Abstract
A substantial body of research has illuminated psychological adaptations motivating pathogen avoidance, mechanisms collectively known as the behavioral immune system. Can knowledge about these mechanisms inform how people respond to widespread disease outbreaks, such as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [coronavirus disease 2019 (COVID-19)] pandemic? We review evidence suggesting that the evolutionary history of the behavioral immune system, and the cues that activate it, are distinct in many ways from modern human experiences with pandemics. Moreover, the behaviors engaged by this system may have limited utility for combating pandemic diseases like COVID-19. A better understanding of the points of distinction and points of overlap between our evolved pathogen-avoidance psychology and responses to pandemics may help us realize a more precise and intervention-ready science.
Keywords: behavioral immune system, infectious disease, evolution, social psychology, health
A Cautionary Guide to Pandemic Research
As a result of the worldwide severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [coronavirus disease 2019 (COVID-19)] pandemic, research on the psychology of infectious disease has leapt from niche topic to the center of myriad investigations. Many of these recent investigations focus on the behavior of the uninfected: how people assess infection threats, what promotes preventive actions, when downstream effects on decision-making emerge, and so on [1., 2., 3.]. Much of this work has focused on broad social psychological concepts such as identity and authority [4,5], whereas other work has drawn from frameworks aimed at specifically explaining how humans avoid infectious disease [6,7]. The human pathogen-avoidance literature illuminates many of the mechanisms involved in detecting, processing, and reacting to cues of infection risk, making it a seemingly promising source of knowledge for explaining behavior during this pandemic. But is this promise realized? How well can existing knowledge about pathogen avoidance inform our understanding of responses to pandemics?
As a cautionary guide for those wishing to apply research insights more broadly, we present historical, ecological, and perceptual reasons to expect that the pathogen-avoidance mechanisms we possess may not always be relevant to how people navigate and respond to dangers associated with pandemics like COVID-19. We follow with a discussion of how attending to these points of distinction might help realize a more precise and intervention-ready psychological science of infectious disease.
Insights from the Behavioral Immune System
The behavioral immune system (BIS) literature provides the most comprehensive body of research on pathogen-avoidance and other psychological responses to infectious disease threats [8,9]. Unlike work examining the consequences of infection, and unlike perspectives emphasizing responses to putative domain-general threats (e.g., threatening perceptions of control) [10,11], this framework focuses on sensory and motivational systems functionally specialized for avoiding infection [12., 13., 14.].
Because certain aspects of the physical and social environment provide more information about infection risk than do others, the behavioral immune system exhibits input specificity (e.g., toward features connoting risk, such as lesions and bodily fluids, and transmitting behaviors, such as coughs and sneezes) [15,16]. Similarly, because infection prevention is better facilitated by certain reactions, these mechanisms also show output specificity (e.g., avoidance-oriented emotions such as disgust and anxiety) [17., 18., 19.]. Further, infection threats are often ambiguous (a cough can result from allergies or from communicable influenza) and the costs of avoidance are typically small compared with the costs of infection. The behavioral immune system therefore exhibits an overgeneralization bias toward features resembling infection symptoms (e.g., facial disfigurements) [20,21]. Finally, individual and situational differences exist in activation of certain (but not all) [22] behavioral immune processes, with activation strengthening after exposure to verbal, visual, or olfactory pathogen cues [23., 24., 25.].
A rapidly expanding literature has revealed the implications of these aspects of the behavioral immune system for phenomena ranging from political ideology [26,27] to intergroup relations [24,28], to psychopathology [29., 30., 31.]. Even so, the behavioral immune system framework might have more limited application to pandemics than researchers realize. A brief review of the psychological literature indicates the relevance of this concern. As of November, 2020 (9 months into the COVID-19 pandemic), approximately 30 published papers and preprints have applied behavioral immune logic to studies of COVID-19 (e.g., [5,7,32., 33., 34.]). Explicit attention to the issues discussed here should help researchers seeking to use an understanding of the evolved psychology of pathogen avoidance in their work by: (i) identifying which, and when, aspects of this framework are relevant to understanding responses to COVID-19; and (ii) improving precision in study designs. To achieve these goals, we next detail areas of fit and misfit between the types of information and reactions applicable to the behavioral immune system and to pandemics, focusing explicitly on COVID-19, though we expect many of these points are relevant for respiratory diseases that share similar properties.
Connecting the Behavioral Immune System to Pandemics
Areas of Fit
Intuition suggests that pathogen-avoidance mechanisms should play some role in human behavior during pandemics. Many inputs to these mechanisms are indeed involved in the spread of COVID-19, including direct (e.g., fluids expelled from the body) and indirect indicators of transmission likelihood (e.g., prior contact between objects and potentially sick individuals). Detection of such cues during the current pandemic should engage mechanisms documented in the behavioral immune system literature.
The same is true for certain outputs of pathogen-avoidance mechanisms. For example, avoiding physical contact with people and the objects they touch represent goals of anti-COVID-19 public health campaigns as well as the behavioral immune system [21,35]. Such avoidance can take many forms. Findings from the behavioral immune system literature suggest that people from areas of the world with higher infectious-disease burdens tend to be less open to new experiences and innovations [36,37] and more oriented toward traditional norms and ideologies [38]. Similarly, studies from the USA and the Netherlands indicate that those who are more disgusted by pathogen cues are also less open to new experiences [37,39]. Such tendencies might be useful in managing many pandemic threats.
Despite these points of similarity, many of the cues, problems, and solutions involved in responding to certain pandemics diverge from those associated with an evolved psychology of pathogen avoidance. Some of these issues have been discussed previously in the behavioral immune system literature (see our discussion of parasite stress theory later); others are novel to the current situation. What does the behavioral immune system miss with respect to pandemics like COVID-19?
Areas of Misfit: Historical Issues
Animals across taxa possess behavioral immune systems, each specialized for different ecologies, life histories, mating systems, and diets. The human behavioral immune system is specialized for the conditions humans faced over hundreds of thousands of years, including low-density subsistence societies with close-knit kin structures and an omnivorous diet, among other things. Many salient features of our modern society depart from these conditions. Manhattan holds approximately 27 000 people per square kilometer; Manila holds approximately 46,000. A coronavirus that hops from a non-human animal to a human for the first time in China can wreak havoc upon New York a mere 4 months later, transmitted by asymptomatic individuals who themselves are transported across the world in less than a day. Hence, mechanisms tailored for defending against pathogens in preindustrial, small-scale conditions might be poorly equipped to deal with the infection threats of a densely populated, globally interconnected world. This idea of a mismatch between modern and ancestral environments is broadly applicable to human psychology [40., 41., 42.] and health [43., 44., 45.] and it is critical for interpreting behavioral immune responses. To the extent that modern environments correspond with ancestral ones, pathogen-avoidance mechanisms can continue to fulfill their functions, sometimes even more successfully due to cultural transmission about which cues are diagnostic. Yet, many aspects of modern industrialized life relevant to pathogen transmission differ from those in the environments that shaped evolution of the behavioral immune system.
Perhaps most critically, pandemics are civilized events (that is, they are events of civilization). They require both the aggregation and regular geographic movement of significant numbers of individuals, conditions greatly exacerbated by the development of farming, cities, and extensive trade routes [46]. Over the last ten millennia, the spread of pandemics has been facilitated by increases in population density and social complexity, contact with animal vectors such as rodents and mosquitoes that swelled in numbers due to agricultural land transformation and unhygienic living conditions (e.g., bubonic plague), broadly shared utilization of resources such as contaminated water (e.g., cholera), sexual interaction with partners that moved between diffuse social networks (e.g., HIV, syphilis), and exhalation of respiratory droplets in contexts more socially dense and physically enclosed than any we inhabited while mobile hunter-gathers (e.g., smallpox, measles, influenza) (see: https://www.visualcapitalist.com/history-of-pandemics-deadliest/).
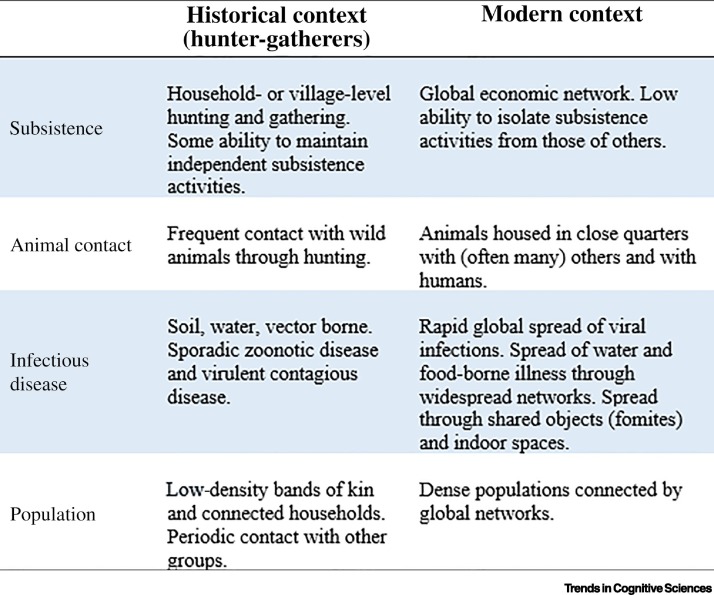
Several observations suggest that, because multiple features of ancestral small-scale societies did not afford the types of pandemics observed in recent centuries (Figure 1 ), selection is unlikely to have shaped pandemic-specific mental mechanisms. First, small-scale societies hold fewer people with less geographic and intergroup mobility than do larger societies. For diseases with longer initial asymptomatic periods, pathogens could have spread through an entire group before signs of illness were exhibited. With especially virulent pathogens, small groups may have faced extinction before transmission between groups could occur. Pathogens that did spread between groups likely would have been less virulent, perhaps with extended latency periods (e.g., Mycobacterium tuberculosis) [47] or periods of dormancy due to propagation through insect vectors, environmental reservoirs, or zoonotic reserves (e.g., helminths, Cryptosporidium).
Figure 1.
Key Features of Ancestral and Modern Contexts for Infectious Disease Spread.
Second, routes of transmission would have been more limited in the past. For example, many modern infectious diseases spread via fomites [48]: objects that transmit pathogens through prior contact with infected people. Fomites may have played some role in the evolution of behavioral immune reactions, as suggested by evidence for the universality of contact-based contagion beliefs [49]. But amongst hunter-gatherers, material goods were comparatively limited. Those available would have been extensively shared within families or bands (e.g., shared food processing instruments), but unlike today, few public fomites (e.g., public computers or doors) were present to facilitate transmission between strangers.
Finally, pathogenic agents themselves differ from those common in preagricultural, small-scale societies. The ratio of macroparasites (e.g., schistosomes), many of which are transmitted through vectors rather than through person-to-person contact or proximity, to disease-causing microbes would have been relatively higher in those societies [50]. And prior to the broad adoption of farming, zoonotic disease transmission was characterized by incidental infections from hunting or other animal interactions, rather than by sustained close contact with domesticated animals who are themselves housed in artificially dense populations [51]. With a few exceptions (e.g., HIV), sporadic interactions would have limited the ability for pathogens to evolve specializations for human hosts, even though such pathogens occasionally cause outbreaks (e.g., Ebola) [52]. In addition to spreading through different pathways, other features distinguish parasitic diseases from bacterial or viral illnesses. Many macroparasites, for example, cannot replicate inside a host. Instead, they require an external life stage for reproduction, making infection load a consequence of continuous exposure, not initial exposure. Thus, unlike pathogens, macroparasites and their vectors are much less likely to behave as contaminants in which small exposures cause serious disease.
These three features suggest that the behavioral immune system evolved to navigate conditions that differ in some ways from those associated with pandemic diseases. Could recent selection have tuned behavioral immune system responses to better fit pandemic conditions? Most known examples of recent human evolution involve simple genetic polymorphisms (e.g., lactase persistence), or shuffling of additive genes that contribute to a continuous trait (e.g., skin color). Complex functional adaptations are expected to involve many unique, nonadditive genes and so take much longer to evolve. Further, unlike single polymorphisms, which have diverged across human populations, psychological mechanisms of the behavioral immune system appear to be relatively universal [49,53], suggesting recent evolutionary history has not caused levels of divergence seen with simpler traits.
Areas of Misfit: Proximate Issues
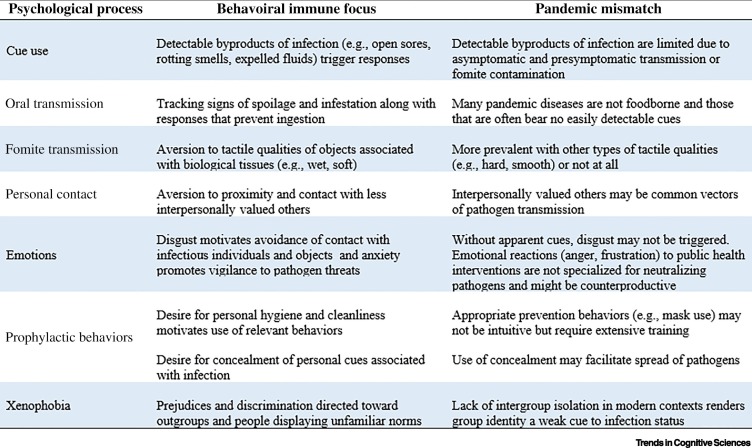
The behavioral immune system attunes us to specific content and facilitates specialized responses when pathogen cues are detected. This specificity does not always align well with public behavior and health knowledge about the transmission and mitigation of respiratory pandemics such as COVID-19. Consider the following examples (also see Figure 2 ).
Figure 2.
Mismatches between Pathogen-Avoidance Responses and Respiratory Pandemic Factors.
Cue Use
Pathogens are difficult to detect. Byproducts of infection (e.g., coughs, sneezes, rashes) are used as cues, despite false positive errors made in response to noninfectious ailments and conditions (e.g., allergies) [15,54,55]. However, infected individuals are often contagious before illness symptoms emerge and some never develop illness symptoms at all [56]. Whereas an infected lesion presents colors and textures that trigger a pathogen-avoidance response, the respiratory droplets expelled during a conversation with an asymptomatic COVID-19 carrier are effectively invisible to our pathogen-detection mechanisms (see: https://theconversation.com/how-the-coronavirus-escapes-an-evolutionary-trade-off-that-helps-keep-other-pathogens-in-check-140706). Similar issues arise when pathogens are transmitted via fomite contamination, water (as with cholera), or difficult-to-detect vectors (e.g., fleas and bubonic plague). Instead, information about many pandemic diseases is typically gleaned from sources outside of our specialized pathogen-detection mechanisms, via experts, leaders, and the media.
Oral Transmission
Disgust elicited by the sight and smell of bacterially contaminated foods prevents ingestion and subsequent infection. Because most pandemic diseases (including COVID-19) are not spread through food, this set of psychological mechanisms do little to defend against such diseases. In fact, most foodborne diseases in industrialized societies (e.g., those involving Escherichia coli-contaminated vegetables or Salmonella-contaminated meats) do not readily trigger pathogen-avoidance reactions, as food with relevant cues is discarded before it reaches the table.
Fomite Transmission
Specialized pathogen-avoidance mechanisms promote aversions to contact with objects and people characterized by specific features. For instance, wet and soft items are unpleasant to touch, presumably due to their sensory resemblance to biological tissues [57]. Pathogen-avoidance mechanisms also produce devaluation of items in prior contact with others, but cues to this contact must be obvious (e.g., used clothing) [58]. Although most COVID-19 infections do not appear to result from fomite transmission, fomites can transmit coronaviruses and influenza [59,60], which have caused past, and will presumably cause future, pandemics.
Personal Contact
Although the behavioral immune system outputs motivations to avoid infection-risky social contact, it relaxes such motivations during some contact rituals (e.g., handshakes) [61] and with targets of high interpersonal value, such as family, friends, and romantic partners [62]. Such targets are as likely to carry infections as strangers, yet people embrace the type of contact with close others that would be aversive with less valued others. Refusing to hug close others, or shake their hands, may even be interpreted as rude, in part, because it implies that an individual is not sufficiently valued to risk infection. Of course, people also avoid contact because they are motivated not to infect others, but this motivation is unlikely to be an output of the behavioral immune system and instead may require higher-order understanding of infection risk or changes in social norms facilitating a mutual understanding of the meaning of avoidance.
Emotions
The proximate emotions underlying pathogen avoidance include disgust and anxiety [63,64]. The former is specialized for avoiding infectious microbes and is triggered by the presence of sensory information associated with microbial action [19,57]; the latter is a general response to threat that promotes vigilance to personal dangers [65., 66., 67.]. Both emotional states inhibit some routes of transmission. However, many of the routes through which COVID-19 is transmitted (e.g., invisible respiratory droplets from asymptomatic individuals) do not involve cues that elicit emotions like disgust. And though people may commonly experience anxiety about aspects of this pandemic, many other emotional reactions associated with the COVID-19 crisis (e.g., anger, frustration, depression) likely do not serve pathogen-avoidance functions.
Xenophobia
Studies suggest that exposure to, and disgust toward, pathogen cues is associated with greater negativity toward foreigners and immigrants [23,68]. The behavioral immune system may have evolved to sometimes treat outgroup membership as a cue to infectiousness [26,69], but substantial debate exits regarding the plausibility of this interpretation [70,71] as well as about which cues produce negativity against which groups under which circumstances [24,28,72,73]. Regardless, xenophobia directed against group identity markers is unlikely to prevent disease transmission in modern contexts because many racial and cultural groups are not geographically or socially isolated, making group identity only a weak correlate of infection risk.
Where Do We Go from Here?
The disjunctions that exist between behaviors well-suited for neutralizing pandemic diseases and the motivations outputted by our functionally specialized pathogen-avoidance psychology might imply that the behavioral immune system is obsolete for the current pandemic battle, as effective as a longbow would be in modern military combat. Imagine, though, the likely spread of COVID-19 without the behavioral immune system; if we embraced contact with strangers as readily as we did with our children or closest friends, or if we experienced no aversion toward feverish faces or the liquid spewing from someone’s mouth during a sneeze. Even so, the inherent vulnerabilities of this system, such as relaxed avoidance around loved ones and an inability to detect asymptomatic carriers, leave us just vulnerable enough to allow pandemics to flourish.
Though much of our discussion has cautioned against reflexively applying behavioral immune thinking to psychological responses to pandemics, similar caution is warranted when considering whether observations during the COVID-19 pandemic provide good tests of behavioral immune hypotheses. The behavioral immune system literature is replete with suggestions that ethnocentrism and ideological conservatism serve pathogen-avoidance functions [26,74,75]. Indeed, following the spread of COVID-19, reports have suggested an epidemic of prejudice against Chinese nationals and individuals of East-Asian descent in the USA and Western Europe (see: https://www.hrw.org/news/2020/05/12/covid-19-fueling-anti-asian-racism-and-xenophobia-worldwide#), with reciprocal prejudice against Westerners and Africans in China (see: https://www.abc.net.au/news/2020-04-09/coronavirus-intensifies-anti-foreigner-sentiment-in-china/12128224). At the same time, in the USA, ideologically conservative Republicans have been much less concerned about the pandemic than more liberal Democrats (see: https://www.pewresearch.org/politics/2020/06/25/republicans-democrats-move-even-further-apart-in-coronavirus-concerns/). In fact, political affiliation appears to be one of the strongest predictors of precautions taken against COVID-19 spread [5]. Should different reactions to COVID-19 from liberals versus conservatives be interpreted as undermining earlier behavioral immune work? Or should reports of increased ethnocentrism be interpreted as confirming behavioral immune work? In both cases, strong inferences may be premature. First, the USA represents only one (possibly unique) data point in the political analysis, with more widespread research needed. Second, the informational inputs most relevant to the behavioral immune system are likely quite different from the types of information commonly provided about the current pandemic, leading to different types of outcomes. For instance, verbal information about the case-fatality risks and viral reproduction numbers of COVID-19 bear little similarity to the sensory and affectively laden information that researchers have used to test pathogen-avoidance hypotheses of ethnocentrism [24,68,76]. We should expect the latter types of information to influence only those people exposed to that information (e.g., those who have spent time with sick individuals). And, though masks are indeed prophylactic, their use likely stems more from trust in health experts and normative pressures than whatever processes give rise to the greater disgust sensitivity among conservatives than liberals. Identifying the causes and functions of pandemic behaviors is thus a necessary precursor to mapping these behaviors onto pathogen-avoidance mechanisms.
Further, mechanistic accounts for how COVID-19 leads to pathogen-avoidance responses will be critical. As an example of the need to understand psychological mechanisms, consider the parasite stress literature, which has highlighted covariation between the prevalence of infectious disease within nations and national averages in religiosity, aggression, and personality, among other variables [77]. People in nations with more infectious disease are more religious [78], but the mechanisms producing these outcomes have yet to be clarified. Areas with more infectious disease might be less hospitable to the development of effective secular institutions [79], religious norms could be better transmitted and maintained in such areas for other reasons, or individual-level psychological mechanisms could detect ecological pathogens during development and output a more religious phenotype. Even if this last account is correct, the precise information extracted from the environment to estimate parasite stress is unclear. Moreover, focusing on patterns at the level of national averages obscures processes that can generate very different patterns at the level of individuals [80,81]. For COVID-19 research to avoid the pitfalls that characterize parasite stress work, clear mechanistic accounts of how and why the pandemic affects behavior will be important.
Interventions designed to improve preventative behaviors during this pandemic might also benefit from attention to differences between how information has been provided about COVID-19 and how pathogen threat cues have been presented in laboratory research. Many public health recommendations intended to promote prophylactic behaviors highlight statistics about rates of spread, mortality, and so forth (see: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/us-cases-deaths.html). As evidenced by the eventual need of governments to implement restrictions requiring these behaviors, such recommendations are not especially effective. Instead, public health officials might consider leveraging cues relevant to the behavioral immune system; motivations to engage in prophylactic behaviors increase following exposure to visual and olfactory pathogen cues [39,82., 83., 84.]. Examining the suitability of such work for large-scale implementation might lead to more effective interventions. For instance, mask-wearing might be better encouraged by messages featuring visual representations of snot spewing from one person and speckling the face of another. Of course, the goals of such interventions must be balanced against other potential consequences of behavioral immune activation (e.g., negative reactions to other people and social situations).
Concluding Remarks
What role does pathogen-avoidance psychology play in pandemics? Here, we have highlighted how pandemic diseases differ from the more common infectious diseases that have shaped the evolution of our antipathogen psychological defenses. These differences suggest caution when applying insights from the pathogen-avoidance literature to aid understanding of responses to pandemics such as COVID-19. Of course, this caution need not preclude researchers from addressing the interplay between relevant mechanisms and contexts. Indeed, many empirical questions remain regarding the extent to which prior findings and models will usefully inform our understanding of pandemic responses (see Outstanding Questions).
Outstanding Questions.
What mechanistic accounts of psychological responses to pandemic diseases such as COVID-19 are supported by data? Such accounts should include information about social norms, governmental pressures, and other relevant influences in addition to those related to disease-specific cues.
How does the behavioral immune system interact with coalitional and political psychology?
What role does social information play in activating or suppressing behavioral immune responses? What happens when these contradict one another?
How should researchers treat differences between the psychological outcomes produced by behavioral immune research and those that emerge during pandemics such as COVID-19? Do such differences stem from mismatches between ancestral cues and features of modern disease spread, or do they provide evidence against existing hypotheses of how pathogens influence behavior?
Do any similarities in ‘downstream’ effects flowing from both the behavioral immune system and pandemics, such as potential increases in ethnocentrism and xenophobia, reflect similar underlying processes or do they stem from distinct causes?
Can insights from the behavioral immune literature be used to develop useful interventions against pandemic disease spread?
Alt-text: Outstanding Questions
Finally, we note that the cautions emphasized here are not only relevant to pandemics and pathogen avoidance. The conceptual logic underlying functionally specialized mental mechanisms suggests that problems can arise when researchers are quick to apply models developed about a particular type of psychology to situations that appear superficially similar. By carefully considering the specific adaptive dilemmas and relevant contextual factors associated with psychological mechanisms, we may realize a more precise and intervention-ready science.
References
- 1.Betsch C. Monitoring behavioural insights related to COVID-19. Lancet. 2020;395:1255–1256. doi: 10.1016/S0140-6736(20)30729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang J. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Bavel J.J. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 5.Samore T. Of pathogens and party lines: social conservatism positively associates with COVID-19 precautions among Democrats but not Republicans. PsyArXiv. 2020 doi: 10.31234/osf.io/9zsvb. Published online August 8, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karwowski M. When in danger, turn right: does COVID-19 threat promote social conservatism and right-wing presidential candidates. Hum. Ethol. 2020;35:37–48. [Google Scholar]
- 7.Makhanova A., Shepherd M.A. Behavioral immune system linked to responses to the threat of COVID-19. Pers. Individ. Diff. 2020;167:110221. doi: 10.1016/j.paid.2020.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray D.R., Schaller M. The behavioral immune system: implications for social cognition, social interaction, and social influence. In: Olson J.M., Zanna M.P., editors. Vol. 53. Academic Press; 2016. pp. 75–129. (Advances in Experimental Social Psychology). [Google Scholar]
- 9.Schaller M. The behavioural immune system and the psychology of human sociality. Philos. Trans. R. Soc. B Biol. Sci. 2011;366:3418–3426. doi: 10.1098/rstb.2011.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greenberg J. Terror management theory of self-esteem and cultural worldviews: empirical assessments and conceptual refinements. In: Zanna M.P., editor. Vol. 29. Academic Press; 1997. pp. 61–139. (Advances in Experimental Social Psychology). [Google Scholar]
- 11.Landau M.J. Compensatory control and the appeal of a structured world. Psychol. Bull. 2015;141:694. doi: 10.1037/a0038703. [DOI] [PubMed] [Google Scholar]
- 12.Ackerman J.M. The behavioral immune system: current concerns and future directions. Soc. Personal. Psychol. Compass. 2018;12 [Google Scholar]
- 13.Kavaliers M., Choleris E. The role of social cognition in parasite and pathogen avoidance. Philos. Trans. R. Soc. B Biol. Sci. 2018;373:20170206. doi: 10.1098/rstb.2017.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tybur J.M., Lieberman D. Human pathogen avoidance adaptations. Curr. Opin. Psychol. 2016;7:6–11. [Google Scholar]
- 15.Michalak N.,.M. Sounds of sickness: Can people identify infectious disease using sounds of coughs and sneezes? Proc. R. Soc. B Biol. Sci. 2020;287:20200944. doi: 10.1098/rspb.2020.0944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kurzban R., Leary M.R. Evolutionary origins of stigmatization: the functions of social exclusion. Psychol. Bull. 2001;127:187. doi: 10.1037/0033-2909.127.2.187. [DOI] [PubMed] [Google Scholar]
- 17.Oaten M. Disgust as a disease-avoidance mechanism. Psychol. Bull. 2009;135:303. doi: 10.1037/a0014823. [DOI] [PubMed] [Google Scholar]
- 18.Duncan L.A. Perceived vulnerability to disease: Development and validation of a 15-item self-report instrument. Personal. Individ. Differ. 2009;47:541–546. [Google Scholar]
- 19.Tybur J.M. Microbes, mating, and morality: individual differences in three functional domains of disgust. J. Pers. Soc. Psychol. 2009;97:103. doi: 10.1037/a0015474. [DOI] [PubMed] [Google Scholar]
- 20.Michalak N.M., Ackerman J.M. A multi-method approach to measuring mental representations of threatening others. J. Exp. Psychol. Gen. 2020 doi: 10.1037/xge0000781. Published online May 28, 2020. [DOI] [PubMed] [Google Scholar]
- 21.Ryan S. Facial disfigurement is treated like an infectious disease. Evol. Hum. Behav. 2012;33:639–646. [Google Scholar]
- 22.Perone P. Visual disgust-elicitors produce an attentional blink independent of contextual and trait-level pathogen avoidance. Emotion. 2020 doi: 10.1037/emo0000751. Published online April 23, 2020. [DOI] [PubMed] [Google Scholar]
- 23.Aarøe L. The behavioral immune system shapes political intuitions: why and how individual differences in disgust sensitivity underlie opposition to immigration. Am. Polit. Sci. Rev. 2017;111:277–294. [Google Scholar]
- 24.Ji T. Generalized or origin-specific out-group prejudice?: the role of temporary and chronic pathogen-avoidance motivation in intergroup relations. Evol. Psychol. 2019;17 doi: 10.1177/1474704919826851. 1474704919826851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang I.M., Ackerman J.M. The infectiousness of crowds: crowding experiences are amplified by pathogen threats. Personal. Soc. Psychol. Bull. 2019;45:120–132. doi: 10.1177/0146167218780735. [DOI] [PubMed] [Google Scholar]
- 26.Terrizzi J.A., Jr. The behavioral immune system and social conservatism: a meta-analysis. Evol. Hum. Behav. 2013;34:99–108. [Google Scholar]
- 27.Billingsley J. Sexual disgust trumps pathogen disgust in predicting voter behavior during the 2016 US Presidential Election. Evol. Psychol. 2018;16 doi: 10.1177/1474704918764170. 1474704918764170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karinen A.K. Disgust sensitivity and opposition to immigration: does contact avoidance or resistance to foreign norms explain the relationship? J. Exp. Soc. Psychol. 2019;84:103817. [Google Scholar]
- 29.Amoroso C.R. Disgust theory through the lens of psychiatric medicine. Clin. Psychol. Sci. 2020;8:3–24. [Google Scholar]
- 30.Hedman E. Health anxiety in a disease-avoidance framework: investigation of anxiety, disgust and disease perception in response to sickness cues. J. Abnorm. Psychol. 2016;125:868–878. doi: 10.1037/abn0000195. [DOI] [PubMed] [Google Scholar]
- 31.Tybur J.M. Genetic and environmental influences on disgust proneness, contamination sensitivity, and their covariance. Clin. Psychol. Sci. 2020;8:1054–1061. [Google Scholar]
- 32.McKay D., Asmundson G.J. Substance use and abuse associated with the behavioral immune system during COVID-19: the special case of healthcare workers and essential workers. Addict. Behav. 2020;110:106522. doi: 10.1016/j.addbeh.2020.106522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seitz B.M. The pandemic exposes human nature: 10 evolutionary insights. Proc. Natl. Acad. Sci. U. S. A. 2020;117:27767–27776. doi: 10.1073/pnas.2009787117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shook N.J. Disease avoidance in the time of COVID-19: the behavioral immune system is associated with concern and preventative health behaviors. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mortensen C.R. Infection breeds reticence: the effects of disease salience on self-perceptions of personality and behavioral avoidance tendencies. Psychol. Sci. 2010;21:440–447. doi: 10.1177/0956797610361706. [DOI] [PubMed] [Google Scholar]
- 36.Murray D.R. Direct and indirect implications of pathogen prevalence for scientific and technological innovation. J. Cross-Cult. Psychol. 2014;45:971–985. [Google Scholar]
- 37.Schaller M., Murray D.R. Pathogens, personality, and culture: disease prevalence predicts worldwide variability in sociosexuality, extraversion, and openness to experience. J. Pers. Soc. Psychol. 2008;95:212. doi: 10.1037/0022-3514.95.1.212. [DOI] [PubMed] [Google Scholar]
- 38.Tybur J.M. Parasite stress and pathogen avoidance relate to distinct dimensions of political ideology across 30 nations. Proc. Natl. Acad. Sci. U. S. A. 2016;113:12408–12413. doi: 10.1073/pnas.1607398113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tybur J.M. Smells like safe sex: olfactory pathogen primes increase intentions to use condoms. Psychol. Sci. 2011;22:478–480. doi: 10.1177/0956797611400096. [DOI] [PubMed] [Google Scholar]
- 40.Boyer P., Petersen M.B. Folk-economic beliefs: an evolutionary cognitive model. Behav. Brain Sci. 2018;41:1–51. doi: 10.1017/S0140525X17001960. [DOI] [PubMed] [Google Scholar]
- 41.Sell A. Physically strong men are more militant: a test across four countries. Evol. Hum. Behav. 2017;38:334–340. [Google Scholar]
- 42.Li N.P. The evolutionary mismatch hypothesis: implications for psychological science. Curr. Dir. Psychol. Sci. 2018;27:38–44. [Google Scholar]
- 43.Gurven M.D., Lieberman D.E. WEIRD bodies: mismatch, medicine and missing diversity. Evol. Hum. Behav. 2020;41:330–340. doi: 10.1016/j.evolhumbehav.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wells J.C. Evolutionary public health: introducing the concept. Lancet. 2017;390:500–509. doi: 10.1016/S0140-6736(17)30572-X. [DOI] [PubMed] [Google Scholar]
- 45.Stearns S.C. Evolutionary perspectives on health and medicine. Proc. Natl. Acad. Sci. U. S. A. 2010;107:1691–1695. doi: 10.1073/pnas.0914475107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McNeill W.H., McNeill W. Anchor; 1998. Plagues and Peoples. [Google Scholar]
- 47.Wirth T. Origin, spread and demography of the Mycobacterium tuberculosis complex. PLoS Pathog. 2008;4 doi: 10.1371/journal.ppat.1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boone S.A., Gerba C.P. Significance of fomites in the spread of respiratory and enteric viral disease. Appl. Environ. Microbiol. 2007;73:1687–1696. doi: 10.1128/AEM.02051-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Apicella C.L. Evidence from hunter-gatherer and subsistence agricultural populations for the universality of contagion sensitivity. Evol. Hum. Behav. 2018;39:355–363. doi: 10.1016/j.evolhumbehav.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hurtado A.M. The role of helminthes in human evolution. In: Elton S., Higgins P., editors. Medicine and Evolution: Current Applications, Future Prospects. CRC Press; 2008. pp. 153–180. [Google Scholar]
- 51.Wolfe Origins of major human infectious diseases. Nature. 2007;447:279–283. doi: 10.1038/nature05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marí Saéz A. Investigating the zoonotic origin of the West African Ebola epidemic. EMBO Mol. Med. 2015;7:17–23. doi: 10.15252/emmm.201404792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Curtis V. Evidence that disgust evolved to protect from risk of disease. Proc. R. Soc. Lond. Ser. B Biol. Sci. 2004;271:S131–S133. doi: 10.1098/rsbl.2003.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ackerman J.M. A pox on the mind: disjunction of attention and memory in the processing of physical disfigurement. J. Exp. Soc. Psychol. 2009;45:478–485. doi: 10.1016/j.jesp.2008.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nussinson R. Sensitivity to deviance and to dissimilarity: basic cognitive processes under activation of the behavioral immune system. Evol. Psychol. 2018;16 doi: 10.1177/1474704918813433. 1474704918813433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carrat F. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am. J. Epidemiol. 2008;167:775–785. doi: 10.1093/aje/kwm375. [DOI] [PubMed] [Google Scholar]
- 57.Oum R.E. A feel for disgust: tactile cues to pathogen presence. Cognit. Emot. 2011;25:717–725. doi: 10.1080/02699931.2010.496997. [DOI] [PubMed] [Google Scholar]
- 58.Argo J.J. Consumer contamination: how consumers react to products touched by others. J. Mark. 2006;70:81–94. [Google Scholar]
- 59.Boone S.A., Gerba C.P. The occurrence of influenza A virus on household and day care center fomites. J. Infect. 2005;51:103–109. doi: 10.1016/j.jinf.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 60.Van Doremalen N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Murray D.R. The kiss of death: three tests of the relationship between disease threat and ritualized physical contact within traditional cultures. Evol. Hum. Behav. 2017;38:63–70. [Google Scholar]
- 62.Tybur J.M. Behavioral immune tradeoffs: interpersonal value relaxes social pathogen avoidance. Psychol. Sci. 2020;31:1211–1221. doi: 10.1177/0956797620960011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schaller M. When and how disgust is and is not implicated in the behavioral immune system. Evol. Behav. Sci. 2014;8:251. [Google Scholar]
- 64.Randler C. Anxiety, disgust and negative emotions influence food intake in humans. Int. J. Gastron. Food Sci. 2017;7:11–15. [Google Scholar]
- 65.Mathews A. Why worry? The cognitive function of anxiety. Behav. Res. Ther. 1990;28:455–468. doi: 10.1016/0005-7967(90)90132-3. [DOI] [PubMed] [Google Scholar]
- 66.Ackerman J.M. Infectious disease and imperfections of self-image. Psychol. Sci. 2018;29:228–241. doi: 10.1177/0956797617733829. [DOI] [PubMed] [Google Scholar]
- 67.Ackerman, J. M., et al. What people believe about detecting infectious disease using the senses. Curr. Res. Ecol. Soc. Psychol. Published online October 19, 2020. 10.1016/j.cresp.2020.100002 [DOI] [PMC free article] [PubMed]
- 68.Faulkner J. Evolved disease-avoidance mechanisms and contemporary xenophobic attitudes. Group Process. Intergroup Relat. 2004;7:333–353. [Google Scholar]
- 69.Shook N.J. In defense of pathogen disgust and disease avoidance: a response to Tybur et al. (2015) Evol. Hum. Behav. 2015;36:498–502. [Google Scholar]
- 70.De Barra M., Curtis V. Are the pathogens of out-groups really more dangerous? Behav. Brain Sci. 2012;35:85. doi: 10.1017/S0140525X11000975. [DOI] [PubMed] [Google Scholar]
- 71.Tybur J.M. Pathogen disgust requires no defense: a response to Shook, Terrizzi, Clay, & Oosterhoff (2015) Evol. Hum. Behav. 2015;36:502–504. [Google Scholar]
- 72.Petersen M.B. Healthy out-group members are represented psychologically as infected in-group members. Psychol. Sci. 2017;28:1857–1863. doi: 10.1177/0956797617728270. [DOI] [PubMed] [Google Scholar]
- 73.van Leeuwen F., Petersen M.B. The behavioral immune system is designed to avoid infected individuals, not outgroups. Evol. Hum. Behav. 2018;39:226–234. [Google Scholar]
- 74.Inbar Y., Pizarro D.A. Pollution and purity in moral and political judgment. In: Sarkissian H., Wright J., editors. Advances in Experimental Moral Psychology: Affect, Character, and Commitments. Bloomsbury Academic; 2014. pp. 111–129. [Google Scholar]
- 75.Navarrete C.D., Fessler D.M. Disease avoidance and ethnocentrism: the effects of disease vulnerability and disgust sensitivity on intergroup attitudes. Evol. Hum. Behav. 2006;27:270–282. [Google Scholar]
- 76.Huang J.Y. Immunizing against prejudice: effects of disease protection on attitudes toward out-groups. Psychol. Sci. 2011;22:1550–1556. doi: 10.1177/0956797611417261. [DOI] [PubMed] [Google Scholar]
- 77.Thornhill R., Fincher C.L. Springer; 2014. The Parasite-Stress Theory of Values and Sociality: Infectious Disease, History and Human Values Worldwide. [Google Scholar]
- 78.Fincher C.L., Thornhill R. Parasite-stress promotes in-group assortative sociality: the cases of strong family ties and heightened religiosity. Behav. Brain Sci. 2012;35:61–79. doi: 10.1017/S0140525X11000021. [DOI] [PubMed] [Google Scholar]
- 79.Hruschka D.J., Henrich J. Institutions, parasites and the persistence of in-group preferences. PLoS One. 2013;8 doi: 10.1371/journal.pone.0063642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pollet T.V. What can cross-cultural correlations teach us about human nature? Hum. Nat. 2014;25:410–429. doi: 10.1007/s12110-014-9206-3. [DOI] [PubMed] [Google Scholar]
- 81.Ross C.T., Winterhalder B. A hierarchical Bayesian analysis of parasite prevalence and sociocultural outcomes: the role of structural racism and sanitation infrastructure. Am. J. Hum. Biol. 2016;28:74–89. doi: 10.1002/ajhb.22757. [DOI] [PubMed] [Google Scholar]
- 82.Gruijters S.L. Sex, germs, and health: pathogen-avoidance motives and health-protective behaviour. Psychol. Health. 2016;31:959–975. doi: 10.1080/08870446.2016.1161194. [DOI] [PubMed] [Google Scholar]
- 83.Huang J.Y. (De) contaminating product preferences: a multi-method investigation into pathogen threat's influence on used product preferences. J. Exp. Soc. Psychol. 2017;70:143–152. [Google Scholar]
- 84.Pellegrino R. Using olfaction and unpleasant reminders to reduce the intention-behavior gap in hand washing. Sci. Rep. 2016;6:18890. doi: 10.1038/srep18890. [DOI] [PMC free article] [PubMed] [Google Scholar]