Repurposing of existing medications has widely been used in studies since the emergence of coronavirus disease 2019 (COVID-19). Besides dexamethasone in selected patients,1 no medical treatment to date has been shown to improve mortality in patients with COVID-19 infection. Aspirin is associated with reduced mortality and lower risk of acute respiratory distress syndrome in critically ill patients without COVID-19.2 , 3 Although the exact mechanism behind this effect remains unclear, possible protective effects of aspirin may be related to its antithrombotic, anti-inflammatory, and immuno-modulation effects.3 As severe COVID-19 infection is mainly a multisystem inflammatory process, use of aspirin can theoretically provide positive outcomes. However, the role of aspirin in patients with COVID-19 is not clear and has not adequately been studied. In this meta-analysis, we report the association between aspirin use and mortality in COVID-19.
We searched PubMed database looking for relevant articles using (“COVID-19” and “aspirin”) and (“SARS-CoV-2” and “aspirin”) from inception until December 19, 2020. Nolanguage restriction was applied. Inclusion criteria were (1) clinical trials or cohort studies, (2) the study population included patients with confirmed COVID-19 infection, (3) use of aspirin was reported in the study, (4) mortality among aspirin users was reported or could be calculated and compared with nonaspirin users. All other studies were excluded. Review Manager 5.4.1 was used to perform a random effect model analysis to compare mortality between patients with COVID-19 infection who use aspirin compared with those who do not. Mantel-Haenszel risk ratio with its 95% confidence intervals was calculated. Cochran's Q and I2 index were used for heterogeneity estimation. An I2 index <25% was considered to be low, an I2 index between 25% and 80% was considered to be moderate, and an I2 index >80% was considered to be high. Sensitivity analysis was done by excluding 1 study at a time.
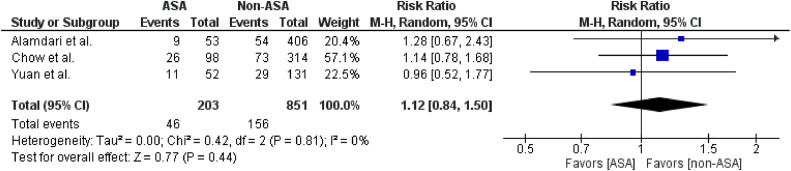
Initial search resulted in 112 articles. After applying our inclusion criteria and deduplications, only 3 studies with a total of 1,054 patients were included in the analysis.4, 5, 6 Characteristics of the included studies are summarized in (Table 1 ). About 19.2% of these patients were aspirin users. Mortality among aspirin users was 22.6% compared with mortality of 18.3% among nonaspirin users (risk ratio 1.12, 95% confidence intervals [0.84, 1.50]). I2 index was 0%, suggestive of low heterogeneity. Due to the small number of studies (<10), small-study bias was not assessed as the analysis was underpowered to detect such bias. Sensitivity analysis yielded consistent results (Figure 1 ).
Table 1.
Characteristic of the included studies
| Study | Year | Country | Study type | Characteristics of patients |
|---|---|---|---|---|
| Amadari et al | 2020 | Iran | Retrospective | Hospitalized patients with COVID-19 |
| Yuan et al | 2020 | China | Retrospective | Hospitalized patients with concurrent COVID-19 and coronary artery disease |
| Chow et al | 2020 | United States | Retrospective | Hospitalized patients with COVID-19 |
Figure 1.
Forest plot examining the association between the use of aspirin and mortality in COVID-19 infection. ASA = aspirin; CI = confidence interval; M-H = Mantel-Haenszel.
The results of this analysis suggest no association between the use of aspirin and mortality in patients with COVID-19. Although patients on aspirin tend to have more risk factors for severe COVID-19 infection (eg, older age, pre-existing coronary artery disease, diabetes mellitus, etc), the low heterogeneity in this analysis despite differences in characteristics of the population of the included studies likely suggests no protective effect of aspirin among different groups of patients. However, more studies are needed to confirm this finding.
Disclosures
The authors have no conflict of interest to disclose.
Footnotes
Funding: None.
References
- 1.RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ. Dexamethasone in hospitalized patients with Covid-19—preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du F, Jiang P, He S, Song D, Xu F. Antiplatelet therapy for critically ill patients: a pairwise and Bayesian network meta-analysis. Shock. 2018;49:616–624. doi: 10.1097/SHK.0000000000001057. [DOI] [PubMed] [Google Scholar]
- 3.Wang L, Li H, Gu X, Wang Z, Liu S, Chen L. Effect of antiplatelet therapy on acute respiratory distress syndrome and mortality in critically ill patients: a meta-analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0154754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alamdari NM, Afaghi S, Rahimi FS, Tarki FE, Tavana S, Zali A, Fathi M, Besharat S, Bagheri L, Pourmotahari F, Irvani SSN, Dabbagh A, Mousavi SA. Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran. Tohoku J Exp Med. 2020;252:73–84. doi: 10.1620/tjem.252.73. [DOI] [PubMed] [Google Scholar]
- 5.Yuan S, Chen P, Li H, Chen C, Wang F, Wang DW. Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease. J Cell Mol Med. 2020 doi: 10.1111/jcmm.16198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, McCurdy MT, Tabatabai A, Kumar G, Park P, Benjenk I, Menaker J, Ahmed N, Glidewell E, Presutto E, Cain S, Haridasa N, Field W, Fowler JG, Trinh D, Johnson KN, Kaur A, Lee A, Sebastian K, Ulrich A, Peña S, Carpenter R, Sudhakar S, Uppal P, Fedeles BT, Sachs A, Dahbour L, Teeter W, Tanaka K, Galvagno SM, Herr DL, Scalea TM, Mazzeffi MA. Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesth Analg. 2020 doi: 10.1213/ANE.0000000000005292. [DOI] [PubMed] [Google Scholar]