS call rates on weekly excess cerebrovascular-specific death. One- and two-week lags of weekly EMS calls were created because prior research has demonstrated 2 peaks in the natural history of stroke-related deaths: (1) the first week after ischemic stroke (between days 3–6 after stroke) and intracranial hemorrhage (days 1–3 after hemorrhage) due to herniation and (2) the end of the second week due to complications of immobility such as poststroke pneumonia, pulmonary embolism, and sepsis.20 The association between each covariate and excess stroke-related death was tested in univariable models. Bonferroni-adjusted P values were used to account for multiple testing. Adjusted R2 values were calculated to assess the degree of variance explained by covariates.
As a sensitivity analysis to determine whether the trends we identified for excess cerebrovascular-related deaths and EMS utilization were plausible, we performed all analyses outlined above for excess (1) cardiovascular disease–related death and (2) Alzheimer disease–related deaths. Like cerebrovascular deaths, cardiovascular deaths can be mitigated with timely medical and procedural intervention. We thus hypothesize that excess cardiovascular-related deaths will be significantly associated with lower EMS utilization. Alzheimer deaths may occur due to factors not modifiable by an acute hospitalization, such as changes in goals of care during the pandemic. As such, we hypothesize that the magnitude of the relationship between EMS calls and excess Alzheimer-related deaths will be comparably low.
Cardiovascular (ICD-10-CM codes I00–I09, I11, I13, and I20–I50) and Alzheimer (G30) disease–specific mortality were also gathered from NCHS and observed versus expected counts were compared. We tested the association between the number of cardiovascular disease–specific EMS calls, identified by a primary provider impression of cardiovascular disease (ICD-10-CM codes I00–I09, I11, I13, and I20–I50), and excess cardiovascular mortality, using the same methodology described for the national excess cerebrovascular deaths. Similarly, we also compared the number of EMS calls for all complaints to the number of excess Alzheimer-related deaths since patients living with this chronic neurological diagnosis may develop a new symptom affecting any organ system.
State-Level Analysis
In the state-level analysis of the first height of the pandemic, the state-specific covariates of interest were the degree of reduced movement and the cumulative number of COVID-19 related deaths from January 1 to May 16, 2020. Although many states implemented social distancing and stay-at-home mandates during the pandemic, compliance with these mandates varied. We, therefore, used individual mobility, measured as the percent change in time spent at home, as our exposure variable to capture the true effect of distancing policies. Geography-specific observed counts of cerebrovascular-related deaths from March 1 to May 16, 2020, offset by the expected count of cerebrovascular-related deaths were analyzed using negative binomial regression. We tested the association between cerebrovascular mortality and degree of change in mobility while adjusting for the log-transformed, cumulative number of COVID-19 deaths per population in each geography. To account for completeness of deaths attributed to COVID-19, we also adjusted for the log-transformed proportion of pneumonia and influenza deaths that are coded as secondary to COVID-19 infections.
In a sensitivity analysis, observed cardiovascular and Alzheimer-related deaths by geography, offset by geography-level predictions, were analyzed using the same state-level methodology. Again, given the proven association between emergency medical procedures and cardiovascular survival, we expect a significant association between decreased mobility and excess cardiovascular deaths, even upon adjusting for COVID-related deaths. In contrast, we hypothesize no association between decreased mobility and excess Alzheimer-related deaths since death from this cause may be related to factors other than timeliness of access to emergency medical care.
This analysis will also elucidate whether individuals who died from non-COVID causes during the pandemic also had unreported COVID-19 infections, which may underlie an observed association between mobility and cause-specific death (Figure 1). Although the incidence of stroke among COVID-19 infected patients is 0.9% and the incidence of myocardial injury is 28% among COVID-19 patients,21,22 there is no known biologic link between Alzheimer disease and COVID-19 infections. Thus, if a strong association is observed between time spent at home and Alzheimer-related deaths, this may indicate that individuals with Alzheimer-related deaths, and by methodologic extension, other cause-specific deaths including cerebrovascular deaths, may have had comorbid and unreported COVID-19 infections.
Data Availability
All data are publicly available. The ExcessILI R package can be accessed at https://github.com/weinbergerlab/ExcessILI.
Results
Of 52 states and cities, 40 states and NYC reported complete mortality data and were included in the analysis.
National Analysis
There were 918 more cerebrovascular deaths than expected from January 1 to May 16, 2020. The percent change in observed stroke-related mortality compared with expected ranged from −4.9% (95% CI, −9.8% to −0.4%) to 2.9% (95% CI, −3.3% to 6.9%) from January 1 to February 29; however, starting from March 1 onwards, the range shifted to -3.4% (95% CI, −9.5 to 1.5) to a peak of 7.8% (95% CI, 1.6–13.5) occurring the week of April 18 (Figure 2). The observed/expected stroke-related mortality ratios were positive throughout the weeks of March 28 to May 2 (Table I in the Data Supplement).
Figure 2.
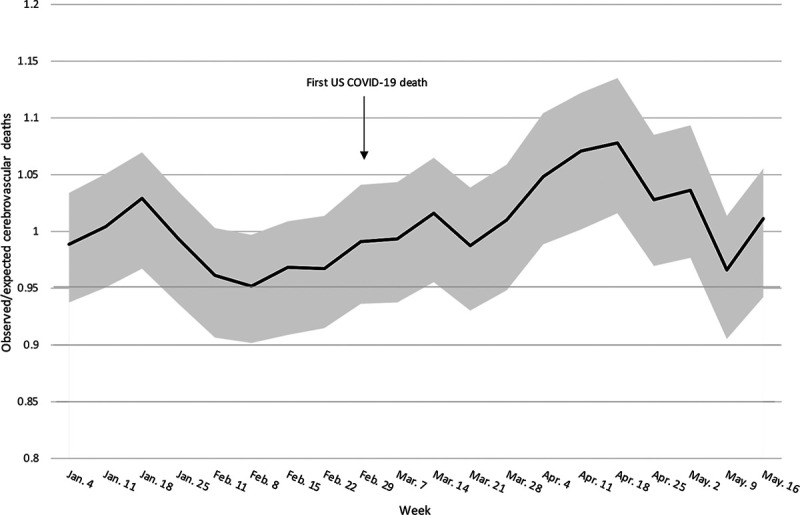
Increase in national excess cerebrovascular mortality during the coronavirus disease 2019 (COVID-19) pandemic. Observed divided by expected counts for each week in the study period±95% prediction interval.
National estimates of excess cerebrovascular-related deaths, stroke-related EMS calls and emergency department visits, and COVID-19 deaths, transformed by a factor of 10, are visualized in Figure 3. A 2-week rolling average was applied to the cerebrovascular-related death curve for the purpose of visualization. The number of EMS calls for cerebrovascular-related symptoms declined by 23%, from 7666 calls in the week of February 29 to 5805 calls in the week of April 11, and then plateaued. There were excess cerebrovascular deaths in the pandemic era starting the week of March 14, increasing through the week of April 18, and decreasing thereafter. During the week of March 14 when there were excess stroke-related deaths, there were only 37 incident COVID-19 deaths. The slope of weekly incident COVID-19 deaths increased quickly and was steepest from March 28 to April 18. These trends demonstrate that the first occurrence of excess cerebrovascular-related death occurred 2 weeks after EMS stroke-related calls began to decline and when COVID-19 deaths were relatively low. Comparisons between the weekly counts of national EMS calls for cerebrovascular disease in each year from 2017 to 2020 are shown in Figure I in the Data Supplement. A negative association between calendar week and counts of EMS calls for cerebrovascular disease was observed in 2020 only (β coefficient [β], −92.83 [95% CI, −151.58 to −34.08]; Table II in the Data Supplement). In univariable linear regression analysis, fewer EMS calls for cerebrovascular-related symptoms was associated with greater excess cerebrovascular deaths one (β, −69.2 deaths per 1000 EMS calls [95% CI, −117.9 to −20.4], adjusted R2=0.3, Table) and 2 weeks later (β, −84.8 deaths per 1000 EMS calls [95% CI, −132.9 to −36.6, adjusted R2=0.4, Table). Additionally, weekly incident COVID-19 deaths were associated with greater excess cerebrovascular deaths (β, 10.6 deaths per 1000 COVID-19 deaths [95% CI, 3.8–17.3]).
Figure 3.
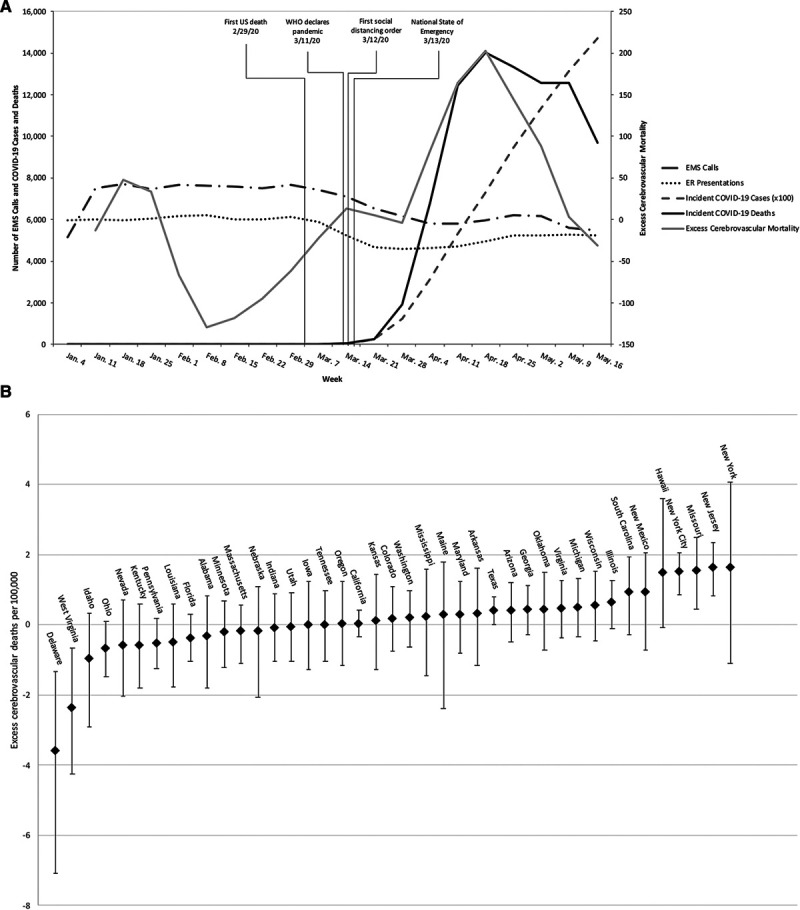
National and state-level excess cerebrovascular disease–related mortality. A, National counts of cerebrovascular disease–related emergency medical service (EMS) calls and emergency room (ER) presentations, and weekly coronavirus disease 2019 (COVID-19) deaths are plotted on the primary y axis. Excess cerebrovascular mortality as point estimates and as a 2-wk rolling average are plotted on the secondary y axis. B, The total number of excess deaths from March 1–May 16 in each geography and associated 95% CIs are plotted on the y axis. WHO indicates World Health Organization.
Table.
Univariable Linear Regression Models of National Excess Cerebrovascular, Cardiovascular, and Alzheimer-Related Mortality
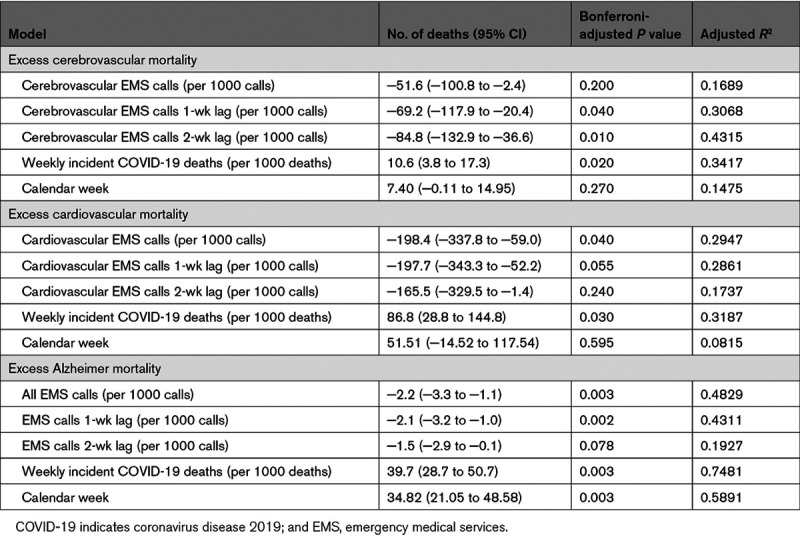
There were 6367 more cardiovascular and 2910 more Alzheimer deaths than expected from January 1 to May 16, 2020. We found a similar association between cardiovascular-specific deaths and cardiovascular-related EMS calls. Fewer EMS calls for cardiovascular symptoms were associated with greater excess cardiovascular mortality contemporaneously (β, −198.4 deaths per 1000 EMS calls [95% CI, −337.8 to −59.0], adjusted R2=0.3, Table, Figure II in the Data Supplement). A positive association was also noted between cardiovascular-specific deaths and weekly incident COVID-19 deaths (β, 86.8 deaths per 1000 COVID-19 deaths [95% CI, 28.8–144.8], adjusted R2=0.32).
In contrast to cerebrovascular and cardiovascular deaths, there was an association of low magnitude between the total number of EMS calls for all complaints and Alzheimer-related mortality (β: −2.2 deaths per 1000 EMS calls [95% CI, −3.3 to −1.1). There were positive relationships noted between Alzheimer-related death and both weekly COVID-19 deaths (β, 39.7 deaths per 1000 COVID-19 deaths [95% CI, 28.7–50.7], adjusted R2=0.75) as well as calendar week (β: 34.82 [95% CI, 21.05–48.58], adjusted R2=0.59).
State-Level Analysis
During the first height of the pandemic from March 1 to May 16, 23 states and NYC, experienced excess cerebrovascular mortality (Figure 3B, Table III in the Data Supplement). Observed stroke-related mortality was elevated by 19.4% (95% CI, 8.9–30.3) in New Jersey, 14.6% (95% CI, 3.9–25.6) in Missouri, and 29.8% (95% CI, 14.6–44.7) in NYC. In univariable analyses, there was an association between the increase in stroke deaths and the percent change in time spent at home (incidence rate ratio per 10% increase in time spent at home: 1.061 [95% CI, 1.026–1.096]) in each geography (Figure 4). Cerebrovascular mortality was also associated with the total number of COVID-19 related deaths per geography (incidence rate ratio, 1.020 [95% CI, 1.001–1.039]). In the multivariable negative binomial regression model, the change in time spent home remained positively associated with cerebrovascular mortality from March 1 to May 16 (incidence rate ratio per 10% increase, 1.043 [95% CI, 1.001–1.085]) while adjusting for cumulative COVID-19 deaths and the estimated completeness of COVID-19 death reporting.
Figure 4.
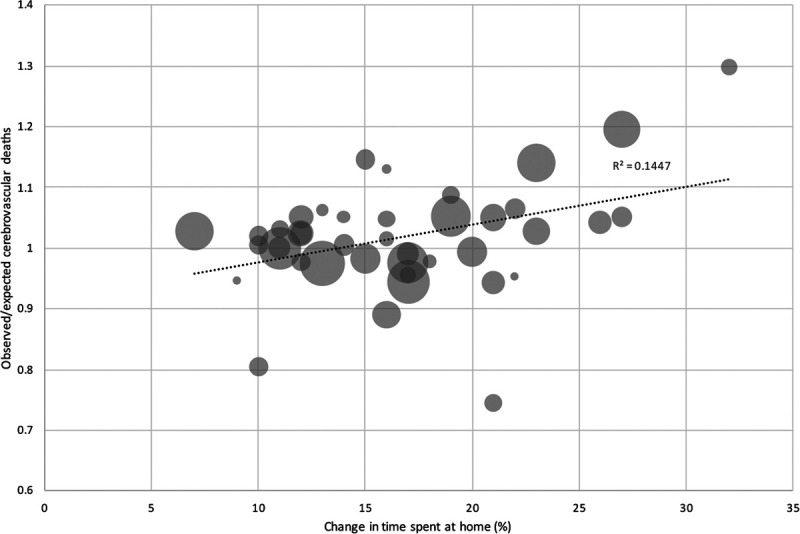
Associations between time spent at home and cerebrovascular mortality during the height of the coronavirus disease 2019 (COVID-19) pandemic by geography. The ratio of observed divided by expected cerebrovascular deaths in each geography are presented as a function of the percent change in time spent at home. The size of the bubbles represents the inverse variance in the expected counts of cerebrovascular deaths. Larger bubbles indicate greater certainty in the estimate.
Similarly, excess geography-level cardiovascular mortality during the pandemic height was associated with percent change in time spent at home in unadjusted and adjusted analyses (adjusted incidence rate ratio per 10% increase, 1.050 [95% CI, 1.012–1.080], Table IV in the Data Supplement). In contrast, there was no significant association between time spent at home and excess geography-level Alzheimer-related mortality during the height of the pandemic (Table V in the Data Supplement).
Discussion
In this population-based study, we analyzed national and state-level cerebrovascular-related excess mortality during the COVID-19 pandemic. Excess cerebrovascular-related deaths occurred in the United States from the last week of March through May 16, 2020. In univariate analyses, decreased utilization of EMS for cerebrovascular-related symptoms was associated with increased rates of cerebrovascular-related mortality one and 2 weeks later. Weekly excess stroke-related deaths were also positively associated with COVID-19 deaths. During the first height of the pandemic, decreased mobility from home residence was associated with excess stroke mortality, independent of the cumulative number of COVID-19 related deaths. Although we observed increased stroke-related deaths associated with increased time spent at home, distancing measures have been critical in mitigating COVID-19-related deaths, which far outnumber stroke-related deaths. This study emphasizes the need to seek emergency medical attention for stroke within the COVID-19 response construct.
We observed a rise in US stroke-related mortality that was temporally correlated with a decline in EMS calls for stroke symptoms in 2020. In the national analysis, excess stroke deaths were associated with a decrease in seeking EMS care one and 2 weeks before stroke-related death. Strokes due to large vessel occlusions and sizable hemorrhage tend to cause mass effect and herniation within the first week. Death 2 weeks after stroke is often due to secondary complications, such as recurrent stroke, systemic thrombosis, or infections, such as aspiration pneumonia.20 A subcortical lacune may be as likely associated with complications such as aspiration pneumonia as strokes due to large vessel occlusions,23 suggesting heterogeneity in stroke subtype among patients who died. The importance of timely presentation for acute stroke is well-established. Prevention, monitoring, and treatment of poststroke complications result in improved early survival. The risk of long-term mortality increases after an incident stroke, compounding the potential implications of avoiding early care.24 Stroke workup and secondary stroke prevention measures are routinely implemented during hospitalization. Before the pandemic, these processes were incrementally improved (ie, 3341 hospitals participated in Get-With-The-Guidelines Stroke Registry in 2020 compared with 2247 in 2019), resulting in decreased mortality in early 2020 compared with prior years. During the pandemic, emergency stroke teams were ready to manage potential stroke, but these systems were underutilized, likely resulting in excess stroke-related deaths possibly due to secondary complications from stroke.25
The national trend in excess stroke mortality and decreased EMS utilization during the height of the pandemic aligns with the observation of excess stroke mortality in states where more individuals practiced social distancing and decreased their mobility. Although we did not have public access to state-level EMS data, it is conceivable that a mandate, either personal or societal, to socially isolate and decrease mobility to prevent contagion may deter patients and their caregivers from seeking EMS care during the pandemic. Social network constriction is a known risk factor of delay in EMS activation during stroke.26 In the context of COVID-19, multidimensional psychosocial mechanisms could have affected stroke patients and caregivers including fear amplification, less recognition due to fewer witnesses, or increased negotiation within social networks.27 These processes may have been exaggerated due to stay-at-home policies, schools and work closures, and transportation restrictions, in which the percent of individuals leaving their residence plummeted.28 Such measures in geographies where they were implemented resulted in significant flattening of the curve of new cases and coronavirus-related deaths.29 However, one unintended consequence may be an increase in stroke-related deaths due to residents being encouraged to decrease mobility. This may also be a driving factor for patients with milder stroke symptoms not seeking EMS care, and further study of this hypothesis is needed. It is imperative that the public be urged to seek emergency care if acute neurological symptoms occur for life-saving and time-sensitive treatment and informed that seeking care is not a violation of stay-at-home initiatives.
The sensitivity analysis of excess mortality due to cardiovascular and Alzheimer-related causes augments the validity of the association noted in this study between excess cerebrovascular deaths and the degree of time spent at home. Given the correlation between COVID-19–related deaths and decreased mobility by geography in our data (β, 2.7 per COVID-19 deaths per 100 000 population, P=0.0001, adjusted R2 0.2956) and the link between COVID-19 and cerebrovascular pathology noted in the literature, it is conceivable that excess cerebrovascular-related deaths were in fact attributable to undiagnosed COVID-19 infections as a confounder rather than distancing behaviors.30–32 A similar pattern emerged in our analysis of excess cardiovascular mortality, which was studied since it is analogous to cerebrovascular mortality in terms of acuity and its link with COVID-19 infection. In contrast, our analysis of deaths due to a chronic disease process, Alzheimer disease, revealed no association between increased time at home and excess Alzheimer disease–related death. We would not expect an excess of Alzheimer deaths directly due to COVID-19 since there has not been a biologic connection observed between these 2 diseases. Excess Alzheimer deaths may have been due to changes in goals of care and alterations in the fragile system of caregiving during the pandemic. The lack of an association between increased time at home and Alzheimer deaths argues against undiagnosed COVID-19–related pathology inordinately confounding the association between distancing behaviors and cerebrovascular-related mortality.
Our study has several limitations. Our analysis relies on NCHS mortality data, which is affected by underreporting. NCHS reports data at a 2-week delay but recent data may remain incomplete for some time. To allow at least 1 month for data reporting, we limited our analysis to May 16 and used data updated on June 17. Due to data missingness, we were unable to evaluate cerebrovascular mortality in all states. Thus, our national analysis does not capture all deaths, and state-level analyses may be skewed by geographies with more thorough mortality reporting. It is possible that the cause of death reported by NCHS may be misclassified. We were also unable to know how many stroke-related deaths concurrently carried a COVID-19 diagnosis. Similarly, EMS calls for cerebrovascular disease were identified using the provider’s primary impression, which may not always capture true stroke events. As EMS data was not publicly available on a state-wide level, we were unable to identify state-specific changes in EMS call rates. In addition, we were not able to assess local changes in behavior or distancing policies, which also may have affected mobility and EMS utilization. However, this potential source of confounding is attenuated by the fact that local distancing policies would likely be ultimately translated to changes in time spent at home. Lastly, our study only captures a truncated portion of 2020, and we were not able to analyze mortality in the weeks after the initial peak of the pandemic.
Conclusions
Excess cerebrovascular deaths correlated with both a national decline in EMS utilization for stroke symptoms and weekly incident COVID-19–related deaths. Increases in time spent at home predicted excess stroke deaths at the state-level, even upon adjusting for COVID-19 related deaths. Our results suggest that during the pandemic, social distancing behavioral changes may have been a factor in the decrease in seeking medical care for acute, life-threatening conditions like stroke, resulting in excess cerebrovascular-related deaths. We emphasize the need to seek emergency medical attention for stroke symptoms within the construct of the COVID-19 response.
Acknowledgments
We sincerely thank Dr Mary G. George, at the Center for Disease Control within the Division for Heart Disease and Stroke Prevention, for her valuable input and guidance on this analysis. Dr Sharma, L.R. Kuohn, and Dr Sheth conceptualized and designed the study. Dr Sharma and L.R. Kuohn acquired and analyzed data. Dr Sharma, L.R. Kuohn, Drs Weinberger, Warren, Sansing, Jasne, Falcone, Dhand, and Sheth interpreted data. Dr Sharma, L.R. Kuohn, and Dr Sheth prepared the article. Drs Weinberger, Warren, Sansing, Jasne, Falcone, and Dhand reviewed and edited the article.
Sources of Funding
None.
Disclosures
Dr Weinberger reports receiving grants from Pfizer and the National Institute of Allergy and Infectious Diseases (R01AI137093) and personal fees from Pfizer, Merck, GlaxoSmithKline, and Affinivax outside the submitted work. Dr Sansing is supported by NIH (U01NS113445, R01NS097728, R01NS095993) and AHA (19EIA34770133). Dr Falcone is supported by the National Institutes of Health (K76AG059992 and R03NS112859), the American Heart Association (18IDDG34280056), the Yale Pepper Scholar Award (P30AG021342), and the Neurocritical Care Society Research Fellowship. Dr Dhand reports personal fees for expert testimony outside of the submitted work. Dr Sheth is supported by the NIH (U24NS107136, U24NS107215, R01NR018335, R01NS107215, U01NS106513, R03NS112859), the American Heart Association (18TPA34170180, 17CSA33550004), and grants from Hyperfine Research Inc, Bard, Biogen, and Novartis; personal fees from Zoll; personal fees from Ceribell; and other support from Alva outside the submitted work. These funding sources had no role in design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; and decision to submit the article for publication. The other authors report no conflicts.
Supplemental Materials
Figures I–II
Tables I–V
Supplementary Material
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
- EMS
- emergency medical service
- ICD-10-CM
- International Classification of Diseases, 10th Revision, Clinical Modification
- NCHS
- National Center for Health Statistic
- NYC
- New York City
*Drs Sharma and Kuohn contributed equally.
This article was sent to Marc Fisher, Senior Consulting Editor, for review by expert referees, editorial decision, and final disposition.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.120.031975.
For Sources of Funding and Disclosures, see page 571.
Contributor Information
Lindsey R. Kuohn, Email: lindseykuohn@gmail.com.
Daniel M. Weinberger, Email: Daniel.weinberger@yale.edu.
Joshua L. Warren, Email: Joshua.warren@yale.edu.
Lauren H. Sansing, Email: lauren.sansing@yale.edu.
Adam Jasne, Email: adam.jasne@yale.edu.
Guido Falcone, Email: guido.falcone@yale.edu.
Amar Dhand, Email: adhand@bwh.harvard.edu.
Kevin N. Sheth, Email: kevin.sheth@yale.edu.
References
- 1.Weinberger DM, Chen J, Cohen T, Crawford FW, Mostashari F, Olson D, Pitzer VE, Reich NG, Russi M, Simonsen L, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan CW, Low JGH, Wong WH, Chua YY, Goh SL, Ng HJ. Critically ill COVID-19 infected patients exhibit increased clot waveform analysis parameters consistent with hypercoagulability. Am J Hematol [Internet]. 2020;95:E156–E158. doi: 10.1002/ajh.25822. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262023/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, Baluha A, Bar N, Bona RD, Burns AJ, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, Henninger N, Trivedi T, Lillemoe K, Alam S, et al. SARS2-CoV-2 and stroke in a New York Healthcare System [published online May 20, 2020]. Stroke. 2020;51:2002–2011. doi: 10.1161/STROKEAHA.120.030335. https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.030335. Accessed June 5, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uchino K, Kolikonda MK, Brown D, Kovi S, Collins D, Khawaja Z, Buletko AB, Russman AN, Hussain MS. Decline in stroke presentations during COVID-19 surge. Stroke. 2020;51:2544–25470. doi: 10.1161/STROKEAHA.120.030331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Man S, Xian Y, Holmes DN, Matsouaka RA, Saver JL, Smith EE, Bhatt DL, Schwamm LH, Fonarow GC. Association between thrombolytic door-to-needle time and 1-year mortality and readmission in patients with acute ischemic stroke. JAMA. 2020;323:2170–2184. doi: 10.1001/jama.2020.5697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ganesh A, Lindsay P, Fang J, Kapral MK, Côté R, Joiner I, Hakim AM, Hill MD. Integrated systems of stroke care and reduction in 30-day mortality: a retrospective analysis. Neurology. 2016;86:898–904. doi: 10.1212/WNL.0000000000002443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charidimou A, Friedrich JO, Greenberg SM, Viswanathan A. Core cerebrospinal fluid biomarker profile in cerebral amyloid angiopathy: a meta-analysis. Neurology. 2018;90:e754–e762. doi: 10.1212/WNL.0000000000005030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, Schieve LA, Imperatore G, Benoit SR, Kite-Powell A, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:795–800. doi: 10.15585/mmwr.mm6925e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsh JD. The Mystery of ‘Excess Fatality’. Intelligencer. 2020 https://nymag.com/intelligencer/2020/04/coronavirus-is-only-part-of-the-excess-fatality-mystery.html. Accessed June 5, 2020.
- 12.Avoiding the hospital over coronavirus fears could be leading to deaths, ER doctor says. https://www.cbsnews.com/news/coronavirus-hospital-avoid-deaths-non-covid-19-patients/. Accessed June 5, 2020.
- 13.weinbergerlab/ExcessILI. GitHub. https://github.com/weinbergerlab/ExcessILI. Accessed June 5, 2020
- 14.Calgary O. Weekly Counts of Deaths by State and Select Causes, 2019-2020. Centers for Disease Control and Prevention. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/muzy-jte6. Accessed June 5, 2020.
- 15.EMS Data Cube. NEMSIS. https://nemsis.org/view-reports/public-reports/ems-data-cube/. Accessed June 5, 2020
- 16.The COVID Tracking Project. The Atlantic Monthly Group. https://covidtracking.com/. Accessed June 5, 2020
- 17.Google COVID-19 Community Mobility Report. https://www.google.com/covid19/mobility?hl=en. Accessed June 5, 2020
- 18.COVID-19 Projections. Institute for Health Metrics and Evaluation. http://www.healthdata.org/covid. Accessed June 5, 2020
- 19.nychealth/coronavirus-data. GitHub. https://github.com/nychealth/coronavirus-data. Accessed June 5, 2020
- 20.Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke. 2011;42:3214–3218. doi: 10.1161/STROKEAHA.110.610881 [DOI] [PubMed] [Google Scholar]
- 21.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286 [DOI] [PubMed] [Google Scholar]
- 23.Armstrong JR, Mosher BD. Aspiration pneumonia after stroke: intervention and prevention. Neurohospitalist. 2011;1:85–93. doi: 10.1177/1941875210395775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rutten-Jacobs LC, Arntz RM, Maaijwee NA, Schoonderwaldt HC, Dorresteijn LD, van Dijk EJ, de Leeuw FE. Long-term mortality after stroke among adults aged 18 to 50 years. JAMA. 2013;309:1136–1144. doi: 10.1001/jama.2013.842 [DOI] [PubMed] [Google Scholar]
- 25.AHA/ASA Stroke Council Leadership. Temporary emergency guidance to US Stroke Centers during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. 2020;51:1910–1912. doi: 10.1161/STROKEAHA.120.030023 [DOI] [PubMed] [Google Scholar]
- 26.Dhand A, Luke D, Lang C, Tsiaklides M, Feske S, Lee JM. Social networks and risk of delayed hospital arrival after acute stroke. Nat Commun. 2019;10:1206.doi: 10.1038/s41467-019-09073-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mantica G, Riccardi N, Terrone C, Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020;183:40–41. doi: 10.1016/j.puhe.2020.04.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lasry A, Kidder D, Hast M, Poovey J, Sunshine G, Winglee K, Zviedrite N, Ahmed F, Ethier KACDC Public Health Law Program. Timing of community mitigation and changes in reported COVID-19 and community mobility―four U.S. metropolitan areas, February 26–April 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:451–457. doi: 10.15585/mmwr.mm6915e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood). 2020;39:1237–1246. doi: 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- 30.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. doi: 10.1172/JCI137244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blum A, Vaispapir V, Keinan-Boker L, Soboh S, Yehuda H, Tamir S. Endothelial dysfunction and procoagulant activity in acute ischemic stroke. J Vasc Interv Neurol. 2012;5:33–39. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are publicly available. The ExcessILI R package can be accessed at https://github.com/weinbergerlab/ExcessILI.


