Abstract
Objectives
Asymptomatic carriers account for over a third of all Coronavirus Disease 19 (COVID-19) cases and are characterized by the absence of symptoms but the same infectivity as symptomatic infections. The high percentage of asymptomatic COVID-19 patients is significant in settings with specific vulnerabilities, such as homeless shelters, where the consequences of an outbreak may be dramatic. In this work, we briefly report our experience on residents and staff of homeless shelters in the City of Rome, Italy, with a particular focus on asymptomatic transmission, and compare it with the available evidence.
Methods
We performed routine Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) nasopharyngeal swab tests in all residents and staff of homeless shelters managed by the Eleemosynaria Apostolica of the Vatican City State in the city of Rome, Italy, in addition to daily symptom screening, body temperature monitoring, and application of other prevention measures.
Results
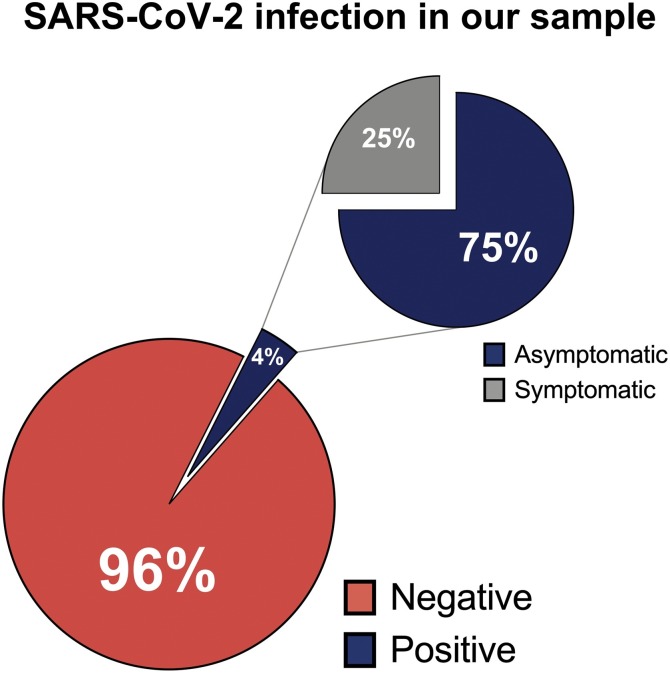
We evaluated 298 persons and identified twelve positive cases (4%). Most of the positive cases (75%) were asymptomatic, while only three patients reported symptoms that included fever, diarrhea, and cough.
Conclusions
Our data confirm the importance of early identification of asymptomatic carriers that could, in vulnerable conditions such as homeless shelters, spread the infection and cause outbreaks with severe consequences on individual and public health.
Keywords: COVID-19, SARS-CoV-2, Homeless population, Vulnerable populations, Homeless shelters
As of November 29, 2020, the Coronavirus Disease 19 (COVID-19) pandemic caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has been characterized by more than 60 million cases worldwide, over 1.4 million deaths, and nearly 43 million persons discharged. Although the main symptoms of COVID-19 include fever, cough, respiratory difficulties, fatigue, and loss of smell and taste, up to severe complications such as interstitial pneumonia and acute respiratory distress syndrome, a large portion of cases are asymptomatic (Kronbichler et al., 2020).
Asymptomatic carriers account for about 40% of COVID-19 cases and are characterized by the absence of symptoms but the same infectivity as symptomatic infections (Chen et al., 2020). Furthermore, asymptomatic cases can lead to significant subclinical lung abnormalities in a short time, suggesting that the absence of symptoms may not imply the absence of harm. In a recent review and meta-analysis published by Kronbichler et al. (2020), the first systematic analysis of asymptomatic COVID-19 cases in the literature, the authors focused on the role of asymptomatic SARS-CoV-2 carriers in disease transmission. They concluded that they represent a significant portion of COVID-19 patients and their early identification is extremely important to prevent transmission. The authors also reported that more than half of the 506 asymptomatic patients from 34 studies included in their meta-analysis had lung alterations on computed tomography, mainly ground-glass opacities, although with normal laboratory findings in the majority of cases. A similar result was reported in a study on the outbreak of the Diamond Princess cruise ship in February 2020; in fact, 73% of the cases were asymptomatic or paucisymptomatic, and over half of them presented lung abnormalities at computed tomography (Tabata et al., 2020).
The large number of asymptomatic patients is an extremely important characteristic of SARS-CoV-2 infection; however, it becomes even more important in settings with specific vulnerabilities, such as homeless shelters, where the consequences on individual and public health may be dramatic (Karb et al., 2020). In homeless shelters characterized by the physical proximity of residents, elevated population density, a limited use of face masks, and often precarious hygienic conditions outside the shelter, the reported prevalence of COVID-19 is higher than the general population (Karb et al., 2020). Also, homeless persons have more physical and mental comorbidities, usually undiagnosed and uncontrolled, that may worsen the disease's course. In these congregated living settings, asymptomatic cases represent the most common means of contagion, as reported by Baggett in Boston (Baggett et al., 2020), Tobolowsky in Seattle and King County (Tobolowsky et al., 2020), and Imbert in San Francisco (Imbert et al., 2020) (Table 1 ).
Table 1.
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) outbreaks in homeless shelters available in the scientific literature.
| Author | Location | SARS-CoV-2 Positive (%) | Symptoms | Asymptomatic rate (%) |
|---|---|---|---|---|
| Baggett et al. (2020) | Boston, USA | 36% | Fever (0.7%), cough (7.5%), shortness of breath (1.4%) | 87.8% |
| Tobolowsky et al. (2020) | Seattle and King County, USA | 18.5% | Not reported | Not reported |
| Imbert et al. (2020) | San Francisco, USA | 67% | Fever, cough, shortness of breath, pain when breathing | 52.9% |
Our experience is consistent with these findings. Over the past months, we performed routine SARS-CoV-2 Real-Time Reverse-transcription Polymerase Chain Reaction (rRT-PCR) nasopharyngeal swab tests in all residents and staff of homeless shelters managed by the Eleemosynaria Apostolica of the Vatican City State in the city of Rome, Italy, in addition to daily symptom screening and body temperature monitoring. Tests were performed at admission and routinely afterward. Additional prevention measures were implemented, including mandatory use of face masks, daily health education programs, application of hygiene protocols, and adequate distancing. As of October 31, 2020, we evaluated 298 persons and identified twelve positive cases, with a prevalence of infection of 4%. Most of the positive cases (75%) were asymptomatic at the time of the testing and in the 14 days before, while only three patients had symptoms that included fever, diarrhea, and cough (Figure 1 ).
Figure 1.
Results of routine Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Real-Time Reverse transcription-polymerase Chain Reaction (rRT-PCR) nasopharyngeal swab tests in residents and staff of homeless shelters managed by the Eleemosynaria Apostolica of the Vatican City State in the city of Rome, Italy. The large pie chart represents the number of positive/negative cases; the small pie chart represents the number of symptomatic/asymptomatic positive cases.
Our data, along with the evidence available in the literature, confirm the importance of early identification of asymptomatic carriers that could, in particularly vulnerable conditions such as homeless shelters, spread the infection and cause outbreaks with severe consequences (Ralli et al., 2020). In fact, asymptomatic cases in these settings may rapidly spread COVID-19 among other residents and staff, leading to more severe forms of COVID-19 due to the higher number of comorbidities and precarious health conditions among homeless persons (Tsai and Wilson, 2020), as well as to closures of the shelters with resident relocation in alternative structures (Bodkin et al., 2020).
In conclusion, the role of asymptomatic carriers must always be considered, especially in vulnerable settings and congregate living conditions. Prevention measures including routine surveillance with molecular and nasopharyngeal antigen swabs and serological tests, in addition to other measures such as strict hygiene rules inside and outside the shelter, adequate distancing protocols, continuous symptom screening, and health education programs, should be implemented in all homeless shelters to intercept new clusters of infection and prevent outbreaks. Concurrently, temporary shelter closures may have severe effects on residents and public health, and alternative residential solutions should be carefully planned and made promptly available in case of outbreaks.
Funding
None declare.
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
Not applicable.
Acknowledgments
The authors wish to thank His Holiness Pope Francis for providing directions, structures, and equipment to make healthcare available for vulnerable populations through the Offices of Papal Charities (Eleemosynaria Apostolica), and Cardinal Konrad Krajewski, Apostolic Almoner, for the extraordinary efforts in the realization of this mission.
References
- Baggett T.P., Keyes H., Sporn N., Gaeta J.M. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020;323(21):2191–2192. doi: 10.1001/jama.2020.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodkin C., Mokashi V., Beal K., Wiwcharuk J., Lennox R., Guenter D., et al. Pandemic planning in homeless shelters: a pilot study of a COVID-19 testing and support program to mitigate the risk of COVID-19 outbreaks in congregate settings. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa743. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Wang A.H., Yi B., Ding K.Q., Wang H.B., Wang J.M., et al. [Epidemiological characteristics of infection in COVID-19 close contacts in Ningbo city] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(5):667–671. doi: 10.3760/cma.j.cn112338-20200304-00251. [DOI] [PubMed] [Google Scholar]
- Imbert E., Kinley P.M., Scarborough A., Cawley C., Sankaran M., Cox S.N., et al. Coronavirus disease 2019 (COVID-19) outbreak in a San Francisco homeless shelter. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1071. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karb R., Samuels E., Vanjani R., Trimbur C., Napoli A. Homeless shelter characteristics and prevalence of SARS-CoV-2. West J Emerg Med. 2020;21(5):1048–1053. doi: 10.5811/westjem.2020.7.48725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronbichler A., Kresse D., Yoon S., Lee K.H., Effenberger M., Shin J.I. Asymptomatic patients as a source of COVID-19 infections: a systematic review and meta-analysis. Int J Infect Dis. 2020;98:180–186. doi: 10.1016/j.ijid.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralli M., Cedola C., Urbano S., Morrone A., Ercoli L. Homeless persons and migrants in precarious housing conditions and COVID-19 pandemic: peculiarities and prevention strategies. Eur Rev Med Pharmacol Sci. 2020;24(18):9765–9767. doi: 10.26355/eurrev_202009_23071. [DOI] [PubMed] [Google Scholar]
- Tabata S., Imai K., Kawano S., Ikeda M., Kodama T., Miyoshi K., et al. Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis. Lancet Infect Dis. 2020;20(9):1043–1050. doi: 10.1016/S1473-3099(20)30482-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobolowsky F.A., Gonzales E., Self J.L., Rao C.Y., Keating R., Marx G.E., et al. COVID-19 outbreak among three affiliated homeless service sites—King County, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):523–526. doi: 10.15585/mmwr.mm6917e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J., Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5(4):e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]