Abstract
Objective
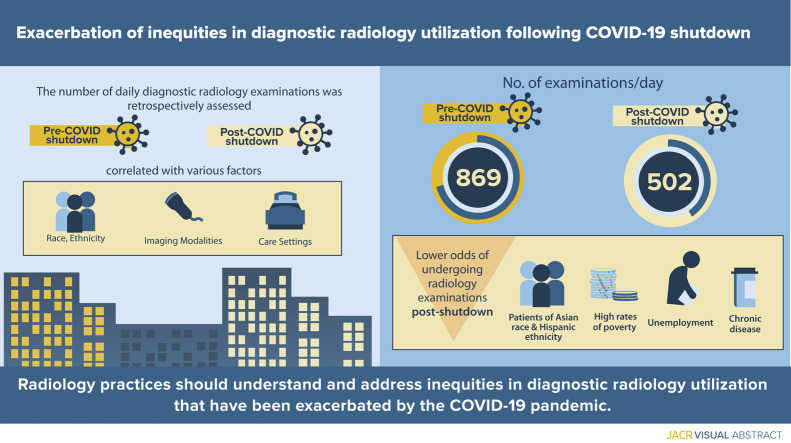
Assess diagnostic radiology examination utilization and associated social determinants of health during the early stages of reopening after state-mandated shutdown of nonurgent services because of coronavirus disease 2019 (COVID-19).
Methods
This institutional review board–approved, retrospective study assessed all patients with diagnostic radiology examinations performed at an academic medical center with eight affiliated outpatient facilities before (January 1, 2020, to March 8, 2020) and after (June 7, 2020, to July 15, 2020) the COVID-19 shutdown. Examinations during the shut down (March 9, 2020, to June 6, 2020) were excluded. Patient-specific factors (eg, race, ethnicity), imaging modalities, and care settings were extracted from the Research Data Warehouse. Primary outcome was the number of diagnostic radiology examinations per day compared pre- and post-COVID-19 shutdown. Univariate analysis and multivariable logistic regression determined features associated with completing an examination.
Results
Despite resumption of nonurgent services, marked decrease in radiology examination utilization persisted in all care settings post-COVID-19 shutdown (869 examinations per day preshutdown [59,080 examinations in 68 days] versus 502 examinations per day postshutdown [19,594 examinations in 39 days]), with more significantly decreased odds ratios for having examinations in inpatient and outpatient settings versus in the emergency department. Inequities worsened, with patients from communities with high rates of poverty, unemployment, and chronic disease having significantly lower odds of undergoing radiology examinations post-COVID-19 shutdown. Patients of Asian race and Hispanic ethnicity had significantly lower odds ratios for having examinations post-COVID-19 shutdown compared with White and non-Hispanic patients, respectively.
Discussion
The COVID-19 pandemic has exacerbated known pre-existing inequities in diagnostic radiology utilization. Resources should be allocated to address subgroups of patients who may be less likely to receive necessary diagnostic radiology examinations, potentially leading to compromised patient safety and quality of care.
Key Words: Diagnostic imaging, health care disparities, health care utilization, social determinants of health
Visual Abstract
Credits awarded for this enduring activity are designated “SA-CME” by the American Board of Radiology (ABR) and qualify toward fulfilling requirements for Maintenance of Certification (MOC) Part II: Lifelong Learning and Self-assessment. To access the SA-CME activity visit https://cortex.acr.org/Presenters/CaseScript/CaseView?Info=nStKx24vrpLs8oANZ9bFrcH%2fzE8Ycm1Qb1fDkW3r2IE%253d. SA-CME credit for this article expires May 2, 2024.
Introduction
Significant decreases in diagnostic radiology utilization were reported during the early stages of the coronavirus disease 2019 (COVID-19) pandemic [1, 2, 3, 4]. Reasons for reduced imaging volumes were likely multifactorial but include patient concern regarding risks of leaving home, patient unwillingness to come to hospitals and clinics for fear of acquiring the virus [2,5], and governmental policies mandating cessation of nonurgent testing and procedures. In some cases, this resulted in delayed management of non-COVID-19-related diseases [6,7]. Because patients are missing or deferring management for non-COVID-19 conditions [8], major concern has risen for further risk of compromised patient care and safety because of delays in diagnosis even after resumption of nonurgent care.
The COVID-19 pandemic is also highlighting deep pre-existing inequities in health care delivery in the United States [9], including in radiology [10,11]. Social determinants of health such as race, ethnicity, and socioeconomic status are known to affect screening and follow-up for conditions such as breast cancer and lung cancer [12,13] and have been associated with delayed disease presentations in some vulnerable groups [14,15]. Some clinical specialties have begun to identify additional potential deleterious effects of delayed care for patients of low socioeconomic status, from racial and ethnic minority groups, patients with limited English proficiency, and the uninsured [16]. These populations already faced difficulty accessing care prepandemic and were more likely to present with advanced-stage disease.
Although social determinants of health were identified as factors that influence diagnostic radiology examination utilization prepandemic [13,15], this has not been explicitly addressed in the early stages of the COVID-19 pandemic [17]. Therefore, the purpose of this study was to assess diagnostic radiology examination utilization and associated social determinants of health during early stages of reopening after state-mandated shutdown of nonurgent services because of COVID-19.
Methods
Setting and Population
This HIPAA-compliant study was approved by the institutional review board with a waiver of the requirement for informed consent. We performed a retrospective cohort study at an urban academic quaternary care hospital in Boston, Massachusetts, with a level I emergency department (ED) and eight freestanding outpatient practices within 50 miles of the main hospital. Before COVID-19, the study institution typically performed >600,000 imaging studies per year.
Between March 9, 2020, and June 6, 2020, all nonurgent health care services were deferred per statewide COVID-19 mandate. Therefore, the sampling frame for this study included all adult patients who completed a diagnostic radiology examination between January 1, 2020, and March 8, 2020, or between June 7, 2020, and July 15, 2020 (post-COVID-19 shutdown). Examinations during the shut down (March 9, 2020, to June 6, 2020) were excluded from the analysis.
Initial Cohort Identification
All radiology reports and imaging examinations for patients in the sampling time frames were identified and retrieved from the institutional research data repository populated by the electronic health record (Epic Systems Corporation, Madison, Wisconsin). The institutional research data repository is updated daily and includes patient data, such as encounter detail, demographic detail, laboratory tests, radiology tests, providers, clinical textual notes, ambulatory notes, and clinical reports from Epic. After registration, faculty members at the academic institution are granted access to detailed medical record information on identified patient populations with an approved institutional review board protocol. Corresponding patient features were extracted from the repository, including age, sex, race, ethnicity, marital status, health insurance, and zip code. Lastly, we extracted the patient care setting (inpatient, outpatient, or ED) and imaging modality (CT scan, dual energy x-ray absorptiometry, mammography, MRI, ultrasound, and x-ray). Zip codes were used to identify patients coming from priority populations in our community [18], areas with persistent racial and ethnic inequities in health care [19]. The priority populations in our community were identified previously by a hospital-sponsored community health needs assessment based on disproportionate burden of poverty, housing instability, and other social determinants of health, along with citywide health equity studies. The age and sex distribution of priority populations is similar to that of Boston overall, but they are more racially and ethnically diverse. They have a larger Black population and a larger percentage of residents who are Hispanic or Latino. A significantly higher proportion are foreign born and speak a language other than English, primarily Spanish. Residents in the priority communities have significantly lower income, greater unemployment rates, and below-college educational levels. These zip codes included Dorchester (02121-02122, 02124-02125), Jamaica Plain (02130), Mattapan (02136), Mission Hill (02120), and Roxbury (02119-02120).
Outcome Measures
The primary outcome measure was the mean number of diagnostic radiology examinations per day post-COVID-19 shutdown and the proportion of post-COVID-19 shutdown examinations compared with pre-COVID-19 shutdown. We also assessed factors that may be associated with completing a diagnostic radiology examination post-COVID-19 shutdown, including social determinants of health (eg, race, ethnicity, health insurance, coming from priority population), care setting, and imaging modality. We assessed ethnicity as a binary category (Hispanic or not) based on patient-stated ethnicity in our institution’s data repository. We assessed a patient’s coming from a priority population as a binary category (yes or no) based on patient-reported zip code as matching those that were previously identified. We assessed age in increments of 10 years, as well as based on the Centers for Disease Control Hospitalization and Death Risk by Age categories (ie, 18-29 years, 30-39 years, 40-49 years, 50-64 years, 65-74 years, 75-84 years, 85+ years) [20]. Secondarily, we assessed factors that may be associated with completing a diagnostic radiology examination post-COVID-19 shutdown in the outpatient setting alone. Compared with the ED and inpatient settings, outpatient examinations are expected to be less urgent and do not require hospitalization.
Statistical Analysis
The mean frequency of diagnostic radiology examinations per day pre-COVID-19 shutdown was calculated as the total number of diagnostic radiology examinations for unique patients between January 1 and March 8, divided by the 68 calendar days in the interval. Similarly, the mean diagnostic radiology examinations per day was calculated post-COVID-19 shutdown counting all examinations between June 7 and July 15 and divided by 39 calendar days. Calendar days were counted uniformly without regard for weekdays or weekends. Frequency and percentage of each variable potentially associated with diagnostic radiology examination completion was reported and mean frequency was compared using t test. χ2 analysis was performed, comparing all binary patient variables (ie, sex, ethnicity, and coming from priority communities). Logistic regression was used to assess nominal variables (ie, age and race categories, insurance, marital status, imaging modality, and care setting) during the post-COVID-19 shutdown period compared with pre-COVID-19 shutdown. Multivariable logistic regression was then used to assess patient characteristics (ie, sex, ethnicity, coming from priority communities, age, race, insurance, marital status), imaging modality, and care setting (ie, independent variables) for all variables, with P < .25, assessing those who had diagnostic examinations post-COVID-19 shutdown (ie, dependent variable). This cutoff is traditionally used in purposeful variable selection for logistic regression [21]. The reference category for nominal variables was selected based on the largest category for all nominal variables, except for care setting. ED was chosen as the reference category because it was anticipated that diagnostic imaging utilization at the ED would not decrease post-COVID-19 shutdown. In the multivariable model, P < .05 was considered statistically significant. All analyses were performed for diagnostic radiology examinations in all care settings and secondarily for examinations performed only in outpatient sites. All statistical analyses were conducted using R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study Cohort
After exclusion of duplicate or multiple examinations belonging to the same patient, 78,674 distinct patients with diagnostic radiology examinations were included in the study; 59,080 of the examinations were pre-COVID-19 shutdown. Mean patient age was 56 years pre- and post-COVID-19 shutdown.
Diagnostic Radiology Examinations per Day
Marked decrease in radiology examination utilization persisted in all care settings post-COVID-19 shutdown with 19,594 examinations in 39 days post-COVID-19 shutdown (mean of 502 examinations per day, 95% confidence interval [CI] = 415-590]) compared with 59,080 examinations in 68 days pre-COVID-19 shutdown (mean of 869 examinations per day, 95% CI = 747-991). The mean number of examinations post-COVID-19 shutdown represents a proportion of 0.58 of the mean number of examinations pre-COVID-19 shutdown despite the reopening (P < .001). When looking at outpatient sites only, a decrease in radiology examination utilization persisted post-COVID-19 shutdown with 16,946 examinations in 39 days (mean of 435 examinations per day postshutdown, 95% CI = 350-519) compared with 50,194 examinations in 68 days pre-COVID-19 shutdown (mean of 738 examinations per day, 95% CI = 621-856), a proportion of 0.59 of total examinations per day (P < .001).
Univariate Analysis
On univariate analysis (Table 1 ), Asian and Black race and Hispanic ethnicity were associated with a smaller proportion of imaging examinations post-COVID-19 shutdown (P < .01). Also, patients from priority communities had significantly smaller proportion of imaging examinations post-COVID-19 shutdown versus pre-COVID-19 shutdown (6.4% versus 1.8%; P < .0001). Finally, age assessed as a continuous variable was significantly associated with increased diagnostic radiology examination utilization post-COVID-19 shutdown for each 10-year increase in age. The mean age for patients pre-COVID-19 shutdown was 56.0 (95% CI 55.9-56.1, standard error = 0.07), and post-COVID-19 shutdown was 56.4 (95% CI = 56.2-56.6, standard error = 0.12). On further analysis, grouping patients based on Centers for Disease Control age risk, patients in the 30- to 39-year age group were associated with a smaller proportion of imaging examinations post-COVID-19 shutdown (11.7% pre- versus 10.2% postshutdown, P = .0002).
Table 1.
Univariate comparison between patients undergoing diagnostic radiology examinations pre- and post-COVID-19 shutdown
| Variable | All Care Settings (n = 78,674), n (%) |
Outpatient Only (n = 67,140), n (%) |
||||
|---|---|---|---|---|---|---|
| Pre (n = 59,080) | Post (n = 19,594) | P Value | Pre (n = 50,194) | Post (n = 16,946) | P Value | |
| Age (y) | ||||||
| Mean | 56 | 56 | 57 | 57 | ||
| 18-29 | 5,232 (8.9) | 1,749 (8.9) | Reference | 3,673 (7.3) | 1,207 (7.1) | Reference |
| 30-39 | 6,898 (11.7) | 2,006 (10.2) | .0002∗ | 5,654 (11.3) | 1,629 (9.6) | .002∗ |
| 40-49 | 7,643 (12.9) | 2,467 (12.6) | .33 | 6,609 (13.2) | 2,167 (12.8) | .96 |
| 50-64 | 17,808 (30.1) | 6,092 (31.1) | .46 | 15,668 (31.2) | 5,444 (32.1) | .13 |
| 65-74 | 12,925 (21.9) | 4,370 (22.3) | .73 | 11,470 (22.8) | 4,002 (23.6) | .11 |
| 75-84 | 6,649 (11.3) | 2,311 (11.8) | .29 | 5,714 (11.4) | 2,054 (12.1) | .03∗ |
| 85+ | 1,925 (3.3) | 599 (3.1) | .19 | 1,406 (2.8) | 443 (2.6) | .51 |
| Male | 19,509 (33.0) | 6,276 (32.0) | .01∗ | 15,781 (31.4) | 5,045 (29.8) | <.0001∗ |
| Race | ||||||
| White | 44,187 (74.8) | 14,909 (76.1) | Reference | 38,562 (76.8) | 13,340 (78.7) | Reference |
| Black | 4,631 (7.8) | 1,294 (6.6) | <.0001∗ | 3,302 (6.6) | 886 (5.2) | <.0001∗ |
| Asian | 2,222 (3.8) | 667 (3.4) | <.01∗ | 1,971 (3.9) | 580 (3.4) | <.0001∗ |
| Other | 8,040 (13.6) | 2,724 (13.9) | .86 | 6,359 (12.7) | 2,140 (12.6) | .31 |
| Hispanic ethnicity | 1,852 (3.1) | 436 (2.2) | <.0001∗ | 1,384 (2.8) | 330 (1.9) | <.0001∗ |
| Priority community | 3,775 (6.4) | 345 (1.8) | <.0001∗ | 2,441 (4.9) | 224 (1.3) | <.0001∗ |
| Insurance | ||||||
| Private | 36,598 (61.9) | 12,159 (62.1) | Reference | 31,529 (62.8) | 10,613 (62.6) | Reference |
| Public | 20,012 (33.9) | 6,459 (33.0) | .10 | 16,478 (32.8) | 5,490 (32.4) | .59 |
| Other or unknown | 2,470 (4.2) | 976 (5.0) | <.0001∗ | 2,187 (4.4) | 843 (5.0) | .001∗ |
| Marital status | ||||||
| Single | 14,181 (24.0) | 4,782 (24.4) | Reference | 10,917 (21.7) | 3,692 (21.8) | Reference |
| Married | 32,482 (55.0) | 10,921 (55.7) | .88 | 28,855 (57.5) | 9,890 (58.4) | .55 |
| Divorced or separated | 4,324 (7.3) | 1,431 (7.3) | .59 | 3,661 (7.3) | 1,230 (7.2) | .86 |
| Other | 8,093 (13.7) | 2,460 (12.6) | .0002∗ | 6,761 (13.5) | 2,134 (12.6) | .03∗ |
| Modality | ||||||
| X-ray | 16,939 (28.7) | 4,875 (24.9) | Reference | 11,601 (23.1) | 3,438 (20.3) | Reference |
| CT | 11,463 (19.4) | 3,582 (18.3) | .001∗ | 9,532 (19.0) | 2,933 (17.3) | .19 |
| DEXA | 1,187 (2.0) | 493 (2.5) | <.0001∗ | 1,187 (2.4) | 493 (2.9) | <.0001∗ |
| Mammography | 7,386 (12.5) | 3,385 (17.3) | <.0001∗ | 7,383 (14.7) | 3,383 (20.0) | <.0001∗ |
| MR | 8,024 (13.6) | 2,772 (14.1) | <.0001∗ | 7,749 (15.4) | 2,654 (15.7) | <.0001∗ |
| Ultrasound | 11,732 (19.9) | 3,790 (19.3) | <.0001∗ | 10,417 (20.8) | 3,352 (19.8) | <.01∗ |
| Other | 2,349 (4.0) | 697 (3.6) | .51 | 2,325 (4.6) | 693 (4.1) | .90 |
| Setting | ||||||
| Emergency department | 5,287 (8.9) | 1,732 (8.8) | Reference | n/a | n/a | n/a |
| Inpatient | 3,599 (6.1) | 916 (4.7) | <.0001∗ | n/a | n/a | n/a |
| Outpatient | 50,194 (85.0) | 16,946 (86.5) | .30 | n/a | n/a | n/a |
COVID-19 = coronavirus disease 2019; DEXA = dual energy x-ray absorptiometry; n/a = not applicable; Post = postshutdown; Pre = preshutdown;
Statistically significant.
When looking only at diagnostic examinations performed in the outpatient setting, similar results were demonstrated for race and ethnicity with a smaller proportion of imaging examinations post-COVID-19 shutdown (Table 1). On assessing age using the Centers for Disease Control age risk categories, there was some increase in higher age groups, specifically in the 75- to 84-year age group (11.4% to 12.1%; P = .03).
Multivariable Analysis
On multivariable analysis assessing radiology examination utilization post-COVID-19 shutdown (Table 2 ), Asian race (odds ratio [OR] = 0.90, P = .02) and Hispanic ethnicity (OR = 0.82, P < .01) had lower OR for imaging examinations post-COVID-19 shutdown. And similar to results from the univariate analysis, imaging examinations for patients from priority communities had significantly lower OR for post-COVID-19 shutdown examinations (OR = 0.25, P < .0001). Specifically, after the end of the state-mandated COVID-19 shutdown, the odds of having diagnostic radiology examinations for patients in priority communities compared with patients from other communities was 0.25 that of during the pre-COVID-19 shutdown period. Age remained significant with lower OR for imaging examinations post-COVID-19 shutdown in the 30- to 39-year age group (OR = 0.87, P < .01). Marital status was noted to be a significant factor in multivariable analysis with married (OR = 0.93, P < .01) and divorced or separated patients (OR = 0.93, P < .05) with lower OR for post-COVID-19 shutdown diagnostic radiology examinations. Inpatient (OR = 0.66, P < .0001) and outpatient imaging utilization (OR = 0.81, P < .0001) were less than that for ED patients. Dual energy x-ray absorptiometry examinations, mammography, MRI, and ultrasound had significantly greater odds of being performed compared with x-ray examinations (Table 2).
Table 2.
Multivariable analysis assessing diagnostic radiology examination utilization post-COVID-19 shutdown
| Variable | All Care Settings |
Outpatient Only |
||
|---|---|---|---|---|
| Odds Ratio | P Value | Odds Ratio | P Value | |
| Age (y) | ||||
| 18-29 | Reference | Reference | ||
| 30-39 | 0.87 | <.01∗ | 0.88 | <.01∗ |
| 40-49 | 0.89 | <.01∗ | 0.92 | .06 |
| 50-64 | 0.96 | .22 | 0.99 | .74 |
| 65-74 | 0.98 | .56 | 1.02 | .59 |
| 75-84 | 1.05 | .24 | 1.10 | .05 |
| 85+ | 0.99 | .91 | 1.02 | .79 |
| Male | 1.03 | .13 | 1.00 | .93 |
| Race | ||||
| White | Reference | Reference | ||
| Black | 1.02 | .66 | 0.93 | .10 |
| Asian | 0.90 | .02∗ | 0.87 | <.01∗ |
| Other | 1.19 | <.01∗ | 1.12 | <.01∗ |
| Hispanic ethnicity | 0.82 | <.01∗ | 0.81 | <.01∗ |
| Priority community | 0.25 | <.0001∗ | 0.26 | <.0001∗ |
| Insurance | ||||
| Private | Reference | Reference | ||
| Public | 0.99 | .63 | 0.99 | .80 |
| Other or unknown | 1.15 | <.01∗ | 1.13 | .02∗ |
| Marital status | ||||
| Single | Reference | Reference | ||
| Married | 0.93 | <.01∗ | 0.93 | <.01∗ |
| Divorced or separated | 0.93 | <.05∗ | 0.92 | <.05∗ |
| Other | 0.81 | <.01∗ | 0.84 | <.01∗ |
| Modality | ||||
| X-ray | Reference | Reference | ||
| CT | 1.03 | .23 | 1.00 | .92 |
| DEXA | 1.40 | <.0001∗ | 1.34 | <.0001∗ |
| Mammogram | 1.63 | <.0001∗ | 1.58 | <.0001∗ |
| MR | 1.17 | <.0001∗ | 1.14 | <.0001∗ |
| Ultrasound | 1.16 | <.0001∗ | 1.15 | <.0001∗ |
| Other | 0.97 | .46 | 0.95 | .34 |
| Setting | ||||
| ED | Reference | n/a | n/a | |
| Inpatient | 0.66 | <.0001∗ | n/a | n/a |
| Outpatient | 0.81 | <.0001∗ | n/a | n/a |
COVID-19 = coronavirus disease 2019; DEXA = dual energy x-ray absorptiometry; ED = emergency department; n/a = not applicable.
Statistically significant.
On multivariable analysis for outpatient settings alone, similar lower ORs for imaging examinations post-COVID-19 shutdown were noted in those with Asian race, Hispanic ethnicity, in the 30- to 39-year age group, married patients, divorced or separated patients, and examinations from patients in priority communities (Table 2).
Discussion
In the study institution, the total number of radiologic examinations per day decreased post-COVID-19 shutdown to 0.58 of those pre-COVID-19 shutdown at all care settings and to 0.59 of those pre-COVID-19 shutdown in outpatient settings alone—a marked decrease in radiology examination utilization despite a statewide reopening of nonessential services but similar to those reported in previously published studies [1,2]. However, the reductions in radiology examination utilization were not equivalent across patient populations, with significantly lower odds of imaging noted in patients from communities with high rates of poverty, unemployment, and chronic disease, exacerbating inequities that existed pre-COVID-19. In addition, patients with Hispanic ethnicity and Asian race had a statistically significantly lower OR for having radiology examinations post-COVID-19 shutdown compared with non-Hispanics and Whites, respectively.
Pre-COVID-19, Hispanic ethnicity had been identified in several studies to be significantly associated with delays in diagnostic imaging [13,22]. However, more conflicting results have been seen with Asian patients and diagnostic radiology examination follow-ups [19]. In breast imaging, for instance, Asian women were significantly more likely to have timely follow-ups compared with White women [13]. Patients of Asian ethnicity have been reported to have higher levels of subjective fear of COVID-19 [23], which may in part account for our finding. These findings are also consistent with other studies that demonstrate the negative effects on health behaviors of the Asian community as a result of xenophobia and discrimination [24,25].
The Boston Public Health Commission reported that socioeconomic determinants such as education, employment, income and poverty, housing, and bias and racism are unevenly distributed within our city among those of differing races and ethnicities, socioeconomic status, and geographic locations [19]. Our institution specifically evaluated zip codes and defined priority populations in Boston, identified by the Boston Public Health Commission, and named specific neighborhood and zip codes with residents who experience disproportionately high rates of poverty, unemployment, and chronic disease [18]. Patients from these priority communities had significantly lower odds of having radiology examinations post-COVID-19 shutdown, with an OR of 0.25 in our adjusted model. This may be related to reduced access to health care among patients who are unemployed or having lower income [18]. In a publication from another Boston institution that described disease severity of COVID-19 on chest x-ray and evaluated the impact of race and ethnicity including in patients who live in priority populations, non-White patients hospitalized with COVID-19 infection were more likely to present with higher severity of disease [26]. This highlights the need for more outreach to these communities to address potential resource underutilization and delay in diagnostic care in these vulnerable patients. In addition, it is important to raise societal awareness regarding various socioeconomic factors that need to be addressed more globally, including providing more financial resources and health care access during times of calamities and pandemics.
We also identified lower odds of having radiology examinations post-COVID-19 in married and divorced patients compared with single patients, even adjusting for patient demographics. A contributing factor may include the potential impact of childcare on not seeking health services. Married people are more likely to have children than those who are single [27], and this presents a barrier to seeking care during COVID-19 because of potential difficulties in arranging childcare as well as prioritizing their children’s needs.
We demonstrated an overall decrease in imaging utilization post-COVID-19 shutdown, which has been corroborated by several other studies in the United States and varied by subspecialty and geographic location [1,2]. We further noted that radiology examination utilization remained at significantly lower levels in inpatient and outpatient settings compared with the ED post-COVID-19 shutdown. This supports the contention that procedures that are considered more elective in nature were likely more susceptible to deferral than those that are considered more urgent [2,28].
Finally, we demonstrated significant changes in composition of imaging modality post-COVID-19. The odds of undergoing mammography, dual energy x-ray absorptiometry, MRI, and ultrasound were greater than that of x-rays. Perhaps these could be related to a surge in imaging volumes for preventive services that were not delivered during the statewide closure [2]. This emphasizes results in several studies highlighting changes in composition of imaging modalities during COVID-19 [2,29]. Radiology practices need to be prepared for these shifts in imaging utilization to appropriately allocate health care resources.
Radiology practices need to understand and address factors, particularly social determinants of health, which may exacerbate known inequities in diagnostic radiology examination utilization during the COVID-19 pandemic. The clinical significance of the observed reduction in radiology examination utilization should be studied further, especially its impact on subgroups of patients who receive less diagnostic imaging. Providing resources to address patients who need to receive necessary diagnostic radiology examinations may be necessary to achieve safer and more effective care for our most vulnerable populations.
Limitations
Limitations of this study include the retrospective nature of our data analysis. We did not account for specific household incomes, gender identity, or disease acuity and severity, although outpatient examinations are more likely to be less urgent than ED examinations. In addition, this study was conducted in a single academic medical center and outpatient practices in the Boston area and may not generalize to other institutions. Finally, patient outcomes and instances of delayed diagnoses were not specifically evaluated.
Take-Home Points
-
▪
Health care inequities in diagnostic radiology have been exacerbated in the early stages of reopening post COVID-19 with patients from priority communities including specific neighborhood and zip codes with residents who experience disproportionately high rates of poverty, unemployment, and chronic disease having significantly lower odds (OR of 0.25) of having radiology examinations post-COVID-19 shutdown.
-
▪
Patients of Asian race and Hispanic ethnicity had a significantly lower OR for having radiology examinations post-COVID-19 shutdown compared with Whites and non-Hispanics, respectively.
-
▪
Additional focus and outreach to some of the most vulnerable patients (based on socio-economic status, race, and ethnicity) will be needed to diminish the potential patient safety and quality of care risks associated with delayed or deferred clinically necessary diagnostic radiology examinations during and after the COVID-19 pandemic.
Acknowledgments
This work was supported by Agency for Healthcare Research and Quality grant number R01HS024722. We thank Ms Laura Peterson for reviewing the manuscript.
Footnotes
The authors state that they have no conflict of interest related to the material discussed in this article. Dr Lacson, Dr Shi, Dr Kapoor, Dr Eappen, Dr Boland, and Dr Khorasani are nonpartner, non–partnership track employees.
References
- 1.Naidich J.J., Boltyenkov A., Wang J.J., Chusid J., Hughes D., Sanelli P.C. Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J Am Coll Radiol. 2020;17:865–872. doi: 10.1016/j.jacr.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Madhuripan N., Cheung H.M.C., Alicia Cheong L.H., Jawahar A., Willis M.H., Larson D.B. Variables influencing radiology volume recovery during the next phase of the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020;17:855–864. doi: 10.1016/j.jacr.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi J., Giess C., Martin L. Radiology workload changes during the COVID-19 pandemic: implications for staff redeployment. Acad Radiol. 2021 Jan;28(1):1–7. doi: 10.1016/j.acra.2020.09.008. Epub 2020 Oct 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parikh K.D., Ramaiya N.H., Kikano E.G. COVID-19 pandemic impact on decreased imaging utilization: a single institutional experience. Acad Radiol. 2020;27:1204–1213. doi: 10.1016/j.acra.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 Pandemic on radiology practices. Radiology. 2020;296:E141–E144. doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solomon M.D., McNulty E.J., Rana J.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 7.Bres Bullrich M., Fridman S., Mandzia J.L. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693–696. doi: 10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hostetter M., Klein S. As the pandemic evolves, so do ambulatory care practices. Commonwealth Fund. Available at: Published June 2020. Accessed January 18, 2020. [DOI]
- 9.Egede L.E., Walker R.J. Structural racism, social risk factors, and Covid-19—a dangerous convergence for Black Americans. N Engl J Med. 2020;383:e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Payne N.R., Puumala S.E. Racial disparities in ordering laboratory and radiology tests for pediatric patients in the emergency department. Pediatr Emerg Care. 2013;29:598–606. doi: 10.1097/PEC.0b013e31828e6489. [DOI] [PubMed] [Google Scholar]
- 11.Betancourt J.R., Tan-McGrory A., Flores E., López D. Racial and ethnic disparities in radiology: a call to action. J Am Coll Radiol. 2019;16(4 Pt B):547–553. doi: 10.1016/j.jacr.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 12.Flores E.J., Park E.R., Irwin K.E. Improving lung cancer screening access for individuals with serious mental illness. J Am Coll Radiol. 2019;16(4 Pt B):596–600. doi: 10.1016/j.jacr.2018.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lacson R., Wang A., Cochon L. Factors associated with optimal follow-up in women with BI-RADS 3 breast findings. J Am Coll Radiol. 2020;17:469–474. doi: 10.1016/j.jacr.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henderson L.M., O’Meara E.S., Haas J.S. The role of social determinants of health in self-reported access to health care among women undergoing screening mammography. J Womens Health (Larchmt) 2020;29(11):1437–1446. doi: 10.1089/jwh.2019.8267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mishra S.I., DeForge B., Barnet B., Ntiri S., Grant L. Social determinants of breast cancer screening in urban primary care practices: a community-engaged formative study. Womens Health Issues. 2012;22:e429–e438. doi: 10.1016/j.whi.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Burks C.A., Ortega G., Bergmark R.W. COVID-19, disparities, and opportunities for equity in otolaryngology-unequal America. JAMA Otolaryngol Head Neck Surg. 2020;146(11):995–996. doi: 10.1001/jamaoto.2020.2874. [DOI] [PubMed] [Google Scholar]
- 17.Mossa-Basha M., Medverd J., Linnau K. University of Washington. Radiology; 2020. Policies and guidelines for COVID-19 preparedness: experiences from the. 296:E26-E31. [DOI] [PubMed] [Google Scholar]
- 18.Brigham and Women’s Hospital Center for Community Health and Health Equity Community health needs assessment and implementation plan. https://www.brighamandwomens.org/about-bwh/community-health-equity/community-health-needs-assessment Available at: Published 2016. Accessed November 26, 2020.
- 19.Boston Public Health Commission—Research and Evaluation Office. Health of Boston 2016-2017. Boston, MA, 2016-2017. Available at: https://www.bphc.org/healthdata/health-of-boston-report/Pages/Health-of-Boston-Report.aspx. Accessed January 18, 2021.
- 20.Centers for Disease Control and Prevention COVID-19 hospitalization and death by age. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html Available at:
- 21.Bursac Z., Gauss C.H., Williams D.K., Hosmer D.W. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yee A.M., Mazumder P.K., Dong F., Neeki M.M. Impact of healthcare access disparities on initial diagnosis of breast cancer in the emergency department. Cureus. 2020;12 doi: 10.7759/cureus.10027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fitzpatrick K.M., Drawve G., Harris C. Facing new fears during the COVID-19 pandemic: the state of America’s mental health. J Anxiety Disord. 2020;75:102291. doi: 10.1016/j.janxdis.2020.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubey A.D. The resurgence of cyber-racism COVID-19 pandemic and its after effects. JMIR Public Health Surveill. 2020;6(4):e19833. doi: 10.2196/19833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darling-Hammond S., Michaels E.K., Allen A.M. After “the China virus” went viral: racially charged coronavirus coverage and trends in bias against Asian Americans. Health Educ Behav. 2020;47(6):870–879. doi: 10.1177/1090198120957949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joseph N.P., Reid N.J., Som A. Racial and ethnic disparities in disease severity on admission chest radiographs among patients admitted with confirmed coronavirus disease 2019: a retrospective cohort study. Radiology. 2020;297:E303–E312. doi: 10.1148/radiol.2020202602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Livingston G. The changing profile of unmarried parents. Pew Research Center. https://www.pewsocialtrends.org/2018/04/25/the-changing-profile-of-unmarried-parents/ Available at: Published 2018. Accessed January 18, 2021.
- 28.Best M.J., McFarland E.G., Anderson G.F., Srikumaran U. The likely economic impact of fewer elective surgical procedures on US hospitals during the COVID-19 pandemic. Surgery. 2020;168(5):962–967. doi: 10.1016/j.surg.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naidich J.J., Boltyenkov A., Wang J.J., Chusid J., Hughes D., Sanelli P.C. Coronavirus disease 2019 (COVID-19) pandemic shifts inpatient imaging utilization. J Am Coll Radiol. 2020;17(10):1289–1298. doi: 10.1016/j.jacr.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]