Abstract
Background
Amid the opioid crisis, the health care system is restructuring to prevent and treat COVID-19. Individuals in opioid agonist treatment (OAT) are uniquely challenged because of disruption to treatment, medication diversion, and isolation during the pandemic.
Methods
Between January and September 2020, we utilized the electronic medical record from a chain of 67 opioid agonist treatment clinics in Ontario, Canada, to examine routinely collected urine drug screen results of patients in opioid agonist treatment by Public Health Units.
Results
We present evidence of a 108% increase in the percentage of fentanyl positive urine drug screens from April to September (p< 0.001). During the same period, health regions in northern and southwestern Ontario, areas with a high concentration of rural communities, have seen the most notable increase in the percent of fentanyl positive urine drug screen results.
Conclusion
The use of fentanyl increased by 108% among OAT patients in Ontario during the COVID 19 pandemic. We argue that the persistent increase of fentanyl exposure over time, specifically in the OAT population, suggests that reduced monitoring may decrease OAT's effectiveness and negatively impact patient outcomes.
Keywords: Opioid agonist treatment, COVID-19, Fentanyl
Background
Opioid use has been referred to as a public health crisis in Canada (1). A total of 16,364 opioid-related deaths occurred between January 2016 and March 2020 (Special Advisory Committee on the Epidemic of Opioid Overdoses 2020). Ontario is the most populated province in Canada, and it is one of the hardest-hit regions by the opioid crisis, along with British Columbia and Alberta. Compounding the complexity of the ongoing opioid crisis, on March 11, 2020, the World Health Organization declared the COVID-19 pandemic (World Health Organization 2020). The pandemic has led to over 11,800 deaths in Canada and over 3500 deaths in Ontario in only nine months (The Public Health Agency of Canada 2020). In an effort to address the pandemic, the Ontario health care system has dramatically restructured to prevent and treat COVID-19.
The evidence to support the efficacy of opioid agonist treatment (OAT), including methadone and buprenorphine/naloxone, is well established to treat opioid use disorder (OUD) (Amato et al., 2005). In Ontario, most patients receiving OAT will start treatment at a specialized addiction clinic for observed daily dosing by a nurse or pharmacist.The treatment involves taking an opioid agonist medication daily. Daily contact is in place to ensure patient safety and treatment effectiveness. After a period of stabilization, physicians can allocate take-home doses, also known as carries, but this is done on a case by case basis depending on the patient's progress with treatment (Center for Addiction & Mental Health 2014. Some patients are then followed in a family physician's office or community pharmacy following stabilization. In Ontario, increasing the provision of take-home doses is done as part of a contingency management strategy to provide incentives to reduce the use of opioids and other drugs during treatment. Contingency management has been shown to be effective in reducing substance use and to maximize patient psychosocial function (Griffith, Rowan-Szal, Roark & Simpson, 2000). The pre-pandemic guidelines in Ontario required that patients receiving OAT start treatment with observed medication intake daily for at least two months (Center for Addiction & Mental Health 2016).
Recently, OAT Guidelines were altered in response to COVID-19 (Centre for Addiction & Mental Health 2020). The revised guidelines suggest that during this time of widespread COVID-19 community transmission, exceptional OAT take-home doses can be considered a way to provide ongoing care (Centre for Addiction & Mental Health 2020). The changes present an opportunity for physical distancing by reducing pharmacy and clinic visits. However, the reduction in monitoring and frequency of clinical contact may undermine OAT's effectiveness and reduce the ability to provide contingency management. The decrease in observed dosing can also pose a risk to public safety through enhanced diversion of medications to people with OUD who are not patients in OAT.
Several commentaries have been published in response to the opioid crisis and COVID-19 pandemic. This study aims to present a Canadian perspective on increased fentanyl positive urine drug screen results among OAT patients during the COVID-19 pandemic.
Methods
Ontario context
In Ontario, the highest level of lockdown measures in the first wave of the COVID-19 pandemic were in place between April and June 2020. During this time, only services deemed essential, such as grocery stores, hospitals, pharmacies, and very few others, remained open. Ontarians were advised to leave their homes only if absolutely necessary. In June of 2020, the Ontario government took a staged approach to allow other businesses such as restaurants, fitness and leisure facilities and retail stores to open. Physical distancing measures can compound stress and further isolate people with OUD, a population with an already elevated prevalence of pre-existing mental disorders and health conditions.
Between January and September 2020, we utilized the electronic medical record from a chain of 67 OAT clinics in Ontario, Canada, to examine routinely collected urine drug screen results of patients in OAT. All data were de-identified. The data were cross-tabulated by Public Health Units across Ontario.
The percent positive urine drug screen results were calculated by dividing the number of positive samples by the total number of samples by month. We used a Fractional Logistic Regression model to estimate the differences of fentanyl positive urine drug screen results over time. We calculated the odds ratio for each month, keeping January as a reference month. Lastly, using Public Health Ontario, Easy Maps, we displayed the positive fentanyl urine drug screen results by Public Health Units in Ontario.
Results
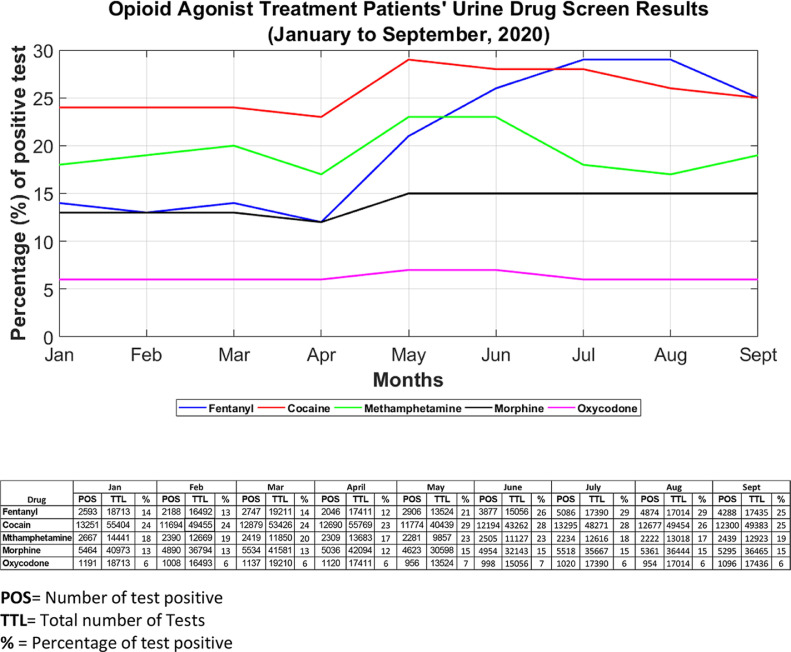
A total of 14,669 individual patients were included in the analysis. Of the 152,246 fentanyl urine drug screen tests analyzed, over 9 months, 30,605 (20.1%) were positive. As shown in Fig. 1 , the urine drug screen results indicate a drastic increase in the positive fentanyl urine drug screen results among OAT patients in Ontario from April to September 2020. The percentage of fentanyl positive urine drug screens increased by108% from April to September. The highest percentage being in July (29%) and August (29%). There was a significant increase in the percentage of fentanyl positive urine samples between January 2020 and September 2020 (p< 0.001). The odds ratio (OR) for April was 0.9, (95% Confidence Interval (CI) 0.8–0.9), for May (OR=1.7, 95% CI 1.5–1.89), for August (OR= 2.6, 95% CI 2.3- 2.9) and for September (OR= 2.2, 95% CI 1.9–2.6). The log odds results are reported in Figure 2 ia available as supplementary material.
Fig. 1.
Urine Drug Screen Results (January to September 2020).
We also examined an increase in fentanyl use in OAT patients in all areas of the province between March and September 2020. In most areas of the province, there was a 1 to 3 fold increase. The most notable increase was in the northern and southwestern regions of Ontario, with a 3 to 4.1 fold increase. The results are depicted in Figure 3, available as supplementary material.
Discussion
As is evident from our findings, the positive fentanyl urine drug screen results doubled during the period with the most strict lockdown measures of the first wave of COVID-19 in Ontario (from April to September 2020). Fentanyl exposure was disproportionately evident in northern and southwestern regions of Ontario, where there is a high concentration of rural communities. These findings are especially alarming because patients in northern Ontario already face significant barriers to accessing treatment due to well-documented geographic characteristics, contributing to reduced access to care and limited health human resources (Kiepek et al., 2012). Quantifying the absolute impact of COVID-19 on OAT is challenging. However, the reports of an increase in overdose-related death (Ontario Drug Policy Research Network 2020) and the data presented in this study indicating an increase in fentanyl exposure in OAT patients are all reasonable markers to support evidence of the continued severity of the opioid crisis and potential negative consequences of the COVID-19 pandemic for patients with OUD.
A unique concern brought forth in this study is that patients whose drug use would typically decrease while in OAT (Amato et al., 2005) has increased during a period of reduced monitoring. It is well established in the literature that enrollment in OAT that involves observed dosing and contingency management strategies is associated with a decrease in drug use (Griffith et al., 2000). Therefore, we argue that the persistent increase of fentanyl positive urine samples over time demonstrated in Fig. 1 suggests that reduced monitoring may decrease OAT's effectiveness and thus negatively impact patient outcomes. In other medical settings, including primary care, community care, and hospitals, measures such as increased personal protective equipment for staff, physical distancing and masks are in place to reduce the spread of the COVID 19 virus. We suggest that strict infection control measures be implemented rather than reduced monitoring to avoid OAT patients' negative health outcomes.
Several factors are likely influencing the increase in fentanyl exposure during the pandemic. Top of mind in the media are disrupted supply chains and border closures that cause shortages of goods, including drugs. The sharp increase in positive fentanyl urine drug screen results demonstrated in Fig. 1 in April may suggest that people are turning to the illicit market due to disruptions in services. Still, it may also indicate that people are seeking drugs from unfamiliar drug networks due to temporary shortages in their usual supply. That being said, the persistence of high fentanyl levels from June to September may be evidence of increased fentanyl in the market. The overall pattern may also be explained by increased rates of intentional use of fentanyl by individuals due to pandemic-related stress, anxiety and isolation.
Despite the COVID-19 pandemic, the opioid crisis continues, and it has escalated during this time. Several factors limit our collective ability to address the complex issue of opioid use. Perhaps the most significant factor is the resource-intensive nature of services OAT patients require. As we have seen in the last few months with COVID-19, we were able to come together as a society to prioritize the issue of COVID-19 by improving data collection and increasing funding to health and social services. We mobilized collaboration at all levels of government and businesses. It is our opinion that the same urgency should be placed on the opioid crisis. Also, OAT guidelines should return to the level of monitoring and support indicated by best evidence while including infection control efforts implemented in other essential health care settings to ensure OAT treatment effectiveness during this pandemic.
Conclusion
The use of fentanyl increased by 108% among OAT patients in Ontario during the COVID-19 pandemic from April to September 2020. It has been shown that several factors contribute to the increase of fentanyl in the drug market. However, unique to our study, we argue that the persistent rise of fentanyl exposure over time, specifically in the OAT population, suggests that reduced monitoring may decrease OAT's effectiveness.
Declarations of Interest
Dr. David Marsh maintains the following roles: Chief Medical Director at CATC (Canadian Addiction Treatment Center), opioid agonist therapy provider. Dr. Marsh has no ownership stake in the CATC as a stipendiary employee. We do not foresee any conflict of interest as data will be made freely available to the public. Neither the CATC nor the Universities can prevent the publication and dissemination of -knowledge. The authors have no conflicts declared.
Acknowledgement
We thank our funders the Northern Ontario Academic Medical Association through the 2020 Novel Coronavirus (COVID-19) Rapid Research Funding Opportunity Project No: RR-20–03. We also thank Bruce Weaver for generously providing his expert opinion on the analysis for this study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.drugpo.2020.103088.
Appendix. Supplementary materials
References
- Amato L., Davoli M., Perucci C.A., Ferri M., Faggiano F., Mattick R.P. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: Available evidence to inform clinical practice and research. Journal of Substance Abuse Treatment. 2005;28(4):321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Center for Addiction and Mental Health Hidden in our midst: homeless newcomer youth in Toronto – Uncovering the supports to prevent and reduce homelessness. Society CfAaMHaCA; 2014 [Google Scholar]
- Center for Addiction and Mental Health . Health CfAaM; Canada: 2016. Making the choice, making it work: Treatment for opioid addiction. (Ed.) [Google Scholar]
- Centre for Addiction and Mental Health . ON; 2020. COVID-19 opioid agonist treatment guidance Toronto.Https://www.camh.ca/-/media/files/covid-19-modifications-to-opioid-agonist-treatment-delivery-pdf.pdf [Available from: [Google Scholar]
- Griffith J.D., Rowan-Szal G.A., Roark R.R., Simpson D.D. Contingency management in outpatient methadone treatment: A meta-analysis. Drug and Alcohol Dependence. 2000;58(1–2):55–66. doi: 10.1016/s0376-8716(99)00068-x. [DOI] [PubMed] [Google Scholar]
- Kiepek N., Hancock L., Toppozini D., Cromarty H., Morgan A., Kelly L. Facilitating medical withdrawal from opiates in rural Ontario. Rural and Remote Health. 2012;12:2193. [PubMed] [Google Scholar]
- Ontario Drug Policy Research Network . Ontario Drug Policy Research Network; Toronto, ON: 2020. Office of the chief coroner for Ontario/Ontario Forensic Pathology Service; Ontario Agency for health protection and promotion (Public Health Ontario); Centre on Drug Policy. Evaluation. Preliminary patterns in circumstances surrounding opioid-related deaths in Ontario during the COVID-19 pandemic. [Google Scholar]
- Special Advisory Committee on the Epidemic of Opioid Overdoses . Public Health Agency of Canada; ON: 2020. Opioid-related harms in Canada Ottawa,Https://health-infobase.canada.ca/substance-related-harms/opioids [Available from: [Google Scholar]
- The Public Health Agency of Canada . Government of Canada; ON: 2020. Coronavirus disease (COVID-19): Outbreak update Ottawa.Https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html?topic=tilelink [Available from: [Google Scholar]
- World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19(2020).[Available from: Https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid- 19—11-march-2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.