Abstract
Objectives
COVID-19 escalated into a global pandemic affecting countries around the world. As communities shut down to reduce disease spread, all aspects of life have been altered, including sleep. This study investigated changes in sleep patterns and correlates of sleep health in a global sample and examined relationships between sleep health and psychological distress.
Design
Cross-sectional.
Settings
Online survey distributed between April 19 and May 3, 2020.
Participants
Total 6882 participants (18-94 years) across 59 countries.
Measurements
Sleep health (RU-SATED), demographics, pandemic-related factors, mood.
Results
More than half the sample shifted their sleep toward later bed- and wake-times, and more than a third reported increased sleep disturbances during the pandemic. Older age, being partnered, and living in a higher income country were associated with better sleep health, while a stricter level of quarantine and pandemic-related factors (being laid off from job, financial strain, or difficulties transitioning to working from home) were associated with poorer sleep health. Domestic conflict was the strongest correlate of poorer sleep health. Poorer sleep health was strongly associated with greater depression and anxiety symptoms. Participants from Latin America reported the lowest sleep health scores.
Conclusions
COVID-19-associated factors have impacted sleep health on a global level. While our data are correlational, sleep health is strongly linked with mental health and could play a protective role against developing mental distress during pandemic-related isolation. Sleep health should be incorporated into public health messages aimed at helping people cope with the effects of a pandemic to maintain optimal mental and physical health.
Keywords: COVID-19, Sleep health, Mood, Sleep disturbances, Social isolation, Psychological distress
Introduction
The outbreak of COVID-19 in December 2019 rapidly escalated into a global pandemic affecting countries around the world, which imposed social isolation measures to stop the spread of the disease. The mass (home) confinement in addition to the uncertainty of the pandemic led to drastic changes in people's lives, affecting social interaction, work, school, physical activity, and sleep.1 Thus, the COVID-19 pandemic has imposed extreme psychological stress on many individuals, the extent of which we are only just beginning to understand.
Poor sleep is associated with adverse health outcomes, including cardiovascular disease,2 cancer,3 hypertension,4 obesity & diabetes,5 and all-cause mortality,6 as well as psychological disorders such as depression.7 Therefore, maintaining sleep health may be critical to preserving good overall physical and mental health during the COVID-19 pandemic. Initial regional studies conducted during the COVID-19 pandemic have suggested increases in sleep disturbances8., 9., 10., 11., 12., 13. and shifts in sleep patterns14 , 15 in frontline health care workers and the general community. Also, there is preliminary evidence that depression and anxiety levels during the COVID-19 pandemic are elevated and potentially associated with poorer sleep quality (for a review see:11).
Studies that have examined factors related to sleep quality amidst social isolation measures have shown that older age was associated with less difficulties falling asleep during the pandemic, and strict home confinement without working and female sex were associated with increased sleep difficulties in a Portuguese sample of respiratory patients (half of them had a confirmed diagnosis of sleep disordered breathing).10 Also, spending more time outside has been associated with better sleep in the general UK population, though being infected with COVID-19 contributed to worse sleep quality.16 An investigation focusing on health care workers in Bahrain found that female sex and being a nonphysician health-allied member were correlates of poorer sleep quality and moderate-severe stress levels.17 Finally, Wang et al (2020) reported that medical occupation, parental burden, death of a loved one, anxiety, and depression were correlates of poorer sleep quality among Chinese health care workers.9
Due to the novelty of this topic, findings on correlates of sleep behavior and quality during the COVID-19 pandemic are rare and are influenced by different sample populations studied (eg, health care workers, respiratory patients, the general population of a single country), measurement instruments used (with some studies using only a single item for sleep quality), different assessment times across the stages of the pandemic, and small sample sizes. The COVID-19 pandemic has caused massive psychosocial and economic changes for billions of people worldwide simultaneously (eg, working from home, restrictions on seeing family and friends), which could be associated with changes in sleep behavior. Sleep could also be influenced by different lockdown and other pandemic-related mitigation efforts across the world. There is a lack of studies investigating sleep in the general population or global samples, and there is a need for more research to determine the effects of the COVID-19 pandemic on sleep and how those effects are associated with demographic and social isolation specific factors. The current study focuses on sleep health, defined as “a multidimensional pattern of sleep-wakefulness, adapted to individual, social, and environmental demands, that promotes physical and mental well-being.”18 The prioritizing of sleep health in the public health domain is under way,19 and has the advantage over singular sleep measures of addressing the multidimensionality of sleep. Therefore, the purpose of the current study was to investigate correlates of sleep health and its relationship with psychological distress during the COVID-19 pandemic in the general population of 59 countries.
Methods
Participants
Of the initial sample of 9083 people who started the survey, 26 did not consent to participate, and 7 provided a nonsensical name for their city. About 2175 participants did not finish the current survey. Exploratory analyses on the participants who dropped out showed they had similar demographic characteristics; however, they differed as a function of employment status and were slightly more likely to be a student or on disability leave. The final sample consisted of 6882 participants from 59 countries (58.5% upper-middle income countries, according to the Word Bank country classification (https://datahelpdesk.worldbank.org) from 5 continents, who ranged in age from 18 to 94 years old and mostly identified as women (78.8%). The majority reported being employed (included students) (80.1%) and being in a romantic relationship (51.1%). Sociodemographic characteristics are presented in Table 1 . A list of the participating countries with sample size for each country has been published elsewhere.20
Table 1.
Sociodemographic characteristics of the study participants (n = 6882)
| Age (years), M, SD | 42.30 | 13.95 |
|---|---|---|
| Gender, N, % | ||
| Man | 1440 | 20.9 |
| Woman | 5425 | 78.8 |
| Non-binary, transgender, or other | 17 | 0.2 |
| Employment status, N, % | ||
| Active | 5514 | 80.1 |
| Not active | 1368 | 19.9 |
| Relationship status, N, % | ||
| Partnered | 3519 | 51.1 |
| Not partnered | 3363 | 48.9 |
| Dependents at home, N, % | ||
| Children <18 years | 2162 | 31.4 |
| No children | 4720 | 68.6 |
| Country income classification, N, % | ||
| Low | 1 | 0 |
| Lower-middle | 63 | 0.9 |
| Upper-middle | 4025 | 58.5 |
| High | 2793 | 40.6 |
Measures
The online survey consisted of questions covering 5 domains: (1) demographics: age (years), gender (man/women or other), country, employment status (categorized as active/not active), relationship status (categorized as partnered/not partnered), and presence of dependents under the age of 18 years in the home; (2) COVID-19-related quarantine or restriction level; (3) COVID-19 exposure; (4) COVID-19-related change in life; (5) COVID-19-related sleep changes; (6) sleep health, and (7) psychological distress.
In order to determine what kind of quarantine or social isolation measures participants were following at the time of data collection, they were asked to select one of 4 levels of restriction followed in the past week (Level 0—no specific restrictions; Level 1—mild restrictions (eg, not gathering with 10 or more people, not traveling outside city or state); Level 2—moderate restrictions (eg, not leaving home except for working, care of another family member, exercise); Level 3—severe restrictions (eg, not leaving home at all, or only leaving to buy food or medicine).
The Epidemic-Pandemic Impacts Inventory21 was used to determine participant exposure to COVID-19 and to assess how the pandemic impacted different life domains. This inventory originally consisted of 92 statements, 21 of which were used in the survey: “Infection history”—8; “Work and Employment”—7; “Economic”—2; “Home life”—2; and “Social activities”—2. Participants were asked to answer Yes/No about the impact on these specific domains.
To assess changes in sleep behavior (sleep timing, duration, trouble falling asleep, and waking up during the night) during the pandemic, participants were asked to report how each aspect of sleep had changed during the past week compared to before the pandemic using a 5-point scale: much less than usual; less than usual; the same as usual; more than usual; or much more than usual. Participants were also asked to report how much sleep they got in a 24-hour period.
Sleep health and psychological distress were assessed through standardized and validated self-report scales. Sleep health was assessed by the Regulatory Satisfaction Alertness Timing Efficiency Duration (RU-SATED) scale.18 This measure consists of 6 items corresponding to key dimensions of sleep consistently associated with health outcomes: regularity (getting in and out of bed at similar times each day), satisfaction (feeling satisfied with one's sleep), alertness (ability to stay awake during the day without dozing), timing (sleeping between 2:00 a.m. and 4:00 a.m.), efficiency (being awake for less than 30 minutes each night after trying to fall asleep), and duration (obtaining between 6 and 8 hours of sleep per night). Participants were asked to rate the frequency with which they experienced these behaviors on a 3-point Likert scale (0—Rarely /Never; 1—Sometimes; 2—Usually/Always) in the past week. A total score is obtained by summing all items (range: 0-12), with higher scores indicating better sleep health.18 , 22 The scale has been shown to be psychometrically valid.23 Psychological distress was measured using 2 scales. DASS-2124 was used to assess stress and depression over the past week, and the GAD-725 for assessing anxiety over the past 2 weeks. Each DASS-21 scale consists of 7 items of symptoms rated on a 4-point Likert scale. A total score provides a severity index of stress and depression symptoms. The GAD-7 is a 7-item scale scored on a 4-point Likert scale, and higher total scores reflect higher anxiety. Participants’ home countries were classified by income (low, lower-middle, upper-middle, and high) and by geographical region (East Asia and Pacific, Europe and Central Asia, Latin America and the Caribbean, North America, Sub-Saharan Africa, and South Asia; The World Bank, 2017).
Procedure
The survey was created in English by a group of psychologists and health scientists and later translated into Spanish, Italian, German, Turkish, and French. Adapted and validated versions in each language were used for standardized questionnaires, and bilingual native speakers translated and reviewed all items without formal translations to generate a final version. Using a snowball sampling method, the online survey was distributed through social media (WhatsApp, Twitter, and Instagram) and professional emailing lists. In addition, Facebook ads were used to promote participation among the general population and to expand the sample across different countries and age ranges. Data collection took place between April 19 and May 3, 2020.
Before starting the 15-minute survey, participants were provided with a university ethics-committee approved informed consent specifying that participation was completely voluntary and anonymous, and that they would not receive any financial compensation.
Data analysis
All analyses were conducted using IBM SPSS 26. A chi-square test of independence showing associations between sleep quantity (assessed on the RUSATED scale) and reported changes in sleep duration during the pandemic relative to usual times is shown in Table 2 . A bivariate correlation matrix showing the associations among sleep health and demographic characteristics is shown in Table 3 . In order to investigate demographic characteristics, COVID-19-related changes in life, and effects of the pandemic as predictors of sleep health, a hierarchical stepwise multiple linear regression was computed with sleep health as the outcome variable. In this regression, demographic characteristics (man vs woman or nonbinary/trans, age, country income classification, partnered vs not partnered, active vs not active work status, and dependent <18 years in the home vs not) were included as Step 1 variables. Step 2 included variables reflecting participants’ personal exposure to COVID-19. Step 3 included level of quarantine, while Step 4 included effects of the pandemic on participants’ lives.
Table 2.
Significant association between sleep quantity (assessed on the RU-SATED scale) and changes in sleep duration during the pandemic relative to usual times (χ28 = 1652.06, P< .001)
| I have been sleeping |
|||||||
|---|---|---|---|---|---|---|---|
| Much less than usual | Less than usual | The same as usual | More than usual | Much more than usual | Total | ||
| Do you sleep between 6 and 8 hours per day? | Never/Rarely | 222 | 161 | 139 | 41 | 26 | 589 |
| Sometimes | 346 | 747 | 548 | 323 | 84 | 2048 | |
| Usually/Always | 97 | 535 | 2294 | 1131 | 188 | 4245 | |
| Total | 665 | 1443 | 2981 | 1495 | 298 | 6882 | |
Table 3.
Correlation matrix among demographic variables and sleep health
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Sleep health | ||||||
| 2. Man vs woman or nonbinary/trans | 0.021 | |||||
| 3. Age | 0.188* | 0.032** | ||||
| 4. Country income classification | 0.123** | 0.033** | 0.079** | |||
| 5. Partnered vs not partnered | 0.134** | 0.027** | 0.312** | 0.041** | ||
| 6. Active vs not active employment | −0.016 | 0.012 | −0.251** | −0.055* | −0.046** | |
| 7. Dependent <18 years in home vs not | −0.005 | −0.031** | −0.067** | −0.093** | 0.300* | 0.069** |
Because correlations and linear regressions require variables to be continuous or dichotomous, women and the small group of nonbinary/trans individuals were combined in order to compare the connections between the primary study variables and these 2 gender groups relative to men.
P < .05.
P < .01.
Second, sleep health scores were compared by global region using an analysis of covariance (ANCOVA). Demographics included in Step 1 of the previous regression were included as covariates. Participants from South Asia were excluded from the ANCOVA because the small group size precluded meaningful comparisons (n = 4). Finally, a partial correlation matrix was constructed to evaluate the associations among sleep health, depression, anxiety, and stress scores, controlling for demographics. Because of the large number of predictors included in the analyses, significance level was set at P< .01.
Results
Changes in sleep behavior during the COVID-19 pandemic
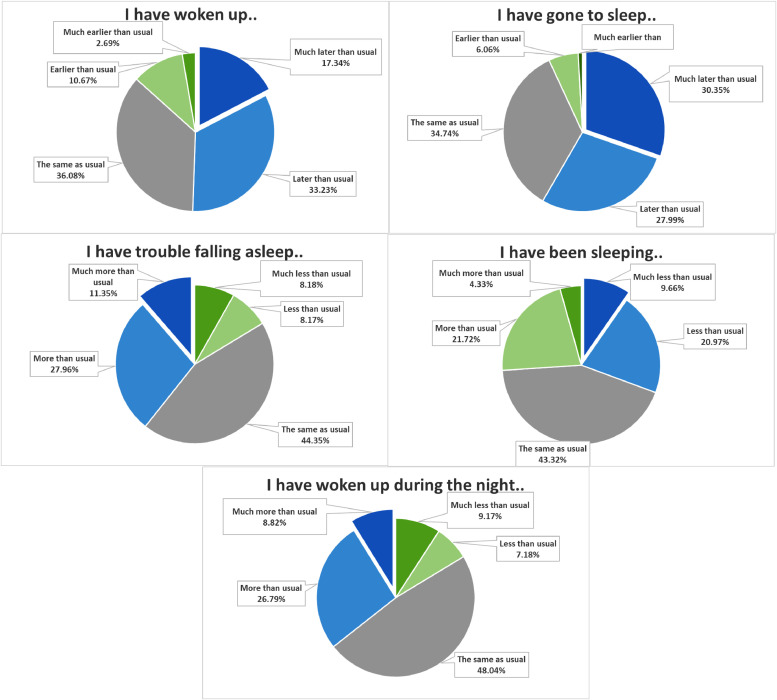
On average, participants reported sleeping 7.1 (standard deviation [SD] = 1.5) hours in a 24-hour period. Compared to prepandemic routines, 58.4% of the participants reported going to bed later/much later than usual and 50.5% reported that that they woke up later/much later than usual. About 30.7% of the participants reported sleeping less/much less than usual, whereas 25.5% reported sleeping more/much more than usual. About 39.3% had trouble falling asleep more/much more than usual, and 35.6% woke up during the night more/much more than usual, compared to pre-pandemic (Fig. 1 ). Sleep quantity (RU-SATED item) and changes in sleep duration during the pandemic relative to usual times were significantly associated (χ2 (8) = 1652.06, P< .001). Individuals who reported usually or always sleeping between 6 and 8 hours per night most often reported that they had been sleeping the same amount as usual or more than usual during the pandemic. Individuals who reported sometimes sleeping 6 to 8 hours per night tended to report sleeping less than usual or the same amount as usual during the pandemic. Participants who reported never or rarely sleeping 6 to 8 hours per night most often reported sleeping less than usual or much less than usual during the pandemic (Table 2).
Fig. 1.
Sleep routines, sleep duration, and sleep disturbances during COVID-19-related quarantine- and isolation measures in late April 2020 relative to usual times in 6882 participants.
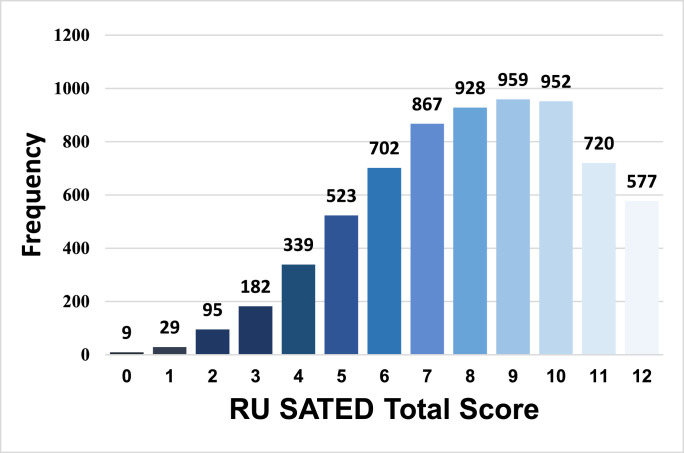
Participants reported an average score of 8.06 (SD = 2.54) on the RU-SATED measure of sleep health. Distribution of sleep health scores was somewhat positively skewed, with fewer participants reporting extremely low levels of sleep health (Fig. 2 ). Although no clinical cutoff scores are currently available for the RU-SATED scale, 3059 participants (44.4%) scored below the median of 7.0 using the 5-item SATED scale, which was used as an indicator of poor sleep health in previous studies of sleep health.22 , 26
Fig. 2.
Histogram of sleep health (RU SATED) scores in the sample of participants (n = 6882). Higher scores reflect better sleep health.
Associations between sleep health and demographics during the COVID-19 pandemic
In the correlation matrix (Table 3), older age, higher country income classification, and being partnered were all associated with better sleep health. Sleep health was not associated with gender, employment, or having a dependent child under 18 years of age in the home.
Correlates of sleep health during the COVID-19 pandemic
Percentages of participants who endorsed each of the predictors in the hierarchical linear regression model have been published elsewhere.20 In order to determine whether multicollinearity might be operating among the factors in the stepwise regression model, correlations were calculated among all predictors. No correlation coefficient exceeded an absolute value of 0.425, suggesting a lack of multicollinearity; as a result, nonsignificance of individual predictors within the model (including within each step of the regression model) could not be accounted for by overlapping predictors.
In the hierarchical linear regression predicting sleep health, Step 1 was statistically significant, F(6, 6875) = 65.92, R2 = 0.054, P< .001. Consistent with the correlation matrix, sleep health was significantly and uniquely associated with older age, higher country income classification, and being partnered. Sleep health was not associated with gender (ie, identifying as a man vs identifying as a woman or as transgender). However, inconsistent with the bivariate correlations, sleep health was positively associated with being employed. With the addition of COVID-19 exposure predictors in Step 2, the overall model was still statistically significant, F(14, 6867) = 30.38, R2 = 0.058, P< .001. Within this model, currently having symptoms of the disease but not having been tested was significantly associated with poorer sleep health. Stricter quarantine level (Step 3) significantly predicted lower sleep health, P< .001, and the overall model was significant, F(15, 6866) = 29.32, R2 = 0.060, P< .001. After the Step 4 addition of effects of the pandemic on one's life, the overall model was still significant, F(28, 6853) = 32.04, R2 = 0.116, P< .001 (Table 4 ), and explained 11.6% of the variance of sleep health. Within this step, significant correlates of poorer sleep health included getting laid off from one's job or closing one's business, having a hard time transitioning to working from home, being unable to get enough food or healthy food, being unable to pay important bills, and experiencing an increase in verbal arguments or conflict with other adults in the home. Two variables that significantly predicted sleep health in previous steps, being employed and currently having symptoms of the disease but having not been tested, were no longer significant after the addition of Step 4 predictors. Notably, having increased verbal conflicts with other adults in the home emerged as the strongest correlate of sleep health out of all variables in the model at Step 4.
Table 4.
Sleep health multiple regression with standardized B-weights from the final model that included 4 steps
| Sleep health |
||
|---|---|---|
| Predictor variable | β | P value |
| Entered in Step 1 | ||
| Man vs woman or nonbinary/trans | −0.005 | .685 |
| Age | 0.118 | <.001 |
| Country income classification | 0.057 | <.001 |
| Partnered vs not partnered | 0.079 | <.001 |
| Employed vs unemployed | 0.031 | .017 |
| Dependent <18 years old in home vs not | 0.006 | .714 |
| Entered in Step 2 | ||
| Currently have symptoms of this disease but have not been tested | −0.027 | .027 |
| Tested and currently have this disease | −0.013 | .310 |
| Had symptoms of this disease but never tested | 0.010 | .434 |
| Tested positive for this disease but no longer have it | 0.014 | .292 |
| Got medical treatment due to severe symptoms of this disease | −0.023 | .065 |
| Hospital stay due to this disease | 0.013 | .322 |
| Someone died of this disease while in our home | 0.012 | .309 |
| Death of close friend or family member from this disease | −0.017 | .150 |
| Entered in Step 3 | ||
| Quarantine level | −0.043 | .001 |
| Entered in Step 4 | ||
| Laid off from job or had to close own business | −0.060 | <.001 |
| Reduced work hours or furloughed | −0.020 | .105 |
| Had to continue to work even though in close contact with people who might be infected | −0.006 | .633 |
| Provided direct care to people with the disease | −0.036 | .004 |
| Increase in workload or work responsibilities | −0.012 | .345 |
| Hard time doing job well because of needing to take care of people in the home | −0.023 | .079 |
| Hard time making the transition to working from home | −0.050 | <.001 |
| Unable to get enough food or healthy food | −0.092 | <.001 |
| Unable to pay important bills like rent or utilities | −0.046 | <.001 |
| Had a child in home who could not go to school | 0.013 | .400 |
| Increase in verbal arguments or conflict with other adult(s) in home | −0.143 | <.001 |
| Separated from family or close friends | −0.029 | .020 |
| Events/celebrations cancelled or restricted | 0.013 | .292 |
Because correlations and linear regressions require variables to be continuous or dichotomous, women and the small group of nonbinary/trans individuals were combined in order to compare the connections between the primary study variables and these 2 gender groups relative to men.
Differences in sleep health across global regions during the COVID-19 pandemic
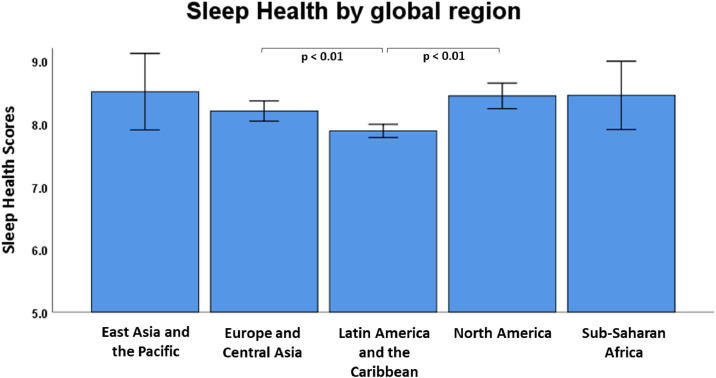
In the ANCOVA predicting sleep health, there was a statistically significant effect of global region, F(4, 6867) = 5.31, P< .001, partial-eta2 = 0.003 (Fig. 3 ). Bonferroni-corrected post hoc pairwise comparisons showed that participants from Latin America and the Caribbean (M = 7.79, SD = 2.47) reported significantly poorer sleep health than participants from Europe and Central Asia (M = 8.32, SD = 2.56; P< .001) and North America (M = 8.64, SD = 2.60; P< .001). No other significant differences emerged, although participants from Latin America and the Caribbean tended to exhibit poorer sleep health than participants from East Asia and the Pacific (M = 8.72, SD = 2.67; P= .029) and Sub-Saharan Africa (M = 8.64, SD = 2.50, P= .025), and participants from Europe and Central Asia tended to experience poorer sleep health than participants from North America (P= .019).
Fig. 3.
Covariate-adjusted sleep health (RU SATED) scores (mean with 95% confidence intervals) by global region in a sample of 6882 participants. Sleep health scores were significantly lower in participants from Latin America and the Caribbean than in participants from North America or Europe and central Asia at P < .01 after Bonferroni corrections. Note. Means were adjusted for the following covariates: gender, age, country income classification, marital status, work status, and having dependents in the home.
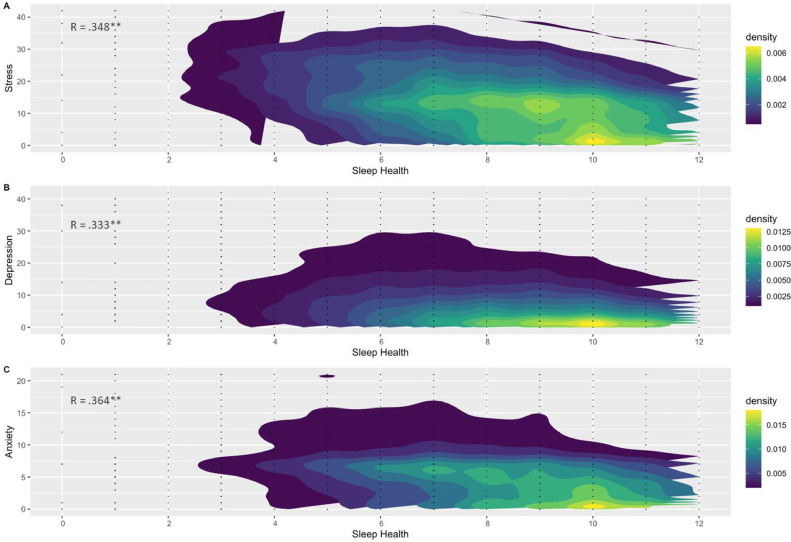
Associations between sleep health and psychological distress during the COVID-19 pandemic
All associations among sleep health, depression, anxiety, and stress were highly significant (Fig. 4 , P< .01). Sleep health demonstrated moderate negative associations with depression, anxiety, and stress scores, after controlling for demographic variables (gender, age, country income classification, marital status, work status, and having dependents in the home).
Fig. 4.
Scatter density plots of the partial correlations among sleep health, depression, anxiety and stress, adjusting for the following covariates: gender, age, country income classification, marital status, work status, and having dependents in the home. Darker colors represent a lower density of the distribution, and lighter colors represent a higher density. A lower sleep health was associated to higher levels of depression, anxiety and stress (P < .01).
Discussion
This study investigated correlates of sleep health during the COVID-19 pandemic in the general adult population of 59 countries. A number of significant correlates were identified with demographic characteristics such as older age, having a partner, and living in a higher-income country being associated with better sleep health, and a stricter level of quarantine being associated with a poorer sleep health. In addition, the strongest correlate of poorer sleep health emerged from COVID-19-related life changes including being laid off from job, having difficulty transitioning to working from home, or being unable to pay important bills, and most significantly, increases in verbal arguments or conflicts at home. A large proportion of participants reported changed sleep patterns toward later bed- and wake-times, and greater sleep disturbances as compared to prepandemic routines. Participants from Latin America and the Caribbean exhibited the lowest sleep health scores. Poorer sleep health was correlated with higher depression, anxiety, and stress, reflecting the close relationship between sleep and mood.
Changes in sleep patterns during the COVID-19 pandemic
Healthy sleep is associated with enhanced mood,27 improved immune functioning,28 and better physical health.22 , 26 For these reasons, healthy sleep is likely vital during the COVID-19 pandemic. Early regional studies during the pandemic have indicated that sleep disturbances8., 9., 10., 11. , 17 and changes in sleep patterns14 , 15 are common. The current findings extend those of these regional studies to show substantial changes in sleep behavior in a global general population sample.
Almost 60% of participants reported going to bed (much) later, and ~50% stated that they woke up (much) later, compared to prepandemic routines. With this delay in timing on both sides of the sleep period, changes in sleep duration varied, with some (~26%) reporting sleeping more than usual, possibly due to having less constraints on their sleep, whereas others (~43%) reported no change, and the remaining (~31%) reported sleeping less than usual. More than a third of the sample claimed to have more trouble falling asleep or waking up more often during the night than pre-pandemic, indicating profound changes in sleep routines and increased sleep disturbances. Results are in line with those of others,14 who reported later bed- and wake-times, more time in bed, and paradoxically lower sleep quality during the initial period of lockdown in young Italian adults. Notably, sleep quantity during the pandemic was associated with pandemic-related changes in sleep duration, such that participants who reported rarely or never sleeping 6 to 8 hours per night indicated that they were sleeping less or much less than usual compared to prepandemic times. This finding further emphasizes the importance of maintaining regular sleep schedules during quarantine- and lockdown measurements. Shifts in sleep schedules may lead to negative consequences such as reduced daylight exposure or physical activity,29 further affecting mood and health.
Correlates of sleep health during the COVID-19 pandemic
Several demographic factors were associated with better sleep health, including older age, being partnered, and living in a country with a higher income classification. Older age has previously been associated with a better sleep quality and less lockdown-related sleep changes during the COVID-19 pandemic,10 , 16 suggesting age as a protective factor for maintaining sleep health during quarantine and restriction measures. Being partnered and living in a higher income classification country—factors that are characterized by providing a certain degree of security and life stability—also were associated with better sleep health. However, the strictness in the level of quarantine—which differed across the global sample from strict home confinement to lighter restrictions—was associated with a poorer sleep health. Even though this finding has not been previously reported, Pinto et al10 found that strict home confinement without working was associated with increased sleep difficulties in respiratory patients during the lockdown measures in Portugal. Stricter quarantine levels potentially decrease time spent outside, physical activity, and sunlight expose, which is vital for maintaining healthy circadian rhythms, sleep, and mood.30 Even though some studies indicated female sex as a predictor of sleep disturbances during the COVID-19 pandemic,17 , 31 the current study found that gender was not associated with overall sleep health. Similarly, in a sample of adults studied in the United States in nonpandemic times, while women reported more insomnia symptoms and lower sleep self-efficacy than men, reflecting the common finding that women report a poorer sleep quality than do men, overall sleep health did not differ according to gender.23
Most correlates of poorer sleep health emerged from the individual COVID-19-related life changes such as being laid off from work or closing one's business, having difficulty transitioning to working from home, being unable to pay important bills, or the inability to get enough or healthy food. Not surprisingly, financial and socioeconomic burdens are a major stress factor linked to sleep disturbances,32 and can exacerbate an already stressful experience of the COVID-19 pandemic. Increases in verbal arguments or conflict with other adults in the home emerged as the strongest correlate of a poorer sleep health during the pandemic. Current research urgently warns of a dramatic increase in domestic conflicts around the globe during the pandemic, primarily caused by stresses such as isolation and economic vulnerability.33 Associations between family strain and sleep disturbances have been reported outside of the pandemic which may reflect a bidirectional relationship, such that stressful relationships with others at home could interfere with sleep and inadequate or poor quality sleep could contribute to stressful relationships.34 Although some correlates reported are also associated with sleep in nonpandemic times (eg, family conflict or financial burden), significantly more people are directly affected by these conditions during the COVID-19 pandemic, making these factors a global concern with an urgent need for further investigation.
Interestingly, in contrast to other studies,16 none of the correlates reflecting COVID-19 exposure reached significance, and COVID-19 exposure-related variables only accounted for an additional 0.4% of the variance in sleep health in the step-wise regression. Quarantine and isolation characteristics (resulting in feelings of anxiety, worry, and distress) could have surpassed the influence of the presence of the virus in the immediate vicinity on sleep health. It could be that not the objective exposure to COVID-19, but rather the subjective experience of the pandemic influences sleep health. However, the current sample was relatively underexposed to actual COVID-19 disease at the time of data collection, and further work is needed to investigate sleep health in the context of infection and recovery from COVID-19.
Global differences in changes of sleep health during the pandemic
Participants from Latin America and the Caribbean area reported the lowest total scores in sleep health relative to European and Central Asian as well as North American participants, although pandemic-related quarantine and isolation measures were ongoing in all regions at the time of data collection. However, at the time of data collection, the number of cases in Latin America and the Caribbean area were lower compared to other global regions. To our knowledge, no studies have yet compared sleep health on a global level during the pandemic, but previous research suggests a high prevalence of sleep difficulties35 and sleep-related symptoms, eg, excessive daytime sleepiness or insomnia,36 in the Latin American population. Possibly, sleep health was already lower in this population, although further reasons beyond what was measured in the current study that contributed to this finding need to be determined.
Sleep health and mood during the pandemic
Previous studies reported associations between lower mood, higher anxiety- or stress levels, and worsened sleep quality or sleep behavior during the COVID-19 pandemic in different countries and populations.12 , 13 , 16 , 37., 38., 39. The current results are in line with previous research, suggesting higher levels of anxiety, depression, and stress being associated with poorer sleep health. These results emphasize the importance of maintaining good sleep health during the pandemic, since poorer sleep health may trigger or exacerbate mental health disorders.
Future research and limitations
The current study was cross-sectional and included mostly female participants from middle- and high-income countries that were in different stages of the pandemic. Causality and generalizability of the findings, therefore, should be considered with caution. The final regression model explained roughly 11% of the variance, and there is more research needed to identify other key factors related to sleep health during the COVID-19 pandemic. Since no data were collected on multimorbidity of health conditions, which is strongly associated with sleep health,40 we were unable to determine the relationship between sleep and other health problems in this sample. The current study employed a virtual snowball sampling technique to collect data, which includes some limitations such as specific populations might not have internet access, but also advantages such as an extended geographical radius to reach potential participants.41 A virtual snowball sampling method using social networks such as Facebook has been shown to be an effective method to engage “hard to reach” populations.41 This study has a limitation due to sample selection since just over 2000 participants did not finish the current survey. These participants showed similar demographic characteristics; however, they differed as a function of employment status. Also, the current data represent a partial snapshot of the pandemic since data were collected during a single time point when the included countries were in the mid-phase of the social isolation measures, and may not be generalizable to later stages of the pandemic. Interestingly, there were no associations between the objective exposure to the virus (eg, experiencing symptoms of the virus infection) and sleep health, which may indicate that the impact of the COVID-19-related quarantine- and isolation measures are more correlated to sleep health than the objective presence of the virus, or could be due to the low sample size of participants with COVID-19 exposure. Reasons for this finding need to still be determined, and future studies should specifically focus on COVID-19 patients and their relatives, employing longitudinal study designs to investigate disease-related effects on sleep health. Although the COVID-19 pandemic is undoubtedly still affecting billions of people, the full extent of its consequences is still unclear, and more research is needed to understand the long-term impacts on health, including sleep.
Conclusion
Physiological and psychological consequences of the COVID-19 pandemic are far-reaching and wide-ranging, not only affecting people directly involved such as frontline health care workers or patients, but also the general population. Maintaining a healthy sleep has become challenging during the pandemic. Our investigation is one of the first showing the impact of the COVID-19 pandemic on sleep health in a large global sample. It is likely that risk factors of a poorer sleep health, primarily caused by profound disruption of daily life (ie, working from home, school closures or social isolation), will persist in the pandemic for many people. Current research also indicates that sleep disturbances will likely accelerate anxiety, depression, and suicidal behavior during the COVID-19 pandemic,42 and may put individuals at a higher risk for long-term adverse health effects,1 which is a call for public health interventions.
Having healthy sleep is key to overall health. Sleep is a modifiable behavior, and sleep health can be strengthened by implementing habits including increased time spent outside while social distancing (to increase sunlight exposure and physical activity), as well as keeping regular sleep routines (ie, maintaining similar bed- and wake-times on all days of the week while avoiding under- or over-sleeping). At the public health level, sleep health should be supported by increasing public awareness, and ensuring education programs so that chronic sleep problems caused or aggravated by major life stresses such as the COVID-19 pandemic can be detected early to avoid chronicity. Attention should be directed to prevent, monitor, and treat sleep problems on a global level to strengthen sleep and overall health during the COVID-19 pandemic and during any future epidemic/pandemic outbreaks.
Declaration of conflict of interest
The authors report no conflict of interests related to the submission of this manuscript.
Funding
Ramos-Usuga was supported by a predoctoral fellowship from the Basque Government (PRE_2019_1_0164).
McKee was supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Medical Research Service of the Veterans Affairs Central Virginia Health Care System, and the Department of Veterans Affairs Mid-Atlantic Mental Illness Research, Education, and Clinical Center (MIRECC).
Caffarra was funded by the European Commission (H2020-MSCA-IF-2018-837228-ENGRAVING).
Copyright statement
Since Dr McKee is an employee of the US Government and contributed to the manuscript “Sleeping when the world locks down: Correlates of sleep health during the COVID-19 pandemic across 59 countries” as part of her official duties, the work is not subject to US copyright.
Disclaimer
The contents of this manuscript do not represent the views of the US Department of Veterans Affairs or the United States Government.
Acknowledgments
We thank everyone involved in this project for their efforts in translating and distributing the survey including Harun Yuksel, Gabriele Yuksel-Schroder, Ali Yilmaz, Arda Yilmaz, Martin Hansch, Severine Lannoy, Anne-Pascale Le Berre, and Cristian Logatt. We also thank all research participants for their time and effort in filling out the questionnaires.
References
- 1.Morin CM, Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brindle RC, Yu L, Buysse DJ. Empirical derivation of cutoff values for the sleep health metric and its relationship to cardiometabolic morbidity: results from the Midlife in the United States (MIDUS) study. Sleep. 2019:42. doi: 10.1093/sleep/zsz116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.von Ruesten A, Weikert C, Fietze I. Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. PLoS One. 2012;7:e30972. doi: 10.1371/journal.pone.0030972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gangwisch JE, Heymsfield SB, Boden-Albala B. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 5.Grandner MA, Patel NP, Perlis ML. Obesity, diabetes, and exercise associated with sleep-related complaints in the American population. Z Gesundh Wiss. 2011;19:463–474. doi: 10.1007/s10389-011-0398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cappuccio FP, D'Elia L, Strazzullo P. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015;32:664–670. doi: 10.1002/da.22386. [DOI] [PubMed] [Google Scholar]
- 8.Li DJ, Ko NY, Chen YL. COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: a Facebook survey. Int J Environ Res Public Health. 2020:17. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang W, Song W, Xia Z. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei Province, China. Front Psychiatry. 2020;11:733. doi: 10.3389/fpsyt.2020.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinto J, van Zeller M, Amorim P. Sleep quality in times of Covid-19 pandemic. Sleep Med. 2020;74:81–85. doi: 10.1016/j.sleep.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casagrande M, Favieri F, Tambelli R. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cellini N, Canale N, Mioni G. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krishnan V, Gupta R, Grover S, Basu A. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62:370–375. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carrigan N, Wearn AR, Meky S. Sleep quality, mental health and circadian rhythms during COVID lockdown: results from the sleep quest study. medRxiv. 2020 doi: 10.1101/2020.07.08.20148171. 2020.2007.2008.20148171. [DOI] [Google Scholar]
- 17.Jahrami H, BaHammam AS, AlGahtani H. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2020 doi: 10.1007/s11325-020-02135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaput JP. The integration of pediatric sleep health into public health in Canada. Sleep Med. 2019;56:4–8. doi: 10.1016/j.sleep.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 20.Alzueta E, Perrin P, Baker FC. How the COVID-19 pandemic has changed our lives: a study of psychological correlates across 59 countries. J Clin Psychol. 2020 doi: 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- 21.Grasso DJ, Briggs-Gowan MJ, Ford JD. University of Connecticut School of Medicine; 2020. The Epidemic – Pandemic Impacts Inventory (EPII) [Google Scholar]
- 22.Dalmases M, Benitez I, Sapina-Beltran E. Impact of sleep health on self-perceived health status. Sci Rep. 2019;9:7284. doi: 10.1038/s41598-019-43873-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ravyts SG, Dzierzewski JM, Perez E. Sleep health as measured by RU SATED: a psychometric evaluation. Behav Sleep Med. 2019;19:48–56. doi: 10.1080/15402002.2019.1701474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Osman A, Wong JL, Bagge CL. The depression anxiety stress scales-21 (DASS-21): further examination of dimensions, scale reliability, and correlates. J Clin Psychol. 2012;68:1322–1338. doi: 10.1002/jclp.21908. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 26.Dalmases M, Benitez ID, Mas A. Assessing sleep health in a European population: results of the Catalan Health Survey 2015. PLoS One. 2018;13 doi: 10.1371/journal.pone.0194495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Triantafillou S, Saeb S, Lattie EG. Relationship between sleep quality and mood: ecological momentary assessment study. JMIR Ment Health. 2019;6:e12613. doi: 10.2196/12613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Besedovsky L, Lange T, Haack M. The sleep-immune crosstalk in health and disease. Physiol Rev. 2019;99:1325–1380. doi: 10.1152/physrev.00010.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Altena E, Baglioni C, Espie CA. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020:e13052. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 30.Blume C, Garbazza C, Spitschan M. Effects of light on human circadian rhythms, sleep and mood. Somnologie (Berl) 2019;23:147–156. doi: 10.1007/s11818-019-00215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gualano MR, Lo Moro G, Voglino G. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020:17. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hall M, Buysse DJ, Nofzinger EA. Financial strain is a significant correlate of sleep continuity disturbances in late-life. Biol Psychol. 2008;77:217–222. doi: 10.1016/j.biopsycho.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campbell AM. An increasing risk of family violence during the Covid-19 pandemic: strengthening community collaborations to save lives. Forensic Sci Int Rep. 2020:2. doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ailshire JA, Burgard SA. Family relationships and troubled sleep among U.S. adults: examining the influences of contact frequency and relationship quality. J Health Soc Behav. 2012;53:248–262. doi: 10.1177/0022146512446642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blanco M, Kriber N, Cardinali DP. A survey of sleeping difficulties in an urban Latin American population. Rev Neurol. 2004;39:115–119. [PubMed] [Google Scholar]
- 36.Bouscoulet LT, Vazquez-Garcia JC, Muino A. Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med. 2008;4:579–585. [PMC free article] [PubMed] [Google Scholar]
- 37.Sun L, Sun Z, Wu L. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv. 2020 doi: 10.1101/2020.03.06.20032425. 2020.2003.2006.20032425. [DOI] [Google Scholar]
- 38.Xiao H, Zhang Y, Kong D. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xiao H, Zhang Y, Kong D. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nicholson K, Rodrigues R, Anderson KK. Sleep behaviours and multimorbidity occurrence in middle-aged and older adults: findings from the Canadian longitudinal study on aging (CLSA) Sleep Med. 2020;75:156–162. doi: 10.1016/j.sleep.2020.07.002. [DOI] [PubMed] [Google Scholar]
- 41.Baltar F, Brunet I. Social research 2.0: virtual snowball sampling method using Facebook. Internet Res. 2012;22:57–74. [Google Scholar]
- 42.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]