Abstract
Background
The fear of contagion during the coronavirus disease-2019 (COVID-19) pandemic may have potentially refrained patients with ST-segment elevation myocardial infarction (STEMI) from accessing the emergency system, with subsequent impact on mortality.
Objectives
The ISACS-STEMI COVID-19 registry aims to estimate the true impact of the COVID-19 pandemic on the treatment and outcome of patients with STEMI treated by primary percutaneous coronary intervention (PPCI), with identification of “at-risk” patient cohorts for failure to present or delays to treatment.
Methods
This retrospective registry was performed in European high-volume PPCI centers and assessed patients with STEMI treated with PPPCI in March/April 2019 and 2020. Main outcomes are the incidences of PPCI, delayed treatment, and in-hospital mortality.
Results
A total of 6,609 patients underwent PPCI in 77 centers, located in 18 countries. In 2020, during the pandemic, there was a significant reduction in PPCI as compared with 2019 (incidence rate ratio: 0.811; 95% confidence interval: 0.78 to 0.84; p < 0.0001). The heterogeneity among centers was not related to the incidence of death due to COVID-19. A significant interaction was observed for patients with arterial hypertension, who were less frequently admitted in 2020 than in 2019. Furthermore, the pandemic was associated with a significant increase in door-to-balloon and total ischemia times, which may have contributed to the higher mortality during the pandemic.
Conclusions
The COVID-19 pandemic had significant impact on the treatment of patients with STEMI, with a 19% reduction in PPCI procedures, especially among patients suffering from hypertension, and a longer delay to treatment, which may have contributed to the increased mortality during the pandemic. (Primary Angioplasty for STEMI During COVID-19 Pandemic [ISACS-STEMI COVID-19] Registry; NCT04412655).
Key Words: COVID-19, primary angioplasty, STEMI
Abbreviations and Acronyms: ACS, acute coronary syndrome; CI, confidence interval; DES, drug-eluting stent(s); IRR, incidence rate ratio; PCI, percutaneous coronary intervention; PPCI, primary PCI; STEMI, ST-segment elevation myocardial infarction
Central Illustration
The global pandemic of coronavirus disease-2019 (COVID-19) has dramatically affected health care, and the effects are ongoing. The outbreak was initially identified in Wuhan, China, in December 2019 (1), and recognized as a pandemic on March 11, 2020. As of May 26, 2020, more than 5.54 million cases of COVID-19 have been reported in 185 countries and territories, resulting in more than 348,000 deaths, especially in Europe and the United States.
During this pandemic period, health care resources have understandably been focused on the treatment of patients with COVID-19, with many clinical units converted to treat patients with COVID-19, limiting access for patients with chronic conditions while maintaining acute services for the treatment of acute coronary syndrome (ACS), particularly ST-segment elevation myocardial infarction (STEMI). Combined with this diversion of resource, lockdown rules, guidance on social distancing, and a public fear of coronavirus contagion appear to have affected patient willingness to present to hospital, as evidenced by a reduction in percutaneous coronary intervention (PCI) procedures for ACS, including STEMI (2, 3, 4, 5, 6, 7). The observation of extended time from symptom onset to treatment (8, 9, 10) is certainly expected to heavily affect mortality for acute myocardial infarction worldwide.
The ISACS-STEMI (International Study on Acute Coronary Syndromes–ST Elevation Myocardial Infarction) COVID-19 was established in response to the emerging outbreak of COVID-19 to provide a European snapshot and aims to estimate the true impact of the COVID-19 pandemic on the treatment and outcome of patients with STEMI treated by primary angioplasty, with identification of “at-risk” patient cohorts for failure to present or delays to treatment.
Methods
Study design and population
This is a retrospective multicenter registry promoted by the Eastern Piedmont University, Novara, Italy, planned to include at least 40 European primary PCI (PPCI) centers, performing more than 120 PPCIs per year (with expected average >10/month), with the case load of STEMI not expected to be affected by a potential planned reorganization of the STEMI network. The inclusion period was 2 months (from March 1 to April 30). The data were compared with those retrospectively collected in the same time window (from March 1 to April 30) of 2019.
Inclusion criteria
STEMI treated by primary angioplasty (including mechanical reperfusion for failed thrombolysis).
Data collection
Anonymized data were collected through a dedicated case report form (CRF). Each center identified a local principal investigator. We collected demographic, clinical, and procedural data, including total ischemia time, door-to-balloon time, referral to primary PCI facility, COVID positivity, PCI procedural data, and in-hospital mortality. After collection, each participating center submitted the CRF to the coordinating unit Eastern Piedmont University, in charge of reporting all data onto the central electronic database. Data were finally checked for missing or contradictory entries.
Study outcomes
Study outcomes included: 1) number of patients with STEMI undergoing percutaneous revascularization; 2) proportion of patients with ischemia time >12 h; 3) proportion of patients with a door-to-balloon time >30 min; and 4) in-hospital mortality.
Statistics
Data were analyzed using SPSS Statistics Software 23.0 (IBM SPSS Inc., Chicago, Illinois) and R software (version 3.6.2) by an independent statistician (GC). Quantitative variables were described using median and interquartile range. Means and confidence intervals (CIs) were obtained assuming Poisson distributions for count data. Incidence rate ratio (IRR) was defined as the ratio between count data in 2019 and 2020, over the same population and time period. Poisson regression models (with log link function) were applied to compare the incidence rate of PPCI per million of residents per year in 2019 with the same rate in 2020, correcting for possible impact of major risk factors (11). Details are described in the Supplemental Appendix. Analysis was also conducted according to major European geographic areas (Supplemental Appendix) and subgroups of patients, such as according to age, sex, diabetes, and hypertension.
A subsequent analysis was based on individual data that were grouped according to the year of the intervention (2019 vs. 2020). Absolute frequencies and percentages were used for qualitative variables. Analysis of variance or Mann-Whitney U test and chi-square test were used for continuous and categorical variables, respectively. Normal distribution of continuous variables was tested by the Kolmogorov-Smirnov test.
Multivariable logistic regression analyses were performed to identify the impact of the year of intervention on time delays and mortality after adjustment for baseline confounding factors between the 2 groups. All significant variables (set at p < 0.10) were entered in block into the model. A p < 0.05 was considered statistically significant. The data coordinating center was established at the Eastern Piedmont University.
Sample size calculation
In view of the observational nature of this registry, no sample size calculations or statistical power analyses were performed. However, with the participation of at least 40 high-volume centers, with approximately 40 patients per center (based on average PPCI per month), we expected the inclusion of at least 1,600 patients with STEMI for 2019.
Ethical issues
The study is a retrospective registry, with anonymized data collection, therefore formal approval from the ethical committee was deemed not necessary; however, it was approved by the Ethical Committee of AOU Maggiore della Carità, Novara. The need to notify or ask for approval to the local ethical committees was left to each investigator’s discretion according to local and national regulations.
Results
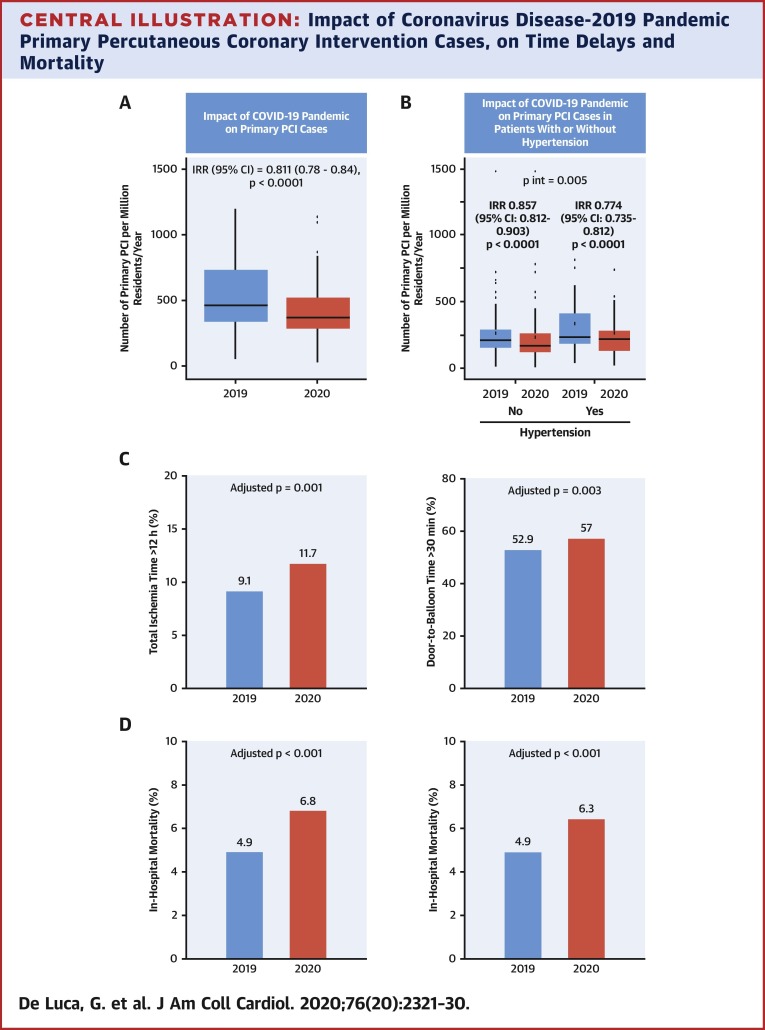
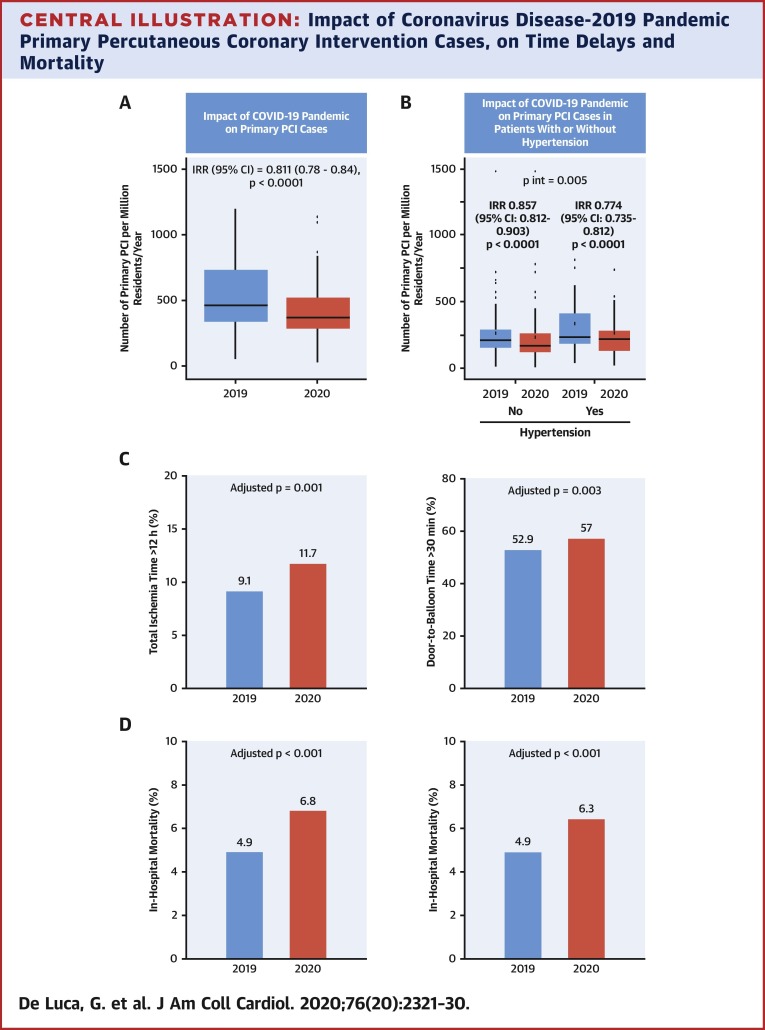
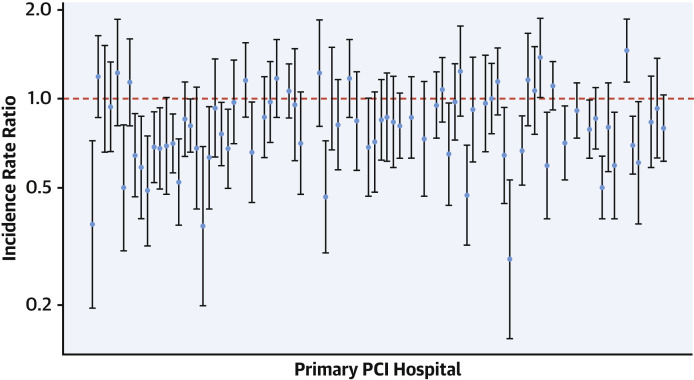
A total of 77 European centers agreed to participate, including a total of 6,609 patients with STEMI undergoing mechanical reperfusion: 3,653 patients in 2019 and 2,956 patients in 2020. Characteristics of study centers are reported in Supplemental Table 1. Almost all European countries were represented (Supplemental Figure 1, Supplemental Table 1), especially Italy (n = 24), Spain (n = 13), and the Netherlands (n = 9). The number of STEMIs treated percutaneously per million residents had a consistent reduction, on average, from 595 (95% CI: 548 to 645) in 2019 to 494 (95% CI: 451 to 539) in 2020 (Central Illustration , Supplemental Figure 2). The IRR was 0.811 (95% CI: 0.78 to 0.84; p < 0.0001), showing a significant reduction of 18.9% in the number of STEMIs from 2019 to 2020. A significant heterogeneity was observed among centers (IRR had high variability between centers measured by SE = 0.18 in a random effect Poisson model; chi-square analysis of variance test with p < 0.001) (Figure 1 ). A significant reduction was observed in 39% of the centers under investigation, and was not related to the incidence of COVID disease, neither to the COVID mortality. In fact, the reduction in STEMI procedures was not associated with the number of COVID-positive patients, at both local (p = 0.31) (Supplemental Figure 3) and national levels (p = 0.79) (Supplemental Figure 4), neither with national (p = 0.36) (Supplemental Figure 5) nor local number (p = 0.82) (Supplemental Figure 6) of COVID-related deaths. Moreover, the reduction in STEMI procedures was not associated with the type of institutional center (private [1], academic [2], or nonacademic [3] hospitals; IRR: 0.989; 95% CI: 0.774 to 1.205; p = 0.925 type 2 vs. 1; IRR: 1.058; 95% CI: 0.843 to 1.273; p = 0.249 type 3 vs. 2). All participating geographic areas had a significant reduction in STEMI, especially the Balkans (Supplemental Figures 7 to 9). Furthermore, we used Poisson regression to investigate the reduction in STEMI in subgroups of subjects, by age (≤75, >75), sex, diabetes, and hypertension, and found a significant difference in this reduction (10%) only between subjects with (IRR: 0.857; 95% CI: 0.812 to 0.903; p < 0.0001) and without hypertension (IRR: 0.774; 95% CI: 0.735 to 0.812; p < 0.0001) (p interaction = 0.005) (Supplemental Figures 10 to 12). No significant differences were found for the other risk factors (Supplemental Figures 10 to 13).
Central Illustration.
Impact of Coronavirus Disease-2019 Pandemic Primary Percutaneous Coronary Intervention Cases, on Time Delays and Mortality
Box-and-whisker plot showing the number of patients with STEMI treated by mechanical reperfusion per million of inhabitants/year in 2019 and 2020 in the overall population (A) and according to hypertension, the only clinical variable significantly affecting the number of cases (B). Bar graphs show the association between the year of intervention with time delays (ischemia time longer than 12 h, left graph) and door-to-balloon time longer than 30 min, right graph(C). Bar graphs show the association between the year of intervention with in-hospital mortality with (left graph) and without (right graph) COVID-positive patients (D). CI = confidence interval; COVID-19 = coronavirus-2019; IRR = incidence rate ratio; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial intervention.
Figure 1.
Impact of COVID-19 Pandemic on Mechanical Reperfusion for STEMI
Forest plot of the incidence rate ratio on the log-scaled axis, with 95% confidence interval, across each hospital center. COVID-19 = coronavirus disease-2019; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Baseline demographic and clinical characteristics
Individual data analysis was restricted to 6,295 patients with complete demographic, clinical procedural, and outcome data (complete cases, 95.2%), 3,484 in 2019 and 2,811 in 2020. Table 1 shows baseline characteristics of the 2 groups of patients according to the year of intervention. No difference was observed in baseline characteristics. We found a different distribution across the centers.
Table 1.
Baseline Demographic and Clinical Characteristics
| 2019 (n = 3,484) | 2020 (n = 2,811) | p Value | |
|---|---|---|---|
| Age, yrs | 64 (55–73) | 64 (55–73) | 0.64∗ |
| Age >75 yrs | 758 (21.8) | 598 (21.3) | 0.65 |
| Male | 2,567 (73.7) | 2,095 (74.5) | 0.45 |
| Medical history | |||
| Diabetes mellitus | 0.18 | ||
| Type 1 | 130 (3.7) | 81 (2.9) | |
| Type 2 | 629 (18.1) | 516 (18.4) | |
| Hypertension | 1,906 (54.7) | 1,501 (53.4) | 0.30 |
| Hypercholesterolemia | 1,445 (41.5) | 1,195 (42.5) | 0.40 |
| Active smoker | 1,438 (41.3) | 1,155 (41.1) | 0.89 |
| Family history of CAD | 837 (24.0) | 658 (23.4) | 0.57 |
| Previous STEMI | 327 (9.4) | 272 (9.7) | 0.73 |
| Previous PCI | 439 (12.6) | 354 (12.6) | 0.94 |
| Previous CABG | 59 (1.7) | 55 (2.0) | 0.43 |
| Geographic area | 0.037 | ||
| Italy | 964 (27.7) | 779 (27.7) | |
| Iberian Peninsula | 549 (15.8) | 445 (15.8) | |
| Central Europe | 910 (26.1) | 742 (26.4) | |
| Balkan Peninsula | 454 (13.0) | 301 (10.7) | |
| Northeast Europe | 607 (17.4) | 544 (19.4) | |
| Referral to primary PCI hospital | |||
| Type | 0.005 | ||
| Direct access to Hub | 649 (18.6) | 497 (17.7) | |
| Ambulance (from community) | 1,893 (54.3) | 1,639 (58.3) | |
| Transfer from spoke | 942 (27.0) | 675 (24.0) | |
| Time delays | |||
| Total ischemia, min | 181 (120–301) | 200 (127–357) | 0.004∗ |
| Total ischemia time, h | 0.003 | ||
| <6 | 2,732 (78.4) | 2,109 (75.0) | |
| 6–12 | 437 (12.5) | 374 (13.3) | |
| 12–24 | 196 (5.6) | 193 (6.9) | |
| >24 h | 119 (3.4) | 135 (4.8) | |
| Total ischemia time >12 h | 316 (9.1) | 328 (11.7) | <0.001 |
| Door-to-balloon time, min | 34 (21–36) | 36 (24–60) | 0.007∗ |
| Door-to-balloon time, min | 0.005 | ||
| <30 | 1,640 (47.1) | 1,209 (43) | |
| 30–60 | 1,066 (30.6) | 917 (32.6) | |
| >60 | 778 (22.3) | 685 (24.4) | |
| Door-to-balloon time >30 min | 1,843 (52.9) | 1,602 (57) | <0.001 |
| Clinical presentation | |||
| Anterior STEMI | 1,592 (45.7) | 1,279 (45.5) | 0.86 |
| Out-of-hospital cardiac arrest | 231 (6.6) | 198 (7.0) | 0.51 |
| Cardiogenic shock | 267 (7.7) | 247 (8.8) | 0.11 |
| Rescue PCI for failed thrombolysis | 124 (3.6) | 95 (3.4) | 0.70 |
Values are median (interquartile range) or n (%).
CABG = coronary artery bypass grafting; CAD = coronary artery disease; IQR = interquartile range; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Mann-Whitney U test.
As shown in Table 1, we observed a significant difference in referral to primary PCI facility, with a larger number of patients reaching the primary PCI center by ambulance with direct transfer from community in 2020 as compared with 2019. Despite a greater proportion of patients presenting by the most efficient route, patients treated in 2020 had a significantly longer total ischemia and door-to-balloon time (Table 1, Central Illustration). The association between the COVID pandemic and ischemia time longer than 12 h was confirmed after correction for baseline clinical confounders (geographic area, direct access by ambulance, door-to-balloon, radial access, multivessel disease, use of drug-eluting stent [DES]) (adjusted odds ratio [OR]: 1.34; 95% CI: 1.13 to 1.58; p = 0.001). No significant interaction was observed for major risk factors (age, p = 0.11; sex, p = 0.65; diabetes, p = 0.83; hypertension, p = 0.13).
The association between the COVID pandemic and door-to-balloon longer than 30 min was confirmed after correction for baseline clinical confounders (geographic area, direct access by ambulance, ischemia time, radial access, multivessel disease, use of DES) (adjusted OR: 1.17; 95% CI: 1.05 to 1.29; p = 0.003, respectively). No significant interaction was observed for major risk factors (age, p = 0.83; sex, p = 0.49; diabetes, p = 0.55; with a significant interaction for hypertension, p = 0.044) (patients with hypertension had a shorter door-to-balloon time in 2019 [p < 0.001] but not in 2020 as compared with patients without hypertension).
No difference was observed in the rate of cardiogenic shock at presentation, infarct location, out-of-hospital cardiac arrest, or rescue procedures after failed thrombolysis.
Procedural characteristics
Concerning procedural characteristics (Table 2 ), the use of DES was more frequent in 2020 (92.7% vs. 90.6%, p = 0.003), whereas no significant difference was observed in culprit vessel, lesion location, the rate of pre- and post-procedural Thrombolysis in Myocardial Infarction flow, use of intravenous antiplatelet therapies, thrombectomy, multivessel disease, and additional in-hospital coronary revascularization.
Table 2.
Angiographic and Procedural Characteristics
| 2019 (n = 3,484) | 2020 (n = 2,811) | p Value | |
|---|---|---|---|
| Radial access | 2,945 (84.5) | 2,419 (86.1) | 0.09 |
| Culprit vessel | 0.30 | ||
| Left main | 70 (2.0) | 52 (1.8) | |
| Left anterior descending artery | 1,590 (45.6) | 1,264 (45.0) | |
| Circumflex | 484 (13.9) | 438 (15.6) | |
| Right coronary artery | 1,312 (37.8) | 1,029 (36.6) | |
| Anterolateral branch | 11 (0.2) | 6 (0.2) | |
| SVG | 17 (0.5) | 22 (0.8) | |
| Lesion location | 0.78 | ||
| Proximal | 1,732 (49.7) | 1,395 (49.6) | |
| Mid | 1,386 (39.8) | 1,134 (40.4) | |
| Distal | 366 (10.5) | 281 (10.0) | |
| In-stent thrombosis | 150 (4.3) | 128 (4.6) | 0.63 |
| Multivessel disease | 1,594 (45.8) | 1,346 (47.9) | 0.092 |
| Pre-procedural TIMI flow grade 0 | 2,114 (60.7) | 1,754 (62.4) | 0.16 |
| Thrombectomy | 652 (18.7) | 489 (17.4) | 0.17 |
| Stenting | 3,190 (91.6) | 2,589 (92.1) | 0.44 |
| Drug-eluting stent | 3,157 (90.6) | 2,607 (92.7) | 0.003 |
| Post-procedural TIMI flow grade 3 | 3,212 (92.2) | 2,567 (91.3) | 0.21 |
| Group IIb/IIIa inhibitors/cangrelor | 776 (22.3) | 671 (23.9) | 0.13 |
| Bivalirudin | 24 (0.7) | 11 (0.4) | 0.11 |
| Additional PCI | 0.12 | ||
| During the index procedure | 500 (14.4) | 442 (15.7) | |
| Staged | 415 (11.9) | 361 (12.8) | |
| DAPT therapy | 3,453 (99.0) | 2,777 (98.8) | 0.21 |
Values are n (%).
DAPT = dual antiplatelet therapy; PCI = percutaneous coronary intervention; SVG = saphenous vein graft; TIMI = Thrombolysis In Myocardial Infarction.
In-hospital clinical outcome
A significantly higher mortality was observed in 2020 as compared with 2019 (192 deaths, 6.8% vs. 169 deaths, 4.9%, OR: 1.41; 95% CI: 1.15 to 1.71; p < 0.001) (Central Illustration). The mortality rate was extremely high among patients positive for COVID-19. In fact, a total of 18 of 62 positive patients died (29% vs. 5.5%, OR: 7.0; 95% CI: 4.1 to 12.3; p < 0.001).
The significantly poorer outcomes observed in patients with STEMI treated in 2020 persisted after correction for all potential confounding factors (geographic area, direct access by ambulance, ischemia time, door-to-balloon, radial access, use of DES) (adjusted OR: 1.46; 95% CI: 1.17 to 1.82; p <0.001), and even after exclusion of the patients positive for COVID (adjusted OR: 1.43; 95% CI: 1.15 to 1.79; p < 0.001) (Central Illustration).
Discussion
The ISACS-STEMI COVID-19 registry represents the largest study of patients with STEMI undergoing mechanical reperfusion during the COVID pandemic, to date. The main finding of the present study is that the number of primary PCI procedures is significantly reduced during the pandemic (in 2020) as compared with 2019, especially in patients suffering from arterial hypertension. Nevertheless, we found a significant heterogeneity among centers that was explained neither by the local or national spread of COVID-19 nor by the local or national deaths due to the pandemic. Importantly, a higher mortality rate was observed during the COVID pandemic period, and this is likely to reflect the significantly longer ischemia time associated with treatment during this challenging time.
As of now, the COVID-19 pandemic has rapidly spread around the world, resulting in an excess death toll of several hundreds of thousands of lives, especially in Europe and the United States. The true impact of COVID-19 on cardiovascular disease and mortality is still a matter of debate. In fact, COVID-19 may have increased cardiovascular mortality due to a direct and indirect effect on occurrence and management of acute heart disease. COVID-19 has been shown to cause acute cardiac injury that varies from acute heart failure or worsening of pre-existing systolic dysfunction, cardiogenic shock, tachyarrhythmias, myopericarditis, Tako-Tsubo syndrome, or ACS (12).
Reports about the presence of inflammatory pathophysiological mechanisms, triggering plaque disruption and generating a pro-thrombotic milieu (12, 13, 14) supported an anticipated increase in the number of patients presenting with ACS during the COVID-19 pandemic.
However, initial small reports from small-sized registries showed a remarkable reduction in the number of patients with ACS. Numerous factors are likely to contribute to the finding that the number of patients seeking help for chest pain and ACS-related symptoms have decreased, with huge national and regional differences varying from −20% to −70%, compared with pre-pandemic times (2, 3, 4, 5, 6, 7). It has been speculated that during lockdown and with media attention highlighting the need to preserve health care resources for treatment of COVID-19, patients may have avoided acute treatment for fear of COVID infection, or avoidance of burdening an already overwhelmed clinical service. These behaviors may lead to increased morbidity and mortality, especially in patients with STEMI in whom a longer time delay has a significant negative impact on myocardial salvage, preservation of left ventricular function, and (short- and long-term) survival (8, 9, 10).
Furthermore, associated effects of social distancing and lockdown may have played a role, including less business-related stress, improved air quality, and a more sedentary lifestyle.
A recent small-sized report (7), including a total of 465 patients with STEMI in 54 Italian centers, showed a sizable reduction (26.5%) in STEMI procedures, more marked among women. Notably, patients with STEMI treated in 2020 had a tripled mortality rate (13.7% vs. 4.1%); however, this observation was restricted to no more than a single week, shortly after the lockdown, with fewer than 10 cases per center. An additional limitation of that study is the fact that it was not based on individual patient data, which prevents the correction for potential confounding factors.
As of now, the current study is the worldwide largest international multicenter registry in patients with STEMI who underwent mechanical reperfusion procedures, conducted in high-volume primary PCI centers. Therefore, it contributes relevant, reliable information to this controversial debate. Consistent with previous small-sized reports, we found a significant reduction in the number of patients with STEMI undergoing mechanical reperfusion; however, it was not consistent across all the centers. The results were not related to the local or national incidence of COVID or rates of death due to COVID-19.
We found a significant interaction with the decline in procedures in patients with hypertension, whereas no interaction was observed for age, sex, and diabetes. We may certainly speculate that due to the alarming message about the interplay between COVID-19 and the renin-angiotensin-aldosterone system, specifically with the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) that could have increased the expression of ACE2 and patient susceptibility to COVID-19, in addition to the large prevalence of hypertension declared among patients affected by COVID 19, and the observation that hypertension had increased risk of COVID-19 mortality (15), may have impacted more relevantly in terms of fear of contagion in this group of patients. Professional societies have overcome this uncertainty by recommending that patients receiving ACE inhibitors and ARBs should continue taking their medication (16). Despite that, and because of the absence of data to unequivocally demonstrate the safety of these drugs, the entire discussion may have made hypertensive patients feel uneasy and it may have prevented some from promptly activating the emergency system in case of chest pain.
A significant reduction in patients with STEMI was observed in 39% of the centers under investigation and was not related to the incidence of COVID disease or to the COVID mortality. Moreover, the reduction in primary PCI was not associated with the type of institutional center and significant reduction in primary PCI was seen in all geographic areas. We cannot exclude local disparities among health care organizations and management of the COVID cardiovascular emergencies, which may have affected both the fear of contagion and the risk of out-of-hospital sudden death (17,18). Both factors may have contributed to the observed heterogeneity among centers.
Furthermore, we found that the COVID-19 pandemic was associated with a significantly longer ischemia time, with higher rates of late presentation and door-to-balloon beyond 30 min, both of which contribute to a longer ischemia time. The longer door-to-balloon time may certainly be explained by organizational delay because of the specific COVID-19 protocols for screening patients and preparing equipment and personnel in the catheterization laboratory. Several additional factors may play a role in the observed longer ischemia time during the COVID pandemic. A delayed time from symptoms to first medical contact may be a consequence of both direct patient delay or emergency system–related delay, as recently described (17). In fact, we observed in 2020 a longer ischemia time despite a higher proportion of patients who were transferred by ambulance from the community to PCI hospitals.
The longer delay to treatment contributes to the significantly higher mortality observed during this pandemic, as compared with 2019. This association persisted after correction for major differences and additionally for COVID positivity. Importantly, the COVID-positive population represented a very high-risk subgroup, with mortality exceeding 25%, confirming recent smaller reports (7,18).
Scientific societies and health authorities must adapt existing guidance for the public and health care professionals, highlighting the importance of recognition and response to characteristic symptoms of acute myocardial infarction, especially among patients suffering from hypertension. In fact, recent studies in different populations and with different designs arrived at the consistent message that the continued use of ACE inhibitors and ARBs is unlikely to be harmful in patients with COVID-19 and this may certainly reduce any fear of contagiousness for these patients (19, 20, 21, 22).
Study limitations
This study is limited by its retrospective design. It was conducted during a pandemic emergency, which was challenging and expected to encounter missing data. Nevertheless, our main data analysis and conclusions are based on counts and, therefore, the overall cohort of patients was included. Furthermore, even in the analysis based on full individual patient data, this limitation and the potential risk of type II error was largely overcome by the high complete case series (>95%) and the high statistical power due to the size of the study population. Finally, even though we did not find any difference in out-of-hospital cardiac arrest, we cannot exclude that the reduction in patients with STEMI observed in 2020 may have resulted from higher rates of prehospital death due to longer delays to first medical contact, as has been described during the COVID-19 pandemic (17,18).
Conclusions
The COVID-19 pandemic had a significant impact on the treatment of patients with STEMI, resulting in a reduction in primary PCI procedures, especially among patients suffering from hypertension, and in longer delay to treatment, which may have contributed to the increased mortality during this pandemic. Our data suggest that health authorities, supported by scientific societies, should take vigorous action to prevent patients from neglecting characteristic symptoms of an acute myocardial infarction, especially among patients who suffer from hypertension.
Perspectives.
COMPETENCY IN PATIENT CARE AND PROCEDURAL SKILLS: The COVID-19 pandemic had a substantial impact on the management of patients with STEMI, resulting in a 19% reduction in primary PCI procedures, especially among patients with hypertension, and in longer delays to treatment, which could have contributed to increased mortality during the pandemic.
TRANSLATIONAL OUTLOOK: Health care authorities, supported by scientific societies, should implement strategies that deter patients from neglecting symptoms of acute myocardial infarction, and the impact of these measures should be assessed in regions where COVID-19 is prevalent.
Author Relationship With Industry
This study was promoted by the Eastern Piedmont University, Novara, Italy, without any financial support. Dr. Cortese has been funded by PRIN2017 (20178S4EK9). All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
Appendix
For a supplemental statistical analysis, tables, figures, and study organization details, please see the online version of this paper.
Appendix
References
- 1.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood S. The mystery of the missing STEMIs during the COVID-19 pandemic. tctMD. https://www.tctmd.com/news/mystery-missing-stemis-during-covid-19- pandemic Available at:
- 3.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam C.F., Cheung K.S., Lam S. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piccolo R., Bruzzese D., Mauro C. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation. 2020;141:2035–2037. doi: 10.1161/CIRCULATIONAHA.120.047457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roffi M., Guagliumi G., Ibanez B. The obstacle course of reperfusion for STEMI in the COVID-19 pandemics. Circulation. 2020;141:1951–1953. doi: 10.1161/CIRCULATIONAHA.120.047523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Rosa S., Spaccarotella C., Basso C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. SocietàItaliana di Cardiologia and the CCU Academy investigators group. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Luca G., Suryapranata H., Ottervanger J.P., Antman E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 9.De Luca G., van 't Hof A.W., de Boer M.J. Time-to-treatment significantly affects the extent of ST-segment resolution and myocardial blush in patients with acute myocardial infarction treated by primary angioplasty. Eur Heart J. 2004;25:1009–1013. doi: 10.1016/j.ehj.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Ibanez B., James S., Agewall S., ESC Scientific Document Group 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 11.Gelman A., Hill J. Cambridge University Press (Chap. 6); New York: 2007. Generalized linear models. In: Data analysis using regression and multilevel/hierarchical models. p. 109-133. [Google Scholar]
- 12.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 13.Madjid M., Vela D., Khalili-Tabrizi H., Casscells S.W., Litovsky S. Systemic infections cause exaggerated local inflammation in atherosclerotic coronary arteries: clues to the triggering effect of acute infections on acute coronary syndromes. Tex Heart Inst J. 2007;34:11–18. [PMC free article] [PubMed] [Google Scholar]
- 14.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao C., Cai Y., Zhang K. Association of hypertension and antihypertensive treatment with COVID-19 mortality: a retrospective observational study. Eur Heart J. 2020;41:2058–2066. doi: 10.1093/eurheartj/ehaa433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.European Society of Cardiology Position statement of the ESC Council on Hypertension on ACE-inhibitors and angiotensin receptor blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang Available at: Accessed June 2, 2020.
- 17.Baldi E., Sechi G.M., Mare C., Lombardia CARe Researchers Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stefanini G.G., Montorfano M., Trabattoni D. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141:2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Abajo F.J., Rodríguez-Martín S., Lerma V. MED-ACE2-COVID19 study group. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020;395:1705–1714. doi: 10.1016/S0140-6736(20)31030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sama I.E., Ravera A., Santema B.T. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41:1810–1817. doi: 10.1093/eurheartj/ehaa373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo X., Zhu Y., Hong Y. Decreased mortality of covid-19 with renin-angiotensin-aldosterone system inhibitors therapy in patients with hypertension: a meta-analysis. Hypertension. 2020;76:e13–e14. doi: 10.1161/HYPERTENSIONAHA.120.15572. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.