Abstract
Background
Although there are increasing concerns on mental health consequences of the COVID-19 pandemic, no large-scale population-based studies have examined the associations of risk perception of COVID-19 with emotion and subsequent mental health.
Methods
This study analysed cross-sectional and longitudinal data from the PsyCorona Survey that included 54,845 participants from 112 countries, of which 23,278 participants are representative samples of 24 countries in terms of gender and age. Specification curve analysis (SCA) was used to examine associations of risk perception of COVID-19 with emotion and self-rated mental health. This robust method considers all reasonable model specifications to avoid subjective analytical decisions while accounting for multiple testing.
Results
All 162 multilevel linear regressions in the SCA indicated that higher risk perception of COVID-19 was significantly associated with less positive or more negative emotions (median standardised β=-0.171, median SE=0.004, P<0.001). Specifically, regressions involving economic risk perception and negative emotions revealed stronger associations. Moreover, risk perception at baseline survey was inversely associated with subsequent mental health (standardised β=-0.214, SE=0.029, P<0.001). We further used SCA to explore whether this inverse association was mediated by emotional distress. Among the 54 multilevel linear regressions of mental health on risk perception and emotion, 42 models showed a strong mediation effect, where no significant direct effect of risk perception was found after controlling for emotion (P>0.05).
Limitations
Reliance on self-reported data.
Conclusions
Risk perception of COVID-19 was associated with emotion and ultimately mental health. Interventions on reducing excessive risk perception and managing emotional distress could promote mental health.
Keywords: COVID-19, Risk perception, Emotion, Mental health
1. Introduction
COVID-19, a public health emergency of international concern as declared by the WHO, is rapidly sweeping the world and threatening human health both physically and mentally. Since the lockdown of Wuhan, China on January 23, 2020, most countries around the world have implemented lockdown restrictions or social isolation to stop the spread of the COVID-19. Although humans have experienced many epidemics in the past years, the COVID-19 has caused one of the largest global lockdowns in human history. During this special period, it is essential to investigate how people worry about being infected or other adverse consequences of COVID-19, how this risk perception (Paek and Hove, 2017; Dryhurst et al., 2020) affects their emotions, and whether it will eventually lead to mental health problems (Ren et al., 2020).
Risk perception of COVID-19 is the cognitive response and assessment for the threat of the COVID-19 pandemic. Risk perception has two main dimensions according to the psychometric paradigm (Slovic, 1987): “dread” which reflects the perceived lack of control and catastrophic potential, and “risk of the unknown” which refers to the unobservable of the hazard (Peters and Slovic, 1996; Siegrist et al., 2005). The emergence of the COVID-19 pandemic could seriously arouse these two psychological dimensions and make people feel threatened. Extensive evidence from previous research in psychology, clinical science and economics indicated that people perceive the risk cognitively and respond to it emotionally (Loewenstein et al., 2001); in other words, risk perceptions typically drive emotions and psychological distress (Loewenstein et al., 2001; Slovic et al., 2004; Leppin and Aro, 2009). In addition to the direct evidence, stress and motivational prioritisation may link risk perception to emotion and mental health. Consistent evidence has shown that risk perception has a remarkably positive association with the feeling of stress (Lopez-Vazquez, 2001; Lopez-Vazquez and Marvan, 2003). In this case, the threat of the pandemic will induce stress, which will in turn affect people's emotion and mental health according to the social stress theory and empirical evidence (Aneshensel, 1992; Kessler, 1997; Wu et al., 2020; Guidi et al., 2021). In addition, high risk perception of COVID-19 may reflect motivational prioritisation of the COVID-19 threat over other important life goals, needs and duties. This motivational preoccupation could cause emotional fluctuations following the pandemic escalation (Kopetz, 2017). Therefore, we propose that the risk perception of COVID-19 could be associated with emotion and mental health.
Emerging evidence from the previous pandemics (e.g., SARS, H1N1, Ebola) also implied that risk perception could be highly associated with public's emotional responses (Qian et al., 2003; Qian et al., 2005; Raude and Setbon, 2009; Bults et al., 2011; Yang, 2016). For example, Prati et al. (2011) found a positive association between perceived severity and affective response to the H1N1 pandemic in 2009. Yang and Chu (2018) also associated risk perception about the Ebola outbreak with some negative emotions like fear, anger, anxiety, disgust and sadness. In the context of the COVID-19 pandemic, the concerns of getting infected and the economic consequences have been proposed as two major aspects of risk perception of COVID-19 and assessed by several preliminary studies (Soiné et al., 2020; Bruine de Bruin, 2020).
Given the emotional strain during the pandemic, there is increasing concern about its impact on mental health (Burhamah et al. 2020; Planchuelo-Gómez et al., 2020). A national survey in China at the initial stage of COVID-19 outbreak indicated that 27.9% of participants had symptoms of depression, and 31.6% had symptoms of anxiety (Shi et al., 2020). Another survey of US adults in April 2020 reported that 13.6% of participants had symptoms of serious psychological distress, which was substantially higher than the estimate in 2018 (3.9%); and 13.8% of participants frequently felt lonely (McGinty et al., 2020). Several preliminary studies have evaluated the risk perception of COVID-19 in relation to mental health. A survey by Ding et al. (2020) found that the risk perception of COVID-19 was associated with the level of depression. Teufel et al. (2020) observed similar time trends of the levels of risk perception and COVID-19 related fear, depression and generalised anxiety in their survey data. However, these studies were limited by small sample size, being restricted to one country, or the measurement of single dimension of COVID-19 related risk perception. A comprehensive understanding of the association between risk perception and mental health is crucial for developing relevant preventive interventions and social policies during the pandemic.
In this regard, we conducted one of the first large-scale international surveys focusing on risk perception and psychological responses during the peak period of the worldwide outbreak of COVID-19. This study aimed to examine: a) the concurrent association of risk perception with emotion during the pandemic, at both the individual level and the country level, and b) whether the risk perception was associated with subsequent self-rated mental health through its emotional impact.
2. Methods
2.1. Data source
This study was based on the cross-sectional and longitudinal data from the PsyCorona Survey, an international project on COVID-19 that included over 60,000 participants from 112 countries (see www.psycorona.org for details). This 20-minute web-based survey, which has been translated into 30 languages, aims to investigate the psychological impact of the coronavirus spread. Data on risk perception of COVID-19 and emotion were collected in the baseline survey from March 19, 2020. After the baseline survey, participants were invited by email to complete a follow-up survey one week later on a voluntary basis, in which mental health data were collected to reflect the subsequent acute mental health response to the COVID-19 pandemic.
To increase the representativeness of the baseline survey, a subset of participants from 24 countries were sampled online through Qualtrics’ panel management service (or WJX Company in China) from April 10 to May 11, 2020. For each of the 24 countries (Argentina, Australia, Brazil, Canada, China, France, Germany, Greece, Indonesia, Italy, Japan, Netherlands, Philippines, Romania, Russia, Saudi Arabia, Serbia, South Africa, South Korea, Spain, Turkey, the United Kingdom, Ukraine, and the United States), around 1000 participants were selected who are representative of the country's general population in terms of gender and age.
PsyCorona Survey was approved by the Ethical committee of the University of Groningen (study code: PSY-1920-S-0390) and New York University Abu Dhabi (study code: HRPP-2020-42). All participants gave informed consent before taking the survey. Detailed methodology and quality control procedures of the PsyCorona Survey are presented in the CHERRIES checklist (Eysenbach, 2004) as a Supplementary File.
2.2. Measures
Response variables. a) Emotion. PsyCorona Survey measured 12 specific emotions using an adapted PANAS Scale (Russell, 1980; Watson et al., 1988), including anxious, bored, depressed, nervous, exhausted, lonely (all classified as negative emotions; Cronbach's α=0.80), calm, content, excited, inspired, relaxed and happy (positive emotions; Cronbach's α=0.78). All emotions were measured in a 5-point Likert scale from 1 (very slightly or not at all) to 5 (extremely) except for happiness, which was originally measured in a 10-point rating scale and then re-scaled to 5-point through linear transformation. b) Mental health. PsyCorona Survey used a single-item self-reported measure of mental health (“How is your current mental health?”) in the follow-up survey (Ahmad et al., 2014), with a 10-point scale from 1 (terrible) to 10 (excellent). According to a review by Ahmad et al. (2014), this single-item measure correlates well with several validated multi-item measures of mental health.
Explanatory variables. Risk perception of COVID-19: PsyCorona Survey measured the risk perception of getting infected (infection-risk) and the risk perception of suffering from economic consequences of COVID-19 (economic-risk) in two separate items, with an 8-point Likert scale from 1 (exceptionally unlikely) to 8 (already happened).
Potential confounding variables. Two groups of confounders were considered in this study. The first group is basic demographic factors: age, gender and education level. The second group is other variables that may have an impact on risk perception, emotion or mental health, including religion, employment status, personal financial strain, social contact (online/in person), presence of someone to discuss personal matters with, close relationship with infected patients, knowledge about COVID-19 and its potential economic consequences, and clear message received on coping with COVID-19. Details of relevant items are displayed in Supplementary Table 1. The relationships between these potential confounders and explanatory and response variables, assessed by correlation coefficients or one-way analysis of variance, are presented in Supplementary Table 2 and Supplementary Table 3.
2.3. Eligible participants
For the cross-sectional analysis of risk perception and emotion, we used baseline data collected from 61,676 participants during March 19 to May 17, 2020. We excluded 3212 participants with any missing values in the explanatory and response variables and country, age group and gender, and conducted complete-case analysis given the small proportion (5%) of missing data (Bennett, 2001) and the quality concerns of incomplete questionnaires. We further excluded 3619 participants who chose option 8 (“already happened”) in either of the two risk perception items, so that the highest risk perception category is 7 (“all but certain”). This resulted in a sample population of 54,845 participants across 112 countries. In addition, we conducted a sensitivity analysis by repeating the analytical procedures in the representative sample of baseline survey, including 23,278 participants from 24 countries. This sensitivity analysis aimed to increase the representativeness of the results and assess the robustness of main findings.
For the analyses involving mental health, we included 1404 participants who had valid data on self-rated mental health in the follow-up survey. Complete-case analysis was used to deal with missing values on covariates in this study (each covariate had 0 to <1% missing values).
2.4. Statistical analysis
Characteristics of study population and mean values of self-reported risk perception, negative/positive emotion and overall mental health were described. For countries with at least 200 participants, a cross-sectional ecological analysis was conducted to examine the correlations between country-level mean values of risk perception items and country-level mean values of negative emotion items or positive emotion items.
Since there are multiple items for each construct and various analytical options to test the association between risk perception and emotion or mental health, it is hard to select one optimal model specification (i.e., which items to use and how many covariates to adjust for) objectively. In this regard, specification curve analysis (SCA) (Simonsohn et al., 2015; Orben and Przybylski, 2019) was adopted which considers all reasonable model specifications to avoid subjective analytical decisions (Table 1 ). Based on multilevel linear regressions with emotion or mental health as response variable and country-level intercepts as random effect, multiple analytical options regarding response variables, explanatory variables and covariate adjustment were tested. All variables were standardised before analysis using the mean and standard deviation (SD) of the full sample. After implementing all model specifications, the median standardised β and median standard error (SE) were used as summary statistics. No conventional effect size was computed in this study because all models were multilevel linear regressions with random-intercept, for which the standardised regression coefficient has been recommended as one of the optimal effect sizes to represent the magnitude of fixed effects (i.e., associations between explanatory and response variables), especially when working with large samples (Lorah, 2018). In addition, since there are multiple model specifications in one SCA, a median SE is more suitable as a summary statistic to quantify the precision of effect estimate than a median confidence interval (each specification has its upper and lower bounds).
Table 1.
Items on risk perception of COVID-19, emotion and mental health with possible model specifications.
| Constructs | Items | Analytical decisions |
|---|---|---|
| Risk perception of COVID-19 | How likely is it that the following will happen to you in the next few months: you will get infected with the coronavirus. | Each item individually; or average score of the two items. |
| How likely is it that the following will happen to you in the next few months: your personal situation will get worse due to economic consequences of coronavirus. | ||
| Emotion | Negative emotions (item scores reversed): How did you feel over the last week? –Anxious; Bored; Depressed; Nervous; Exhausted; Lonely (or isolated from others/left out). | Each of the 12 emotions individually; average score of the six negative emotions, six positive emotions or all 12 emotions; the first principal component score of the six negative emotions, six positive emotions or all 12 emotions (which represents 51%, 48% or 37% of total variance, respectively). |
| Positive emotions: How did you feel over the last week? -Calm; Content; Excited; Inspired; Relaxed; Happy. | ||
| Mental health | How is your current mental health? | Only one specification. |
SCA of association between risk perception and emotion. In this analysis, the scores of negative emotions were reversed for consistency with positive emotions so that a higher score reflects a lower level of negative emotions. Three model specification factors were considered: 1) Response variable (the 12 emotions were modelled as response variable individually, or in combination as average score of positive emotion, negative emotion or all emotion items, or principal component score through principal component analysis (PCA)); 2) Explanatory variable (two items on risk perception were used individually, or as average score); 3) Covariate adjustment (no covariates; only adjusting for basic demographics; or further adjusting for a full set of potential confounders mentioned above). After combining the three model specification factors, the total numbers of model specifications were 162 (18 for emotion × 3 for risk perception × 3 for covariate adjustment). The sample size was 54,845, 54,731 or 49,911 for models with no covariates, with adjustment for basic demographics or fully adjusted models.
SCA of associations of risk perception and emotion with subsequent mental health. Multilevel linear regression was conducted to test whether the average score of risk perception items in baseline survey was associated with subsequent mental health in follow-up survey. A separate SCA was further used to examine whether the association between risk perception and mental health was mediated by emotion. Different from the traditional SCA (Simonsohn et al., 2015; Orben and Przybylski, 2019), this adapted SCA simultaneously included risk perception and emotion as explanatory variables of interest in each model, and considered different combinations of their analytical choices which allows the examination of an overall mediation effect. Four model specification factors were considered: 1) Response variable (the item on mental health); 2) Explanatory variable of risk perception (three options similar as in the previous SCA); 3) Explanatory variable of emotion (average score or PCA score of negative emotion, positive emotion or all emotion items; no individual emotion item was used here since we want to examine the mediation effect of emotional composite); and 4) Covariate adjustment (three options similar as in the previous SCA). The total numbers of model specifications after combination were 54 (1 for mental health × 3 for risk perception × 6 for emotion × 3 for covariate adjustment). The sample size of models with no covariates, with adjustment for basic demographics or fully adjusted models was 1404, 1403 or 1354, respectively.
Statistical inferences for SCA. To test the overall hypothesis that risk perception was associated with emotion, we used bootstrapping technique to perform joint significance tests of SCA while accounting for the inflation of type 1 error rate due to multiple testing with various model specifications. Based on a pseudo-dataset where the null hypothesis is true, 1000 bootstrapped datasets of the same size were generated by random sampling with replacement. 1000 repeated SCAs were then conducted for the estimation of distribution of estimated median standardised β. The null hypothesis was rejected if the probability of re-sampled median standardised β being larger in magnitude than observed value in original SCA was below 0.05.
Similar bootstrapped tests were conducted in the second SCA for the hypotheses that risk perception was not independently associated with mental health after controlling for emotion (i.e., complete mediation), while emotion was independently associated with mental health. All statistical analyses were conducted using R software (version 4.0.0). Codes for SCA were adapted from R functions developed by Orben and Przybylski (2019). All statistical tests were two-sided. Where applicable, P<0.05 indicates statistical significance.
3. Results
3.1. Population characteristics and descriptive analysis
Of the 54,845 participants included in this study, 61% are female; 47%, 45% or 8% are aged between 18-34, 35-64 or over 65 years old; and 48%, 31% or 21% have education level below, equivalent or above Bachelor's degree. The mean scores of risk perception of getting infected and suffering from economic consequences of COVID-19 are 3.5 and 4.2 (range from 1 to 7; SD=1.4 and 1.6); the mean scores of negative emotions on average and positive emotions on average are 2.5 and 2.7 (range from 1 to 5; SD=0.8 and 0.7); and the mean score of self-rated mental health is 6.9 (ranges from 1 to 10; SD=2.0). Of the 1404 participants with follow-up data, 69% are female; 50%, 46% or 4% are aged between 18-34, 35-64 or over 65 years old; and 39%, 32% or 29% have education level below, equivalent or above Bachelor's degree.
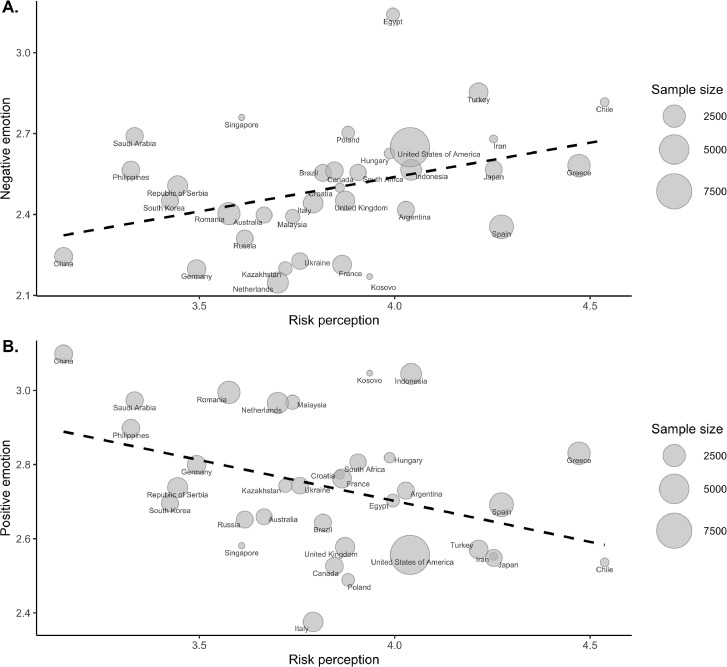
The scatter plots of country-level summary statistics showed that country-level mean values of risk perception was positively correlated with mean values of negative emotion (Fig. 1 A; r=0.371, P=0.031), and negatively correlated with positive emotion (Fig. 1B; r=-0.393, P=0.022). Among the 34 countries displayed in the plots, the country-level mean risk perception varies from 3.2 to 4.5 (SD=0.3); the country-level mean negative emotion and positive emotion vary from 2.1 to 3.1 (SD=0.2) and 2.4 to 3.1 (SD=0.2), respectively. Results of the sensitivity analysis with representative sub-sample of 24 countries revealed similar patterns (Supplementary Figure 1).
Fig. 1.
Scatter plots of country-level mean values of negative emotion (A) and positive emotion (B) against country-level mean values of risk perception of COVID-19.
Only 34 countries with at least 200 participants are displayed. The size of bubbles was proportional to the sample size of the corresponding country. The dashed line in each plot was fitted by simple linear regression. Six negative emotions and six positive emotions were rated in 5-point scale from 1 (very slightly or not at all) to 5 (extremely); the average score for each of the two groups of emotion is shown on y axis in the two plots separately. Two items of risk perception of getting infected or suffering from economic consequences were in 7-point scale from 1 (exceptionally unlikely) to 7 (all but certain); the average score is shown on x axis in both plots.
3.2. Specification curve analysis for association between risk perception and emotion
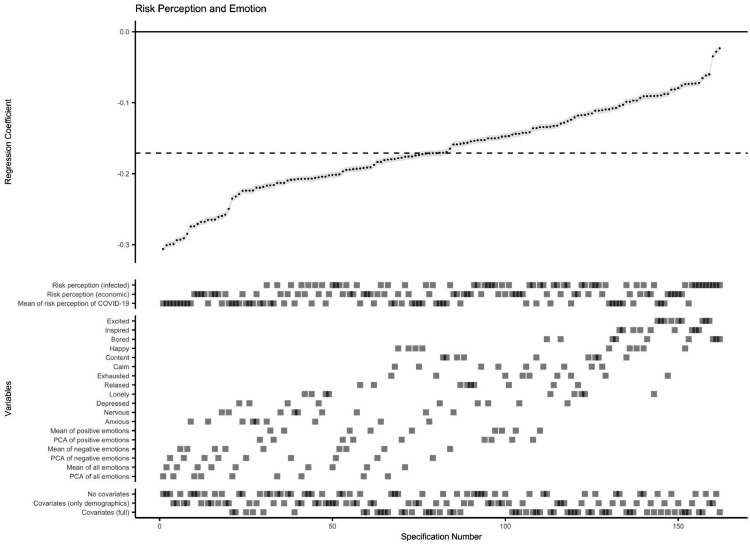
All 162 model specifications for multilevel linear regressions showed higher risk perception of COVID-19 was significantly associated with less positive or more negative emotions (median standardised β=-0.171, median SE=0.004, maximum P=2×10−7; Fig. 2 ). Results of bootstrapped test based on 1000 re-sampled datasets, accounting for the multiple testing across specifications, supported the overall hypothesis of an association between risk perception and emotion. Under the null hypothesis, the probability of getting a larger median standardised β in magnitude than observed value in original SCA (0.171) was below 0.001.
Fig. 2.
Results of specification curve analysis for association between risk perception and emotion.
The standardised β coefficients for the association of risk perception of COVID-19 with emotion obtained from all 162 specifications (listed on x axis) are plotted at the upper half of the graph (all P<0.001). Each point represents the β coefficient of one specification, and the error bar (in grey) represents the corresponding standard error (SE). The dashed line indicates the median standardised β coefficient (median standardised β=-0.171, median SE=0.004, median sample size=54,731). At the lower half of the graph, the corresponding specifications for each level of the three model specification factors are displayed as squares.
Furthermore, the SCA plot visualised the influences of different analytical options on the effect estimates. As shown in Fig. 2, using the average score of negative emotion items as response variable yielded a larger magnitude of effect estimate (median standardised β=-0.218, median SE=0.004) than using the average score of positive emotion items (median standardised β=-0.176, median SE=0.004; Table 2 ), suggesting a stronger association of risk perception with negative emotion. In addition, the economic-risk was in stronger association with emotion (median standardised β=-0.165, median SE=0.004) than the infection-risk (median standardised β=-0.139, median SE=0.004). Not adjusting for covariates (median standardised β=-0.186, median SE=0.004) or only adjusting for basic demographics yielded similar effect estimates (median standardised β=-0.182, median SE=0.004), whereas adjusting for a full set of covariates resulted in a weaker independent effect of risk perception on emotion (median standardised β=-0.136, median SE=0.005).
Table 2.
Results of specification curve analyses by different choices of emotion variables.
| Response variable | Explanatory variables | Median sample size | Median standardised β | Median SE |
|---|---|---|---|---|
| SCA 1 | ||||
| Overall emotion* | Risk perception | 54,731 | -0.232 | 0.004 |
| Positive emotion* | Risk perception | 54,731 | -0.176 | 0.004 |
| Negative emotion* | Risk perception | 54,731 | -0.218 | 0.004 |
| SCA 2 | ||||
| Mental health | Overall emotion* | 1403 | 0.577 | 0.025 |
| Risk perception | 1403 | -0.033 | 0.025 | |
| Mental health | Positive emotion* | 1403 | 0.497 | 0.027 |
| Risk perception | 1403 | -0.071 | 0.024 | |
| Mental health | Negative emotion* | 1403 | 0.539 | 0.025 |
| Risk perception | 1403 | -0.031 | 0.024 |
*. Overall emotion, positive emotion and negative emotion refer to the average score of all emotion items, positive emotion items and negative emotion items, respectively.
Abbreviations: SCA = specification curve analysis; SE = standard error.
The sensitivity analysis using representative sample of 23,278 participants also showed similar SCA estimates (median standardised β=-0.167, median SE=0.007; P of bootstrapped test<0.001; Supplementary Figure 2).
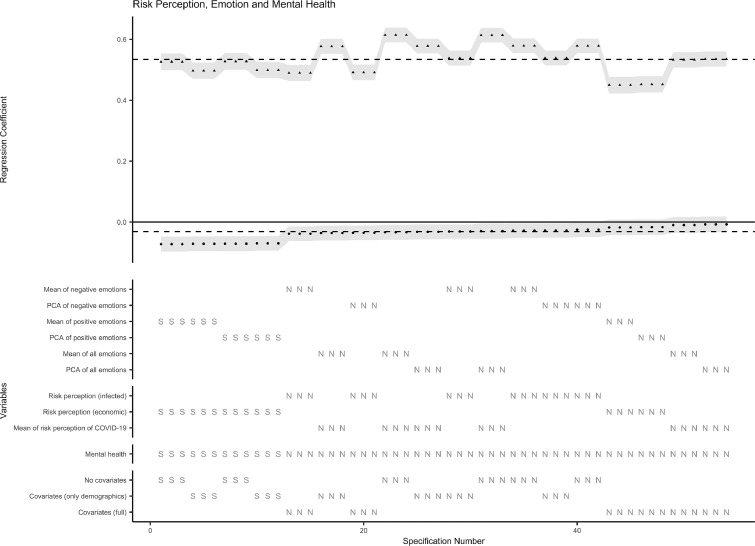
3.3. Specification curve analysis for associations of risk perception and emotion with subsequent mental health
Multilevel linear regression showed a significant inverse association between the average score of risk perception items in baseline survey and self-rated mental health in follow-up survey (standardised β=-0.214, SE=0.029, P<0.001). The association remained significant after adjusting for basic demographics or a full list of covariates (standardised β=-0.201 or -0.143, SE=0.028 or 0.029, P<0.001). Based on this result, an adapted SCA was further conducted to explore whether the inverse association was mediated by emotion. Among the 54 multilevel linear regressions of mental health on both risk perception and emotion, 42 models showed a strong mediation effect, where no significant direct effect of risk perception was found after controlling for emotion (median standardised β=-0.031, median SE=0.024; Fig. 3 ). However, the overall bootstrapped test showed there was still a significant direct effect of risk perception on mental health, with the probability of getting the observed SCA results by chance below 0.001. In contrast, all 54 model specifications indicated a strong positive independent association of emotion with mental health (median standardised β=0.534, median SE=0.025, maximum P=9×10−56; Fig. 3), which was confirmed by the bootstrapped test (P<0.001).
Fig. 3.
The standardised β coefficients for the association of risk perception of COVID-19 with mental health after controlling for emotion in all 54 specifications (listed on x axis) are plotted as black dots at the upper half of the graph; the association of emotion with mental health in the same model specification was also plotted as black triangular (all P<0.001). The error bar (in grey) represents the corresponding standard error (SE). The dashed lines indicate the median standardised β coefficients for risk perception (median standardised β=-0.031, median SE=0.024, median sample size=1403) and emotion (median standardised β=0.534, median SE=0.025). At the lower half of the graph, the corresponding specifications for each level of the four model specification factors are displayed as letter S or N. S refers to significant standardised β coefficients for risk perception (P<0.05); N refers to nonsignificant results (P>0.05).
As shown in Fig. 3, the direct effect of risk perception on mental health was weaker after controlling for the average score of negative emotions (median standardised β=-0.031, median SE=0.024) than controlling for the average score of positive emotions (median standardised β=-0.071, median SE=0.024; Table 2), implying a stronger mediating effect through negative emotions. In addition, the direct effect of economic-risk on mental health (median standardised β=-0.071, median SE=0.024) was stronger compared with that of infection-risk (median standardised β=-0.030, median SE=0.023). Similar as the situation in the previous SCA, adjusting for a full set of covariates resulted in a weaker effect estimate (median standardised β=-0.017, median SE=0.026).
4. Discussion
In this large-scale cross-country study of psychological impact of COVID-19, we found a robust association between risk perception and emotion. Consistent with the literature on emotional reactions during previous pandemic periods (Prati et al., 2011; Yang and Chu, 2018), higher risk perception was associated with higher levels of overall negative emotion and individual negative emotions (anxious, nervous, depressed, exhausted, lonely, bored; in descending order of the magnitude of association). In addition, risk perception had a slightly weaker but significant inverse association with the levels of overall positive emotion and individual positive emotions (relaxed, calm, content, happy, inspired, excited; in descending order of the magnitude of association). These findings imply that reducing unnecessary risk perception or avoiding excessive concern of the pandemic may be a candidate strategy to mitigate emotional distress. For instance, some health institutes such as the UK National Health Service (NHS, 2020) suggested that people should only look for COVID-19 updates less than twice a day.
In addition, this study highlighted the need for caring about people's mental health during the pandemic. Our data showed that higher risk perception was significantly associated with worse self-rated mental health, which was largely mediated by the emotional responses, especially negative emotions. Therefore, mental health issues may be a secondary impact of COVID-19, and early detection and intervention of negative emotions could contribute to the prevention of mental health problems. It is also reasonable that early signs of emotional changes are easier to be modified or properly managed before developing into clinically significant mental disorders (Davey and McGorry, 2019; Galea et al., 2020). In this regard, people should seek psychological or social support in time when suffering from long-lasting or severe emotional distress, either from professional staff or families/friends. On the other hand, although there is a gap between real risk and subjective risk perception, the risk perception is inevitably shaped by the risk environment to which an individual is exposed. Thus, special attention should be paid to the mental health issues of populations at high risk of COVID-19, such as healthcare workers (Cai et al., 2020; Zhou et al. 2020), carers of infected patients, residents in severely affected areas, and the elderly or those with existing comorbidities.
Furthermore, we found that the risk perception of economic consequences is also a remarkable factor associated with emotion and mental health, with an even larger effect estimate than the risk perception of getting infected. Despite the consistent evidence that elevating the risk perception of infection could increase the adoption of health behaviours (Floyd et al., 2000; Sheeran et al., 2014), especially during disease outbreaks (Bish and Michie, 2010; van der Weerd et al., 2011; Rudisill, 2013), no evidence showed risk perception of economic consequences has such health-related behavioural influence. Therefore, interventions on reducing economic risk perception could have higher efficacy on mental health promotion as well as lower safety risk than modifying risk perception of infection. Targeted public policies on economic stability during the COVID-19 pandemic, such as tax relief or offering grants or loans to employees, may help reduce the risk perception of potential financial crisis and minimise its psychological consequences.
This study is the largest cross-country study to date that examined the relationships between risk perception of COVID-19, emotions and mental health. We also collected information on a number of demographic variables, knowledge and social support during the pandemic to control for as potential confounding factors. In addition, as a methodological innovation, we developed an adapted SCA method in this study to achieve the examination of structural mediation effects. Previous conventional SCA studies mostly focused on a bivariate association (Simonsohn et al., 2015; Orben and Przybylski, 2019), where only one response variable and one explanatory variable of interest were considered. In contrast, this adapted SCA included two explanatory variables of interest simultaneously in each model specification, and inspected their independent regression coefficients together across different combinations of model specifications. Moreover, we applied multilevel linear regression with random intercept for the first time into the SCA, in order to account for the multilevel cross-country nature of this dataset.
Several limitations need to be considered when interpreting our results. Since the analyses on risk perception and emotion were based on cross-sectional data, the direction of causal links between them, and the mediating role of emotion in the risk perception-mental health association need to be confirmed by future longitudinal or experimental studies. The emotion regulation during the pandemic could also influence mental health in people with high risk perception and warrants further research (Restubog et al., 2020). Moreover, we did not collect data on physical health, obesity and mental health status at the baseline survey. These factors may influence the risk perception of COVID-19 and lead to potential residual confounding bias. The longitudinal analysis was based on a small subsample with available follow-up data, which may lead to selection bias. Furthermore, the mental health data was collected through self-rating at follow-up survey. Although the single-item measure of self-rated mental health has been shown to correlate well with validated multi-item measures of mental health (e.g., Kessler Psychological Distress Scale, mental health subscales of the Short-Form Health Status Survey, and World Mental Health Clinical Diagnostic Interview Schedule) (Ahmad et al., 2014), a deeper investigation into the clinical diagnosis or primary symptoms of specific mental disorders (e.g., depression and anxiety) during the pandemic is needed for more precise policy recommendations. Similarly, the dimensions of risk perception on COVID-19 may not be completely captured with the two items (infection-risk and economic-risk) in this survey. A comprehensive definition and exploration of the construct of COVID-19 related risk perception (e.g., risk of family members or friends, severity of getting infected) is needed (Dryhurst et al., 2020).
In conclusion, this study demonstrated that the risk perception of COVID-19 was associated with emotional states and mental health. Relevant public health policies on reducing unnecessary risk perception and caring about negative emotions could be beneficial for the prevention of mental health problems during the pandemic.
Contributors
Han and Zheng contributed to the conceptualization, formal analysis, methodology, visualization and writing of original draft. Leander, Bélanger, Agostini, Gützkow, Kreienkamp, Reitsema and van Breen contributed to project administration and funding acquisition. All authors were involved in the conceptualization, data curation and reivew & editing of the manuscript. Leander is the director of the PsyCorona project. Han and Zheng had full access to the data.
Role of the funding source
This study was funded by the University of Groningen (Sustainable Society & Ubbo Emmius Fund); the New York University Abu Dhabi (VCDSF/75-71015); and the Government of Spain (COV20/00086). The funders had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Prior presentations
Partial data and statistical methods of this manuscript have been presented in MathPsych/ICCM 2020 Conference on July 31, 2020 as an oral presentation.
Data availability statement
Data from the PsyCorona Survey may only be used for scientific research purposes. For further details on PsyCorona data re-use, please see https://psycorona.org . R code and scripts to perform the analyses presented in this manuscript can be found on the Open Science Framework at: https://osf.io/jh8vk .
Declaration of Competing Interest
None.
Acknowledgement
The full co-author list of the PsyCorona Collaboration is: Georgios Abakoumkin, University of Thessaly. Jamilah H. B. Abdul Khaiyom, International Islamic University Malaysia. Vjollca Ahmedi, Pristine University. Handan Akkas, Ankara Science University. Carlos A. Almenara, Universidad Peruana de Ciencias Aplicadas. Mohsin Atta, University of Sargodha. Sabahat Cigdem Bagci, Sabancı University. Sima Basel, New York University Abu Dhabi. Edona Berisha Kida, Pristine University. Nicholas R. Buttrick, University of Virginia. Phatthanakit Chobthamkit, Thammasat University. Hoon-Seok Choi, Sungkyunkwan University. Mioara Cristea, Heriot Watt University. Sára Csaba, ELTE Eötvös Loránd University. Kaja Damnjanović, University of Belgrade. Ivan Danyliuk, Taras Shevchenko University. Arobindu Dash, Leuphana University of Luneburg. Daniela Di Santo, University "La Sapienza", Rome. Karen M. Douglas, University of Kent. Violeta Enea, Alexandru Ioan Cuza University. Daiane Gracieli Faller, New York University Abu Dhabi. Gavan J. Fitzsimons, Duke University. Alexandra Gheorghiu, Alexandru Ioan Cuza University. Joanna Grzymala-Moszczynska, Jagiellonian University. Ángel Gómez, Universidad Nacional de Educación a Distancia. Ali Hamaidia, Setif 2 University. Mai Helmy, Menoufia University. Joevarian Hudiyana, Universitas Indonesia. Bertus F. Jeronimus, University of Groningen. Ding-Yu Jiang, National Chung-Cheng University. Veljko Jovanović, University of Novi Sad. Željka Kamenov, University of Zagreb. Anna Kende, Eötvös Loránd University. Shian-Ling Keng, Yale-NUS College. Tra Thi Thanh Kieu, HCMC University of Education. Yasin Koc, University of Groningen. Kamila Kovyazina, Independent researcher, Kazakhstan. Inna Kozytska, Taras Shevchenko University. Joshua Krause, University of Groningen. Arie W. Kruglanski, University of Maryland. Anton Kurapov, Taras Shevchenko National University of Kyiv. Maja Kutlaca, Durham University, University of Osnabrück. Nóra Anna Lantos, ELTE Eötvös Loránd University. Edward P. Lemay, University of Maryland. Cokorda Bagus J. Lesmana, Udayana University. Winnifred R. Louis, University of Queensland. Adrian Lueders, Université Clermont-Auvergne. Najma Iqbal Malik, University of Sargodha. Anton P. Martinez, University of Sheffield. Kira O. McCabe, Vanderbilt University. Jasmina Mehulić, University of Zagreb. Mirra Noor Milla, Universitas Indonesia. Idris Mohammed, Usmanu Danfodiyo University Sokoto. Erica Molinario, University of Maryland. Manuel Moyano, University of Cordoba. Hayat Muhammad, University of Peshawar. Silvana Mula, University "La Sapienza", Rome. Hamdi Muluk, Universitas Indonesia. Solomiia Myroniuk, University of Groningen. Reza Najafi, Islamic Azad University, Rasht Branch. Claudia F. Nisa, New York University Abu Dhabi. Boglárka Nyúl, ELTE Eötvös Loránd University. Paul A. O’Keefe, Yale-NUS College. Jose Javier Olivas Osuna, National Distance Education University (UNED). Evgeny N. Osin, National Research University Higher School of Economics. Joonha Park, NUCB Business School. Gennaro Pica, University "La Sapienza", Rome. Antonio Pierro, University "La Sapienza", Rome. Jonas H. Rees, University of Bielefeld. Elena Resta, University "La Sapienza", Rome. Marika Rullo, University of Siena. Michelle K. Ryan, University of Exeter, University of Groningen. Adil Samekin, International Islamic Academy of Uzbekistan. Pekka Santtila, New York University Shanghai. Edyta Sasin, New York University Abu Dhabi. Birga M. Schumpe, New York University Abu Dhabi. Heyla A. Selim, King Saud University. Michael Vicente Stanton, California State University, East Bay. Wolfgang Stroebe, University of Groningen. Samiah Sultana, University of Groningen. Robbie M. Sutton, University of Kent. Eleftheria Tseliou, University of Thessaly. Akira Utsugi, Nagoya University. Caspar J. Van Lissa, Utrecht University. Kees Van Veen, University of Groningen. Michelle R. vanDellen, University of Georgia. Alexandra Vázquez, Universidad Nacional de Educación a Distancia. Robin Wollast, Université Clermont-Auvergne. Victoria Wai-lan Yeung, Lingnan University. Somayeh Zand, Islamic Azad University, Rasht Branch. Iris Lav Žeželj, University of Belgrade. Andreas Zick, University of Bielefeld. Claudia Zúñiga, Universidad de Chile.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.01.049.
Appendix. Supplementary materials
References
- Ahmad F., Jhajj A.K., Stewart D.E., Burghardt M., Bierman AS. Single item measures of self-rated mental health: a scoping review. BMC Health Serv. Res. 2014;14:398. doi: 10.1186/1472-6963-14-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel C.S. Social stress: theory and research. Annu Rev. Sociol. 1992;18:15–38. doi: 10.1146/annurev.so.18.080192.000311. [DOI] [Google Scholar]
- Bennett D.A. How can I deal with missing data in my study? Aust. N Z J. Public Health. 2001;25(5):464–469. doi: 10.1111/j.1467-842X.2001.tb00294.x. [DOI] [PubMed] [Google Scholar]
- Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br. J. Health Psych. 2010;15:797–824. doi: 10.1348/135910710x485826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in March 2020. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020:gbaa074. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bults M., Beaujean D.J.M.A., de Zwart O., et al. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health. 2011;11(2) doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhamah W., AlKhayyat A., Oroszlányová M., et al. The psychological burden of the COVID-19 pandemic and associated lockdown measures: experience from 4000 participants. J. Affect Disord. 2020;277:977–985. doi: 10.1016/j.jad.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q., Feng H., Huang J., et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J. Affect Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey C.G., McGorry P.D. Early intervention for depression in young people: a blind spot in mental health care. Lancet Psychiat. 2019;6(3):267–272. doi: 10.1016/S2215-0366(18)30292-X. [DOI] [PubMed] [Google Scholar]
- Ding Y., Xu J., Huang S., et al. Risk perception and depression in public health crises: evidence from the COVID-19 crisis in China. Int. J. Environ. Res. Public Health. 2020;17(16):5728. doi: 10.3390/ijerph17165728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryhurst S., Schneider C.R., Kerr J., et al. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020 doi: 10.1080/13669877.2020.1758193. [DOI] [Google Scholar]
- Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J. Med. Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd D.L., Prentice-Dunn S., Rogers R.W. A meta-analysis of research on protection motivation theory. J. Appl. Soc. Psychol. 2000;30(2):407–429. doi: 10.1111/j.1559-1816.2000.tb02323.x. [DOI] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Guidi J., Lucente M., Sonino N., Fava G.A. Allostatic load and its impact on health: a systematic review. Psychother. Psychosom. 2021;90(1):11–27. doi: 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- Kessler R.C. The effects of stressful life events on depression. Annu. Rev. Psychol. 1997;48(1):191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kopetz C.E. The motivation-cognition interface. Routledge; 2017. Risk and self-defeating behaviors as goal pursuit rather than regulatory failure; pp. 124–148. [Google Scholar]
- Leppin A., Aro A.R. Risk perceptions related to SARS and avian influenza: theoretical foundations of current empirical research. Int. J. Behav. Med. 2009;16(1):7–29. doi: 10.1007/s12529-008-9002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenstein G.F., Weber E.U., Hsee C.K., Welch N. Risk as feelings. Psychol. Bull. 2001;127(2):267–286. doi: 10.1037//0033-2909.127.2.267. [DOI] [PubMed] [Google Scholar]
- Lopez-Vazquez E. Risk perception interactions in stress and coping facing extreme risks. Environ. Manag. Health. 2001;12(2):122–133. doi: 10.1108/09566160110389889. [DOI] [Google Scholar]
- Lopez-Vazquez E., Marvan M.L. Risk perception, stress, and coping strategies in two catastrophe risk situations. Soc. Behav. Pers. 2003;31(1):61–70. doi: 10.2224/sbp.2003.31.1.61. [DOI] [Google Scholar]
- Lorah J. Effect size measures for multilevel models: definition, interpretation, and TIMSS example. Large-scale assess educ. 2018 6: 8. 10.1186/s40536-018-0061-2.
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Service, 2020. Mental wellbeing while staying at home. https://www.nhs.uk/oneyou/every-mind-matters/coronavirus-covid-19-staying-at-home-tips/ (accessed 2 October 2020).
- Orben A, Przybylski AK. The association between adolescent well-being and digital technology use. Nat. Hum. Behav. 2019;3(2):173–182. doi: 10.1038/s41562-018-0506-1. [DOI] [PubMed] [Google Scholar]
- Paek H.-J., Hove T. Oxford University Press; Oxford: 2017. Risk Perceptions and Risk Characteristics. [DOI] [Google Scholar]
- Peters E., Slovic P. The role of affect and worldviews as orienting dispositions in the perception and acceptance of nuclear power. J. Appl. Soc. Psychol. 1996;26:1427–1453. doi: 10.1111/j.1559-1816.1996.tb00079.x. [DOI] [Google Scholar]
- Planchuelo-Gómez Á., Odriozola-González P., Irurtia M.J., et al. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect Disord. 2020;277:842–849. doi: 10.1016/j.jad.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Pietrantoni L., Zani B. A social-cognitive model of pandemic influenza H1N1 risk perception and recommended behaviors in Italy. Risk Anal. 2011;31(4):645–656. doi: 10.1111/j.1539-6924.2010.01529.x. [DOI] [PubMed] [Google Scholar]
- Qian M.Y., Ye D.M., Dong W., et al. Behaviour, cognition, and emotion of the public in Beijing towards SARS [in Chinese] Chin. Ment. Health J. 2003;17(8):515–520. doi: 10.1023/A:1022289509702. [DOI] [Google Scholar]
- Qian MY, Ye DM, Zhong J, et al. Behavioural, cognitive and emotional responses to SARS: differences between college students in Beijing and Suzhou. Stress Health. 2005;21(2):87–98. doi: 10.1002/smi.1043. [DOI] [Google Scholar]
- Raude J., Setbon M. Lay perceptions of the pandemic influenza threat. Eur. J. Epidemiol. 2009;24(7):339–342. doi: 10.1007/s10654-009-9351-x. [DOI] [PubMed] [Google Scholar]
- Ren Y., Qian W., Li Z., et al. Public mental health under the long-term influence of COVID-19 in China: geographical and temporal distribution. J. Affect Disord. 2020;277:893–900. doi: 10.1016/j.jad.2020.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restubog S.L.D., Ocampo A.C.G., Wang L. Taking control amidst the chaos: emotion regulation during the COVID-19 pandemic. J. Vocat. Behav. 2020;119 doi: 10.1016/j.jvb.2020.103440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudisill C. How do we handle new health risks? Risk perception, optimism, and behaviors regarding the H1N1 virus. J. Risk Res. 2013;16(8):959–980. doi: 10.1080/13669877.2012.761271. [DOI] [Google Scholar]
- Russell J.A. A circumplex model of affect. J. Pers. Soc. Psychol. 1980;39(6):1161–1178. doi: 10.1037/h0077714. [DOI] [Google Scholar]
- Sheeran P., Harris P.R., Epton T. Does heightening risk appraisals change people's intentions and behavior? A meta-analysis of experimental studies. Psychol. Bull. 2014;140(2):511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Shi L., Lu Z.A., Que J.Y., et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236:280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Siegrist M., Keller C., Kiers H.A.L. A new look at the psychometric paradigm of perception of hazards. Risk Anal. 2005;25:211–222. doi: 10.1111/j.0272-4332.2005.00580x. [DOI] [PubMed] [Google Scholar]
- Simonsohn U., Simmons J.P., Nelson L.D. SSRN; 2015. Specification Curve: Descriptive and Inferential Statistics on All Reasonable Specifications. [DOI] [Google Scholar]
- Slovic P., Finucane M.L., Peters E., MacGregor D.G. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24(2):311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- Soiné H., Kriegel L., Dollmann J. The impact of the COVID-19 pandemic on risk perceptions: differences between ethnic groups in Germany. Eur Soc. 2020 doi: 10.1080/14616696.2020.1825766. [DOI] [Google Scholar]
- Teufel M., Schweda A., Dörrie N., et al. Not all world leaders use Twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J. Public Health. 2020;42(3):644–646. doi: 10.1093/pubmed/fdaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Weerd W., Timmermans D.R.M., Beaujean D.J.M.A., Oudhoff J., van Steenbergen J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health. 2011;11:575. doi: 10.1186/1471-2458-11-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative affect - the Panas scales. J. Pers. Soc. Psychol. 1988;54(6):1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wu D., Yu L., Yang T., et al. The impacts of uncertainty stress on mental disorders of chinese college students: evidence from a nationwide study. Front. Psychol. 2020;11:243. doi: 10.3389/fpsyg.2020.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J.Z., Chu H.R. Who is afraid of the Ebola outbreak? The influence of discrete emotions on risk perception. J. Risk Res. 2018;21(7):834–853. doi: 10.1111/j.1539-6924.2010.01529.x. [DOI] [Google Scholar]
- Yang Z.J. Altruism during Ebola: risk perception, issue salience, cultural cognition, and information processing. Risk Anal. 2016;36(6):1079–1089. doi: 10.1186/1471-2458-11-2. [DOI] [PubMed] [Google Scholar]
- Zhou Y., Wang W., Sun Y., et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: workload should be concerned. J. Affect Disord. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from the PsyCorona Survey may only be used for scientific research purposes. For further details on PsyCorona data re-use, please see https://psycorona.org . R code and scripts to perform the analyses presented in this manuscript can be found on the Open Science Framework at: https://osf.io/jh8vk .