Abstract
Introduction
Acute limb ischemia (ALI) is defined as an abrupt decrease in arterial perfusion of a limb with a threat to viability of the limb. Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2, and has been declared as a global pandemic by the World Health Organization. Patients with COVID-19 have deranged blood coagulation parameters and are prone to thromboembolic events. This hypercoagulable state caused by COVID-19 mainly manifests as venous thromboembolism. Peripheral arterial involvement is less frequent. We present a case of a spontaneous ALI in a COVID-19 patient.
Case
A 62-year-old man with an insignificant past medical history presented with ALI 12 days after an initial diagnosis of COVID-19. He was on therapeutic doses of low molecular weight heparin when ischemic symptoms developed. A surgical thrombectomy was unsuccessful. He partially benefited from intravenous unfractionated heparin and iloprost infusions. He was discharged home on postoperative day 14, and is scheduled to have an amputation of the 1st toe.
Conclusions
COVID-19 infection is associated with an increased incidence of thromboembolic events, including ALI. Even young and otherwise healthy patients may develop ALI despite the use of prophylactic anticoagulation. Management of ALI in COVID-19 patients might be harder than expected, due to the hypercoagulable state. Patients may benefit from prolonged postoperative unfractionated heparin administration.
Keywords: Acute limb ischemia, Coronavirus disease 2019, Low molecular weight heparin, Severe acute respiratory syndrome coronavirus 2, Thrombectomy, Unfractionated heparin
1. Introduction
Acute limb ischemia (ALI) is defined as an abrupt decrease in arterial perfusion of a limb with a threat to viability of the limb [1]. The clinical presentation is considered to be acute if symptom duration is less than 2 weeks [1]. The most common causes include embolism from cardiac chambers mainly associated with atrial fibrillation or acute myocardial infarction, embolism from arterial aneurysms, thrombosis of native limb arteries or vascular grafts, iatrogenic thromboembolism during vascular interventions, aortic dissection, and traumatic vascular injuries [1].
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and has been declared as a global pandemic by the World Health Organization [2]. Several reports revealed that patients with COVID-19 have deranged blood coagulation parameters and are prone to thromboembolic events [[2], [3], [4], [5]]. This hypercoagulable state caused by COVID-19 is associated with poor overall prognosis, and mainly manifests as venous thromboembolism (VTE) [4,5]. Peripheral arterial involvement is less frequent [2,5].
Herein we present a case of a spontaneous ALI in a COVID-19 patient.
2. Case
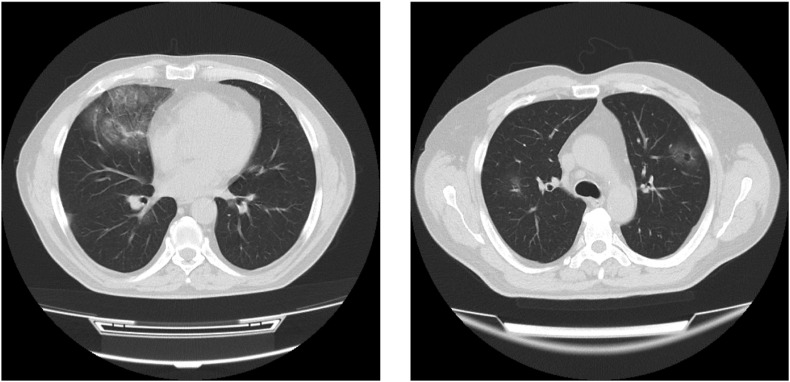
A 62-year-old man presented to the emergency room with complaints of fever, nausea, fatigue and muscle aches. His past medical history was insignificant. Body temperature was 36.7 °C, pulse rate 82 beats per minute, respiratory rate 24 breathes per minute, blood pressure 125/72 mmHg, and oxygen saturation 95%. There were bilateral diffuse fine crackles on auscultation. Laboratory findings were normal except for a D-dimer level of 670 ng/ml (normal range <500 ng/ml) (Table 1 ). A computed tomography (CT) scan of the chest revealed bilateral ground-glass opacities (Fig. 1 ). A swab test result came back positive for COVID-19, and the patient was discharged home on favipiravir, hydroxychloroquine and low-dose subcutaneous enoxaparin.
Table 1.
Laboratory findings at initial diagnosis (day 0), hospitalization (day 5), discharge (day 10), re-hospitalization for acute limb ischemia (day 12).
| Day 0 | Day 5 | Day 10 | Day 12 | Normal range | |
|---|---|---|---|---|---|
| White blood cell, 103/μL | 12.4 | 16 | 19.6 | 20.5 | 4–11 |
| Neutrophil count, 103/μL | 10.2 | 12.6 | 15.2 | 16.4 | 2–7 |
| Lymphocyte count, 103/μL | 1.2 | 1.4 | 1.6 | 2.5 | 1–3 |
| Platelet count, 103/μL | 269 | 306 | 422 | 374 | 100–450 |
| Hemoglobin, g/dL | 13.7 | 14 | 13.3 | 11 | 14–18 |
| Prothrombin time, seconds | 15.5 | 15.1 | 12.5 | 12.6 | 11.5–15.5 |
| Partial thromboplastin time, seconds | 23.1 | 26.2 | 23.2 | 22.8 | 23.5–35 |
| C-reactive protein, mg/dl | 0.78 | 15.4 | 7.34 | 13.38 | <0.5 |
| D-dimer, ng/mL | 670 | 950 | 590 | – | <500 |
| Fibrinogen, mg/dL | 280 | 315 | 172 | – | 200–400 |
| Lactate dehydrogenase, IU/L | 109 | 1276 | 1045 | – | 0–250 |
| Creatine kinase, IU/L | 22 | 386 | 103 | 398 | 30–200 |
| Serum creatinine, mg/dL | 1.14 | 1.39 | 1.34 | 3.54 | 0.67–1.17 |
Fig. 1.
Computed tomography (CT) scan of the chest demonstrating bilateral ground-glass opacities.
Five days later, he was hospitalized for worsening of respiratory symptoms. He appeared severely tachypneic with a respiratory rate of 40 breathes per minute, and dyspneic with an oxygen saturation of 82% on ambient air. D-dimer level was elevated to 950 ng/ml. Low molecular weight heparin dosage was increased to therapeutic doses (enoxaparin 8000 IU twice daily). The patient was discharged home 5 days after his hospitalization with complete resolution of symptoms.
However, 2 days later, he presented to emergency room with a cold, cyanotic and painful left foot. Left pedal pulses were absent with minimal sensory loss and normal motor function. A CT angiography of the lower extremities revealed occlusion of left tibial arteries (Fig. 2 ). The arterial tree was free of atherosclerotic plaques, and there were no collateral vessels, suggesting an acute occlusion. Transthoracic echocardiography and thoraco-abdominal aortic imaging were negative for proximal sources of thromboembolism. 5000 IU unfractionated heparin (UFH) bolus was administered intravenously. Patient was transferred to the operating theatre for surgical intervention. Popliteal trifurcation was explored through medial infragenicular approach under local anesthesia. Popliteal artery and all of its branches appeared healthy without any atherosclerotic plaques. A longitudinal arteriotomy revealed excellent antegrade blood flow with absent retrograde flow. An attempt was made to remove the thrombus using 2 and 3F Fogarty catheters. However, the thrombus was densely organized and catheters could not be passed across the occluded segment. We did not perform thrombolysis due to organized nature of the thrombus. The arteriotomy was closed with patch plasty. Patient was transferred to ward. Intravenous UFH and iloprost infusions were started. Heparin dose was adjusted to maintain an activated clotting time (ACT) of 200–250 seconds. Continuous iloprost infusion was maintained until discharge. The ischemic foot improved significantly with systemic anticoagulation, and posterior tibial and dorsalis pedis arterial Doppler signals became audible on postoperative 2nd day. However, 1st and 2nd toes and medial aspect of the foot became cyanotic again on postoperative day 5, while the ACT was within the target range (Fig. 3 ). Posterior tibial artery pulse was once again absent. A more than two fold increase of serum creatinine was observed following the initial CT angiography therefore a repeat angiography was not performed (Table 1). A duplex ultrasound of the lower leg performed prior to discharge revealed biphasic flow pattern in anterior tibial artery, and no flow in peroneal and posterior tibial arteries. The patient was discharged home with dry gangrene of the 1st toe on postoperative day 14 on enoxaparin 8000 IU twice daily and dual anti-platelet therapy with aspirin and clopidogrel. His condition remains stable 1 month after discharge, and a digital amputation is scheduled.
Fig. 2.
Computed tomography angiography of the left lower extremity demonstrating occlusion of left tibial arteries, 3-dimensional reconstruction.
Fig. 3.
Recurrent ischemia of the left foot.
3. Discussion
Present report describes a case of ALI in a patient with confirmed COVID-19 infection. The patient was otherwise healthy and did not have any conventional risk factors for ALI. However, his condition was resistant to treatment, and tended to recur. This finding is in correlation with reports by others [2,[6], [7], [8]]. Bellosta and colleagues [6] described 20 patients (18 men) with COVID-19-associated ALI over a period of 3 months. Seventeen patients underwent surgical treatment with a successful revascularization in only 12 (70.6%). Authors argued that this lower-than-expected success rate was due to a COVID-19-related hypercoagulable state [6]. They also reported that prolonged use of systemic heparin was associated with better outcomes in this subset of patients [6]. Perini and colleagues [7] reported 4 patients presenting with ALI caused by COVID-19. Two of their patients did not have any comorbidities, were relatively young, and receiving prophylactic doses of LMWH at presentation. One of them, a 53-year-old man, died on postoperative day 2 due to a recurrent aortoiliac occlusion. The other patient, a man aged 37 years with upper extremity thrombosis was successfully managed with UFH administration [7]. Baccellieri and colleagues [8] reported a patient who developed COVID-19-associated ALI while under prophylactic LMWH. The 67-year-old man with no relevant medical history was successfully treated with surgical intervention for simultaneous lower and upper limb ischemia [8].
Thromboembolic events associated with COVID-19 mainly manifest as VTE [5]. This is reasonable since COVID-19 exposes patients to all 3 components of Virchow’s triad: (1) there is direct viral infection of endothelial cells [9]; (2) patients are frequently hospitalized and immobilized; (3) blood coagulation parameters are deranged representing a hypercoagulable state [3,4]. Bilaloglu and colleagues [5] reported less than 1% incidence of ALI in their analysis of 3334 patients hospitalized with COVID-19. Of note, although not as frequent as VTE, incidence of ALI is increased during the COVID-19 pandemic [6].
Evidence from early experience suggests that pathogenesis of arterial thrombosis in COVID-19 patients differs from that of classical arterial thrombosis [[10], [11], [12]]. In-situ arterial thrombosis mainly occurs due to plaque breakdown or reduced perfusion through an atherosclerotic lesion, or stent or graft [13]. However, such as in the present case and others, COVID-19 patients may exhibit acute thrombosis of non-atherosclerotic native arteries [2]. Various mechanisms have been proposed to explain this phenomenon. A dysregulated hyperinflammatory response is thought to be responsible for arterial and venous thromboembolic events seen in patients with COVID-19 [11,12]. Increased levels of D-dimer, fibrinogen, coagulation factors, acquired antiphospholipid antibodies, and decreased levels of protein C, protein S, antithrombin, and hyperactivation of platelets and neutrophils are observed [10]. A consumption coagulopathy similar to sepsis-associated disseminated intravascular coagulopathy (DIC) is seen in COVID-19 patients. However, thrombotic component is more predominant than hemorrhagic component when compared with DIC [11,12]. It has been also speculated that direct viral infection of endothelial cells through the angiotensin-converting enzyme 2 receptor may be the cause of arterial thrombosis in patients with COVID-19 [9,10,12]. It is possible that a combination of these mechanisms, but not one, is responsible for increased rate of arterial thromboembolic events in COVID-19 patients.
4. Conclusion
COVID-19 infection is associated with an increased incidence of thromboembolic events, including ALI. Even young and otherwise healthy patients may develop ALI despite the use of prophylactic anticoagulation. Management of ALI in COVID-19 patients might be harder than expected, due to the hypercoagulable state. Patients may benefit from prolonged postoperative UFH administration.
Funding
There is no funding.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Björck M., Earnshaw J.J., Acosta S., Gonçalves F.B., Frederic C., Debus E.S., Hinchliffe R., Jongkind V., Koelemay M.J.W., Menyhei G., Svetlikov A.V., Tshomba Y., Van Den Berg J.C. Editor’s choice-European society for vascular surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia. Eur. J. Vasc. Endovasc. Surg. 2020;59(2):173–218. doi: 10.1016/j.ejvs.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Gomez-Arbelaez D., Ibarra-Sanchez G., Garcia-Gutierrez A., Comanges-Yeboles A., Ansuategui-Vicente M., Gonzalez-Fajardo J.A. COVID-19-related aortic thrombosis: a report of four cases. Ann. Vasc. Surg. 2020;67:10–13. doi: 10.1016/j.avsg.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han H., Yang L., Liu R., Liu F., Wu K.L., Li J., Liu X.H., Zhu C.L. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin. Chem. Lab. Med. 2020;58(7):1116–1120. doi: 10.1515/cclm-2020-0188. [DOI] [PubMed] [Google Scholar]
- 4.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemostasis. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bilaloglu S., Aphinyanaphongs Y., Jones S., Iturrate E., Hochman J., Berger J.S. Thrombosis in hospitalized patients with COVID-19 in a New York city Health system. JAMA. 2020;324(8):799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellosta R., Luzzani L., Natalini G., Pegorer M.A., Attisani L., Cossu L.G., Ferrandina C., Fossati A., Conti E., Bush R.L., Piffaretti G. Acute limb ischemia in patients with COVID-19 pneumonia. J. Vasc. Surg. 2020 doi: 10.1016/j.jvs.2020.04.483. (article in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perini P., Nabulsi B., Massoni C.B., Azzarone M., Freyrie A. Acute limb ischaemia in two young, non-atherosclerotic patients with COVID-19. Lancet. 2020;395(10236):1546. doi: 10.1016/S0140-6736(20)31051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baccellieri D., Bilman V., Apruzzi L., Monaco F., D’Angelo A., Loschi D., Melissano G., Chiesa R. A case of COVID-19 patient with acute limb ischemia and heparin resistance. Ann. Vasc. Surg. 2020;68:88–92. doi: 10.1016/j.avsg.2020.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Piazza G., Morrow D.A. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19. JAMA. 2020;324(24):2548–2549. doi: 10.1001/jama.2020.23422. [DOI] [PubMed] [Google Scholar]
- 11.Imdes J.E., Koleilat I., Hatch A.N., Choinski K., Jones D.B., Aldailami H., Billett H., Denesopolis J.M., Lipsitz E. Early experience with arterial thromboembolic complications in patients with COVID-19. J. Vasc. Surg. 2020 doi: 10.1016/j.jvs.2020.07.089. (article in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shalbub S. The mystery of COVID-19-associated arterial thrombosis. J. Vasc. Surg. 2020 doi: 10.1016/j.jvs.2020.08.022. (article in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Obara H., Matsubara K., Kitagawa Y. Acute limb ischemia. Ann. Vasc. Dis. 2018;11(4):443–447. doi: 10.3400/avd.ra.18-00074. [DOI] [PMC free article] [PubMed] [Google Scholar]