Credit author statement
All authors were involved in the conceptualization of the manuscript. TC and JL led survey design and administration. TC was responsible for the analysis of the data. TC and AM led the initial drafting of the manuscript. All authors provided critical revisions to manuscript drafts adding important intellectual content. All authors approve of the final version of the manuscript and agree to be accountable for all aspects of the work.
1. Introduction
With millions of confirmed coronavirus (COVID-19) cases and hundreds of thousands of deaths, the United States (U.S.) continues to battle the public health crisis arising from the pandemic spread of the SARS-CoV-2 virus (COVID-19 Dashboard, 2020). COVID-19 has emerged as an American health disparity, with racial and ethnic minorities exhibiting the highest burden of illness and deaths in the U.S. due to COVID-19 (Wortham et al., 2020). According to the Centers for Disease Control and Prevention (CDC), Black and Hispanic persons are 4.7 and 4.6 times more likely, respectively, to be hospitalized for COVID-19 compared to Whites (CDC, 2020). The global pandemic has also imposed significant economic and social costs for individuals, institutions, businesses, and communities. Here too, minorities have borne a disproportionally high share of the economic and social cost of the pandemic (CDC, 2020).
A COVID-19 vaccine will be vital to producing an immune response that slows the pandemic. Depending on its efficacy, modeling studies indicate we could need up to 70% of the American population vaccinated against COVID-19 to effectively interrupt virus transmission (Bartsch et al., 2020). Critically, the decision to fast track a COVID-19 vaccine has raised concern among the public that vaccine development is being rushed. Surveys assessing the share of Americans willing to get vaccinated against COVID-19 place estimates of intention to refuse vaccination between 25 and 50% (The Associated Press, 2020). If that proportion of the public opts out of vaccinating, then vaccination rates may be inadequate to produce herd immunity to the virus.
Vaccine hesitancy, “defined as the decision to delay vaccination or the refusal to vaccinate despite available vaccination services,” is growing increasingly common in the U.S. public (Callaghan et al., 2019). It has been observed for vaccination against influenza (Nyhan and Reifler 2015), human papillomavirus (Fowler and Gollust 2015), and pneumococcal vaccines (Glanz et al., 2011; Gatwood et al., 2020). Critically, however, we see intention to vaccinate against COVID-19 as similar but conceptually distinct from traditional vaccine hesitancy. Whereas traditional hesitancy occurs in circumstances where vaccine safety is established and the vaccine is already widely available, that is not yet the case with COVID-19 vaccination.
Improving intention to vaccinate against COVID-19 to slow the pandemic will require targeted health communication strategies that effectively reach the subpopulations most likely to refuse COVID-19 vaccination and that ameliorate the primary concerns of individuals reluctant to vaccinate using scientific evidence (Goldstein et al., 2015). Consequently, an important first step in this process is to identify who in the American public is least likely to pursue an eventual COVID-19 vaccine and their reasons for not pursuing vaccination.
Our efforts to start this process are, necessarily, an exploratory exercise. The uncertain nature of the COVID-19 pandemic, coupled with the unprecedented pace at which vaccines are being developed, makes it difficult to say with certainty whether previous research on the reasons for vaccine refusal may extend to this particular vaccine. Consequently, our work aims to provide a pluralistic overview of the public opinion landscape surrounding COVID-19 vaccination that considers many potential correlates and justifications for intended vaccine refusal.
Of course, while we are open to the possibility that insights from past research may not apply to this particular vaccine, previous work nevertheless does suggest several areas in which we might expect to observe important differences in vaccination intentions. For example, it is critical to examine the possibility of racial differences in COVID-19 vaccine refusal, as previous research suggests that racial minority groups are less likely to be vaccinated against some vaccine-preventable diseases. For example, Black and Hispanic adults are less likely to receive annual influenza vaccinations (CDC 2019; “Immunizations and African Americans,” 2018).
Moreover, concerning this particular vaccine, anti-vaccine advocacy groups have made a concerted effort to target Black Americans with anti-COVID-19 vaccine messaging. Specifically, the Children's Health Defense – a prominent anti-vaccine advocacy group – has suggested that a COVID-19 vaccine could fit in with a pattern of ‘historical lapses in public health ethics’ and has attempted to tie the COVID-19 vaccine with past medical abuses against Blacks in the U.S. (Children’s Health Defense, 2020). These anti-vaccination messages have invoked the Tuskegee Syphilis Study, in which the United States Public Health Service studied untreated syphilis in Black men who were never told about the purpose of the study, were led to believe they were simply receiving free health care from the federal government, and were never provided penicillin to treat the disease (Brandt 1978). To the extent that anti-vaccine advocacy groups are successful in framing COVID-19 vaccination in terms of past medical abuses against minority groups, it could decrease the likelihood that racial minorities will pursue COVID-19 vaccination, particularly in light of recent findings emphasizing the implications of peripheral trauma (Alsan et al., 2020).
Additionally, while past research has presented a mixed pattern of results concerning the possibility that women are less likely than men to vaccinate, we nevertheless recognize that women make 80% of health care decisions for families and are more likely to be deeply concerned about vaccination issues, especially for children (Matoff-Stepp et al., 2014; Pew Research Center, 2017). Given this increased burden for health care decisions and concern about vaccination, women may pay particularly close attention to information concerning the safety and efficacy of a COVID-19 vaccine.
Finally, we think it is important to consider the possibility of partisan asymmetries in vaccination intentions. Prior research suggests that conservatives are less likely to trust medical and scientific experts (e.g., Motta 2018), and – perhaps consequently – are more likely to think that vaccines are unsafe (Joslyn and Sylvester 2019; Baumgaertner et al., 2018). Conservatives are also less likely to believe that the COVID-19 pandemic poses a serious public health threat (Tyson 2020), potentially due to messaging from President Trump suggesting otherwise (Summers 2020), which could undermine the perceived necessity of vaccinating.
2. Methods
2.1. Sample information
To understand who in the American public is most likely to refuse an eventual COVID-19 vaccine and their reasons not to vaccinate, we developed an original survey that was given to a national sample of 5009 Americans from May 28-June 8, 2020. The survey was administered through the Lucid Marketplace survey platform. Lucid Marketplace surveys rely on quota sampling to provide national samples that mirror population benchmarks on a variety of demographic factors such as age, race, gender, education, and income. To account for any remaining deviations between our sample and the US population, we calculated post-stratification weights to Census benchmarks for gender, education, race, age, and income. Table 1 provides additional information about our sample and demographic representativeness.
Table 1.
Comparison of raw and weighted lucid data to national benchmarks.
| Variable | Our Data (Raw) | Our Data (Weighted) | Benchmark | Benchmark Source |
|---|---|---|---|---|
| Female N = 2520 (N valid = 4989) |
50.5% | 51.5% | 51% | CPS 2018 |
| College degree N = 2286 (N valid = 4992) |
45.79% | 34.34% | 31% | CPS 2018 |
| Hispanic N = 1182 (N valid = 5001) |
23.6% | 19.1% | 18% | CPS 2018 |
| Black (Non-Hispanic) N = 522 (N valid = 4997) |
10.4% | 13.4% | 13% | CPS 2018 |
| White (Non-Hispanic) N = 2964 (N valid = 4997) |
59.3% | 60.0% | 62% | CPS 2018 |
| Mean age in years (N valid = 4953) | 44.5 | 45.9 | 47 | ANES 2016 |
| Median income (N valid = 4960) | $50k-74,999 | $50k-74,999 | $55k-59,999 | ANES 2016 |
Note. This table compares variables from our study's raw and weighted data to known population benchmarks. The CPS is the Current Population Survey from the US Census. The ANES is the American National Election Study. N valid presents the total number of non-missing observations on each variable.
2.2. Outcome measures
All survey respondents were asked a series of questions about their behaviors and attitudes related to COVID-19. Our primary outcome variable is a vaccination intention indicator. We asked respondents: “If a [COVID-19] vaccine is developed, would you pursue getting vaccinated for the coronavirus?” Based on responses to this question, our primary outcome variable takes on a value of 1 if respondents intend to refuse vaccination (“no”) and 0 if they intend to vaccinate (“yes”).
We also investigated the reasons why individuals did not intend to pursue COVID-19 vaccination. All respondents who answered that they did not intend to pursue getting vaccinated against COVID-19 were presented with a follow-up multi-answer question asking whether they were refusing because they thought the vaccine would not be safe, not be effective, because they lacked health insurance, lacked financial resources, and/or because they already had COVID-19. We used this information to create dichotomous indicators of whether or not respondents (1) intended not to vaccinate for a particular reason, or (0) indicated intention to pursue vaccination. Individuals who intended not to vaccinate for a different reason were coded as missing.
2.3. Explanatory measures
Based on insights from previous research, we include a measure for gender – a dichotomous variable with female coded as 1 – as well as dichotomous indicators of whether respondents self-identify as Black or Hispanic in our models. We also include two measures of political sentiments: a 7-point ideology measure ranging from extremely liberal to extremely conservative and a dichotomous indicator coded as 1 if the respondent intended to vote for President Trump in 2020, and 0 otherwise.
We also control for several other demographic factors that could influence intention to vaccinate against COVID-19. Specifically, we include measures for age (intervalized) and its square, a 7-point educational level measure, income (a 12-point scale capturing household income), and a 5-point measure capturing respondents' levels of religiosity. We also include several measures of respondents’ general attitudes towards experts and vaccination. In particular, we include a 5-point measure capturing respondents' trust in experts and three items to capture general sentiments towards vaccination (vaccines are safe, effective, and important).
Finally, our analyses include responses to questions related to experiences with COVID-19 that could impact attitudes towards vaccination. One item captures whether each respondent has been tested for COVID-19, a second asked respondents how often they worry about getting infected, and the third assesses perceived risk of getting COVID-19 compared to others, with 7 options ranging from much lower to much higher risk.
Across covariates included in our analysis, missing data levels never exceed 3.5%. Further, missingness on the vaccination intention outcome variable is below 1%. Consequently, we elected not to use any imputation strategies to adjust for missing data. Given the dichotomous nature of our dependent variables (intention to vaccinate or not and reason for refusal or not), our analysis relies on binary logistic regression. All analyses were performed using Stata 15 statistical software.
3. Results
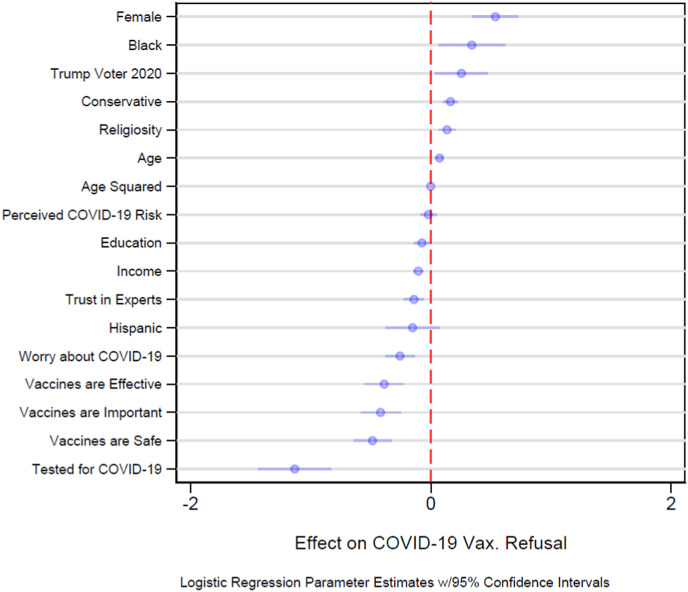
We began our analysis by assessing the prevalence of intention to not pursue COVID-19 vaccination in our sample. Our results suggest that as of our period of analysis from May 28-June 8, 2020, 31.13% of Americans (30.85% unweighted) did not intend to pursue vaccination against COVID-19 when a vaccine becomes available. Of course, it is critical to ask which Americans are most likely to refuse to vaccinate when a vaccine becomes available. We assess that question in Fig. 1 , where we present the results of a logistic regression, regressing vaccine refusal on our explanatory measures. Point estimates to the right of the vertical dashed line without 95% confidence intervals touching the dashed line indicate increased odds of vaccine refusal, while point estimates to the left of the dashed line indicate decreased odds.
Fig. 1.
Predictors of Intention not to Pursue a COVID-19 Vaccine. Note. Shown are results of a binary logistic regression where the dependent variable was coded such that 1 indicated intent not to pursue a COVID-19 vaccine and 0 indicated intent to pursue vaccination. Logistic regression coefficient estimates (circles) to the right of the dashed red line indicate increased intent to refuse and point estimates to the left of the line indicate decreased intent. Lines extending from point estimates indicate 95% confidence intervals. Point estimates where the 95% confidence intervals do not touch the dashed red line are statistically significant at the p < 0.05 level, two-tailed. Robustness tests analyzing the possibility of differences across Census regions and interaction effects between race and gender found no statistically significant effects. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Our results in Fig. 1 demonstrate that the odds of COVID-19 vaccine refusal are significantly higher for Blacks, women, conservatives, individuals who intended to vote for President Trump in 2020, and individuals with high levels of religiosity. The largest positive effect we find is for women – who are 71% more likely not to pursue vaccination, indicating that efforts to improve vaccination intentions in this group should be a top priority. The second largest positive effect we find is for Blacks, who are 41% more likely not to pursue vaccination. Politics also appears to be playing an important role in vaccine refusal. Each 1-point increase in conservatism increases the odds of vaccine refusal by 18% and individuals who intended to vote for President Trump in 2020 vs. making any other political choice, are 29% more likely to refuse COVID-19 vaccination.
Our results also identify several factors underlying why some individuals are more willing to vaccinate against COVID-19. A one-unit increase in worry about COVID-19 is associated with a 23% decrease in intention to refuse and individuals who have been tested for COVID-19 are 68% less likely to refuse vaccination. Additionally, individuals who view vaccines as safe, effective, and/or important are all less likely to oppose COVID-19 vaccination. Finally, we find that wealthier Americans and individuals who trust experts over ordinary people are more likely to pursue COVID-19 vaccination.
While understanding general predispositions towards COVID-19 vaccination is valuable, it is just as important to ask why individuals may be reluctant to vaccinate. We explore that question in Table 2 , which presents reasons for intention not to pursue COVID-19 vaccination in the U.S. population. There, we find that the two most common reasons individuals intend not to pursue COVID-19 vaccination are because they do not think the vaccine will be safe (17.83%) or effective (15.55%). Other reasons for refusal intention are less common but non-trivial: 6.22% are planning to forgo vaccination due to a lack of insurance, 6.17% because they lack financial resources to be vaccinated, 3.31% because they believe they already contracted COVID-19, and 7.41% for other reasons.
Table 2.
Reasons for hesitancy to pursue a COVID-19 vaccine by proportion of the United States population.
| Reason for Refusal | Overall Percentage | White vs. Black | Male vs. Female |
|---|---|---|---|
| Vaccine Won't be Safe | 17.83% (16.67, 18.99) | 16.79% vs. 25.82% (15.50, 18.08 vs. 22.03, 29.61) −9.03** |
13.22% vs. 22.35% (11.76, 14.69 vs. 20.56, 24.15) −9.13** |
| Vaccine Won't be Effective | 15.55% (14.44, 16.67) | 13.49% vs. 24.35% (12.29, 14.69 vs. 20.57, 28.13) −10.86** |
11.45% vs. 19.46% (10.06, 12.84 vs. 17.73, 21.20) −8.01** |
| Lack of Insurance | 6.22% (5.44, 7.00) | 5.08% vs. 12.89% (4.27, 5.88 vs. 9.70, 16.09) −7.81** |
6.50% vs. 5.71% (5.40, 7.61 vs. 4.62, 6.80) +0.79 |
| Lack of Financial Resources | 6.17% (5.40, 6.95) | 5.27% vs. 9.14% (4.45, 6.09 vs. 6.36, 11.92) −3.87* |
6.10% vs. 5.86% (5.02, 7.17 vs. 4.76, 6.96) +0.24 |
| Already had COVID-19 | 3.31% (2.72, 3.90) | 3.14% vs. 4.84% (2.49, 3.78 vs. 2.72, 6.96) −1.70 |
3.89% vs. 2.79% (3.01, 4.77 vs. 2.00, 3.57) +1.10 |
| Other Reasons | 7.41% (6.56, 8.25) | 7.21% vs. 9.47% (6.27, 8.15 vs. 6.64, 12.29) −2.26 |
4.93% vs. 9.75% (3.95, 5.91 vs. 8.38, 11.12) −4.82** |
Note. Percentages indicate the percentage of respondents who intend to forgo COVID-19 vaccination for each reason. Quantities in parentheses indicate 95% confidence intervals.
Quantities in parentheses indicate 95% confidence intervals. Significance determined using lincom command and survey weights in Stata. **p < 0.01, *p < 0.05.
Critically, Table 2 also investigates reasons for refusal among the two groups most likely to refuse – women and Blacks. We find that women are more likely than men to not pursue vaccination because they do not believe the vaccine will be safe or that the vaccine will be effective. When analyzing differences across race, we find that Blacks are more likely than Whites to not pursue vaccination for every reason included in our survey, with statistically significant differences for concerns about safety, effectiveness, lack of insurance, and lack of financial resources.
We assess the robustness of these bivariate comparisons using logistic regression in Table 3 , assessing each reason for refusal against our complete set of explanatory measures. In these fully specified models, we again see that women remain more likely to not pursue vaccination because they do not think that the vaccine will be safe or effective. Notably, however, we find in fully specified models that Blacks are more likely to refuse only because they do not think the vaccine will be safe or effective.
Table 3.
Correlates of reasons individuals give for not pursuing a COVID-19 vaccine.
| VARIABLES | (Model 1) |
(Model 2) |
(Model 3) |
(Model 4) |
(Model 5) |
|---|---|---|---|---|---|
| Not Safe | Not Effective | No Insurance | No Financial Resources | Had COVID | |
| Female | 2.04** | 1.97** | 1.05 | 1.11 | 1.14 |
| (1.58, 2.63) | (1.50, 2.58) | (0.70, 1.58) | (0.73, 1.67) | (0.73, 1.78) | |
| Education | 0.91* | 0.93 | 0.91 | 0.95 | 1.09 |
| (0.83, 0.99) | (0.84, 1.02) | (0.79, 1.05) | (0.82, 1.10) | (0.93, 1.28) | |
| Age | 1.10** | 1.08** | 1.12* | 1.04 | 1.07 |
| (1.05, 1.14) | (1.03, 1.13) | (1.02, 1.22) | (0.97, 1.12) | (0.98, 1.16) | |
| Age Squared | 1.00** | 1.00** | 1.00** | 1.00* | 1.00* |
| (1.00, 1.00) | (1.00, 1.00) | (1.00, 1.00) | (1.00, 1.00) | (1.00, 1.00) | |
| Black | 1.46* | 1.79** | 1.54 | 0.98 | 1.41 |
| (1.01, 2.09) | (1.23, 2.62) | (0.93, 2.57) | (0.57, 1.68) | (0.77, 2.59) | |
| Hispanic | 0.99 | 1.07 | 0.99 | 0.86 | 0.79 |
| (0.74, 1.33) | (0.77, 1.47) | (0.62, 1.56) | (0.56, 1.31) | (0.44, 1.43) | |
| Income | 0.90** | 0.89** | 0.92* | 0.94 | 0.94 |
| (0.85, 0.95) | (0.84, 0.94) | (0.84, 1.00) | (0.87, 1.02) | (0.86, 1.04) | |
| Conservative | 1.23** | 1.22** | 1.15* | 1.09 | 1.04 |
| (1.13, 1.34) | (1.11, 1.33) | (1.03, 1.29) | (0.98, 1.22) | (0.91, 1.18) | |
| Religiosity | 1.11* | 1.04 | 1.15 | 1.10 | 1.02 |
| (1.00, 1.22) | (0.93, 1.15) | (0.98, 1.34) | (0.94, 1.29) | (0.84, 1.23) | |
| Trust in Experts | 0.94 | 0.87* | 0.87 | 0.89 | 0.83 |
| (0.84, 1.05) | (0.77, 0.97) | (0.72, 1.05) | (0.77, 1.03) | (0.67, 1.02) | |
| Vaccines Import. | 0.71** | 0.66** | 0.57** | 0.73* | 0.63* |
| (0.57, 0.87) | (0.53, 0.83) | (0.43, 0.77) | (0.55,0.97) | (0.43, 0.92) | |
| Vaccines Safe | 0.55** | 0.59** | 0.58** | 0.71* | 0.81 |
| (0.46, 0.67) | (0.48, 0.73) | (0.43, 0.78) | (0.54, 0.94) | (0.55, 1.19) | |
| Vaccines Effective | 0.61** | 0.65** | 0.90 | 0.56** | 0.86 |
| (0.50, 0.75) | (0.52, 0.81) | (0.66, 1.22) | (0.40, 0.78) | (0.61, 1.22) | |
| Tested for COVID | 0.36** | 0.24** | 0.60 | 0.30** | 0.91 |
| (0.24, 0.55) | (0.14, 0.40) | (0.34, 1.05) | (0.16, 0.57) | (0.52, 1.59) | |
| Trump Vote 2020 | 1.16 | 1.29 | 0.81 | 0.98 | 1.39 |
| (0.86, 1.56) | (0.94, 1.77) | (0.51, 1.30) | (0.62, 1.53) | (0.85, 2.26) | |
| Perceived Risk | 0.93 | 0.95 | 1.07 | 1.03 | 1.11 |
| (0.85, 1.02) | (0.87, 1.05) | (0.94, 1.22) | (0.92, 1.16) | (0.91, 1.35) | |
| COVID Worry | 0.78** | 0.67** | 1.10 | 1.09 | 1.00 |
| (0.66, 0.91) | (0.56, 0.79) | (0.87, 1.40) | (0.86, 1.40) | (0.69, 1.44) | |
| Constant | 6.29** | 14.48** | 0.58 | 4.45 | 0.34 |
| (1.91, 20.75) | (3.96, 52.89) | (0.09, 3.96) | (0.83, 24.00) | (0.05, 2.33) | |
| Observations | 3877 | 3760 | 3390 | 3402 | 3305 |
| Log Pseudolike. | −1313.71 | −1141.79 | −552.83 | −576.73 | −386.15 |
| Pseudo R2 | 0.27 | 0.28 | 0.19 | 0.19 | 0.12 |
Note. All models present coefficients as odds ratios with 95% confidence intervals in parentheses. Models were estimated using logit models given the binary nature of the dependent variables. Here, dependent variables are coded as 1's if a respondent indicates the intent to refuse for a particular reason and 0's if the respondent intends to vaccinate. **p < 0.01, *p < 0.05.
Several other interesting patterns emerge when studying reasons for vaccine refusal in Table 3. We find that conservatism is a consistent positive and significant predictor of refusal intention. A one-unit increase in conservatism is associated with a 23% increase in refusal due to safety concerns, a 22% increase in refusal due to effectiveness concerns, and a 15% increase in refusal due to lack of insurance.
In contrast, we find that several factors reduce the likelihood of refusing vaccination. We find that wealthier Americans, those who have been tested for COVID-19, those who are more worried about the virus, and those who see vaccines as safe, effective, and/or important are all less likely to refuse COVID-19 vaccination because they think the vaccine will be unsafe. These same predictors are also significant in the same directions for thinking the vaccine will be ineffective in Model 2.
Finally, when examining refusal due to a lack of insurance or financial resources, we find those who view vaccines as safe or important are less likely to refuse for either reason, and that wealthier individuals are less likely to refuse vaccination because they lack insurance.
4. Discussion
Large proportions of the American public intend to forgo vaccination against COVID-19 once a vaccine becomes available, reducing the chances that an effective vaccine will be a panacea that induces immunity and ends the pandemic. More troublesome, vaccination intentions reflect existing inequalities in COVID-19 infection and mortality. In particular, Black Americans who are being infected and dying at higher rates than the rest of the population are also less likely to vaccinate because of a combination of concerns that the vaccine will not be safe, or effective, and because they lack the health insurance and financial resources that might be necessary for access to vaccination. These reasons could exacerbate existing health inequalities once vaccination begins.
Taken together, while our findings present an alarming challenge for the future of combating COVID-19, they also present an opportunity to counteract refusal. Our findings offer a first step towards developing effective health communications to reduce COVID-19 vaccine refusal. By identifying those most likely to refuse vaccination, public health experts can develop health messages targeted at encouraging vaccination among these groups. This approach could prove vital to improving uptake of a COVID-19 vaccine (e.g., see Lunz-Trujillo et al., 2020).
4.1. Limitations
This study has several limitations that are worth noting. First, due to the cross-sectional nature of our data, we are only able to provide a snapshot of vaccination intentions at a single moment in time, which we see as an important confound in our study. As such, we cannot account for how attitudes towards a vaccine may evolve in response to circumstantial changes (e.g., COVID-19 spread; political rhetoric about vaccine safety). Relatedly, it is worthwhile to acknowledge that as the COVID-19 vaccine was not yet released at the time of our survey, the public did not have full information about its safety, effectiveness, or cost. As such, estimates of vaccination intentions and reasons for refusal could change once relevant data becomes available.
Furthermore, our analysis is an effort to explain vaccine hesitancy about a particular vaccine. Given the unprecedented nature of the COVID-19 pandemic, we cannot say with certainty whether these results generalize to other forms of vaccination. Future efforts to study the effects of past childhood vaccination and influenza vaccination on COVID-19 refusal could help shed light on this question. Finally, it is important to recognize that while the data-collection platform Lucid is being used with increasing frequency in social science research, it is nevertheless an internet-based survey platform. Participation requires participants to have an internet connection, which could limit the representativeness of the opt-in online sampling frame.
5. Conclusions
Almost a third of U.S. adults intend to not pursue a COVID-19 vaccine once one becomes available, driven by concerns about safety, effectiveness, and a lack of resources. These intentions are especially prevalent among women, conservatives, and Blacks. Developing effective health communication strategies targeted at these populations could reduce vaccine refusal and help end the pandemic.
Declaration of competing interest
PH and US are developing vaccines against neglected and emerging infectious diseases, including COVID-19.
Funding
This research was funded by the Texas A&M Triads for Transformation grant program. The grant was received by TC and JL. The funder had no role in study design, data collection, data analysis, or the writing of this manuscript.
Author contributions
All authors were involved in the conceptualization of the manuscript. TC and JL led survey design and administration. TC was responsible for the analysis of the data. TC and AM led the initial drafting of the manuscript. All authors provided critical revisions to manuscript drafts adding important intellectual content. All authors approve of the final version of the manuscript and agree to be accountable for all aspects of the work.
Institutional review board
This research was approved by the institutional review board at Texas A&M University.
References
- Alsan M., Wanamaker M., Hardeman R.R. The Tuskegee study of untreated syphilis: a case study in peripheral trauma with implications for health professionals. J. Gen. Intern. Med. 2020;35(1):322–325. doi: 10.1007/s11606-019-05309-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Associated Press Half of Americans would get a COVID-19 vaccine, AP-NORC poll finds. NBC News. 2020;May 27:2020. [Google Scholar]
- Bartsch S.M., O'Shea K.J., Ferguson M.C., Bottazzi M.E., Wedlock P.T., Strych U., McKinnell J.A., Siegmund S.S., Cox S.N., Hotez P.J., Lee B.Y. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am J Prev Med. 2020 Oct. 2020;59(4):493–503. doi: 10.1016/j.amepre.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgaertner B., Carlisle J.E., Justwan F. The influence of political ideology and trust on willingness to vaccinate. PloS One. 2018;13(1) doi: 10.1371/journal.pone.0191728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt A.M. Hastings center report; 1978. Racism and Research: the Case of the Tuskegee Syphilis Study; pp. 21–29. [PubMed] [Google Scholar]
- Callaghan T., Motta M., Sylvester S., Trujillo K.L., Blackburn C.C. Parent psychology and the decision to delay childhood vaccination. Soc. Sci. Med. 2019;238:112407. doi: 10.1016/j.socscimed.2019.112407. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention “COVIDView: a weekly surveillance summary of U.S. COVID-19 activity.” 2020. Centers for disease control and prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
- Centers for Disease Control and Prevention . September vols. 26, 2019. 2019. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm (Flu Vaccination Coverage, United States, 2018-19 Influenza Season). [Google Scholar]
- Children’s Health Defense Historical lapses in public health ethics: will gates-funded COVID vaccine human trials Be business as usual?” Children's health Defense. June. 2020;18:2020. https://childrenshealthdefense.org/news/public-health-and-medical-ethics-learning-from-history/ [Google Scholar]
- COVID-19 Dashboard . Johns Hopkins University; 2020. Center for Systems Science and Engineering.https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 [Google Scholar]
- Fowler E.F., Gollust S.E. The content and effect of politicized health controversies. Ann. Am. Acad. Polit. Soc. Sci. 2015;658(1):155–171. [Google Scholar]
- Gatwood J., Shuvo S., Hohmeier K.C., Hagemann T., Chiu C.Y., Tong R., Ramachandran S. Pneumococcal vaccination in older adults: an initial analysis of social determinants of health and vaccine uptake. Vaccine. 2020;38(35):5607–5617. doi: 10.1016/j.vaccine.2020.06.077. [DOI] [PubMed] [Google Scholar]
- Glanz J.M., McClure D.L., O'Leary S.T., Narwaney K.J., Magid D.J., Daley M.F., Hambidge S.J. Parental decline of pneumococcal vaccination and risk of pneumococcal related disease in children. Vaccine. 2011;29(5):994–999. doi: 10.1016/j.vaccine.2010.11.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein S., MacDonald N.E., Guirguis S. Health communication and vaccine hesitancy. Vaccine. 2015;33(34):4212–4214. doi: 10.1016/j.vaccine.2015.04.042. [DOI] [PubMed] [Google Scholar]
- Joslyn M.R., Sylvester S.M. The determinants and consequences of accurate beliefs about childhood vaccinations. Am. Polit. Res. 2019;47(3):628–649. [Google Scholar]
- Lunz Trujillo K., Motta M., Callaghan T., Sylvester S. Correcting misperceptions about the MMR vaccine: using psychological risk factors to inform targeted communication strategies. Polit. Res. Q. 2020 1065912920907695. [Google Scholar]
- Matoff-Stepp S., Applebaum B., Pooler J., Kavanagh E. Women as health care decision-makers: implications for health care coverage in the United States. J. Health Care Poor Underserved. 2014;25(4):1507–1513. doi: 10.1353/hpu.2014.0154. [DOI] [PubMed] [Google Scholar]
- Motta M. The dynamics and political implications of anti-intellectualism in the United States. Am. Polit. Res. 2018;46(3):465–498. [Google Scholar]
- Nyhan B., Reifler J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine. 2015;33(3):459–464. doi: 10.1016/j.vaccine.2014.11.017. [DOI] [PubMed] [Google Scholar]
- Summers J. NPR; 2020. Timeline: How Trump Has Downplayed the Coronavirus Pandemic.https://www.npr.org/sections/latest-updates-trump-covid-19-results/2020/10/02/919432383/how-trump-has-downplayed-the-coronavirus-pandemic [Google Scholar]
- Tyson A. Pew Research Center; 2020. Republicans Remain Far Less Likely than Democrats to View COVID-19 as a Major Threat to Public Health.https://www.pewresearch.org/fact-tank/2020/07/22/republicans-remain-far-less-likely-than-democrats-to-view-covid-19-as-a-major-threat-to-public-health/ [Google Scholar]
- Wortham Jonathan, et al. vol. 69. Early release on July 10, 2020; 2020. Characteristics of persons who died with COVID-19 — United States, february 12–may 18, 2020.” Centers for disease control and prevention. (Morbidity and Mortality Weekly Report). [DOI] [PubMed] [Google Scholar]