Abstract
Background
The novel coronavirus (COVID-19) was recently declared a pandemic by the World Health Organization (WHO). The first confirmed case in Saudi Arabia was announced on March 2, 2020. Several psychiatric manifestations may appear during pandemics, especially among frontline healthcare providers.
Objectives
This study sought to explore depression and anxiety levels among healthcare providers during the COVID-19 outbreak in Saudi Arabia.
Methods
This was a cross-sectional study of a convenience sample of 502 healthcare providers in the Ministry of Health. Depression and anxiety were assessed via the Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder 7 (GAD-7) questionnaires, respectively.
Results
The respondents represented various healthcare occupations: administrators (28.49%), nurses (26.29%), physicians (22.11%), non-physician specialists (13.94%), technicians (6.77%), and pharmacists (2.30%). The majority of them were male (68.1%). More than half of them had depressive disorder (55.2%), which ranged from mild (24.9%), moderate (14.5%), and moderately severe (10%) to severe (5.8%). Half of the sample had generalized anxiety disorder (51.4%), which ranged from mild (25.1%) and moderate (11%) to severe (15.3%). Multivariate analysis showed that males were significantly less predicted to have anxiety (Beta = −0.22, P-value <0.04), 30–39 years age group were significantly more predicted to have depression and anxiety group (Beta = 0.204, P-value <0.001 and beta = 0.521, P-value <0.003 respectively), and nurses had significantly higher mean score of anxiety (Beta = 0.445, P-value <0.026).
Conclusions
This study revealed that depression and anxiety are prevailing conditions among healthcare providers. Although efforts were accelerated to support their psychological well-being, more attention should be paid to the mental health of female, 30–39 age group and nursing staff. Promoting healthcare service as a humanitarian and national duty may contribute to making it a more meaningful experience in addition to advocating for solidarity, altruism, and social inclusion. Longitudinal research studies need to be conducted to follow up on healthcare providers’ mental health symptoms and develop evidence-based interventions.
Keywords: Depression, Anxiety, Healthcare providers, COVID-19, Pandemic
Introduction
An idiopathic pneumonia began in Wuhan, China in December 2019 [1]. The first case with a similar presentation discovered outside China was in Thailand on January 13, 2020 [2]. The World Health Organization (WHO) gave this new coronavirus disease the name COVID-19 on February 2020 [3]. One month afterward, the WHO declared COVID-19 a global pandemic on March 11, 2020 [2]. Coronaviruses are a group of viruses that can infect humans and animals and the cause of severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and COVID-19 [1]. Saudi Arabia announced its first case of COVID-19 on March 2, 2020 [4]. Psychiatric symptoms and illnesses may emerge secondary to an infectious disease outbreak. They may appear during the acute phase or at later stages. Several presentations could appear, ranging from mild mood and anxiety symptoms to psychosis and significant cognitive deficits [5]. The outbreak itself is a stressful event and it is even more stressful to be a healthcare provider who works in the first line to tackle such serious illness [6]. Several factors play important roles in responses to trauma, including the presence of prior psychiatric history, coping styles, culture, and support systems. In addition to being overwhelmed, it is also stressful to deal with shortages of medical equipment and concerns over infecting family members [7,8]. In China, where COVID-19 started, a cross-sectional study was conducted on 31 hospitals to measure factors linked with mental health outcomes among healthcare providers who encountered COVID-19; this study showed that frontline nurses and healthcare providers had a greater risk of negative mental health outcomes [9]. As far as we know, no local study has addressed this topic yet. We aim to explore the depression and anxiety prevalence among healthcare providers during the COVID-19 outbreak in Saudi Arabia and identify their severity.
Materials and methods
Study design
For this study, data were collected via a cross-sectional survey during the COVID-19 outbreak on March 2020. Ethical approval was provided from the Institutional Review Board at Princess Nourah Bint Abdulrahman University (PNU) in Riyadh, Saudi Arabia. The aims of the study were elucidated and the participants gave their informed consent to participate in the study.
Sample population
This study included both male and female participants who were healthcare providers and Arabic speakers living in Saudi Arabia at the time of the study.
Recruitment
Convenience sampling technique and Google forms were used to collect responses. The sample size was calculated using Raosoft software [10]. The required sample size was estimated at the 95-confidence level with an estimated 50% response distribution and a margin of error of ±5%. The recommended minimum sample size is 384. An online survey was sent to all healthcare providers from different specialties and levels who were working in COVID-19 centers at the Ministry of Health and living in Saudi Arabia. They received the online survey through emails and phone messages, which was arranged by collaborators in the internal communication channels at the health clusters of Riyadh, Qassim and Eastern region.
Data collection
The online survey contained three components. First, the survey recorded socio-demographic characteristics, including age, gender, level of education, and living region. Second, survey included the Patient Health Questionnaire (PHQ-9), which is a widely used and valid tool for detecting depression and has 9 items with Likert-scale answers rated from 0 (not experienced at all) to 3 (experienced nearly daily). These items detect depressive symptoms that occurred during the last two weeks. The final participant’s score is out of 27, which is categorized by the total mean score as mild (score of 5–9), moderate (score 10–14), moderately severe (score 15–19), or severe (score 20–27) [11]. Internal consistency was evaluated using Cronbach’s alpha (α = 0.89). Finally, the survey also included the Generalized Anxiety Disorder 7 (GAD-7) questionnaire, which is also a valid tool for detecting anxiety and has 7 items with Likert-scale answers. The final participant’s score is out of 21 is categorized by the total mean score as mild (score of 5–9), moderate (score 10–14), or severe (score 15–21). Internal consistency was evaluated using Cronbach’s alpha (α = 0.95). Arabic versions of both scales are valid and reliable for screening for depression and anxiety [12].
Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 23.0 software (SPSS Inc., Chicago, IL, USA), which was used for data entry and statistical analysis. We calculated percentages and frequencies for all nominal variables for the different items of the PHQ-9 and GAD-7. Also, we calculated the mean, median, and standard deviation ranges of the total scores of the items of the PHQ-9 and GAD-7. We used non-parametric Mann–Whitney U tests or Kruskal–Wallis tests to compare the total scores of depression (PHQ-9) and total scores of anxiety (GAD-7) with respect to demographic characteristics. Results are considered significant for P-values below 0.05 (P < 0.05). In order to ascertain the findings from the bivariate analysis, the generalized mixed linear models were used to assess the combined and individual associations between the sociodemographic characteristics and the mean of depression and anxiety scores. The association between these characteristics with the depression and anxiety scores were expressed as beta coefficients. The anxiety and depression scores were log-transformed to stabilize their variance via taking the natural logarithm of the mean scores after adding a constant ( = 1) to each participant’s scores of depression and anxiety to get rid of the zero scores when taking the natural logarithm. The statistical significance alpha level was considered at 0.05 level. However, because the anxiety is a known sign of depression, we added the GAD score as a covariate in the analysis in order to adjust the associations between the factors after partialing out the effect of any underlying anxiety [13].
Results
Sociodemographic characteristics
A total of 502 healthcare providers responded to the survey. The sociodemographic characteristics of the surveyed population are presented in Table 1 . The majority of the respondents were male (68.1%) and held a university degree or above (85.5%). More than half of them were 30–39 years old (55.4%). The respondents represented various healthcare occupations: administrators (28.49%), nurses (26.29%), physicians (22.11%), non-physician specialists (13.94%), technicians (6.77%), and pharmacists (2.30%). They were living in diverse regions, including the Qassim region (60.96%), Riyadh region (28.29%), Eastern region (9.16%), and other regions (1.59%).
Table 1.
Frequencies or means of demographic characteristics, by depressive and anxiety symptom score (N = 502).
| Characteristics | Total (%) | Depressive symptom score ± SD | Anxiety symptom score ± SD |
|---|---|---|---|
| Gender | |||
| Male | 342 (68.1%) | 6.56 ± 6.53 | 5.93 ± 6.45 |
| Female | 160 (31.9%) | 8.11 ± 6.17** | 7.43 ± 6.10** |
| Age groups | |||
| 18–29 y | 38 (7.6%) | 7.24 ± 6.70 | 6.58 ± 6.53 |
| 30–39 y | 278 (55.4%) | 8.27 ± 6.37*** | 7.40 ± 6.59** |
| 40–49 y | 141 (28.1%) | 5.40 ± 6.35 | 4.83 ± 5.63 |
| 50 y+ | 45 (8.9%) | 4.62 ± 5.29 | 5.11 ± 5.99 |
| Educational levels | |||
| Secondary or less | 73 (14.5%) | 5.88 ± 6.50 | 5.81 ± 6.52 |
| University or higher | 429 (85.5%) | 7.26 ± 6.43* | 6.51 ± 6.35 |
| Region of residence | |||
| Riyadh region | 142 (28.29%) | 9.07 ± 7.38*** | 8.04 ± 6.88*** |
| Qassim region | 306 (60.96%) | 6.10 ± 5.93 | 5.54 ± 6.01 |
| Eastern region | 46 (9.16%) | 6.67 ± 5.06 | 6.54 ± 5.78 |
| Occupations | |||
| Physician | 111 (22.11%) | 7.45 ± 6.68 | 6.74 ± 5.79 |
| Nurse | 132 (26.29%) | 8.80 ± 6.82* | 7.49 ± 6.27* |
| Administrator | 143 (28.49%) | 6.82 ± 6.03 | 6.38 ± 6.78 |
| Pharmacist | 12 (2.30%) | 5.92 ± 5.68 | 4.50 ± 4.91 |
| Non-physician specialist | 70 (13.94%) | 5.43 ± 5.69 | 4.66 ± 6.03 |
| Technician | 34 (6.77%) | 5.74 ± 6.39 | 5.50 ± 7.25 |
P < 0.05.
P < 0.001.
P < 0.0001.
Depressive symptoms among healthcare providers
Table 2 displays the healthcare providers’ responses to the 9 items of the PHQ-9. Through the last 2 weeks preceding the survey these providers responded affirmatively to the following as occurring for several days, more than half the days, or nearly every day: feeling tired or having little energy (67.9%); little interest or pleasure in doing things (58.5%); trouble falling or staying asleep or sleeping too much (57.9%); poor appetite or overeating (55.5%); feeling down, depressed, or hopeless (52.2%); trouble concentrating on things, such as reading the newspaper or watching television (44.1%); moving or speaking so slowly that other people could have noticed; so fidgety or restless that you have been moving around a lot more than usual (33.1%); feeling bad about yourself or that you are a failure or have let yourself or your family down (25.4%); and thoughts that you would be better off dead or of hurting yourself in some way (9.2%). However, although more than half of the respondents had depressive disorder (55.2%), which was mild (24.9%), moderate (14.5%), moderately severe (10%), or severe (5.8%).
Table 2.
Responses to depression symptoms.
| Depression symptoms: | Not at all | Several days | More than half the days | Nearly every day |
|---|---|---|---|---|
| 1- Little interest or pleasure in doing things. | 208 (41.4%) | 142 (28.3%) | 83 (16.5%) | 69 (13.7%) |
| 2- Feeling down, depressed, or hopeless. | 240 (47.8%) | 138 (27.5%) | 69 (13.7%) | 55 (11.0%) |
| 3- Trouble falling or staying asleep, or sleeping too much. | 211 (42.0%) | 123 (24.5%) | 83 (16.5%) | 85 (16.9%) |
| 4- Feeling tired or having little energy. | 161 (32.1%) | 180 (35.9%) | 82 (16.3%) | 79 (15.7%) |
| 5- Poor appetite or overeating. | 223 (44.4%) | 113 (22.5%) | 93 (18.5%) | 73 (14.5%) |
| 6- Feeling bad about yourself, or that you are a failure or have let yourself or your family down. | 375 (74.7%) | 58 (11.6%) | 44 (8.8%) | 25 (5.0%) |
| 7- Trouble concentrating on things, such as reading the newspaper or watching television. | 281 (56.0%) | 120 (23.9%) | 53 (10.6%) | 48 (9.6%) |
| 8- Moving or speaking so slowly that other people could have noticed? Or the opposite-being so fidgety or restless that you have been moving around a lot more than usual? | 336 (66.9%) | 90 (17.9%) | 47 (9.4%) | 29 (5.8%) |
| 9- Thoughts that you would be better off dead or of hurting yourself in some way | 456 (90.8%) | 22 (4.4%) | 13 (2.6%) | 11(2.2%) |
Anxiety symptoms among healthcare providers
Table 3 displays the participants’ responses to the 7 items of the GAD-7. Through the last 2 weeks preceding the survey for several days, these providers responded affirmatively to the following as occurring more than half the days or nearly every day: feeling nervous, anxious or on edge (62.6%); worrying too much about different things (61.7%); trouble relaxing (55.9%); becoming easily annoyed or irritable (55%); not being able to stop or control worrying (49.4%); feeling afraid as if something awful might happen (46.4%); and being so restless that it is hard to sit still (42.1%). Although half of the respondents had generalized anxiety disorder (51.4%), their cases ranged from mild (25.1%) or moderate (11%) to severe (15.3%).
Table 3.
Responses to anxiety symptoms.
| Anxiety symptoms | Not at all | Several days | More than half the days | Nearly every day |
|---|---|---|---|---|
| 1- Feeling nervous, anxious or on edge | 188 (37.5%) | 177 (35.3%) | 62 (12.4%) | 75 (14.9%) |
| 2- Not being able to stop or control worrying | 254 (50.6%) | 120 (23.9%) | 69 (13.7%) | 59 (11.8%) |
| 3- Worrying too much about different things | 192 (38.2%) | 151 (30.1%) | 84 (16.7%) | 75 (14.9%) |
| 4- Trouble relaxing | 221 (44.0%) | 139 (27.7%) | 77 (15.3%) | 65 (12.9%) |
| 5- Being so restless that it is hard to sit still | 291 (58.0%) | 117 (23.3%) | 61 (12.2%) | 33 (6.6%) |
| 6- Becoming easily annoyed or irritable | 226 (45.0%) | 150 (29.9%) | 65 (12.9%) | 61 (12.2%) |
| 7- Feeling afraid as if something awful might happen | 269 (53.6%) | 112 (22.3%) | 53 (10.6%) | 68 (13.5%) |
Differences in mental health based on sociodemographic characteristics
A number of sociodemographic variables were significantly associated with depression and anxiety, as shown in Table 1. Females had higher scores of depression and anxiety, compared to males (Mean ± SD: 8.11 ± 6.17 and 7.43 ± 6.10, respectively) (P-value <0.001). About third of the female respondents had moderate to severe levels of depression and anxiety (33.6% and 30.7%, respectively). The 30–39 age group had higher scores of depression and anxiety than other age groups (Mean ± SD: 8.27 ± 6.37 and 7.40 ± 6.59, respectively) (P-value <0.0001 and <0.001, respectively). Third or more of the 30–39 age group respondents had moderate to severe levels of depression and anxiety (38.4% and 33.1%, respectively). Nurses had higher scores of depression and anxiety than other healthcare providers, such as physicians, pharmacists, specialists, technicians, and administrators (Mean ± SD: 8.80 ± 6.82 and 7.49 ± 6.27, respectively) (P-value <0.05). Third or more of the nurses had moderate to severe levels of depression and anxiety (37.9% and 32.9%, respectively). Healthcare providers living in the Riyadh region had higher scores of depression and anxiety than respondents living in other regions (Mean ± SD: 9.07 ± 7.38 and 8.04 ± 6.88, respectively) (P-value <0.0001). Finally, healthcare providers with university degrees or above had higher score of depression than respondents with secondary school degrees or less (Mean ± SD: 7.26 ± 6.43) (P-value <0.05).
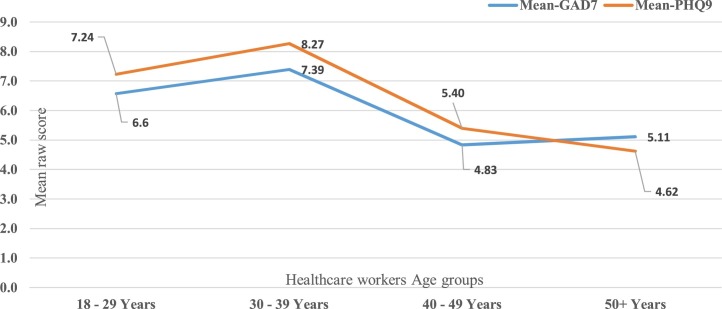
The analysis plan considered a step further via using the multivariate analysis method. Table 4 displays the findings from the analysis model. It shows that male respondents were found to be significantly less predicted to have generalized anxiety on average than female (Beta = −0.22, P-value <0.04). The analysis model suggested that 30–39 years age group were predicted to have been significantly more depressed and anxious compared to ≥50 age group (Beta = 0.204, P-value <0.001 and beta = 0.521, P-value <0.003 respectively). Also, healthcare providers aged between 40–49 years were found to be significantly more depressed than those aged ≥50 years (Beta = 0.108, P-value <0.05). Fig. 1 shows the association between healthcare providers’ age groups and their corresponding mean anxiety and depression scores, indicating that healthcare providers’ age correlated significantly and negatively with their depression score. In addition, nurses had significantly higher mean log-transformed anxiety score than technicians (Beta = 0.445, P-value <0.026). However, the analysis model found that participants’ anxiety score (log transformed GAD-7 score) converged statistically significantly and positively on their mean log transformed depression score (Beta = 0.375, P-value <0.001) indicating that participants’ anxiety predicted significantly higher depression. On the other hand, the healthcare providers’ educational level, residential location and occupation did not converge significantly on their mean log-transformed depression and anxiety score in the multivariate analysis. And the gender did not converge significantly on their mean log-transformed depression score.
Table 4.
Generalized linear mixed model explaining the association of sociodemographic characteristics with depression and anxiety scores (N = 502).
| Characteristics | Beta coefficient (95%CI) for depression | Beta coefficient (95%CI) for anxiety |
|---|---|---|
| Gender | ||
| Male | −0.04 (−0.10 to 0.02) | −0.22 (−0.43 to −0.02)* |
| Female (reference) | 0 | 0 |
| Age groups | ||
| 18–29 y | 0.13 (−0.01 to 0.26) | 0.24 (−0.029 to 0.922) |
| 30–39 y | 0.20 (0.10–0.31)*** | 0.52 (0.15–0.87)** |
| 40–49 y | 0.11 (0.001–0.216)* | 0.15 (−0.21 to 0.50) |
| 50 y+ (reference) | 0 | 0 |
| Educational levels | ||
| Secondary or less | −0.01 (−0.10 to 0.08) | 0.05 (−0.24 to 0.34) |
| University or higher | 0 | 0 |
| Region of residence | ||
| Riyadh region | 0.03 (−0.07 to 0.13) | 0.16 (−0.19 to 0.50) |
| Qassim region | 0.02 (−0.08 to 0.11) | −0.18 (−0.50 to 0.14) |
| Eastern region | 0 | 0 |
| Occupations | ||
| Physician | 0.15 (−0.10 to 0.39) | 0.81 (−0.09 to 1.70) |
| Nurse | 0.10 (−0.02 to 0.21) | 0.45 (0.05–0.84)* |
| Administrator | 0.05 (−0.07 to 0.17) | 0.31 (−0.08 to 0.69) |
| Pharmacist | 0.01 (−0.19 to 0.21) | 0.07 (−0.61 to 0.75) |
| Non-Physician specialist | 0.06 (−0.07 to 0.18) | 0.03 (−0.40 to 0.46) |
| Technician | 0 | 0 |
| GAD-7 score | 0.38 (0.34–0.41)*** | |
P < 0.05.
P < 0.01.
P < 0.001.
Fig. 1.
The association between healthcare providers’ age groups and their corresponding mean raw anxiety and depression scores.
Exploring healthcare providers’ emotions and needs
Various emotions and needs were reported in response to an exploratory question. Negative emotions were reported by 62.15% of the respondents. These emotions included fears about being the cause of spreading the virus to family or other people outside the hospital, anxiety toward the uncertainty and toward people who are uncommitted to social distancing instructions, exhaustion and stress from the workload, and depression with hopelessness. On the other hand, positivity was also reported by 37.85% of the respondents. Many healthcare providers were proud of themselves and feeling happy to serve the country. Many of them were also hopeful, optimistic, or having faith in God’s will. However, their needs were workplace-centered; many of them reported needing more physical, psychological, and financial support in the workplace.
Discussion
It is important to investigate mental health conditions among healthcare providers due to the possible impacts of such conditions on their health and on the quality of patient care [14]. This study is the first to investigate the prevalence of depression and anxiety during the COVID-19 outbreak in Saudi Arabia among healthcare providers from 3 prominent regions in Saudi Arabia and representing various specialties at Ministry of Health. We found that depression and anxiety were prevalent among healthcare providers (55.2% and 51.4%, respectively). We also found that female respondents and nurses had significantly higher mean score of anxiety. And healthcare providers aged from 30 to 39 years had significantly higher mean scores of depression and anxiety. During the COVID-19 outbreak, a Chinese study similarly reported a high prevalence of psychiatric symptoms among 1257 healthcare providers, mainly depression, anxiety and distress (50.4%, 44.6% and 71.5% respectively). Also, similarly, more severe symptoms were reported by nurses and female respondents [9]. In addition, similar recent results of depression and anxiety prevalence were found among ophthalmologists in Saudi Arabia during COVID-19 pandemic (50.5% and 46.7%, respectively). Also, similarly, anxiety was significantly higher among female ophthalmologists [15]. Moreover, the psychological impact of the pandemic on the Saudi general population have been assessed recently and showed lower prevalence of depression and anxiety symptoms compared to our study (40.9% and 29.9%, respectively) [16]. Similarly, the results among Saudi general population indicated that health care providers and females had higher levels of depression, anxiety and stress [16]. Another similar findings were shown in recent Jordanian study, which identified females and pulmonologists as a higher risk of depression group among healthcare providers during COVID-19 pandemic [17]. However, the prevalence of depression and anxiety symptoms among healthcare providers in our study was much lower compared to Jordan (78.1% and 70.8%, respectively) [17]. In another Chinese study, nurses expressed irritability, excitability, and signs of psychological distress. Medical staff were fearful about transmitting the virus to their families. They prioritized the need for rest and protective supplies and psychological skills training for dealing with the patients’ emotional distress [18]. In our study, it was expected that females would have significantly higher levels of anxiety as this disorder is generally more frequent among women [19].
A similar total anxiety prevalence (52%) was found in 2017 among emergency healthcare workers in Saudi Arabia at one of the largest emergency units in the area and level I trauma center. However, the prevalence of severe anxiety in our study was twice the prevalence in this previous study (15.3% versus 7.6%) [20]. These results indicate higher levels of anxiety, compared to any anxiety disorder, among the Saudi population (16%) [21]. Anxiety during emergency situations may be explained by work-related stress and high job demands [22]. Other studies that were conducted among healthcare providers during the SARS outbreak suggested some sources of distress: social stigmatization; family members’ ostracism; social isolation; loss of control; health of self, family and others; changes in work; and spread of the virus [23,24]. A lack of recognition of anxiety symptoms may lead to serious psychological consequences [21].
It is not surprising that nurses reported significantly higher mean score of anxiety than other healthcare providers. The literature has shown that, compared to other professionals, healthcare providers, especially nurses, have a higher risk of developing emotional distress like depression, anxiety, and burnout due to work-related stress [25]. Moderate stress was also evident among frontline nurses in Saudi Arabia who were highly perceived infectability to COVID-19 and germ aversion [26]. There are factors that appeared to increase the risk of developing anxiety symptoms among Chinese nurses, like poor nurse-patient relationships, over-commitment, and lower job rank [27]. Another study that was conducted among nursing staff from various nationalities in Saudi Arabia found that having a Middle Eastern nationality, divorce or widowed marital status, a lack of physical activities, and smoking are risk factors for anxiety and depression [28]. In addition, physical and mental conditions, like depression and anxiety, may be affected by the nurse’s shift timing [29]. Emergency nurses also reported job difficulties like higher work demands, less decision-making authority, and lower financial or social recognition [22]. Previous studies that were conducted among healthcare providers during pandemics illustrated that clinical staff (doctors and nurses) and staff who were working with SARS patients reported significantly higher levels of anxiety [23]. The SARS outbreak had caused increased levels of distress among emergency staff, especially nurses, followed by doctors. Nurses coped mainly through behavioral disengagement and doctors coped mainly through planning, whereas healthcare assistants coped through self-distractions [24]. Frontline nurses may also have higher risk of infection due to their frequent, close contact with the patients and long working hours [30,31].
On the other hand, the significantly higher mean scores of depression and anxiety among the 30–39 age group is similar to the Jordanian study conducted during COVID-19 pandemic, which demonstrated that the ≥50 years age group of healthcare providers had a significant lower risk to develop depression [17]. This is also consistent with previous studies that found increased prevalence of psychiatric disorders among younger adults [[32], [33], [34]]. This finding may be explained by the less adaptive way reacting to stressors [35] and the age-related biopsychosocial changes [36]. It may also be attributed to the higher response rate as they represent 55.4% of our sample.
Limitations
Although this study is the first Saudi survey to explore mental health among healthcare providers, it has multiple limitations. First, the majority of the respondents was from the Qassim region (60.96%), which limits the generalization of our findings to more-affected regions. Second, this study did not assess respondents’ previous histories of mental health conditions, which may have existed before the COVID-19 outbreak. Third, response bias is also possible in convenience sampling. Fourth, this cross-sectional study design is unable to make causal conclusions. Finally, many important variables were not considered in the study for time purpose, as we aimed to make the shortest possible version of the survey in order to increase the response rate during the busy time of the healthcare providers during COVID-19 outbreak. Examples of these important variables that might have association with depression or anxiety include got infected with COVID-19, had a colleague or family member infected with COVID-19, years of experience and had a negative experience with previous outbreaks.
Conclusions
In conclusion, depression and anxiety symptoms occurred in a frequency of 55.2% and 51.4% among healthcare providers in Saudi Arabia with varied severity, as half of those had mild conditions and the rest ranged from moderated to severe. However, more attention should be paid to the mental health of nursing, female staff, and the 30–39 age group. Routine checkups for the mental status should be implemented especially during pandemics. It is also important to ensure that the physical needs of healthcare providers, including sufficient sleep and protected times and places to rest, are met. Promoting healthcare service as a humanitarian and national duty may contribute toward making it a more meaningful experience, in addition to advocating for solidarity, altruism, and social inclusion. Psychiatric and psychotherapeutic interventions may enhance psychological resilience and well-being during the COVID-19 epidemic [37]. Finally, longitudinal research studies need to be conducted to follow up regarding the participants’ mental health symptoms and for evidence-based interventions.
Funding
No funding sources.
Competing interests
None declared.
Ethical approval
Not required.
Acknowledgements
This research was funded by the Deanship of Scientific Research at Princess Nourah Bint Abdulrahman University through the Fast-track Research Funding Program.
References
- 1.World Health Organization; 2020. Coronavirus disease (COVID-19) pandemic.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- 2.World Health Organization; 2020. WHO timeline — COVID-19. [Google Scholar]
- 3.World Health Organization; 2020. Rolling updates on coronavirus disease (COVID-19)https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [Google Scholar]
- 4.REUTERS; 2020. Saudi Arabia announces first case of coronavirus.https://www.reuters.com/article/us-health-coronavirus-saudi/saudi-arabia-announces-first-case-of-coronavirus-idUSKBN20P2FK [Google Scholar]
- 5.Huremović D. Springer; Cham: 2019. Psychiatry of pandemics: a mental health response to infection outbreak. [DOI] [Google Scholar]
- 6.Stress and Coping . 2020. Centers for disease control and prevention.https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html [Google Scholar]
- 7.Send in the therapists? Lancet Psychiatry. 2019;7:291. doi: 10.1016/S2215-0366(20)30102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayanian J.Z. Mental health needs of health care workers providing frontline COVID -19 Care. JAMA Health Forum. 2020 doi: 10.1001/jamahealthforum.2020.0397. Published online April 1, 2020. [DOI] [PubMed] [Google Scholar]
- 9.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. 2020;3:1–12. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sample size calculator by Raosoft, Inc. n.d. http://www.raosoft.com/samplesize.html. [Accessed 16 August 2020].
- 11.Löwe B., Gräfe K., Zipfel S., Witte S., Loerch B., Herzog W. Diagnosing ICD-10 depressive episodes: superior criterion validity of the patient health questionnaire. Psychother Psychosom. 2004;73:386–390. doi: 10.1159/000080393. [DOI] [PubMed] [Google Scholar]
- 12.Alhadi A.N., Alateeq D.A., Al-Sharif E., Bawazeer H.M., Alanazi H., Alshomrani A.T. An Arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017:1–9. doi: 10.1186/s12991-017-0155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroenke K., Wu J., Yu Z., Bair M.J., Kean J., Stump T. Patient health questionnaire anxiety and depression scale: initial validation in three clinical trials. Psychosom Med. 2016;78:716–727. doi: 10.1097/PSY.0000000000000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haynes C. Stress in health professionals. Psychologist. 2000;13:128–129. [Google Scholar]
- 15.Almater A., Tobaigy M., Younis A., Alaqeel M., Abouammoh M. Effect of 2019 coronavirus pandemic on ophthalmologists practicing in Saudi Arabia: a psychological health assessment. Middle East Afr J Ophthalmol. 2020;27:79–85. doi: 10.4103/meajo.MEAJO_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alkhamees A.A., Alrashed S.A., Alzunaydi A.A., Almohimeed A.S., Aljohani M.S. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102 doi: 10.1016/j.comppsych.2020.152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 2020;n/a:e01730. doi: 10.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization; 2018. Gender and women’s mental health.https://www.who.int/mental_health/prevention/genderwomen/en/ [Google Scholar]
- 20.Alharthy N., Alrajeh O.A., Almutairi M., Alhajri A. Assessment of anxiety level of emergency health-care workers by generalized anxiety disorder-7 tool. Int J Appl Basic Med Res. 2017;7:150–154. doi: 10.4103/2229-516X.212963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tanios C.Y., Abou-Saleh M.T., Karam A.N., Salamoun M.M., Mneimneh Z.N., Karam E.G. The epidemiology of anxiety disorders in the Arab world: a review. J Anxiety Disord. 2009;23:409–419. doi: 10.1016/j.janxdis.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Adriaenssens J., De Gucht V., Van Der Doef M., Maes S. Exploring the burden of emergency care: predictors of stress-health outcomes in emergency nurses. J Adv Nurs. 2011;67:1317–1328. doi: 10.1111/j.1365-2648.2010.05599.x. [DOI] [PubMed] [Google Scholar]
- 23.Koh D., Lim M.K., Chia S.E., Ko S.M., Qian F., Ng V. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore what can we learn? Med Care. 2005;43:676–682. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- 24.Wong T.W., Yau J.K.Y., Chan C.L.W., Kwong R.S.Y., Ho S.M.Y., Lau C.C. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. 2005;12 doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Fiabane E., Giorgi I., Sguazzin C., Argentero P. Work engagement and occupational stress in nurses and other healthcare workers: the role of organisational and personal factors. J Clin Nurs. 2013;22:2614–2624. doi: 10.1111/jocn.12084. [DOI] [PubMed] [Google Scholar]
- 26.Pasay-an E. Exploring the vulnerability of frontline nurses to COVID-19 and its impact on perceived stress. J Taibah Univ Med Sci. 2020 doi: 10.1016/j.jtumed.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao Y.-Q., Pan B.-C., Sun W., Wu H., Wang J.-N., Wang J.-N. Anxiety symptoms among Chinese nurses and the associated factors: a cross sectional study. BMC Psychiatry. 2012;12:141. doi: 10.1186/1471-244X-12-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abbas M.A.F., Zaid L.Z.A., Hussaein M., Bakheet K.H., AlHamdan N.A. Anxiety and depression among nursing staff at King Fahad Medical City, Kingdom of Saudi Arabia. J Am Sci. 2012;8:788–794. [Google Scholar]
- 29.Portela L., Rotenberg L., Waissmann W. Self-reported health and sleep complaints among nursing personnel working under 12 h night and day shifts. Chronobiol Int. 2004;21:859–870. doi: 10.1081/CBI-200038513. [DOI] [PubMed] [Google Scholar]
- 30.Li L., Cheng S., Gu J. SARS infection among health care workers in Beijing, China. JAMA. 2003;290:2662–2663. doi: 10.1001/jama.290.20.2662. [DOI] [PubMed] [Google Scholar]
- 31.Shih F.-J., Gau M.-L., Kao C.-C., Yang C.-Y., Lin Y.-S., Liao Y.-C. Dying and caring on the edge: Taiwan’s surviving nurses’ reflections on taking care of patients with severe acute respiratory syndrome. Appl Nurs Res. 2007;20:171–180. doi: 10.1016/j.apnr.2006.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flint A.J., Peasley-Miklus C., Papademetriou E., Meyers B.S., Mulsant B.H., Rothschild A.J. Effect of age on the frequency of anxiety disorders in major depression with psychotic features. Am J Geriatr Psychiatry. 2010;18:404–412. doi: 10.1097/JGP.0b013e3181c294ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-Onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 34.Wells J.E., Oakley Browne M.A., Scott K.M., McGee M.A., Baxter J., Kokaua J. Prevalence, interference with life and severity of 12 month DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40:845–854. doi: 10.1080/j.1440-1614.2006.01903.x. [DOI] [PubMed] [Google Scholar]
- 35.Schilling O.K., Diehl M. Psychological vulnerability to daily stressors in old age. Z Gerontol Geriatr. 2015;48:517–523. doi: 10.1007/s00391-015-0935-7. [DOI] [PubMed] [Google Scholar]
- 36.Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151:640–649. doi: 10.1176/ajp.151.5.640. [DOI] [PubMed] [Google Scholar]
- 37.Christodoulou N., Christodoulou N.G., Christodoulou G.N. Financial crises: impact on mental health and suggested responses. Psychother Psychosom. 2013;82:279–284. doi: 10.1159/000351268. [DOI] [PubMed] [Google Scholar]