Abstract
Objectives
To show that circulation of SARS-COV-2 in nursing homes in France can come from staff as well as residents’ families, whether they are known or not to have had COVID-19.
Methods
This study reports a screening campaign of asymptomatic staff working in elderly nursing homes in Paris where the virus had been circulating actively in March and April 2020.
Results
Before the screening campaign, the rate of symptomatic COVID-19 was 23.3% among the residents and 12.1% among their home employees. Within a 72 h screening period, all employees not known to have the virus were screened by RT-PCR in nasopharyngeal swabs. Among the 241 screened employees, 32 (13.3%) tested positive for SARS-CoV-2 on RT-PCR. SARS-CoV-2 carriers and non-carriers did not differ in term of gender, age or type of staff. Staff carrying SARS-CoV-2 were strictly asymptomatic in 75% of cases while during the days following or before the test, 25% presented mild symptoms of COVID-19. Considering both symptomatic and asymptomatic cases, 66 out of 281 (23.5%) of the home employees had been carriers for COVID-19.
Conclusion
Screening for viral carriage of asymptomatic staff in nursing homes can avoid contact and transmission to frequently severely vulnerable residents.
Keywords: Nursing homes, SARS COV-2, asymptomatic carriers, COVID-19, staff workers
Abbreviations
- COVID-19
Coronavirus Disease 2019
- CT
Cycle Threshold
- RT-PCR
real time polymerase chain reaction
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus-2
1. Introduction
The COVID epidemic has highlighted the extreme vulnerability of the elderly to the SARS-CoV-2 virus. In France, senior residential care homes paid a particularly heavy toll to the COVID-19 epidemic: more than half of COVID-19 deaths were those of elderly residents in nursing homes. Between March 1 and April 30, 2020, according to Santé Publique France (the French public health agency) there were 54,493 cases of COVID-19 among residents of nursing homes in France, and 6517deaths [1]. Care home workers were also very strongly impacted by COVID-19; in the same survey, 18,936 COVID-19 cases were reported among their staffs [1].
These institutions were not prepared to deal with the epidemic. Containment, public health measures and social distancing were difficult to implement for residents often wandering and used to living together. Moreover, nursing homes for dependent elderly people were initially sorely lacking in suitable protective equipment.
In addition, COVID-19 diagnosis in the elderly is difficult insofar as they often develop atypical forms with digestive symptoms (vomiting, diarrhea) or confusion in the forefront and coughing in the background.
Despite the gradual arrival of personal protective equipment, the implementation of very strict public health and containment measures, and a ban on visits as of March 11, 2020, the SARS coronavirus 2 continued to spread in nursing homes in France.
Persistent circulation of the virus led the government to decide on large-scale screening in nursing homes. In an initial phase, all care home residents were to be screened for the virus, the objective being to isolate those who were carrying the virus.
During a second phase, all nursing home workers not known to have had COVID-19 were encouraged to get tested, the objective being to assess the risk of virus importation by non-virus-free staff.
This study reports the first screening phase of asymptomatic staff working in four elderly care nursing homes in Paris connected with the centrally located Paris hospitals (Groupe Hospitalier Paris Centre) in which the virus had been reported to be actively spreading in March and April.
2. Methods
All employees of the four nursing homes who had not previously been tested positive for SARS-CoV-2 RT-PCR and who had not raised strong clinical suspicion of COVID-19 were proposed for participating in an employee screening study.
COVID-19 cases were considered as confirmed in case of (1) virological confirmation of SARS-CoV-2 infection in nasopharyngeal swabs; and/or (2) CT-scan results typical for COVID-19 pneumonia; and/or (3) prior contact with a virologically confirmed case and at least two major symptoms of COVID-19 (fever ≥ 38 °C, cough, pulmonary parenchymal disease, shortness of breath, anosmia/ageusia); and probable in case of strong clinical suspicion based on (1) at least three major symptoms or (2) two major and 2 minor symptoms (aches, sore throat, runny nose, headache, prolonged asthenia, chills, odynophagia, diarrhea, vomiting, cutaneous signs) or 1 major and three minor symptoms.
All employees gave oral consent to participate in this study. All participants, whatever their function, were screened at the COVID-19 screening center in the Hôtel-Dieu Hospital in Paris within a maximum 72-hour screening period. Search for RNA of the SARS-CoV2 virus was carried out by rhinopharyngeal swab and by RT-PCR (Elitech assay, ELITech Group, Puteaux, France). Viral load was expressed by Cycle Threshold (CT) values to provide a semi-quantitative assessment of SARS-CoV2 viral load. As recommended by the SFM [2], the amount of virus present at the nasopharyngeal level was considered moderate or low in case CT between 33 and 37 for at least 2 targets, significant in cases of CT ≤ 33 for at least 2 targets, and negative in case of CT ≥ 37.
Comparisons between characteristics of the different nursing-homes were made with χ2. Characteristics of positive and negative SARS-CoV-2 RT-PCR employees were compared with χ2 for categorical variables and T-test for continuous variables. All analyses were two-sided and a P-value < 0.05 was considered statistically significant. Data analysis was performed using R software version 3.2.3.
3. Results
The four nursing homes (NH) participating in this study were located in Paris (NH of Péan (NH1), Amitié et Partage (NH2), Antoine Portail (NH3) and les Gobelins (NH4). The general characteristics of the nursing homes are summarized in Table 1 .
Table 1.
Description of elderly care home facilities.
| Variables, % (N) | Whole sample |
Nursing home 1 |
Nursing home 2 |
Nursing home 3 |
Nursing home 4 |
P |
|---|---|---|---|---|---|---|
| N = 241 | N = 84 | N = 54 | N = 52 | N = 51 | ||
| Age (years), M (SD) | 39.9 (11.0) | 39.1 (10.7) | 42.6 (11.7) | 39.1 (10.1) | 39.5 (11.6) | 0.26a |
| Women | 83.8 (202) | 84.5 (71) | 83.3 (45) | 82.7 (43) | 84.3 (43) | 0.99 |
| Types of staff | ||||||
| Medical staff | 2.5 (6) | 2.4 (2) | 1.9 (1) | 0 | 5.9 (3) | 0.01 |
| Nurses and nursing assistants | 62.7 (151) | 72.6 (61) | 53.7 (29) | 67.3 (35) | 51.0 (26) | |
| Allied health professionals | 6.2 (15) | 3.6 (3) | 7.4 (4) | 9.6 (5) | 5.9 (3) | |
| Clerical staff | 8.3 (20) | 8.3 (7) | 5.6 (3) | 11.5 (6) | 7.8 (4) | |
| Environmental service staff | 13.7 (33) | 3.6 (3) | 22.2 (12) | 11.5 (6) | 23.5 (12) | |
| Food service staff | 5.0 (12) | 8.3 (7) | 3.7 (2) | 0 | 5.9 (3) | |
| Volunteers | 1.7 (4) | 1.2 (1) | 5.6 (3) | 0 | 0 |
% (N), percentage (count); M (SD), mean (standard deviation). *P-value from χ2 comparing the 4 nursing home groups.
P-value from analysis of variance.
Before the screening campaign, all of the nursing homes had already confirmed cases of COVID-19 among their residents, with an infection rate of 23.3% (77/330) and an infected staff rate of 12.1% (40/263) (Table 2 and Fig. 1 ).
Table 2.
Description of SARS-CoV2 RT-PCR results across the 4 nursing homes.
| Variables | Whole sample | Nursing home 1 | Nursing home 2 | Nursing 3 | Nursing home 4 | P1 |
|---|---|---|---|---|---|---|
| Status before the screening campaign | ||||||
| Number of residents | 330 | 94 | 73 | 70 | 93 | |
| Confirmed or probable COVID-19 | 23.3% (77/330) | 26.2% (25/94) | 4.1% (3/73) | 31.4% (22/70) | 29.0% (27/93) | < 0.0001 |
| Number of staff members | 281 | 100 | 63 | 62 | 56 | |
| Confirmed or probable COVID-19 | 12.1% (34/28154) | 10% (10/100) | 14.3% (9/63) | 16.1% (10/62) | 8.9% (5/56) | 0.54 |
| Screening campaign among staff members | ||||||
| SARS-Cov2 tested staff members | 241 | 84 | 54 | 52 | 51 | |
| Positive RT-PCR | 13.3% (32/241) | 17.9% (15/84) | 9.3% (5/54) | 7.7% (5/52) | 15.7% (8/51) | 0.39 |
| Mean CTa | 29.83 (13.39–36.97) | 27.70 (15.03–36.97) | 35.04 (34.70–35.93) | 35.42 (34.95–35.94) | 26.28 (13.39–31.23) | |
| Totally asymptomatic | 75.0% (24/32) | 11 | 3 | 5 | 6 | |
| Mild symptoms during or after the campaign | 25.0% (8/32) | 4 | 2 | 0 | 2 | |
| Total staff members with SARS-Cov2 infection | 23.5% (66/281) | 25% (25/100) | 22.2% (14/63) | 24.2% (15/62) | 23.2% (13/56) | 0.98 |
P-values from χ2 comparing the 4 nursing home groups.
Median cycle threshold in PCR positive samples.
Fig. 1.
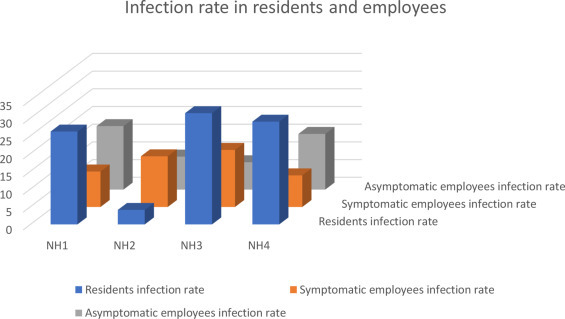
SARS-COV-2 infection rate in residents and in employees in four nursing homes in Paris, France.
Between April 16, 2020 and April 29, 2020, testing was proposed for all asymptomatic or pauci-symptomatic NH employees at the Hôtel-Dieu screening center and 100% (n = 241) agreed to participate.
Among the 241 staff members, 32 (13.3%) persons tested positive for SARS-CoV-2 by RT-PCR. There was a non-significant difference in SARS-CoV-2 carriage prevalence between nursing homes, ranging from 9.3% to 17.9% (Table 2 and Fig. 1).
There was no significant difference between SARS-CoV-2 carriers and non-carriers in terms of gender, age and type of staff (Table 3 ).
Table 3.
Characteristics of the nursing-home employees participating in the screening campaign according to SARS-CoV2 RT-PCR results.
| Variables, %(N) or M (SD) | Whole sample | SARS-CoV2 RT-PCR |
P | |
|---|---|---|---|---|
| Negative |
Positive |
|||
| N = 241 | N = 209 | N = 32 | ||
| Age (years) | 39.9 (11.0) | 39.7 (11.1) | 41.3 (11.0) | 0.47 |
| Women | 83.8 (202) | 83.7 (175) | 84.4 (27) | 0.99 |
| Types of staff | ||||
| Medical staff | 2.59 (6) | 2.9 (6) | 0 | 0.36 |
| Nurses and nursing assistants | 62.7 (151) | 61.2 (128) | 71.9 (23) | |
| Allied health professionals | 6.2 (15) | 6.2 (13) | 6.3 (2) | |
| Clerical staff | 8.3 (20) | 9.6 (20) | 0 | |
| Environmental service staff | 13.7 (33) | 13.9 (29) | 12.5 (4) | |
| Food service staff | 5.0 (12) | 4.3 (9) | 9.4 (3) | |
| Volunteers | 1.7 (4) | 1.9 (4) | 0 | |
| Viral load, M (SD) | 30.1 (7.2) | |||
| Low | 59.6 (19) | |||
| Moderate | 25.0 (8) | |||
| High | 15.6 (5) | |||
| Totally asymptomatic | 75.0 (24) | |||
| Mild COVID-19 symptomsa | 25.0 (8) | |||
P-value from χ2 comparing negative vs. positive PCR groups
during the days after the campaign
In 75.0% of cases staff carrying SARS-CoV-2 had been strictly asymptomatic from the beginning of the pandemic until the screening survey, while 25.0% had presented, or presented in the days following the test, mild symptoms of COVID-19, such as headache, fatigue and runny nose (Table 3).
The amount of virus present at the nasopharyngeal level was moderate or low (CT between 33 and 37) in 14 (41.3%) cases, and significant (CT ≤ 33) in 17 (58.6%). Mean SARS-CoV-2 load was 29.83 (SD = 7.2) and did not differ significantly across the four institutions. Subjects with significant SARS-CoV2 load experienced mild COVID-19 symptoms in 40% (2 out of 3), while subjects with mild or moderate SARS-CoV-2 load experienced mild COVID-19 symptoms in 22.2% (6 out of 27) (P = 0.53).
4. Discussion
Our results show 13.3% of asymptomatic or pauci-symptomatic carriage of SARS-CoV2 in nursing-home employees during the 1st wave of 2020 COVID-19 pandemic.
This asymptomatic carriage prevalence is of the same order as that found during the epidemic on the Diamond Princess cruise ship [17.9% (95% CI = 15.5–20.2%)] [3] but much lower than that found in other regions of France where the virus was not highly circulating [4].
Higher prevalence was found in China among people evacuated from Wuhan (China), Italy or during the epidemic in Oise (France) [5], [6], [7]. In our series, the lower prevalence found in the EHPADs compared to the previous series, may attest to the fact that the virus had already widely spread among staff members, or else be a consequence of the adoption of stricter and more effective barrier measures. It also bears mentioning that the survey was carried out at a time when the PCR test had just been rendered available in France and that employees had in median only one test performed during this period.
All types of nursing home employees, independently of their functions, were similarly affected by SARS-CoV-2,. Interestingly enough, employees not in close contact with residents were no less affected than nurses and MDs.
Viral load at the nasopharyngeal level was considered as low in 41.3% of the cases and significant in 58.6% [2]. These high levels of viral load could present a risk of transmission to residents, their relatives and to other employees.
Of note, the NH2 nursing home, which had the lowest number of infected residents (4% vs. 23% on average) at the end of the 1st wave, had implemented stricter and earlier prevention rules (mask wearing from the 1st case on 14/03/2020, social distancing facilitated by the existence of two buildings with a dedicated team in each building, ample space for breaks, early awareness of caregivers of the need to be tested in case of symptoms). On the other hand, median viral load by institution was similar across the four facilities.
Screening for viral carriage of asymptomatic staff in nursing homes is therefore necessary in order in view of avoiding contact and transmission between these carriers and residents, who are often exceedingly vulnerable. Cases of asymptomatic SARS-CoV-2 virus carriage justify temporarily medical leave with isolation and precautions for at least 7 days after SARS-COV-2 detection [8]. Evaluation of the duration of SARS-CoV-2 carriage in an asymptomatic person and their capacity to develop a protective immune response should also be considered.
If the virus keeps spreading in France over the months to come, the question will arise as to whether to repeat this screening at regular intervals.
Upcoming availability of serological tests will facilitate determination of persons already in contact with the virus, thereby allowing for combined approaches and limiting repeated screening of those who have not been in contact with the virus.
Our limitations are linked to the small study size and to the fact that when it took place, diagnosis of SARS COV-2 infection was based solely on virological RT PCR on swabs, potentially leading to underestimation of the prevalence of SARS-COV-2 infection. However, the participation of all employees, whatever their function, ensured precise assessment of asymptomatic carriage in nursing homes and showed that all staff members were liable to transmit the virus to the residents or to their coworkers.
In conclusion, the virus had been circulating in nursing hommes in France for several weeks and this may well have been partially due to viral carriage by asymptomatic staff members lacking in adequate protective equipment. Our study demonstrates the usefulness of screening asymptomatic nursing home staff for viral carriage, the objective being to avoid contact and transmission of the virus to frequently severely vulnerable residents.
Human and animal rights
The authors declare that the work described has been carried out in accordance with the Declaration of Helsinki of the World Medical Association revised in 2013 for experiments involving humans as well as in accordance with the EU Directive 2010/63/EU for animal experiments.
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patient(s) and/or volunteers.
Disclosure of interest
The authors declare that they no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data sharing statement
No additional data available.
Authors’ contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
Conceptualization: DS, CB, RL and DC; Data management: DS, ES, DC Formal analysis: JSV, DS, CB, OH; Methodology: DS, OH EB Supervision: DS; Validation, DS, ES Writing–original draft: all
Acknowledgements
The authors would like to thank the directors of the four nursing homes who participated in this study: Mrs Romy LASSERRE, Mr François Philippon, Mrs Maud GUILHOT, and Mrs Samia Houari. We thank all the staff who participated in the study. We thank Marie Pierre Pietri and Yannie Cuvillier for technical assistance.
References
- 1.Santé Publique France. COVID 19 point epidemiologique du 21 mai 2020; doi: https://www.santepubliquefrance.fr/content/download/254170/2609369. Accessed May 26, 2020
- 2.Avis du 25 septembre 2020 de la Société Française de Microbiologie FM relatif à l’interprétation de la valeur des Ct (estimation de la charge virale) obtenue en cas de RT-PCR positive sur les prélèvements cliniques réalisés à des fins de diagnostiques ou de dépistage. https://www.sfm-microbiologie.org/covid-19-fiches-et-documents-sfm.
- 3.Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guery R., Delaye C., Brule N., Nael V., Castain L., Raffi F., et al. Limited effectiveness of systematic screening by nasopharyngeal RT-PCR of medicalized nursing home staff after a first case of COVID-19 in a resident. Med Mal Infect. 2020 doi: 10.1016/j.medmal.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ. 2020;368:m1165. doi: 10.1136/bmj.m1165. [DOI] [PubMed] [Google Scholar]
- 6.Nishiura H., Kobayashi T., Miyama T., Suzuki A., Jung S., Hayashi K., et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fontanet A., Tondeur L., Madec Y., Grant R., Besombes C., Jolly N., et al. Cluster of COVID-19 in northern France: A retrospective closed cohort study. medRxiv. 2020 doi: 10.1101/2020.04.18.20071134. [Not peer reviewed] [DOI] [Google Scholar]
- 8.Ameli.fr. Isolement: principes généraux. https://www.ameli.fr/assure/covid-19/isolement-principes-et-regles-respecter/isolement-principes-generaux.


